Abstract
We report the results of impaction bone grafting of the femoral side in revision total hip arthroplasty in Asian hips (South Korean patients) in which the surgery was performed with the use of the Exeter stem. The minimum follow-up was 39 months (mean, 48.4; range, 39–66). There was subsidence of the cement-graft interface (<1 mm) in three hips (5%), of the stem-cement interface (<1 mm) in 12 hips (21%) and of the stem-cement interface (1–2 mm) in 14 hips (25%). Five hips (9%) developed intraoperative femoral fracture and two hips (4%) femoral perforation in revision. The complications of femoral fracture and subsidence did not have an adverse effect on the final clinical outcomes. The impaction of fresh-frozen allograft and use of a cemented, polished, tapered stem (Exeter stem) were also successful with good clinical and radiographic outcomes in our study of Asian hips (South Korean patients). However, we used smaller stems than the usual ones used for Western patients because of the smaller femur sizes.
Résumé
Nous reportons les résultats de la technique d’Exeter avec greffons impactés dans les reprises totales de hanche, étude réalisée sur des hanches asiatiques et sur des patients sud coréens, avec utilisation de la tige d’Exeter. Le suivi minimum a été de 39 mois (48.4 à 39.66). La migration à l’interface ciment greffe a été inférieure à 1 mm dans 3 cas, 5%. A l’interface tige ciment, (<1 mm) dans 12 hanches (21% des cas) et enfin à l’interface tige ciment, cette migration est comprise entre 1 et 2 mm dans 14 hanches (25% des cas). 5 hanches (11%) ont présenté durant l’intervention des complications avec une fracture fémorale dans 5 cas (9%) et une perforation fémorale dans 2 cas (4%). Ces complications ainsi que la migration de la tige n’ont pas entraîné de problèmes cliniques. La technique utilisant des allogreffes compactées cryoconservées et l’utilisation d’une tige cimentée et polie de type Exeter ont donné, dans cette étude, de bons résultats, tant sur le plan clinique que sur le plan radiographique. Cependant, nous avons dû utiliser des tiges beaucoup plus petites qu’habituellement en Europe compte tenu de la petite taille des fémurs asiatiques sud coréens.
Introduction
Among the many methods of reconstruction for dealing with femoral components in the setting of the loss of proximal bone stock, impaction bone grafting has the advantage of having the potential to achieve the stability of an implant with the use of a compacted, morselized bone graft. It subsequently allows the incorporation and remodeling of living bone stock in the host skeleton. Based on the original reports [9], a number of authors have published favorable results [7, 13, 18, 24, 25], though others have reported serious problems [3, 15, 16, 20]. Furthermore, the technique used with the Exeter stem has evolved since it was first reported in the original series [9, 21]. However, so far there are no published reports about impaction bone grafting with cement used with the Exeter stem in Asian hips.
We present the clinical results of the first 56 hips that underwent impaction cancellous allograft into the proximal aspect of the femoral canal for a component inserted with cement within a minimum of 39 months of follow-up in South Korean patients.
Materials and methods
Patients
From March 1998 to March 2003, we performed 56 consecutive femoral revisions in 43 South Korean patients. The mean age of 42 women and 14 men at the time of the surgery was 63 years (53 to 77). The average height of the patients was 157 cm (150 to 176); the average weight was 56 kg (48 to 82) at the time of the surgery. They were followed up for a minimum of 39 months (mean, 48.4; range, 39–66). The indication for the revision of the femoral component was aseptic loosening in 55 hips and septic loosening in one, with severe bone loss in all patients. This was the first revision procedure. One hip with septic loosening was treated with a two-stage procedure, with systemic antibiotics appropriate to the infecting organism administered for at least 6 weeks until the serum C-reactive protein level normalized prior to reimplantation. The original diagnoses were osteoarthritis secondary to osteonecrosis (30 hips), primary osteoarthritis (17 hips), hip dyplasia (4), femoral neck fracture treated by hemiarthroplasty (2), secondary osteoarthritis to childhood tuberculous arthritis (2) and miscellaneous causes (1).
