Abstract
The purpose of our study was to determine the effectiveness of a postoperative autologous blood reinfusion system as an alternative to homologous, banked blood transfusions in total knee arthroplasty. We carried out a prospective randomised controlled study on 60 patients having unilateral total knee replacements. In all these patients, the same surgical team applied the same surgical technique, and all patients followed the same rehabilitation program. In 30 of these patients (group A), a reinfusion system of unwashed salvaged blood was applied, and they were supplemented postoperatively with banked blood transfusions when required. A control group of 30 patients (group B), in whom standard suction drains were used, received one unit of homologous banked blood transfusion intraoperatively and additional blood transfusions postoperatively when required. The administration of banked blood transfusion was determined by the haemoglobin value (<9 mg/dl) and/or clinical signs (blood pressure, pulse, etc.). The values of haemoglobin, haematocrit and platelets were recorded preoperatively and the first, fifth and 15th postoperative days, respectively. Five patients of group A required nine units of homologous blood (0.3 units/patient) postoperatively. Ten patients of group B required an additional 15 banked blood units postoperatively (in total 45 banked blood units for group B; 1.5 units/patient). In the study group, the total homologous blood requirements were reduced by 80%, while the postoperative blood requirements were reduced by 50%. There was no significant difference in the postoperative haematocrit and haemoglobin values between the two groups. The cost of the blood management in the study group was reduced by 36%. The use of an autologous blood reinfusion system reduces highly effectively the demands of homologous banked blood transfusion in total knee arthroplasty.
Résumé
Le but de cette étude était de déterminer l’efficacité d’un système de réinjection post-opératoire de sang autologue comme alternative à la transfusion homologue dans l’arthroplastie totale de genou. Nous avons fait une étude prospective randomisée sur 60 patients opérés d’une prothèse totale du genou unilatérale. Chez 30 patients (groupe A) un système de réinjection sans lavage du sang préservé était utilisé avec supplémentation post-opératoire par du sang de banque si nécessaire. Un groupe de contrôle de 30 patients (groupe B), chez qui un drainage aspiratif classique était utilisé, recevait une unité de sang homologue pendant l’intervention et des transfusions post-opératoires si nécessaire. L’indication de transfusion homologue était posé sur un taux d’hémoglobine < 9mg/dL et/ou des signes cliniques. Les valeurs de l’hémoglobine, de l’hématocrite et des plaquettes étaient relevées avant l’intervention et les premier, cinquième et quinzième jours post-opératoires. 5 patients du groupe A eurent besoin après l’opération de 9 unités de sang homologue (0,3 unité par patient). 10 patients du groupe B eurent besoin de 15 unités supplémentaires de sang homologue après l’opération (au total 45 unités de sang homologue pour le groupe B ; 1,5 unités par patient). Dans le groupe étudié la nécessité globale de sang homologue était réduite de 80% et la nécessité de transfusion post-opératoire de 50%. Le coût de la gestion du sang était réduite de 36% dans le groupe étudié. l’utilisation d’un système de réinjection du sang autologue réduit significativement la nécessité de transfusion homologue dans l’arthroplastie totale du genou.
Introduction
The goal of blood management in orthopaedic and trauma surgery is to minimise exposure to allogenic blood transfusion in elective surgical procedures. Unilateral total knee replacement can result in a substantial blood loss, and 30–50% of these patients receive an allogenic blood transfusion [27, 28]. Since allogenic blood is very expensive with potential disadvantages to the patient [5, 25], different methods to avoid allogenic blood transfusions in these patients have been developed [29, 30]. Among them, preoperative autologous blood donation, perioperative blood salvage and the administration of drugs to either reduce blood loss or stimulate erythrocyte production have been tried with different degrees of effectiveness [29, 30]. In a randomised study that was held in our department, we tried to evaluate if postoperative reinfusion in primary knee arthroplasty is an effective way to avoid allogenic blood transfusions.
