Abstract
Seventy-four total hip arthroplasties using a cementless acetabular component without holes for supplemental screw fixation were evaluated during a follow-up period of 2–6 years. Immediate full weight-bearing walking was allowed after the operation. A comparison of anteroposterior (AP) radiographs of the pelvis taken in the early postoperative period and when the patient returned for the final follow-up revealed that there was no migration of the acetabular component. Based on the early postoperative radiographs and using the zones described by Martell et al. [J Bone Joint Surg (1993) 75-A:554–571], gaps between the acetabular component and the bone occurred at zone A2 in three hips (4.1%), at zone B1 in 12 hips (16.2%), and at zone B2 in seven hips (9.5%). The final follow-up radiographs, however, revealed only one hip to have a gap of 1.1 mm at zone B2; the majority of the gaps had disappeared. The results suggest that immediate weight-bearing walking did not result in the migration of the cementless acetabular component.
Résumé
74 prothèses totales de hanche utilisant une cupule sans ciment avec vis additionnelles ont été évaluées après un suivi de 2 à 6 ans. Les patients ont été mis en charge immédiatement après l’intervention. Des radiographies de face, réalisées en post opératoire immédiat et au dernier suivi ont été réalisées pour cette étude. Nous n’avons constaté aucune migration de la cupule. Nous avons constaté en utilisant la classification de Martell et al. (1993) que de petits liserés entre la cupule et l’os présents en zone A2 dans 3 hanches (4.1%), en zone B1 dans 12 hanches (16.2%) et en zone B2 7 hanches (9.5%), sur les radiographies post opératoires immédiates ont disparu pour la grande majorité d’entre eux au recul final. Seule une hanche a montré 1 liseré résiduel de 1.1 mm en Zone B2. Ces résultats nous indiquent que la mise en charge immédiate, après la mise en place d’une cupule non cimentée avec vis additionnelles n’entraîne pas de migration du composant acétabulaire.
Introduction
The application of cementless acetabular components in primary total hip arthroplasty (THA) has gained widespread popularity by showing reliable intermediate and long-term results in the follow-up [1, 8]. However, two aspects of the technique are controversial. The first is whether supplemental screw fixation is needed. An acetabular component with a screw hole may be used but, on the other hand, a screw need not be inserted at all [7]; alternatively, an acetabular component without a screw hole may be used. The second aspect is whether immediate full weight-bearing walking is possible after the total hip replacement.
The purpose of this study was to evaluate the insertion of a cementless acetabular component without holes for supplemental screw fixation to determine any loss of fixation if full weight-bearing walking were to be allowed after the operation.
Patients and methods
The Duraloc 100 Polished HA acetabular component (Depuy, Johnson and Johnson) (Fig. 1) has hydroxyapatite plasma sprayed onto the porous coating to accelerate bone ingrowth and promote stronger bone interlock. There is no screw hole and no stabilising spike or peg; the acetabular component is inserted with a press-fit technique. The apex hole is plugged and thus completely occludes the acetabular fixation interface from the polyethylene wear debris.
Fig. 1.
The Duraloc 100 Polished HA acetabular component has hydroxyapatite plasma sprayed onto the porous coating. There is no screw hole and no stabilising spike or peg. The apex hole can be plugged to occlude access of polyethylene wear debris into the acetabular fixation interface
The same surgical routine was used in every patient in the series. The patient was put in a lateral position, and the hip was approached posteriorly. The acetabulum was prepared with even-diameter reamers until all of the cartilage had been removed and healthy bleeding bone was exposed. A trial component of the same size as the last reamer was then impacted into the acetabular component. The coverage and contact with the host bone was inspected, and the stability of the trial component was checked by wobbling the shell holder. If the surgeon was satisfied, he would decide on the size of the prosthesis. To achieve press fit stability, a prosthesis 2 mm larger than the trial component was used. Depending on the bone quality, the surgeon might do a final touching up with an odd-diameter reamer that was 1 mm larger than the trial component but 1 mm smaller than the prosthesis. Good stability of the trial component was considered to be extremely important. If the stability was suboptimal, the acetabulum was enlarged or deepened with further reaming, and then the appropriate trial component was re-inserted. If its stability was still doubtful, the surgeon might choose a cementless acetabular component with holes for supplemental screw fixation. If the trial component was still unstable after these various approaches had been attempted, the surgeon should consider changing plan and using a reinforcement ring or even a cemented acetabular component. We allowed all patients to bear full weight on walking after the surgery.