Surgical technique
One surgeon (S.J.Y) performed all the operations using the technique described by Gie et al. [9]. A posterolateral approach with or without a trochanteric osteotomy was used in all hips. Prior to impaction cancellous bone grafting, the femur was reinforced with cerclage cables in 33 hips, metal mesh in 11 hips and a metal plate in 1 hip. Fresh-frozen femoral head allografts were obtained from LifeLink tissue Bank (Tampa, FL), where they had been deep frozen at −70°C after being irradiated with 2.5 megarads. The bank is accredited by the American Association of Tissue Banks [6]. After thawing in a warm (50–60°C) saline solution for approximately 20 min, the articular cartilage was removed and fresh-frozen femoral heads were milled with the use of a bone mill (Tracer Designs Inc., Santa Paula, CA). This mill was used to produce bone chips of approximately 3 mm in size. The bone chips were used to unrinse.
We used a standard collarless double-tapered and polished Exeter stem with the use of the X-change Revision Instruments System (Howmedica International, Ltd., London) in all hips. Impacting allografting and trial reduction were then achieved; the trial stem was withdrawn and Simplex bone cement (Howmedica international Ltd, Rutherford, NJ) with antibiotics in low viscosity was then injected into the neomedullary canal in a retrograde fashion. After pressurization of the cement, a standard Exeter stem with a centralizer on the tip was inserted.
Postoperatively, intravenous antibiotics (three dose of 1 g of cefazolin for 3 days and two doses of 0.25 g of Amikacin for 1 day) and subcutaneous low-molecular-weight heparin for 14 days were given for prophylaxis against infection and thrombosis, respectively. Almost all patients were allowed to sit up by leaning on the bed within 2–4 postoperative days, and to walk with two crutches for 3 months. Weight bearing was restricted for the first 6 weeks, followed by a gradual increase in weight bearing.
Clinical and radiographic examinations were performed preoperatively, at 6 weeks, 3 months, 6 months and 1 year after surgery, and yearly thereafter.
Clinical follow-up
The Charnley modification of the Merle d’Aubigné-Postel classification [1, 17] was used to evaluate pain, function and movement (scoring 1–6 points, with 6 being the best) in all patients. Patients had Charnley category A (unilateral hip disease; 20 hips), Charnley category B (bilateral hip disease; 28 hips) and Charnley category C (hip disease and concomitant disease such as rheumatoid arthritis, hemiplegia and cardiovascular or respiratory disability; 8 hips).
Radiographic follow-up
The radiographic analyses were carried out as a protocol by three orthopedic surgeons (S.J.Y., M.Y.K. and Y.S.S.) in consensus preoperatively, postoperatively and at the follow-ups.
On preoperative radiographs, the deficiency of the bone stock was graded radiologically according to the Endo-klinik classification [5]. In the present study, 24 hips were grade II, 28 hips were grade III, and 4 hips were grade IV.
On postoperative radiographs, anteroposterior and lateral radiographs were reviewed to determine the migration of the stem, the incorporation of the graft and the presence of radiolucent lines through the use of digitized X-rays and the Orthochart system.
In the present study, radiostereometric analysis (RSA) was not available, so the accurate measurement of migration of the stem and the finding the exact location was difficult [14]. However, the geometry of the stem was suitable for the reasonably accurate assessment of subsidence of the stem cement and cement-graft as described by Fowler et al. [8], and it was possible to measure the subsidence of the stem cement and cement-graft accurately. The radiolucent line between the cement and the bone was scored with the use of the classification system of Gruen et al. [12]. Any resorption in relation to the wire or cables was not included in the grading of the classification system of Gruen et al. [12]. The incorporation and trabecular bone formation in the grafts were evaluated with the use of the criteria of Gie et al. [9].
