Abstract
The aim of this study was to determine whether or not detaching the biceps tendon from the glenoid after tenodesis performed with the inclusion of the biceps in the rotator cuff suture results in an improved outcome. From 1999 to 2001, 22 patients had an arthroscopic rotator cuff repair and associated biceps tendon lesions that were repaired with two new arthroscopic techniques of tenodesis incorporating the biceps tendon in the rotator cuff suture. Patients were randomised into one of two groups: tenodesis without tenotomy (group 1) and tenodesis with tenotomy (group 2). Preoperative and postoperative functions were assessed by means of a modified UCLA rating scale and shoulder ROM. The mean follow-up period was 47.2 months (range 36– 59). In group 1 (tenodesis without tenotomy), eight patients had an excellent postoperative score and three a good postoperative score. The UCLA rating system used for evaluation showed a statistically significant improvement from the preoperative average rating of 10.5 (5–15) to the postoperative average score of 33 (29–35) (P<0.05). In group 2 (tenodesis with tenotomy), the UCLA rating system used for evaluation showed a statistically significant improvement from the preoperative rating of 11.1 to the postoperative score of 32.9 (P<0.05). No statistically significant difference in the total UCLA scores was found when comparing the repairs performed with or without tenotomy. Follow-up results with regard to ROM were not different between the two groups, and the range of motion was improved in all measured directions. In this series, every patient qualified as having good to excellent results according to the UCLA score. This study suggests that there is no difference between detaching and not detaching the biceps after including it in the repair.
Résumé
Le but de cette étude est de déterminer si le fait de détacher le tendon du biceps de la cavité glénoïde après ténodèse réalisé avec inclusion du tendon dans la réparation de la coiffe des rotateurs a une influence sur le résultat. De 1999 à 2001, 22 patients ont eu une réparation de la coiffe des rotateurs sous arthroscopie associée à des lésions du tendon du biceps qui furent réparés avec deux nouvelles techniques arthroscopiques de ténodèse incorporant le biceps dans la réparation de la coiffe. Les patients furent randomisés en deux groupes : ténodèse sans ténotomie (groupe 1) et ténodèse avec ténotomie (groupe 2). La fonction préopératoire et post opératoire a été mesurée au moyen de l’échelle UCLA et de la mesure des amplitudes articulaires. La durée moyenne du suivi est de 47.2 mois (allant de 36 à 59). Dans le groupe 1 (ténodèse sans ténotomie) 8 patients ont eu un excellent score post opératoire et 3 un bon score post opératoire. Le score UCLA utilisé pour l’évaluation a montré une amélioration significative avec une moyenne préopératoire de 10.5 (5 à 15) et une moyenne post opératoire de 33 (29 à 35) (P<0.05). Dans le groupe 2 (ténodèse avec ténotomie), le score UCLA utilisé pour l’évaluation montre une différence significative avec un score préopératoire de 11.1 et post opératoire de 32.9 (P<0.05). Il n’a pas été trouvé de différence significative au niveau du score UCLA quand on compare les réparations réalisées avec ou sans ténotomies. Les résultats au recul, en ce qui concerne le score amplitude n’étaient pas différents entre les deux groupes et les amplitudes de mouvements étaient améliorées dans toutes les directions. Dans ces séries, tous les patients étaient considérés comme des bons à excellents résultats selon le score UCLA. Cette étude suggère donc qu’il n’y a pas de différence que l’on détache ou pas le long biceps après l’avoir inclus dans la réparation.
Introduction
Rotator cuff tears are very frequently associated with long head of biceps pathology [8, 5]. If conservative treatment fails, surgery is indicated, and the surgeon may consider either tenotomy or tenodesis combined with cuff repair.
Biceps tenotomy is indicated if the tear is thought to be irreparable or if the patient is older and not willing to participate in the rehabilitation required after rotator cuff repair [1, 13].
Biceps tenodesis is indicated in case of severe biceps tendinopathy, partial biceps tendon tear (greater than 50% of the tendon diameter), full-thickness biceps tendon tears, medial subluxation of the tendon or nonreparable SLAP lesions [4, 9, 14, 24].
Moreover, different authors have recommended open or arthroscopic biceps tenodesis for younger, active patients, for patients requiring an acceptable aesthetic result (Popeye sign) or in order to avoid painful postoperative rehabilitation, probably resulting from the locking of the biceps stump into the bicipital sheath [4, 9, 14, 21, 24].