In the study, we reviewed the radiographic outcomes of Duraloc 100 Polished HA acetabular components (95 hips in 82 patients) that were inserted using the press-fit technique. There were 43 men and 39 women in the study cohort, with an average age at the time of the surgery of 53.4 years [standard deviation (SD): 12.8; range: 24 to 74]. The THA was performed on the left side in 55 hips and on the right side in 40 hips. The indications for surgery were avascular necrosis in 47 hips (alcoholic in 21, steroid-induced in 12, idiopathic in 11, post-traumatic in three), osteoarthritis in 16 hips (primary in 14, secondary to trauma in one, secondary to old Perthes disease in one), ankylosing spondylitis in nine hips, developmental dysplasia in seven hips, rheumatoid arthritis in six hips, post-trauma in five hips (failed internal fixation for proximal femoral fracture in one, failed hemiarthroplasty for femoral neck fractures in three, neglected femoral neck fractures in one), epiphyseal dysplasias in four hips, and old hip tuberculosis in one hip. The available sizes ranged from 48 to 66 mm with 2-mm increments. The femoral components were cemented in 72 hips (69 Elite plus, Depuy, Johnson and Johnson; three Option 3000, Mathys, Switzerland) and cementless in 23 hips (17 Replica A, Depuy, Johnson and Johnson; six Summit, Depuy, Johnson and Johnson).
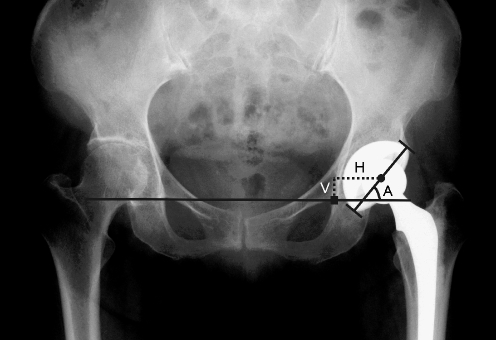
The anteroposterior (AP) radiographs of the pelvis taken in the early postoperative period and when the patient returned for the final follow-up were scanned using VXR-12 plus film digitiser (VIDAR, Denmark). The digital images were stored into the computer for subsequent measurements using the software OSIRIS (Windows ver. 4.17; University Hospital of Geneva, Switzerland). The known hip ball diameter was used to correct for radiographic magnification. The lateral opening or abduction angle of the acetabular component was measured (Fig. 2) and determined to be the angle subtended by a horizontal line touching the lowest points of the two tear drops and a line joining the superolateral and infeomedial corners of the acetabular component. The mid point of the latter line was identified, and its horizontal and vertical distances from the lowest point of the corresponding teardrop were measured (Fig. 2). Migration of the acetabular component was defined as a change in the lateral opening angle of more than 8° or a difference in the component position of over 3 mm [6] based on a comparison of serial radiographs. The prosthesis-bone interface was divided into five zones [5], which is a modification of the three zones that DeLee and Charnley [3] used to describe different extents of the radiolucent lines. The lateral one-third zone of DeLee and Charnely was divided into two equal parts, A1 and A2, while their superomedial quadrant was divided into two equal parts, B1 and B2. The inferomedial part was denoted as C. The presence of a gap was detected in the early postoperative radiographs. Radiolucent lines were present if they could be seen on the follow-up radiographs in areas in which no gaps had existed initially. The zone in which the gap or radiolucent line occurred was recorded, as was the width of the gap/line.
