Abstract
Thirty-six tibial plateau fractures in 35 patients were treated with the less invasive stabilisation system (LISS). Patients’ mean age was 42 years. There were 27 type C fractures and nine type B fractures according to AO/OTA classification. The average time to healing was 4.2 months (3–7 months). Deep infection developed in two cases. One patient healed in 6° of varus, and seven patients had an increased articular angulation of 6° (4–8°) in the sagittal plane. There were no cases of loss of reduction, non-union, or deep vein thrombosis. The LISS system could be considered for the management of tibial plateau fractures.
Résumé
36 fractures du plateau tibial chez 35 patients, âgés en moyenne de 42 ans, étaient traitées avec le système peu invasif (LISS). IL y avaient 27 fractures de type C et 9 de type B selon la classification AO/OTA. Le temps moyen de consolidation était de 4,2 mois (3–7). Il y avait 2 infections profondes. Un patient était consolidé avec 6° de varus et 7 patients avaient une augmentation de l’angulation articulaire sagittale de 6° (4–8). Il n’y avait pas de cas de perte de réduction, de non consolidation, ou de thrombose veineuse profonde. Le système LISS peut être considéré comme un traitement fiable des fractures du plateau tibial.
Introduction
Tibial plateau fractures represent a treatment challenge and range from low-energy injuries in osteopenic bone to high-energy trauma with severe soft-tissue damage. It is often difficult to determine which method of fixation is best for any given fracture pattern. Fundamental principles that must be followed by the surgeons are: (1) reduction in the anteroposterior and lateral planes; (2) avoidance of varus; (3) minimisation of muscle and periosteal damage; and (4) stable internal fixation. The goal is to achieve union and prevent complications. The concept of the principle of preservation of the blood supply and atraumatic surgical technique led to the biological fixation techniques. Using this treatment, one sees lower soft-tissue complications and higher union rates. The less invasive stabilisation system (LISS) is a new internal fixator that combines both principles of the biomechanical properties of fixation and an optimum bone-to-implant contact [9].
The purpose of this study was to report the surgical outcome of patients treated by a minimally invasive approach for tibial plateau fractures.
Patients and methods
Thirty-six tibial plateau fractures in 35 patients were retrospectively studied, from 1999 to 2002. There were 23 male patients and 12 female. Their average age was 42 years (range 18 years to 82 years). The cause of the injury was an auto-versus-pedestrian accident in 17 patients, a motor-vehicle accident in 11 patients, a fall in four patients, a blow in two patients and a shotgun injury in one patient. Other associated injuries were present in five patients. Two patients had pneumothorax and rib fractures, two had upper extremity injuries (shoulder dislocation, humerus fracture), and one patient presented with a foot drop due to peroneal nerve palsy caused by the injury. Standardised radiographic control of the entire tibia (anteroposterior and lateral) and the knee (anteroposterior, lateral, oblique views) was performed in all patients at admission. CT scans were obtained for further investigation in order to identify the size and location of articular fragments.
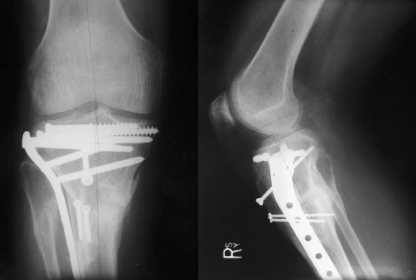
The fracture type was classified according to AO/OTA classification. There were 27 type C fractures and nine type B fractures. In many cases the fracture line extended distally to the metaphysis and/or diaphysis of the tibia. Two patients presented with open fractures that were classified according to Gustilo as type I and type II, respectively. Three patients presented with excessive swelling and blisters about the knee joint. All patients underwent operation within a mean time of 12 days (range 1 day to 30 days) after the injury. Surgery was performed as soon as the swelling resolved and the medical conditions allowed. A LISS plate was used in all patients and was inserted through a lateral approach beneath the tibialis anterior muscle. Intraoperatively, articular reduction was achieved either percutaneously (traction on the leg, femoral distractor, K wires, large pointed reduction forceps) or with a limited open approach. The position of the plate was adjusted under fluoroscopic control. At the end of the procedure a radiograph was routinely performed to verify the adequacy of the reduction of both the articular surface and the metadiaphyseal component of the fracture and the optimal position of the hardware (Fig. 1). Bone grafting was not performed in any of the cases. The mean operating time was 2.5 h, and the mean amount of blood loss was 250 ml.
Fig. 1.
Post-reduction anteroposterior and lateral radiographs of a tibia plateau and diaphyseal fracture treated with LISS plating
The assessment of the alignment and healing process was by radiographic and clinical evaluation in every follow-up visit. Partial weight bearing was allowed, depending on the clinical progress and radiological findings of each patient, but full weight bearing was not allowed for the first 3 months.