Many authors have described a variety of open or arthroscopic techniques employing suture anchors into the bicipital groove [9, 11, 21] or an interference screw fixation inside a reamed humeral tunnel [4]. All these techniques require increased operative time and the detachment of the biceps from the glenoid. Moreover, in cases of massive rotator cuff tear, the anterior leaf of the cuff is often contracted or deficient, and more tissue is required to obtain a strong repair; in this case, Burkhart et al. [22] advocated a margin convergence of the posterior cuff to the biceps tendon.
In this study, we compare two groups of patients affected by the association of massive rotator cuff tear and biceps pathology performing a tenodesis with the inclusion of the biceps tendon in the rotator cuff suture. The aim of this study was to determine whether or not detaching the biceps tendon from the glenoid after the tenodesis results in improved outcome.
Materials and methods
Between 1999 and 2001, we performed 181 arthroscopic rotator cuff repairs. In 22 of these repairs, we found severe associated biceps tendon lesions that were repaired with two new arthroscopic techniques of tenodesis incorporating the biceps tendon in the rotator cuff suture. In all patients appropriate nonoperative therapy, including nonsteroidal anti-inflammatory drugs, physiotherapy, rest and local injections, had previously failed. None of the patients had undergone a prior surgical procedure on the affected shoulder.
We performed all preoperative evaluations the day before surgery and postoperative evaluations at the final follow-up. The mean follow-up period was 47.2 months (range 36–59). Each patient was evaluated for arm dominance, trauma history, onset, duration and the type of preoperative symptoms, activity level, acromial morphology, type of lesion, pre- and postoperative ROM and pre- and postoperative modified shoulder score (UCLA). Pain onset was considered acute if the patient could remember a single event that initiated the pain. The activity level was evaluated and categorised as sedentary, light work and heavy manual work. The anterior acromion was classified according to the classification of Bigliani et al. [2]. All patients had a full-thickness rotator cuff lesion with or without retraction.
Each patient had at least one positive biceps test (Speed’s test, Yergason’s test, active compression test or biceps instability test). All patient were examined by the senior author. All shoulders had preoperative assessment by the use of standard radiographs (anteroposterior projections, neutral, external and internal rotation, a lateral view of the scapula and an axillary view) and MRI scans.
A modified UCLA (University of California, Los Angeles) shoulder rating scale was used to evaluate preoperative and postoperative shoulder pain, function and range of motion, strength and patient satisfaction. The maximum score obtainable is 35. The scores were divided into excellent (34–35 points), good (28–33), fair (21–27) and poor (0–20).
Arthroscopic repair of the lesions was performed by one of two new tenodesis techniques, in all cases incorporating the biceps tendon in the rotator cuff suture. Patients were randomised into one of two groups:
tenodesis without tenotomy
tenodesis with tenotomy.
The assignment of patients to one of the two groups was based on computerised randomization. All surgical interventions were performed by the same surgeon.
Patient demographics are presented in Tables 1 (tenodesis without tenotomy) and 2 (tenodesis with tenotomy).
Table 1.