Fig. 2.
The lateral opening angle (A) of the acetabular component was subtended by a horizontal line touching the lowest points of the two tear drops and a line joining the superolateral and infeomedial corners of the acetabular component. The mid point of the latter line was identified, and its horizontal (H) and vertical (V) distances from the lowest point of the corresponding teardrop were measured
Results
Four patients (four hips) died of unrelated causes, Seven patients (eight hips) defaulted follow-up, and nine hips in eight patients were excluded because of incomplete radiographic documentation. Consequently a total of 74 hips (60 patients) had full radiographic documentation and were followed up for an average of 3.4 years (SD: 1.0; range: 2–6.2).
The lateral opening angle averaged 47.3° in the early postoperative radiographs (SD: 7.2; range: 27–70) and 47.7° (SD: 7.2; range: 29–70) in the final follow-up radiographs. The change in the lateral abduction angle averaged 0.4° (SD: 1.7; range: 3–5). No acetabular component changed its lateral opening angle by more than 8°.
With respect to the positions of the acetabular components, the vertical distance increased by an average of 0.1 mm (SD: 1.3; range: −3.0–2.8), and the horizontal distance decreased by an average of 0.1 mm (SD: 1.3; range: −3.0–3.0). No acetabular component changed its horizontal or vertical position by more than 3 mm.
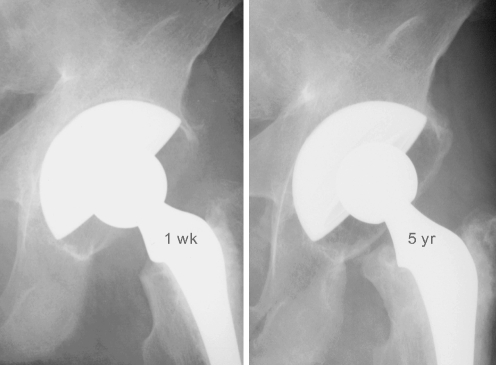
The early post-operative radiographs revealed gaps between the acetabular component and the bone at zone A2 in three hips (4.1%), zone B1 in 12 hips (16.2%), and zone B2 in seven hips (9.5%); there were no gaps at zones A1 and C. In contrast, the final follow-up radiographs revealed only one hip with a gap of 1.1 mm at zone B2; there were no gap at zones A1, A2, B2, and C. The only hip with a gap at zone B2 in the final follow-up radiograph had gaps of 1.3 mm at zone B1 and B2 in the early postoperative radiograph (Fig. 3). The majority of the gaps that appeared in the early postoperative radiographs disappeared during the follow-up (Fig. 4). A radiolucent line was not present in the vicinity of the acetabular component in any of the hips, as determined on the postoperative radiograph.
Fig. 3.
A 65-year-old patient had left THA for developmental dysplasia of the hip. Gaps (1.3 mm in thickness) were present at zones B1 and B2 in the postoperative radiograph (1 week; left); the 3-year postoperative radiograph revealed a gap (1.1 mm in thickness) at zone B2 (right). There was no change in the lateral opening angle and the horizontal and vertical positions of the acetabular component
Fig. 4.
A 30-year-old male patient had left THA for ankylosing spondylitis. Gaps (0.5 mm in thickness) were present at zones A2 and B1 in the first postoperative radiograph (1 week; (left); In the 5-year postoperative radiograph, the gaps were invisible (right)
Discussion
Press-fit implantation of porous-coated acetabular components without screws has several advantages [7]. Firstly, it avoids supplemental screw fixation and eliminates the risks of vascular injury, which can be devastating. Secondly, the avoidance of screw insertion shortens the operative time. Thirdly, the possibility of fretting wear between the screw and metal shell is also eliminated, thereby also reducing the backside wear causing pelvic osteolysis. However, in selected cases with insufficient host bone support and soft host bone, supplemental screws are indicated, even with these disadvantages.