Statistical analysis
The statistical analysis was performed using the statistical computer software SPSS 11.0 (SPSS Inc, Chicago, IL). For estimating the comparison of clinical outcomes, the Wilcoxon matched pairs signed rank sum test was used. P-values below 0.05 were considered significant.
Results
Clinical results
The Charnley modification of the Merle d’Aubigné-Postel scoring for pain, function and movement was improved at the final follow-up in all patients (Table 1). In Charnley categories A and B, the pain, function and movement scores were improved significantly at the final follow-up (P<0.05, respectively). In Charnley category C, the pain, function and movement scores were improved at the final follow-up. However, there were no significant differences between the preoperative and the final follow-up scores (P=0.17). Eight patients with Charnley category A and seven patients with Charnley category B had no pain (scoring for pain, 6), respectively.
Table 1.
Comparison between the preoperative and postoperative Charnley scores for patients who underwent femoral impaction grafting in revision hip arthroplasty
| Charnley score | Pain | Function | Movement | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Preop | Postop | P-value | Preop | Postop | P-value | Preop | Postop | P-value | |
| A | 1.0 | 5.8 | 0.02 | 1.7 | 5.5 | 0.03 | 1.8 | 5.2 | 0.02 |
| B | 1.5 | 5.9 | 0.01 | 1.8 | 5.5 | 0.01 | 1.4 | 5.3 | 0.01 |
| C | 0.5 | 5.0 | 0.18 | 0.5 | 5.5 | 0.16 | 1.0 | 5.0 | 0.16 |
| Mean score | 1 | 5.5 | 1.3 | 5.5 | 1.4 | 5.2 | |||
Radiographic results
The immediate postoperative anteroposterior radiographs showed the stem inserting at a neutral position in 48 hips (86%; 48/56). Five hips were in a varus position. Cortical repair and trabecular incorporation were seen in all hips at a mean of 5.8 months, and trabecular remodeling in 38 hips (68%; 38/56) at a mean of 21.7 months (Table 2). The cement mantle was complete in 54 hips (>2 mm), except in two hips (<2 mm). The radiolucent line at the cement-stem interface was in Gruen zone I in three hips (5%; 3/56). The line was not progressive during the follow-up.
Table 2.
Radiographic findings of the graft-host bone reaction in patients who underwent femoral impaction grafting in revision hip arthroplasty
| Radiographic findings of the graft host bone reaction | Number (% of group) |
|---|---|
| No change | 0 (0) |
| Localized resorption | 0 (0) |
| Cortical repair | 56 (100) |
| Trabecular remodeling | 38 (68) |
| Trabecular union | 56 (100) |
| Cortical repair and trabecular remodeling | 38 (68) |
| Cortical repair and trabecular union | 56 (100) |
Subsidence of the cement-graft interface (<1 mm) occurred in three hips (5%, 3/56) and was not progressive at the final follow-up; it was not seen in the remaining hips at the final follow-up. Subsidence of the stem-cement interface (<1 mm) occurred in 12 hips (21%; 21/56), and subsidence of the stem-cement (1–2 mm) in 14 hips (25%; 14/56) that were seen at the final follow-up. Most subsidence was seen within the first 2 years after the operation.
Complications
There were five intraoperative fractures of the proximal femur (9%; 5/56) and two perforations of the femora by the tip of the stem (4%; 2/56). All proximal fractures were discovered during surgery, two during the removal of the cement before impaction bone grafting and three during the impaction of the allograft. Proximal fractures were stabilized with cerclage cables (four hips) or additional structural allografts (one hip). Two perforations of the femora were covered with mesh fixed with cerclage cables and a plate.
At a minimum of 39 months of follow-up, none of the stems had been re-revised, and none of the hips had infection.