Tenodesis without tenotomy
| Patient no. | Age | Gender | Dominant arm | Trauma history | Activity level | Acromial morphology | Supraspinatus tear | Infraspinatus tear | Subscapularis tear | Biceps lesion |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 41 | M | Yes | Yes | Heavy manual work | Bigliani type III | Yes | Yes | Yes | >50% lesion |
| 2 | 79 | F | Yes | No | Sedentary | Bigliani type I | Yes | No | No | Unstable |
| 3 | 47 | M | Yes | Yes | Heavy manual work | Bigliani type II | Yes | Yes | Yes | >50% lesion |
| 4 | 67 | M | Yes | No | Sedentary | Bigliani type I | Yes | No | Yes | Dislocated |
| 5 | 71 | F | No | No | Sedentary | Bigliani type III | Yes | No | No | Dislocated |
| 6 | 69 | F | Yes | Yes | Sedentary | Bigliani type II | Yes | No | No | >50% lesion |
| 7 | 55 | F | No | No | Light work | Bigliani type III | Yes | Yes | No | Dislocated |
| 8 | 46 | M | Yes | Yes | Heavy manual work | Bigliani type I | Yes | No | Yes | Unstable |
| 9 | 53 | M | Yes | No | Light work | Bigliani type II | Yes | No | No | >50% lesion |
| 10 | 69 | M | No | No | Sedentary | Bigliani type II | Yes | Yes | Yes | Dislocated |
| 11 | 66 | F | Yes | Yes | Sedentary | Bigliani type I | Yes | No | No | Unstable |
| Patient no. | Active preop range of motion Forward flexion | Active preop range of motion External rotation of adducted arm | Active preop range of motion Internal rotation | Active postop range of motion Forward flexion | Active postop range of motion External rotation of adducted arm | Active postop range of motion Internal rotation | ||||
| 1 | 30 | 30 | L2 | 160 | 45 | T10 | ||||
| 2 | 120 | 45 | L4 | 150 | 70 | T7 | ||||
| 3 | 50 | 30 | L5 | 150 | 70 | T6 | ||||
| 4 | 110 | 30 | L4 | 160 | 60 | T5 | ||||
| 5 | 140 | 45 | T10 | 160 | 60 | T5 | ||||
| 6 | 140 | 60 | L3 | 170 | 70 | T7 | ||||
| 7 | 110 | 30 | L1 | 160 | 45 | T7 | ||||
| 8 | 60 | 30 | L4 | 150 | 60 | T7 | ||||
| 9 | 110 | 30 | T12 | 170 | 60 | T7 | ||||
| 10 | 120 | 30 | L4 | 170 | 45 | T11 | ||||
| 11 | 130 | 45 | L5 | 170 | 60 | T10 | ||||
| Patient | Munford procedure | Symptom duration | Onset | Preop UCLA score | Postop UCLA score | Follow-up (months) | ||||
| 1 | Yes | <6 months | Acute | 5 | 30 | 51 | ||||
| 2 | Yes | 6–12 months | Insidious | 15 | 34 | 59 | ||||
| 3 | Yes | 6–12 months | Acute | 7 | 29 | 40 | ||||
| 4 | No | 6–12 months | Insidious | 12 | 35 | 55 | ||||
| 5 | Yes | 6–12 months | Insidious | 10 | 29 | 38 | ||||
| 6 | No | >12 months | Acute | 9 | 34 | 48 | ||||
| 7 | No | >12 months | Insidious | 8 | 35 | 36 | ||||
| 8 | Yes | <6 months | Acute | 7 | 35 | 55 | ||||
| 9 | No | >12 months | Insidious | 14 | 35 | 45 | ||||
| 10 | No | >12 months | Insidious | 15 | 34 | 54 | ||||
| 11 | No | >12 months | Acute | 14 | 34 | 52 |
Table 2.
Tenodesis with tenotomy
| Patient nw | Age | Gender | Dominant arm | Trauma history | Activity level | Acromial morphology | Supraspinatus tear | Infraspinatus tear | Subscapularis tear | Biceps lesion |
| 12 | 78 | M | Yes | No | Sedentary | Bigliani type I | Yes | No | No | Unstable |
| 13 | 43 | M | Yes | Yes | Heavy manual work | Bigliani type I | Yes | Yes | Yes | >50% lesion |
| 14 | 81 | F | No | No | Sedentary | Bigliani type III | Yes | No | Yes | Dislocated |
| 15 | 56 | M | Yes | Yes | Light work | Bigliani type II | Yes | No | No | Unstable |
| 16 | 48 | M | Yes | Yes | Heavy manual work | Bigliani type III | Yes | Yes | Yes | >50% lesion |
| 17 | 40 | M | No | No | Heavy manual work | Bigliani type I | Yes | Yes | Yes | >50% lesion |
| 18 | 67 | M | No | No | Light work | Bigliani type II | Yes | No | No | Dislocated |
| 19 | 73 | F | Yes | No | Sedentary | Bigliani type I | Yes | No | Yes | Unstable |
| 20 | 45 | M | Yes | Yes | Heavy manual work | Bigliani type II | Yes | No | No | Unstable |
| 21 | 57 | F | Yes | No | Sedentary | Bigliani type III | Yes | Yes | No | >50% lesion |
| 22 | 52 | F | Yes | No | Light work | Bigliani type II | Yes | Yes | No | Dislocated |