Results
Of the 35 patients, one died of causes unrelated to the implant. Of the remaining 34 patients with 35 fractures, 24 patients with 25 fractures were followed-up until healing was evident and complete. Follow-up time ranged from 3 to 26 months.
Ten patients could not be located and were lost to follow-up.
The healing possess was determined both clinically and radiographically. The average time to healing of the 25 fractures was 4.2 months (minimum 3 months, maximum 7 months) (Fig. 2). Two patients had delayed union (>7 months). Union in these patients was achieved through protected weight bearing in a cast after 10 months. The overall knee range of motion averaged 105° (range 0–135°) at the latest follow-up.
Fig. 2.
Seven-months postoperative radiographs of a proximal intra-articular tibial fracture stabilized with the LISS
Deep infection developed in two patients (8%). The first patient had suffered a type C closed fracture and developed wound drainage 7 days postoperatively; wound cultures grew Staphylococcus aureus. The patient underwent extensive irrigation and debridement (I&D) with antibiotic beads. A gastrocnemius rotational flap was used. No hardware was removed as it was proven to be very stable. The second patient, with a type B closed fracture, suffered a low-grade infection 1 month postoperatively. He underwent I&D. Infection was resolved following 4-weeks’ antibiotic therapy. There was no evidence of deep infection associated with open fractures.
One of 25 fractures (4%) healed in 6° of varus. In the remaining cases assessment of the fractures in terms of valgus/varus deviation indicated correct alignment. Seven fractures (28%) had an increase in articular angulation in the sagittal plane of 6° (range 4° to 8°). Six of them had an apex posterior angulation and one an apex anterior angulation. In all cases the angulation was present immediately postoperatively and did not increase thereafter. There were no cases of loss of reduction. The articular reduction was maintained in all cases, and there was no articular step-off greater than 2 mm.
Other complications included extended skin necrosis in a patient with a type C fracture. The patient presented with skin blisters and extensive swelling at the time of his first admission. He progressively developed skin necrosis, and a medial gastrocnemius rotational flap graft was used 2 months after his first operation. One patient complained of intermittent pain in the patellofemoral joint, probably due to post-traumatic arthritis. The patient was treated conservatively. A prominent plate was seen in a patient, which was not causing any clinical problems, and, thus, no treatment was given. No deep vein thrombosis was recorded.
Discussion
Tibial plateau fractures are serious injuries and can result in considerable morbidity. These fractures are high-energy injuries and often present with comminution and significant soft-tissue damage. Stable fixation without compromising the soft-tissue envelope is often difficult [18], and poor results are seen in 20% to 50% of all tibial plateau fractures [10].
Although the management of these fractures still remains controversial [3], the rates of complications, especially with bilateral approaches, are high [15, 18, 19]. Regardless of treatment the reported complications include: wound breakdown; deep infection (2.8% to 80%); deep vein thrombosis (3.6% to 10%); compartment syndrome; non-union; myositis ossificans; peroneal palsies; hardware failure; and arthrofibrosis [1–3, 8–10, 15–19].
An important factor in the outcome of tibial plateau fractures is the preservation of adequate anatomical reduction. Blokker et al. [3] found that inadequate anatomical reduction led to unsatisfactory results in 100%, compared to 14.3%, in patients with anatomical reduction. Axis deviation has been reported to be from 4% to 10% [15, 16].
As no current method satisfactorily avoids all these problems, alternative approaches have been explored to minimise these complications. Currently, minimally invasive techniques are gaining favour between orthopaedic surgeons, and there have been reports of patients who suffered tibia plateau fractures being treated exclusively by this technique [4, 5, 9, 11–14]. The LISS system consists of a pre-contoured, anatomically shaped plate that can be inserted with a minimally invasive technique and of screws that can be locked within the plate. Biomechanical testing has shown that the LISS demonstrates elastic deformation equal to that of conventional plates (lateral buttress and medial antiglide constructions) [7]. The LISS plate can also simultaneously achieve fixation of an associated metaphyseal/diaphyseal component of the fracture with a minimal approach.
In this study the LISS plate was used through a lateral approach in all patients. It was expected to minimise the surgical incision by decreasing the soft-tissue stripping, to provide a rigid fracture reduction and to respect the post-traumatic soft-tissue injury. The results showed that the surgical outcome of the patients treated with this technique is comparable to other treatment methods. The infection rate seen in this study (8%) could be expected, as tibia plateau fractures are high-energy injuries with a high rate of soft-tissue complications.
The potential disadvantages of a laterally inserted implant that have been described by Krettek et al. [9] include: (1) devitalisation of the fracture due to elevation of muscles from bone; (2) potential injury to the superficial peroneal nerve; (3) increased risk of developing compartment syndrome; and (4) difficulties in placement of the implant into confined spaces. However, none of the above-mentioned disadvantages was seen in this study. It could be argued that, since LISS technique provokes limited surgical insult to the surrounding soft tissues and to the healing process biology, the number of above-mentioned disadvantages appears to be minimised.