Discussion
Impacted allograft has been used for more than 20 years to fill defects created by the loosening process at the time of revision hip surgery. Femoral impaction allografting with cement was first reported using the Exeter stem [9]. This stem design includes a double-tapered geometry, the absence of a collar and a highly-polished stem surface. The advocates of this stem design in revision with impacted allograft have suggested that the design permits gradual subsidence of the implant within the cement mantle because of plastic deformation of the cement and even viscoelastic deformation of the graft [10]. This leads to a self-tightening that allows restabilization within the cement [4, 9] and provides a beneficial compressive load to the allograft [19]. However, other authors question whether subsidence of a polished stem can be beneficial or if relatively high subsidence of a stem can lead to clinical failures [3, 15, 16]. In the present study, subsidence of the cement-graft interface (<1 mm) occurred in three hips (5%; 3/56), subsidence of the stem-cement interface (<1 mm) in 12 hips (21%; 21/56) and subsidence of the stem-cement (1–2 mm) in 14 hips (25%; 14/56). These findings are in agreement with the results reported by Orstein et al. [21]; migration of the Exeter stem at the stem-cement interface was found in primary hip arthroplasties and in revisions with impacted allografts, and additional migration was observed at the cement-graft interface in revisions. In most of our cases, we could not find a relationship between the observed subsidence and the clinical outcomes as was reported in other studies [13, 18] (Table 3). Most of the subsided stems had been inserted during the first 2 years and subsided below 2 mm. Accordingly, the massive subsidence (>10 mm) found in 9 of the 79 cases reported by Eldrige et al. [3] and 7 of the 35 cases by Masterson et al. [15] seem to have been caused by the surgical technique, the nature of the graft and the geometry of the stem. However, we have considered that massive subsidence may be related to splitting of the cement mantle and some movement between the cement and graft and that early massive subsidence may be expected lead to a failure to obtain initial stability.
Table 3.
Comparison between the final-outcome Charnley scores and stem subsidence
| Subsidence | Final Charnley score | ||
|---|---|---|---|
| Pain | Function | Movement | |
| No subsidence | 5.3 | 5.1 | 5.1 |
| Graft-cement (<1 mm) | 5.2 | 5.3 | 5.0 |
| Stem-cement (<1 mm) | 5.3 | 5.5 | 5.2 |
| Stem-cement (1–2 mm) | 5.2 | 5.3 | 5.2 |
Concerning the sizes of the stems, we used two smaller stems [AP1 (30 mm), AP2 (33 mm)] that were developed in Hong Kong for small femurs in Asian patients [2] (Table 4). The body weights and heights of the South Korean patients in the present study (average: 56 kg and 157 cm, respectively) also were smaller than those of Western patients; femur stems smaller than the usual stem [no. 1, 2 (37.5 mm)] are needed to leave space for a cement mantle thickness of at least 2 mm [23].
Table 4.
Exeter stem size in patients who underwent femoral impaction grafting in revision hip arthroplasty
| Stem size | Number (% of group) |
|---|---|
| AP1 (30 mm) | 1 (2) |
| AP2 (33 mm) | 11 (20) |
| Small CDH (35.5 mm) | 25 (45) |
| Large CDH (37.5 mm) | 13 (23) |
| No. 1 (37.5 mm) | 4 (7) |
| No. 2 (37.5 mm) | 2 (4) |
Femoral fracture and perforation are the most common devastating complications of femoral impaction bone grafting. Most of the reports on this technique that include a section on complications have been highlighted; the prevalence has ranged from 5 to 24% [4, 9, 11, 15, 16, 20, 24]. In our study, intraoperative proximal fractures occurred in two hips during the removal of cement prior to impaction bone grafting, while intraoperative proximal fracture happened in three hips during impaction. Fortunately, none of the postoperative diaphyseal fractures that are the most serious complications of impaction allograft occurred, and all intraoperative fractures were discovered during the operation. In this respect, we have some agreement with the recommendations for preventing the disastrous complications of impaction graft reported by Gore [11].