| Patient no. | Active preop range of motion Forward flexion | Active preop range of motion External rotation of adducted arm | Active preop range of motion Internal rotation | Active postop range of motion Forward flexion | Active postop range of motion External rotation of adducted arm | Active postop range of motion Internal rotation | ||||
| 12 | 150 | 45 | L1 | 160 | 60 | T7 | ||||
| 13 | 30 | 45 | L5 | 170 | 45 | T10 | ||||
| 14 | 110 | 60 | L4 | 160 | 70 | T5 | ||||
| 15 | 130 | 30 | L4 | 150 | 50 | T12 | ||||
| 16 | 60 | 30 | L5 | 140 | 60 | T10 | ||||
| 17 | 30 | 30 | L5 | 150 | 45 | T10 | ||||
| 18 | 140 | 30 | T12 | 170 | 60 | T7 | ||||
| 19 | 130 | 45 | L3 | 170 | 60 | T7 | ||||
| 20 | 140 | 45 | L1 | 150 | 60 | T10 | ||||
| 21 | 150 | 60 | L3 | 170 | 90 | T7 | ||||
| 22 | 140 | 30 | L4 | 160 | 60 | T7 | ||||
| Patient | Munford procedure | Symptom duration | Onset | Preop UCLA score | Postop UCLA score | Follow-up (months) | ||||
| 12 | Yes | >12 months | Insidious | 11 | 34 | 46 | ||||
| 13 | Yes | 6–12 months | Acute | 7 | 29 | 43 | ||||
| 14 | Yes | >12 months | Insidious | 10 | 35 | 39 | ||||
| 15 | No | >12 months | Acute | 14 | 35 | 41 | ||||
| 16 | Yes | >12 months | Acute | 10 | 29 | 47 | ||||
| 17 | No | <6 months | Insidious | 7 | 34 | 43 | ||||
| 18 | No | 6–12 months | Insidious | 12 | 35 | 39 | ||||
| 19 | Yes | >12 months | Insidious | 14 | 34 | 58 | ||||
| 20 | Yes | <6 months | Acute | 11 | 34 | 50 | ||||
| 21 | No | >12 months | Insidious | 14 | 29 | 55 | ||||
| 22 | No | 6–12 months | Insidious | 12 | 34 | 45 |
In group 1 (tenodesis without tenotomy), there were six men and five women. The mean age was 60.3 years (range, 41 to 79). The injury was reported to be acute in five of the patients and insidious in the other six. The dominant arm was affected in seven cases. Three patients were engaged in professions involving regular heavy manual activity (e.g., carpenter).
The biceps tendon was dislocated in four cases, unstable in three cases and torn by more than 50% of its diameter in four cases.
In group 2 (tenodesis with tenotomy), there were five men and six women. The mean age was 58.1 years (range, 40 to 81). The injury was reported to be acute in four of the patients and insidious in the other seven. The dominant arm was affected in eight cases. Three patients were engaged in professions involving regular heavy manual activity. The biceps tendon was dislocated in three cases, unstable in four cases and torn by more than 50% of its diameter in four cases. Statistical analyses were performed with the Wilcoxon Sign Rank test. Significance was set at P<0.05.
Arthroscopic technique
Patients underwent brachial plexus block, associated in five cases with a general anaesthesia, and were then placed in a lateral decubitus position. The arm was suspended at approximately a 45° angle of abduction and 10° forward flexion. Distraction of the shoulder joint was accomplished with 10 to 14 lb of traction. Four to six portals were used during the procedure. A posterior portal was created, and the arthroscope was inserted into the glenohumeral joint. A thorough diagnostic arthroscopic examination was then performed for evaluation of the extent of the rotator cuff tear, lesions of the biceps tendon and other associated lesions. The most important subacromial portals were the posterolateral viewing, the anterolateral and the lateral working portal, equipped with an 8.25-mm cannula. To control bleeding we used radiofrequency with adrenalin admixture to the irrigation fluid and asked the anaesthetist to lower the systolic blood pressure to 90 mmHg if possible. An arthroscopic pump maintained a fluid pressure of 40 mmHg that could be increased temporarily on demand.
A spinal needle was introduced percutaneously to ascertain the precise location for placement of the anterolateral portal created approximately 2 to 3 cm anterior and lateral to the anterolateral corner of the acromion. If the subscapularis tendon was involved, an anterior midlateral portal was created just superior to the lateral half of the subscapularis tendon. The arthroscope was used through the posterior portal to gain visualisation of the biceps tendon. The lateral portal was used to mobilise the rotator cuff back to its bony insertion.