Patients and methods
Our study was based on the hospital records of the general surgical department of the General Hospital of Amfissa, a small town of 8,000 inhabitants and the capital of the Prefecture of Phokida. The hospital serves a population of 42,000 inhabitants.
We carried out a prospective randomised controlled study on 60 patients who underwent unilateral total knee arthroplasty between January 2002–November 2004. There were 47 female and 13 male patients with a mean age of 69.7 years. All the patients were operated on for primary osteoarthritis by the same surgeon and the same surgical team using the same operating technique and following the same rehabilitation program. We examined two similar groups of patients. In group A, consisting of 30 patients (24 female and 6 male patients; mean age 69.2 years), no banked blood unit was given intraoperatively. A reinfusion system of unwashed salvaged blood was used. The type of reinfuser used was a Gish Orthofuser. In all surgical procedures, a tourniquet was applied and deflated before knee closure. The collection of shed blood was completed and reinfusion started within six hours of initiating the collection, following the American Association of Blood Banks Guidelines for salvage and reinfusion. Homologous blood transfusion was supplied postoperatively when required. In group B (the control group), consisting of 30 patients (23 female and 7 male patients; mean age: 70.2 years old), one banked blood unit was given intraoperatively, and a standard wound drainage system was used. Homologous blood transfusion was administered postoperatively when required.
The anaesthetist estimated blood losses in both the operation theatre and the anaesthetic recovery unit. In the ward, measurement of postoperative blood loss and decisions on postoperative transfusions were made by the attending surgeon.
The criteria for homologous blood transfusion postoperatively were the values of haemoglobin (lower than 9 g/dl) in correlation with the clinical signs of the patient.
The values of haemoglobin, haematocrit and platelets were recorded preoperatively and the first, fifth and 15th days postoperatively.
A set of demographics and clinical data was collected for all patients, including age, gender, height, weight, co-morbidities, preoperative treatments, type of anaesthesia, tourniquet and operation time, intra- and postoperative blood losses, volume of unwashed blood salvage returned, number of autologous blood transfusions, perioperative haemoglobin values and the length of hospital stay. Statistical analysis of the results was performed using Student’s t-test and the chi-square test.
Results
In group A, the average blood reinfused was 808 ml (range 300–1,750 ml). The total amount of homologous blood required was nine units (mean: 0.3 units/patient).
In group B, the average blood loss in the drainage was 564 ml (range 350–1,500 ml). Fifteen units of banked blood were transfused postoperatively in ten patients. The total amount of homologous blood required was 45 units (mean: 1.5 units/patient).
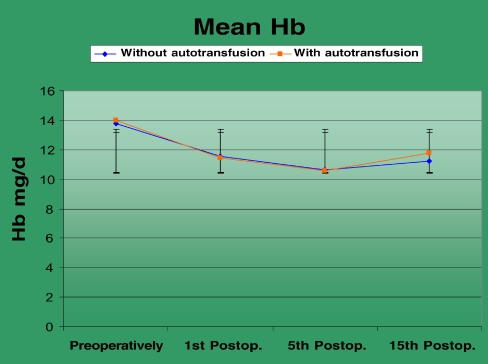
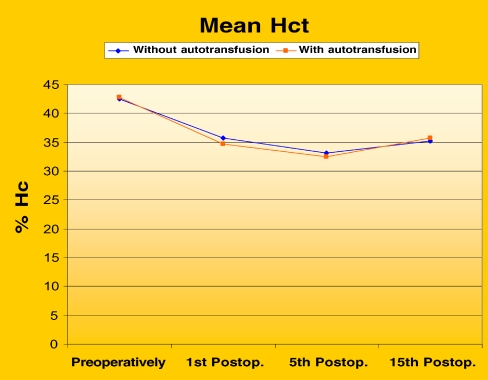
Postoperatively, homologous blood transfusion was required by 16.6% of the patients of group A and 33.3% of the patients of group B. The number of patients who required homologous blood transfusion in the postoperative period was reduced by 50% in the study group (group A) and by 80% in the total mean homologous blood requirements. There were no significant differences in the postoperative haemoglobin and haematocrit values between the two groups (Figs. 1 and 2).