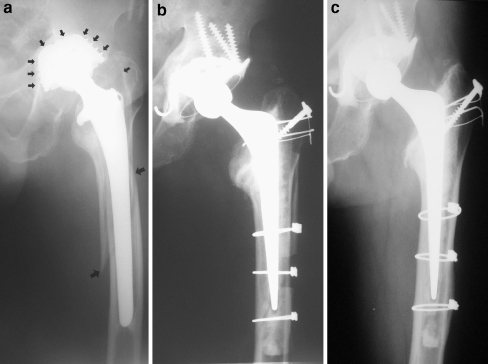
There is controversy about whether the femoral impaction bone-grafting method is best performed using a polished, tapered Exeter stem. In our study with a minimum 39-month follow-up, no progressive subsidence was seen at the final follow-up, and cortical repair and trabecular incorporation were observed in most of the cases (Fig. 1). We believe that the impaction allograft bone may substitute the living bone in the host skeleton and that a polished stem may provide the graft with a radial load that is beneficial to the bone remodeling.
Fig. 1.
Serial radiographs showing cortical repair and trabecular remodeling: (a) preoperative, (b) postoperative and (c) 4-year postoperative radiographs of impaction bone-grafting femur. Cortical repair and trabecular remodeling are visible in all areas around the proximal femur (c). There is no radiolucent line at the cement-bone interface
In conclusion, despite the relatively short-term follow-up compared with other reports in Western patients [11, 13, 18, 24], the impaction of fresh-frozen allograft and use of a cemented, polished, tapered stem were also successful with good clinical and radiographic outcomes in our study of Asian hips (South Korean patients). Furthermore, the complications of femoral fracture and subsidence had no harmful effects on the final clinical outcomes. However, we used two smaller stems [AP1 (30 mm); AP2 (33 mm)] than the usual stems (nos. 1 and 2 (37.5 mm)] for Western patients because of the smaller femurs.
Acknowledgments
We gratefully acknowledge Dr. Sung-Woo Choi and Professor Seung-Han Woo for their assistance with the present study. We also thank Dr. Timothy Barker for assistance in finalizing the manuscript, and Professor Ross Crowford for useful comments during the preparation of the manuscript.
References
- 1.Charnley J (1979) Low friction arthroplasty of the hip; theory and practice. Springer, New York
- 2.Chiu KH, Shen WY, Cheung KW, Tsui HF (2005) Primary Exeter total hip arthroplasty in patients with small femurs: a minimum of 10 years follow-up. J Arthroplasty 20:275–281 [DOI] [PubMed]
- 3.Eldridge JD, Smith EJ, Hubble MJ, Whitehouse SL, Learmonth ID (1997) Massive early subsidence following femoral impaction grafting. J Arthroplasty 12:535–540 [DOI] [PubMed]
- 4.Elting JJ, Mikhail WE, Zicat BA, Hubbell JC, Lane LE, House B (1995) Preliminary report of impaction grafting for exchange femoral arthroplsty. Clin Orthop 319:159–167 [PubMed]
- 5.Engelbrecht E, Heinert K (1987) Klassifikation und Behandlungscrichtlinien von Knochensubstanzverlusten bei Revisionsoperationen am Hüftgelenk-mittelfristige Ergebnisse. In: Primar- und Revisions-alloarthroplastik, Huft- und Kniegelenk: 10 Jahre Endo-klinik Hamburg. Springer-Verlag, Berlin Heidelberg, New York, pp 189–201
- 6.Fawcett KJ, Barr HR (1987) Tissue banking. American Association of Blood Banks, Arlington, VA
- 7.Fetzer GB, Callaghan JJ, Templeton JE, Goetz DD, Sullivan PM, Johnston RC (2001) Impaction allografting with cement for extensive femoral bone loss in revision hip surgery: a 4- to 8-year follow-up study. J Arthroplasty 16:195–202 [DOI] [PubMed]
- 8.Fowler JL, Gie GA, Lee AJ, Ling RS (1988) Experience with the Exeter total hip replcament since 1970. Orthop Clin North Am 19:477–489 [PubMed]