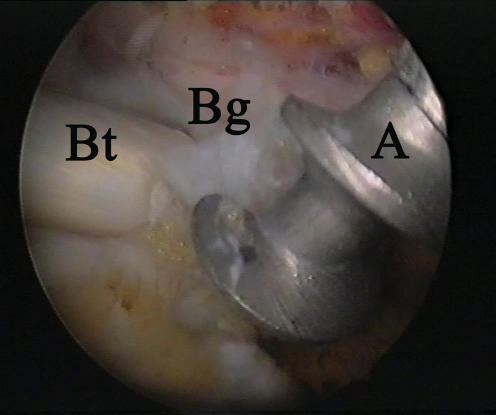
Using a burr through the lateral portal, the articular and bony surface was abraded under the biceps tendon, just proximal to the bicipital groove. Shifting to the lateral portal as a viewing portal, the anterolateral portal was used to insert the first suture anchor slightly proximal to the bicipital groove (Fig. 1).
Fig. 1.
Arthroscopic view from a lateral portal showing suture anchor proximal to the bicipital groove. (A, anchor; Bt, biceps tendon; Bg, bicipital groove)
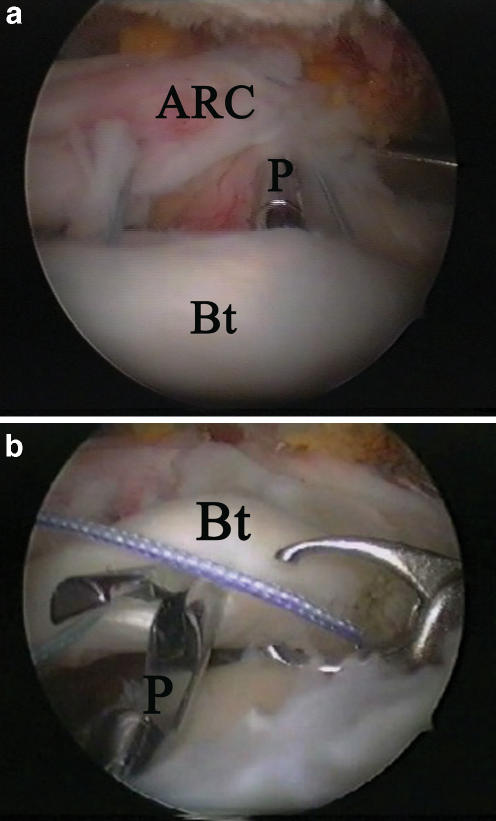
A penetrator suture passer (Arthrex) was passed through the anterior leaf of the rotator cuff tear (Fig. 2a) and through the biceps tendon (Fig. 2b); the sutures were then retrieved through the posterior edge of the rotator cuff tear from a posterior portal in the same manner.
Fig. 2.
Arthroscopic view through a lateral portal showing: (a) penetrator passage through the anterior leaf of the rotator cuff and the biceps. (b) The retrieving of the sutures from an anterolateral portal. (Bt, biceps tendon; ARC, anterior leaf of rotator cuff; P, penetrator)
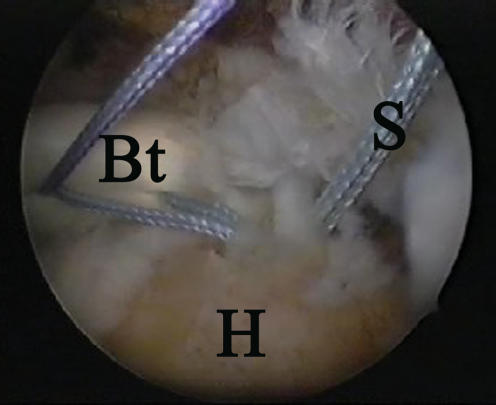
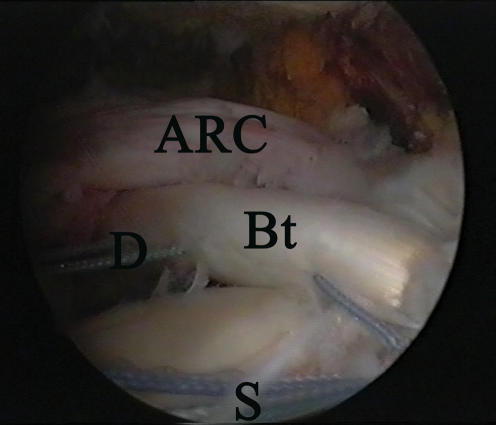
Both ends were tied with a Sixth Finger knot pusher (Arthrex) providing a margin convergence of the two edges of the cuff (Figs. 3, 4). One to two double-loaded anchors (Corkscrew Arthrex) in a double row format were used depending on the size of the rotator cuff footprint.