Fig. 1.
The values of haemoglobin preoperatively, the 1st, 5th and 15th post-operative days in patients of groups A and B
Fig. 2.
The values of haematocrit preoperatively, the 1st, 5th and 15th post-operative days in patients of groups A and B
Correlation analysis was used to assess the significance of the relationship between the total demand of blood transfusion in groups A and B. Values of P<0.05 were regarded as significant.
None of the patients developed any adverse reactions after reinfusion.
Discussion
Total knee arthroplasty (TKA) regularly results in a postoperative requirement of blood transfusion. Because of the disadvantages of allogeneic blood transfusion (ABT) such as the risk of transfusion-associated infections, incompatibility-related transfusion fatalities or immunomodulatory effects, a continuing effort to reduce allogeneic blood transfusion is important. For this purpose, the effect of reinfusion of drain blood via a postoperative wound drainage and reinfusion system on the need for allogeneic blood transfusion was evaluated.
Bieurbaum et al. [2], in a study based on 10,000 patients, reported the serious hazards of allogenic blood transfusion on patients who had had a total joint arththroplasty. They found a rate of infection (deep infection, wound infection, chest infection, urinary tract infection and others) of 7% in transfused patients compared with 3% for those who did not require a blood transfusion. It was also noted that each transfused patient stayed in the hospital for one additional day. Similar observations were made in other studies [4, 16]. The exact mechanism that results in higher rates of febrile episodes and wound problems after homologous transfusion has yet to be determined, but it seems that these problems can be reduced by avoiding the use of bank blood [6, 7, 10, 24]. It is therefore clearly preferable not to transfuse blood if possible, especially in orthopaedic surgery in which deep infection is a devastating complication.
Many studies have been carried out concerning when an orthopaedic patient should be transfused postoperatively. Adams and Lundy in 1942 proposed that patients should be transfused when the postoperative haemoglobin level falls bellow 10 g/dl or the haematocrit below 0.30 [1]. This value was based on the physiological knowledge at that time and may have been appropriate. However, our understanding of human physiology, oxygen delivery and the safety and risks of allogenic transfusion has changed considerably. The transfusion trigger of 10 g/dl is still widely followed [8, 23]. In 1988, the National Institute of Health Consensus Development Conference recommended that a lower level of haemoglobin (8 g/dl) should act as a trigger for transfusion. It was also suggested that decisions about transfusions should be based on an assessment of clinical needs and symptoms rather than laboratory values alone [17]. The British Transfusion Task Force recommends that elderly patients can be allowed haemoglobin levels as low as 8.0 g/dl and younger patients as low as 7.0 g/dl before blood transfusion is required [3].
The quality of the drainage blood was studied with respect to the content of extracellular bioactive substances and coagulation split products by Jensen et al. [11] using the HandyVac ATS auto transfusion system. Drainage blood was collected and reinfused within six hours postoperatively from ten patients undergoing primary total knee arthroplasty. Blood samples were collected from the patients immediately after and one hour after release of the tourniquet and after reinfusion of drainage blood. Samples were also collected from the drainage blood immediately before and at the end of reinfusion. The leucocyte-derived and platelet-derived bioactive substances histamine, eosinophil cationic protein (ECP), eosinophil protein X (EPX), myeloperoxidase (MPO), plasminogen activator inhibitor type 1 (PAI-1) and activated complement factor C3(C3a) and various coagulation factors and split products were analysed in patient and drainage blood samples. None of the patients received additional predonated autologous blood or allogeneic blood components during the study period. Within six hours postoperatively, 250 to 1,000 ml drainage blood was collected and reinfused. Histamine, ECP, EPX, MPO, PAI-1 and C3 content was significantly increased in drainage blood immediately before and at the end of reinfusion. Reinfusion did not change the concentration of these substances in samples from the patients. Coagulation factors and various split products showed that drainage blood was defibrinated. Reinfusion of drainage blood did not change the coagulative capacity of the patients. Drainage blood appeared to be defibrinated and contained various extracellular leucocyte-derived and platelet-derived bioactive substances. Reinfusion did not change the coagulative capacity or the concentration of bioactive substances of patients.