A review of the reported complications that have been published up to now in 139 tibia fractures treated with LISS include: deep or superficial infection; non-union; loss of fixation; screw malposition; peroneal palsy; hardware problems; malalignment; soft-tissue irritation; and removal difficulties [4, 6, 12, 14]. However, all these reported complications concern a limited number of patients.
We want to emphasise the zero rate of deep vein thrombosis. It could be argued that, by this technique, the surgical insult to the surrounding tissue and vessels is limited and thus predisposes to better muscular function and blood flow.
Cole et al. [4] stated that postoperative malalignments are due to surgeons’ unfamiliarity with closed reduction techniques, and discussed how good intraoperative radiographs are needed to minimise the incidence of malreductions. The increase in articular angulation of 6° in seven patients (28%) revealed in this study appeard not to play an important clinical role, as the overall range of motion averaged 105° and was compatible with other reported outcomes [4, 12, 14].
This study has some shortcomings that limit the conclusions. The main weakness is the short follow-up period and the limited number of patients. Longer-term follow-up and prospective randomised studies would certainly lead to additional conclusions. However, based on these results, the LISS technique could be considered for the management of these difficult fractures.
References
- 1.Andrews JR, Tedder JL, Godbout BP (1992) Bicondylar tibial plateau fracture complicated by compartment syndrome. Orthop Rev 3:317–319 [PubMed]
- 2.Blake R, Watson JT, Morandi M (1993) Treatment of complex tibial plateau fractures with the Ilizarov external fixator. J Orthop Trauma 7:167–168
- 3.Blokker CP, Rorabeck CH, Bourne RB (1983) Tibial plateau fractures. An analysis of the results of treatment in 60 patients. Clin Orthop 182:193–199 [PubMed]
- 4.Cole PA, Zlowodzki M, Kregor PJ (2004) Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma 18:528–535 [DOI] [PubMed]
- 5.El Barbary H, Abdel Ghani H, Misbah H, Salem K (2005) Complex tibial plateau fractures treated with Ilizarov external fixator with or without minimal internal fixation. Int Orthop 29:182–185 [DOI] [PMC free article] [PubMed]
- 6.Georgiadis GM, Gove NK, Smith AD, Rodway IP (2004) Removal of the less invasive stabilization system. J Orthop Trauma 18:562–564 [DOI] [PubMed]
- 7.Gosling T, Schandelmaier P, Marti A, Hufner T, Partenheimer A, Krettek C (2004) Less invasive stabilization of complex tibial plateau fractures: a biomechanical evaluation of a unilateral locked screw plate and double plating. J Orthop Trauma 18:546–551 [DOI] [PubMed]
- 8.King GJW, Schatzker J (1991) Case report. Nonunion of a complex tibial plateau fracture. J Orthop Trauma 2:209–212 [DOI] [PubMed]
- 9.Krettek C, Gerich T, Miclau T (2001) A minimally invasive medial approach for proximal tibial fractures. Injury 32(S3):4–13 [DOI] [PubMed]
- 10.Mallik AR, Covall DJ, Whitelaw GP (1993) Internal versus external fixation of bicondylar tibial plateau fractures. Orthop Rev 21:1433–1436 [PubMed]
- 11.Morgan SJ, Jeray KJ (2001) Minimally invasive plate osteosynthesis in fractures of the tibia. Op Tech Orthop 3:195–204 [DOI]
- 12.Schutz M, Kaab MJ, Haas N (2003) Stabilization of proximal tibial fractures with the LIS-system: early clinical experience in Berlin. Injury 34(S1):30–35 [DOI] [PubMed]
- 13.Smith WR, Shrank JR (2001) Tibial plateau fractures: minimally invasive fracture techniques. Op Tech Orthop 3:195–204
- 14.Stannard JP, Wilson TC, Volgas DA, Alonso JE (2004) The less invasive stabilization system in the treatment of complex fractures of the tibial plateau: short-term results. J Orthop Trauma 18:552–558 [DOI] [PubMed]
- 15.Stokel EA, Sadesivan KK (1991) Tibial plateau fractures standardized evaluation of operative results. Orthopedics 14:263–270 [PubMed]
- 16.Tscherne H, Lobenhoffer P (1993) Tibial plateau fractures. Management and expected results. Clin Orthop 292:87–100 [PubMed]
- 17.Waddell JP, Johnston DWC, Neidre A (1981) Fractures of the tibial plateau: a review of ninety-five patients and comparison of treatment methods. J Trauma 21:376–380 [DOI] [PubMed]
- 18.Weiner LS, Kelley M, Yang E, Steuer J, Watnick N, Evans M, Bergman M (1995) The use of combination internal fixation and hybrid external fixation in severe proximal tibia fractures. J Orthop Trauma 9:244–250 [DOI] [PubMed]
- 19.Young MJ, Barrack RL (1994) Complications of internal fixation of tibial plateau fractures. Orthop Rev 23:149–154 [PubMed]