- 9.Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Huiskes R, Gardeniers J (1993) Impacted cancellous allograft and cement for revision total hip arthroplasty. J Bone Joint Surg [Br] 75:14–21 [DOI] [PubMed]
- 10.Giesen EB, Lamerights NM, Verdonschot N, Buma P, Schreurs BW, Huiskes R (1999) Mechanical characteristics of impacted morsellised bone grafts used in revision of total hip arthroplasty. J Bone Joint Surg [Br] 81:1052–1057 [DOI] [PubMed]
- 11.Gore DR (2002) Impaction bone grafting for total hip revision. Int Orthop 26:162–165 [DOI] [PMC free article] [PubMed]
- 12.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 141:17–27 [PubMed]
- 13.Holliday BR, English HW, Timperley AJ, Gie GA, Ling RS (2003) Femoral impaction grafting with cement in revision total hip replacement. Evolution of the techniques and results. J Bone Joint Surg [Br] 85:809–817 [PubMed]
- 14.Malchau H, Karrholm J, Wang YX, Herberts P (1995) Accuracy of migration analysis in hip arthroplasty. Digitized and conventional radiography, compared to radiostereometry in 51 patients. Acta Orthop Scand 66:418–424 [DOI] [PubMed]
- 15.Masterson EL, Masri BA, Duncan CP (1997) The cement mantle in the Exeter impaction allografting technique. A cause for concern. J Arthroplasty 12:759–764 [DOI] [PubMed]
- 16.Meding JB, Ritter MA, Keating EM, Faris PM (1997) Impaction bone-grafting before insertion of a femoral stem with cement in revision total hip arthroplasty. A minimum 2-year follow-up study. J Bone Joint Surg [Am] 79A:1834–1841 [DOI] [PubMed]
- 17.Merle d’Aubigné R, Postel M (1954) Functional results of hip arthroplasy with acrylic prosthesis. J Bone Joint Surg [Am] 36:451–475 [PubMed]
- 18.Mikhail WE, Wretenberg PF, Weidenhielm LR, Mikhail MN (1999) Complex cemented revision using polished stem and morselized allograft. Minimum 5-years’ follow-up. Arch Orthop Trauma Surg 119:288–291 [DOI] [PubMed]
- 19.Nelissen RG, Bauer TW, Weidenhielm LR, LeGolvan DP, Mikhail WE (1995) Revision hip arthroplasty with the use of cement and impaction grafting. Histological analysis of four cases. J Bone Joint Surg [Am] 77:412–422 [DOI] [PubMed]
- 20.Ornstein E, Atroshi I, Franzen H, Johnsson R, Sandquist P, Sundberg M (2006) Early complications after 144 consecutive hip revisions with impacted morselized allograft bone and cement. J Bone Joint Surg [Am] 84:1323–1328 [DOI] [PubMed]
- 21.Ornstein E, Franzen H, Johnsson R, Karlsson MK, Linder L, Sundberg M (2004) Hip revision using the Exeter stem, impacted morselized allograft bone and cement: a consecutive 5-year radiostereometric and radiographic study in 15 hips. Arch Orthop Scand 75:533–543 [DOI] [PubMed]
- 22.Simon JP, Fowler JL, Gie GA, Ling RS, Timperley AJ (1991) Impaction cancellous grafting of the femur in cemented total hip revision arthroplasty. J Bone Joint Surg [Br] 73(Suppl 1):73
- 23.Schmalzried TP, Harris WH (1993) Hybrid total hip replacement. A 6.5-year follow-up study. J Bone Joint Surg [Br] 75:608–615 [DOI] [PubMed]
- 24.Schreurs BW, Arts JJ, Verdonschot N, Buma P, Slooff TJ, Gardeniers JW (2005) Femoral component revision with use of impaction bone-grafting and a cemented polished stem. J Bone Joint Surg [Am] 87:2499–2507 [DOI] [PubMed]
- 25.van Biezen FC, ten Have BL, Verhaar JA (2000) Impaction bone-grafting of severely defective femora in revision total hip surgery: 21 hips followed for 41–85 months. Arch Orthop Scand 71:135–142 [DOI] [PubMed]