Fig. 3.
Arthroscopic view through a lateral portal showing the sutures passed through the biceps and the anterior leaf of the cuff. (Bt, biceps tendon; H, humeral head; S, Anchor suture)
Fig. 4.
Arthroscopic view through a lateral portal before tying knots. (ARC, rotator cuff; Bt, biceps tendon; S, Anchor suture; D, side to side suture
The remaining intra-articular tendon stump of the biceps was resected in 11 patients (group 2) and left attached at the glenoid tubercle in 11 patients (group 1). The surgery was concluded with an acromioplasty, removing anterior and lateral bone spurs in cases of type 2 and 3 acromion.
Postoperative management
Postoperative management was the same for both groups. The arm was supported using a sling with an abduction pillow for 6 weeks. Active elbow flexion and extension were allowed, but terminal extension was restricted. Passive external rotation was started from the first day after surgery and maintained within a comfortable range. Overhead stretching was restricted until 6 weeks postoperatively to avoid damaging the repair. At 6 weeks the sling was removed, and overhead stretching with a rope and pulley were started. Isotonic strengthening and rehabilitation of the rotator cuff, deltoid and scapular stabilisers were initiated at 10 or 12 weeks after the operation. The rehabilitation was continued for 6 months. Heavy manual work and overhead activities were allowed after a good restoration of the shoulder strength, which occurred at 6 to 10 months after surgery.
Results
In group 1 (tenodesis without tenotomy), eight patients had an excellent postoperative score and three a good postoperative score. The UCLA rating system used for evaluation showed a statistically significant improvement from a preoperative average rating of 10.5 (5–15) to a postoperative average score of 33 (29–35) (P<0.05).
The forward flexion averaged 102° (range, 30–140°) preoperatively, and it averaged 161° (range, 150°–170°) at the final follow-up (P<0.05).
The average external rotation of the adducted arm improved from 37° (range, 30–60°) to 59° (range, 45–70°) (P<0.05).
Internal rotation increased from a range of L5 to T10 preoperatively to a range of T11 to T5 at the final follow-up.
In group 2 (tenodesis with tenotomy), the UCLA rating system used for evaluation showed a statistically significant improvement from the preoperative rating of 11.1 to a postoperative score of 32.9 (P<0.05).
The forward flexion averaged 110° (range, 30–150°) preoperatively, and it averaged 159° (range, 140–170°) at the final follow-up (P<0.05).
The average external rotation of the adducted arm improved from 41° (range, 30–60°) to 60° (range, 45–90°) (P<0.05). Internal rotation increased from a range of L5 to T12 preoperatively to a range of T12 to T5 at the final follow-up. No statistically significant difference in the total UCLA scores was found when comparing repairs performed with or without tenotomy. In fact, the mean postoperative UCLA score for tenodesis without tenotomy was 33 versus 32.9 for tenodesis with tenotomy (P>0.05).
Follow-up results with regard to ROM were not different between the two groups, and the range of motion was improved in all measured directions. In the two groups, eight patients qualified as having excellent results. None of the patients rated the surgery as unsuccessful. No infection, intraoperative neurological or vascular compromise was detected in any of the patients. None of the patients had bicipital pain, cosmetic deformity (Popeye sign) or limitations in activities of daily living at the final follow-up.
Discussion
The role of the biceps tendon in shoulder pain has been debated. Historically, the biceps tendon has been considered to be a major source of shoulder pain, and its treatment has been considered to be a primary procedure. Over time, primary surgery on the biceps tendon has become less popular because of major interest in the rotator cuff. Currently, new interest is being focused on the long head of biceps because of the accumulation of research and clinical experience [5, 6].
An association between rotator cuff tears and biceps tendon lesions is frequent [8, 15]. In fact, rotator cuff tears may produce more pressure and friction on the biceps tendon [10], promoting biceps lesions.