Some reports from North America have questioned the requirement for postoperative reinfusion after unilateral total knee arthroplasty. Slagis et al. [20] felt that the cost was not justified, but they routinely used a cell washer, which was expensive. Marks et al. [13] found that postoperative reinfusion was ineffective, but they combined it with the preoperative collection of blood, and it is doubtful if both systems need to be used on the same patient.
Recent studies have shown that the salvage of blood after an operation and reinfusion can reduce the need for homologous blood transfusion and its risk. Kristensen et al. [12] published a study in 1993 of 56 patients undergoing hip or knee replacements who were randomised to receive autologous drain-blood transfusion or homologous blood transfusion according to postoperative need. The number of homologous blood transfusions fell concomitantly from 3.3 to 0.3 after knee replacement. No signs of activation of the complement or coagulation systems were found. In 1994, Rosencher et al. [18] published a study that aimed to compare two systems, Orth-Evac and Solcotrans Plus, and to assess the safety of the reinfusion of non-washed blood cells.
It included 30 patients scheduled for total knee replacement surgery who were allocated randomly into three groups of ten each: the Orth-Evac group (OGr), the Solcotrans Plus group (SGr) and the control group (CGr). Transfusion of homologous blood was required in two patients of the Orth-Evac group, four of the Solcotrans group and six of the control group. Healy et al. [9] made a prospective randomised study on 128 patients who were studied after hip replacement, knee replacement or spine fusion. The efficacy of autologous shed blood in reducing homologous transfusion was evaluated. The reinfusion of shed blood reduced the requirement for homologous blood by 60%.
Xenakis et al. [26] in 1997 performed a prospective study to determine the effect of the postoperative collection and reinfusion of unwashed, filtered, salvaged blood alone and in combination with preoperative predeposited blood on the transfusion requirements of 375 patients treated with a total hip or total knee replacement. Two hundred and eight patients were managed with postoperative blood salvage with the use of the CBC ConstaVac autotransfusion system and closed suction drainage. Another 50 patients predeposited 1–4 units of autologous blood before the operation in addition to postoperative blood salvage. The remaining 117 patients were used as controls and were transfused with homologous blood from the blood bank. Postoperative reinfusion of salvaged blood decreased the need for homologous transfusion after hip and knee arthroplasty (mean 2.7 units) compared to controls (mean 4.2 units). The combination of postoperative reinfusion of salvaged blood and predeposited autologous blood was associated with the lowest requirements for homologous blood transfusions (mean: 1.7 units).
Strumper et al. [22] in a study performed on 135 patients receiving transfusion of filtered shed blood after total knee arthroplasty determined that the number of patients receiving autologous blood transfusions was reduced overall from 35 percent (controls) to 22 percent (study). The decrease of the allogeneic transfusion requirement was most significant after total knee arthroplasty from 18 to 6 percent (P<0.001). Sinha et al. [19] in a study published in 2001 reported that for 50 patients receiving reinfusion of drained blood after total knee arthtroplasty, the homologous blood requirement was reduced by 80%. The use of unwashed salvaged blood after total knee arthroplasty seems to shorten the hospital stay and effectively reduces postoperative requirements for autologous blood transfusion, as has been proved by most recent studies [14, 15, 21].