A literature search revealed that the mandatory use – or not – of supplemental screws is open to controversy. Weber et al. reported that there was no correlation between additional screw and osteolysis necessitating revision [9]. Clohisy and Harris reported the average 1-year results for patients who had the Harris-Galante porous-coated acetabular component (Zimmer, Warsaw, Indiana) with screws [2]; in their study, osteolysis was identified in 5% of the cases. Udomkiat et al. reported the average 10-year results for patients who had received anatomic porous replacement with a hemispheric porous-coated metal shell (APR; Sulzer Orthopaedics, Austin, Texas) without screws [7]. These researchers found that 34% of the patients had a gap around the socket which gradually disappeared in the subsequent radiographs, while pelvic osteolysis was identified in 4% of cases, a percentage comparable that reported by Clohisy and Harris [2]. Engh et al. compared acetabular components with spikes, components inserted with screws, and components inserted with press-fit technique without screws [4] and ultimately obtained similar outcomes with all three approaches.
The surgical approach adopted in our study involved the use of the Duraloc 100 cup, which has no screw hole and the central apical hole can be plugged so that the pelvic bone can be completely sealed off from the particulate debris. During surgery, the choice of acetabular component with or without screw holes must be made after the insertion of the trial component. The stability of the trial component dictates the choice of acetabular components. In our experience, the press-fit technique is feasible in most cases. We believe that the supplemental screws and thus the acetabular component with screw holes are only indicated in selected cases with insufficient rim support and soft bones.
The postoperative rehabilitation regime is also disputed after cementless total hip arthroplasty. Because of the potential risk that motion will affect the bone ingrowth, full weight-bearing walking is always deferred. In this study, immediate weight-bearing walking following the implantation of the cementless acetabular component did not result in migration of the acetabular component. All of the patients reported here had a stable and well-fixed acetabular component at the last follow-up.
References
- 1.Claus AM, Sychterz CJ, Hopper RH Jr, Engh CA (2001) Pattern of osteolysis around two different cementless metal-backed cups: retrospective, radiographic analysis at minimum 10-year follow-up. J Arthroplasty 16[Suppl 1]:177–182 [DOI] [PubMed]
- 2.Clohisy JC, Harris WH (1999) The Harris-Galante porous-coated acetabular component with screw fixation. An average ten-year follow-up study. J Bone Joint Surg 81-A:66–73 [DOI] [PubMed]
- 3.DeLee JG, Charnley J (1976 ) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 121:20–32 [PubMed]
- 4.Engh CA, Hopper RH Jr, Engh CA Jr (2004) Long term porous coated cup survivorship using spikes, screws and press-fitting for initial fixation. J Arthroplasty 19[Suppl 2]:54–60 [DOI] [PubMed]
- 5.Martell JM, Pierson III RH, Jacobs JJ, Rosenberg AG, Maley M, Galante JO (1993) Primary total hip reconstruction with a titanium fiber-coated prosthesis inserted without cement. J Bone Joint Surg 75-A:554–571 [DOI] [PubMed]
- 6.Massin P, Schmidt EA, Engh CA (1989) Evaluation of cementless acetabular component migration. an experimental study. J Arthroplasty 4:245–251 [DOI] [PubMed]
- 7.Udomkiat P, Dorr LD, Wan Z (2002) Cementless hemispheric porous-coated sockets implanted with press-fit technique without screws; average ten-year follow-up. J Bone Joint Surg 84-A:1195–A:1200 [DOI] [PubMed]
- 8.Valle AGD, Zoppi A, Peterson M, Salvati (2004) Clinical and radiological results associated with a modern cementless modular cup design in total hip arthroplasty. J Bone Joint Surg 86-A:1998–A:2004 [DOI] [PubMed]
- 9.Weber D, Schaper LA, Pomeroy DL, Badenhausen Jr WE, Curry JI, Smith MW, Suthers KE (2000) Cementless hemispheric acetabular component in total hip replacement. Int Orthop 24:130–133 [DOI] [PMC free article] [PubMed]