Long head of biceps tendon (LHBT) pathology is more common in shoulders affected by rotator cuff tears due to the higher tendon loads caused by the alteration of shoulder biomechanics [7].
Commonly used solutions are biceps tenotomy or biceps tenodesis. Biceps tenodesis is suggested in young, active patients that present with a degeneration of less than 50% of the biceps tendon fibres, medial subluxation of the biceps tendon, combined subscapularis tears and biceps subluxation or nonreparable SLAP lesions [16, 19].
Biceps tenotomy is indicated if the rotator cuff tear is thought to be irreparable or if the patient is older and not willing to participate in the rehabilitation required after rotator cuff repair [4, 9, 14, 24].
Biceps tenotomy may be a reasonable alternative to biceps tenodesis in patients with refractory chronic bicipital pain [18]. This technique has some disadvantages: distal migration of the LHBT with cosmetic deformity (Popeye sign) and significantly impaired shoulder strength [26]. However, it is a quick procedure that does not require fixation.
Biceps tenodesis has potential advantages over tenotomy that include prevention of muscle atrophy, maintenance of the length-tension relationship, maintenance of elbow flexion and supination strength, avoidance of cramping pain and avoidance of cosmetic deformity [23].
Many authors have dealt with various tenodesis techniques. Boileau et al. [4] and Burkhart et al. [14] described an arthroscopic technique using a biointerference screw technique into a bone socket, a method almost twice as strong as the suture anchor construct described by Garstmann et al. [9].
Checchia et al. [8] first described a soft tissue arthroscopic tenodesis incorporating the biceps into the rotator cuff repair, avoiding the use of a separate fixation technique for the biceps.
All these tenodesis techniques require the detachment of the biceps from the glenoid tubercle. Wolfgang [27] suggested the use of the proximal portion of the biceps tendon as a graft remaining attached and sutured over the gap with the goal of giving additional blood supply to a hypovascular rotator cuff repair. In fact, labral branches of the suprascapular artery may offer blood supply to the long head of the biceps [20]. Moreover, the detachment of the LHBT may produce instability and disfunction, leading to a significant upward migration of the humeral head and a 5.1% decrease of the acromiohumeral space [12, 25].
Neviaser [17] and Bigliani et al. [3] published two different open techniques of rotator cuff augmentation using the biceps tendon as a graft; Burkhart et al. [22] reported a case of an immobile, contracted anterior leaf of the rotator cuff in which they described a technique of margin convergence of the more mobile posterior cuff to the biceps tendon in order to provide an internal splint that decreases strain so as to protect the repair and to enhance the mechanical soundness and stability of the repair.
The concept of our technique, not detaching the biceps, was to create two fixation points for the biceps: the first at the glenoid tubercle and the second at the site of one of the anchors used for the rotator cuff repair, very close to the bicipital groove. This method allows the biceps to serve as a splint in the repair of a massive rotator cuff lesion.
In our series of 22 shoulders, the biceps tendon was resected in 11 patients (group 2) and left attached at the glenoid tubercle in 11 patients (group 1).
We did not find a statistically significant difference in the total UCLA score when comparing tenodesis performed with or without tenotomy. In fact, the mean postoperative UCLA score for tenodesis without tenotomy was 33 versus 32.9 for tenodesis with tenotomy (P>0.05), and follow-up results with regard to ROM were not different between the two groups, improving in all measured directions. By leaving the tendon attached, our goal was to use the biceps as a scaffold in the side-to-side repair and to offer a fresh blood supply to a degenerated rotator cuff that may be hypovascular.