Salvage of unwashed blood after total knee arthroplasty and reinfusion not only reduces the need for autologous blood transfusion, but also reduces the cost as it is an inexpensive method. In our study the total cost of the transfusions (auto- and homologous) in group A (the study group) was 5,247 € (mean: 174.90 €/patient and in group B was 8,235 € (mean: 274.50 €/patient. The transfusion cost was decreased in the study group by 36%. The exact costs of transfusion are hard to quantify. The cost from region to region can vary in the United Kingdom from £50 to £200 per unit. There are also hidden costs such as increased patient stay (about £300 per day) and treatment for complications. Therefore, it can be seen that if one unit of blood less per patient was transfused and the length of stay was reduced by 1 day, a department that performs 400 arthroplasties of the lower limbs each year can save approximately £150,000 per annum.
Conclusion
Our study has proved that the use of an unwashed autologous blood reinfusion system postoperatively reduces highly effectively the demands of homologous banked blood transfusions, the number of patients who require homologous blood transfusions and the cost of blood management after total knee replacement. We therefore strongly recommend that unwashed blood salvage reinfusion should be used postoperatively after total knee arthroplasty as most of the recent studies suggest that there are clinical and economical advantages in avoiding the use of autologous blood.
References
- 1.Adams RC, Lundy JS (1942) Anaesthesia in cases of poor surgical risk: some suggestions for decreasing the risk. Surg Gynaecol Obstet 74:1011–1019
- 2.Bierbaum BE, Callaghan JJ, Galante JO et al (1999) An analysis of blood management in patients having total hip or knee arthroplasty. J Bone Joint Surg 81-A:2–10 [DOI] [PubMed]
- 3.British Committee for Standards in Hematology (2001) Blood Transfusion Task Force. Guidelines for the clinical use of red cell transfusions. Br J Haematol 113:24–31 [DOI] [PubMed]
- 4.Clements DH, Sulco TP, Burke SW, Mayer K, Levine DB (1991) Salvage and reinfusion of postoperative sanguinous wound drainage. J Bone Joint Surg 74:646–651 [PubMed]
- 5.Dodd RY (1992) The risk of transfusion transmitted infection. N Engl J Med 327:419–421 [DOI] [PubMed]
- 6.Faris PM, Ritter MA, Keating EM, Valeri CR (1991) Unwashed filtered shed blood collected after knee and hip arthroplasties. J Bone Joint Surg 73:1169–1178 [PubMed]
- 7.Fernandez MC, Gottlieb M, Menitove JE (1992) Blood transfusion and postoperative infection in orthopaedic patients. Transfusion 32:318–322 [DOI] [PubMed]
- 8.Garrioch M, Sandbach J, Mcllvenny S (1997) Current transfusion practice in three large British teaching hospitals. Br J Anaesth 82:A266
- 9.Healy WL, Pfeifer BA, Kurtz SR, Johnson C, Johnson W, Johnston R, Sanders D, Karpman R, Hallack GN, Valeri CR (1994) Evaluation of autologous shed blood for autotransfusion after orthopaedic surgery. Clin Orthop Relat Res (299):53–59, Feb [PubMed]
- 10.Howard HL, Rushabuzla FG, Martlew VJ, Satchi G, Bolton-Maggs B (1993) Clinical benefits of autologous blood transfusion: an objective assessment. Clin Lab Haemat 15:165–171
- 11.Jensen CM, Pilegaard R, Hviid K, Nielsen JD, Nielsen HJ (1999) Quality of reinfused drainage blood after total knee arthroplasty. J Arthroplasty 14(3):312–318, Apr [DOI] [PubMed]
- 12.Kristensen PW, Sorensen LS, Thyregod HC (1993)Autologous transfusion of drained blood in hip and knee alloplasty. A prospective controlled study of 56 patients. Ugeskr Laeger 155(18):1382–1386, May 3 [PubMed]
- 13.Marks RM, Vaccaro AR, Balderston RA et al (1995) Postoperative blood salvage in total knee arthroplasty using the solcotrans autotransfusion system. J Arthroplasty 10:433–437 [DOI] [PubMed]
- 14.Mont MA, Low K, LaPorte DM, Hostin E, Jones LC, Hungerford DS (2000) Reinfusion drains after primary total hip and total knee arthroplasty. J South Orthop Assoc 9(3):193–201, Fall [PubMed]
- 15.Munoz M, Ariza D, Garceran MJ, Gomez A, Campos A (2005) Benefits of postoperative shed blood reinfusion in patients undergoing unilateral total knee replacement. Arch Orthop Trauma Surg Apr 9 [DOI] [PubMed]
- 16.Murphy P, Heal JM, Blumberg N (1991) Infection or suspected infection after hip replacement surgery with autologous or homologous blood transfusions. Transfusion 31:212–217 [DOI] [PubMed]
- 17.NIH (1989) Summary of NIH Consensus Development Conference on Perioperative Red Cell Transfusion. Am J Haematol 31:144 [DOI] [PubMed]
- 18.Rosencher N, Vassilieff V, Tallet F, Toulon P, Leoni J, Tomeno B, Conseiller C (1994) Comparison of Orth-Evac and Solcotrans Plus devices for the autotransfusion of blood drained after total knee joint arthroplasty. Ann Fr Anesth Reanim 13(3):318–325 [DOI] [PubMed]
- 19.Sinha A, Sinha M, Burgert S (2001) Reinfusion of drained blood as an alternative to homologous blood transfusion after total knee replacement. Int Orthop 25(4):257–259 [DOI] [PMC free article] [PubMed]
- 20.Slagis SV, Benjamin JB, Volz RG, Giordano GF (1991) Postoperative blood salvage in total hip and knee arthroplasty: a randomized controlled study. J Bone Joint Surg 73:591–594 [DOI] [PubMed]
- 21.Steinberg EL, Ben-Galim P, Yaniv Y, Dekel S, Menahem A (2004) Comparative analysis of the benefits of autotransfusion of blood by a shed blood collector after total knee replacement. Arch Orthop Trauma Surg 124(2):114–118, Epub 2004 Jan 27, Mar [DOI] [PubMed]
- 22.Strumper D, Weber EW, Gielen-Wijffels S, Van Drumpt R, Bulstra S, Slappendel R, Durieux ME, Marcus MA (2004) Clinical efficacy of postoperative autologous transfusion of filtered shed blood in hip and knee arthroplasty. Transfusion 44(11):1567–1571 [DOI] [PubMed]
- 23.Sudhindram S (1997) Perioperative blood transfusion: a plea for guidelines. Ann R Coll Surg Engl 79:299–302 [PMC free article] [PubMed]
- 24.Triulzi DJ, Vanek K, Ryan DH, Blumberg N (1992) A clinical and immunologic study of blood transfusion and postoperative bacterial infection in spinal surgery. Transfusion 32:517–524 [DOI] [PubMed]
- 25.Waymack JP, Yurt RW (1990) Effect of blood transfusions on immune function. The effect on the inflammatory response. J Surg Res 48:147–153 [DOI] [PubMed]
- 26.Xenakis TA, Malizos KN, Dailiana Z, Koukoubis T, Zervou E, Golegou C, Soucacos PN (1997) Blood salvage after total hip and total knee arthroplasty. Acta Orthop Scand [Suppl] 275:135–138, Oct [DOI] [PubMed]
- 27.Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM et al (2003) Orthopedic Surgery Transfusion Haemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion 43:459–469 [DOI] [PubMed]
- 28.Sehat KR, Evans R, Newman JH (2000) How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee 7:151–155 [DOI] [PubMed]
- 29.Amin M, Ferguson D, Azizi A, Wilson K, Coyle D, Hebert P (2003) The cost of allogenic red blood cells-a systematic review. Transf Med 13:275–285 [DOI] [PubMed]
- 30.Spahn DR, Casutt M (2000) Eliminating blood transfusions. Anaesthesiology 93:242–255 [DOI] [PubMed]