References
- 1.Barber FA, Byrd JW, Wolf EM, Burkhart SS (2001) How would you treat the partially torn biceps tendon? Arthroscopy 17:636–639 [DOI] [PubMed]
- 2.Bigliani LU, Morrison DS, April EW (1986) The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans 10:228
- 3.Bigliani LU, Cordasco FA, McIlveen SJ, Musso ES (1992) Operative repair of massive rotator cuff tears: long-term results. J Shoulder Elbow Surg 1:120–130 [DOI] [PubMed]
- 4.Boileau P, Krishnan SG, Coste JS, Walch G (2002) Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthroscopy 18:1002–1012 [DOI] [PubMed]
- 5.Burkhead WZ (1990) The biceps tendon. In: Rockwood CA, Matsen FAI (eds) The shoulder. Philadelphia. WB Saunders, pp 791–836
- 6.Burkhead WZ (2000) The biceps tendon. In: Rockwood CAJ, Matsen FAI (eds) The shoulder. Philadelphia. WB Saunders, pp 1009–1063
- 7.Carpenter JE, Wening JD, Mell AG, Langenderfer JE, Kuhn JE, Hughes RE (2005) Changes in the long head of the biceps tendon in rotator cuff tear shoulders. Clin Biomech 20:162–165 [DOI] [PubMed]
- 8.Checchia SL, Doneux PS, Miyazaki AN, Silva LA, Fregoneze M, Ossada A, Tsutida CY, Masiole C (2005) Biceps tenodesis associated with arthroscopic repair of rotator cuff tears. J Shoulder Elbow Surg 14:138–144 [DOI] [PubMed]
- 9.Gartsman GM, Hammerman SM (2000) Arthroscopic biceps tenodesis: operative technique. Arthroscopy 16:550–552 [DOI] [PubMed]
- 10.Gill TJ, McIrvin E, Mair SD, Hawkins RJ (2001) Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg 10:247–249 [DOI] [PubMed]
- 11.Klepps S, Hazrati Y, Flatow E (2002) Arthroscopic biceps tenodesis. Arthroscopy 18:1040–1045 [DOI] [PubMed]
- 12.Kumar VP, Satku K, Balasubramaniam P (1989) The role of the long head of biceps brachii in the stabilization of the head of the humerus. Clin Orthop Relat Res 244:172–175 [PubMed]
- 13.Lo IK, Burkhart SS (2002) Arthroscopic biceps tenodesis: indications and technique. Operat Tech Sports Med 10:105–112 [DOI]
- 14.Lo IK, Burkhart SS (2004) Arthroscopic biceps tenodesis using a bioabsorbable interference screw. Arthroscopy 20:85–95 [DOI] [PubMed]
- 15.Mazzocca AD, Rios CG, Romeo AA, Arciero RA (2005) Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy 21:896 [DOI] [PubMed]
- 16.Murthi AM, Vosburgh CL, Neviaser TJ (2000) The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg 9:382–385 [DOI] [PubMed]
- 17.Neviaser RJ (1980) Lesions of the biceps and tendinitis of the shoulder. Orthop Clin North Am 11:343–348 [PubMed]
- 18.Osbahr DC, Diamond AB, Speer KP (2002) The cosmetic appearance of the biceps muscle after long-head tenotomy versus tenodesis. Arthroscopy 18:483–487 [DOI] [PubMed]
- 19.Ozalay M, Akpinar S, Karaeminogullari O, Balcik C, Tasci A, Tandogan RN, Gecit R (2005) Mechanical strength of four different biceps tenodesis techniques. Arthroscopy 21:992–998 [DOI] [PubMed]
- 20.Rathbun JB, Macnab I (1970) The microvascular pattern of the rotator cuff. J Bone Joint Surg Br 52:540–553 [PubMed]
- 21.Richards DP, Burkhart SS (2004) Arthroscopic-assisted biceps tenodesis for ruptures of the long head of biceps brachii: the cobra procedure. Arthroscopy 20(Suppl 2):201–207 [DOI] [PubMed]
- 22.Richards DP, Burkhart SS (2004) Margin convergence of the posterior rotator cuff to the biceps tendon. Arthroscopy 20:771–775 [DOI] [PubMed]
- 23.Romeo A (2002) Biceps tenodesisis. presented at the american society for sports medicine annual meeting. Orlando, FL, June 30–July 3
- 24.Romeo AA, Mazzocca AD, Tauro JC (2004) Arthroscopic biceps tenodesis. Arthroscopy 20:206–213 [DOI] [PubMed]
- 25.Warner JJ, McMahon PJ (1995) The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg Am 77:366–372 [DOI] [PubMed]
- 26.Wolf RS, Zheng N, Weichel D (2005) Long head biceps tenotomy versus tenodesis: a cadaveric biomechanical analysis. Arthroscopy 21(2):182–185, Feb [DOI] [PubMed]
- 27.Wolfgang GL (1974) Surgical repair of tears of the rotator cuff of the shoulder. Factors influencing the result. J Bone Joint Surg Am 56:14–26 [PubMed]