Abstract
Between 1988 and 2003, 23 patients with paralytic calcaneus-valgus feet were submitted to the Westin procedure and 17 patients (25 feet) were re-evaluated. Nine patients were male and eight were female. The mean age at the surgical procedure was 8±5 years. The aetiology of paralysis was sequelae of poliomyelitis in 6 patients (8 feet) and of myelomeningocele in 11 patients (17 feet). The mean follow-up period was 6±6 years. The results were analysed clinically and radiographically considering the decrease of the retropulsion, the patient’s satisfaction, and the increase of the lateral tibiocalcaneal angle. Results were considered satisfactory when the patients showed a decrease of the retropulsion during gait, improvement of the gait pattern, and an increase of the tibiocalcaneal angle. As an overall result, 16 patients (94.2%) were satisfied and 1 patient (two feet) dissatisfied with the outcome. The increase of the tibiocalcaneal angle was significant for the myelomeningocele patients (P=0.001), but not for poliomyelitis (P=0.053). No statistical relation between the follow-up period and the increase of the tibiocalcaneal angle was found (r=0.04). The authors concluded that the Westin procedure is a good technique for the treatment of paralytic calcaneus valgus feet with myelomeningocele.
Résumé
Entre 1988 et 2003, 23 patients présentant un pied valgus paralytique ont été traités par le procédé de Westin et 17 patients (25 pieds) ont été évalués. Neuf patients étaient de sexe masculin et huit de sexe féminin. L’âge moyen à l’intervention a été de 8 ans ±5 ans. L’étiologie de la paralysie était surtout une séquelle de polio dans six cas (8 pieds), un myéloméningocèle chez 11 patients (17 pieds). Le suivi moyen a été de 6 ans ±6. Les résultats ont été analysés cliniquement et radiographiquement. Les résultats ont été considérés comme satisfaisants lorsque les patients ont présenté une diminution de la rétropulsion durant la marche avec une amélioration de la boiterie et une augmentation de l’angle tibiocalcanéen. Seize patients (94.2%) ont été satisfaits et un patient (deux pieds) satisfait. L’augmentation de l’angle tibiocalcanéen a été significatif chez les myloméningocèle (P=0.001) alors qu’il n’était pas significatif sur les pieds polio (P=0.053). Aucune relation statistiquement significative n’a été trouvée entre la période de suivi et l’amélioration de l’angle tibiocalcanéen (r=0.04). Les auteurs concluent que le procédé de Westin est une bonne technique pour le traitement des pieds valgus paralytiques chez le myéloméningocèle.
Introduction
Foot deformities in patients with Poliomyelitis and lower lumbar myelomeningocele sequelae are frequent and incapacitating. Among the foot deformities that affect patients with myelomeningocele, approximately 20% of the cases presented with calcaneus deformity. But despite the muscle deficit, most of these patients become community walkers [1–6].
Resulting from the muscle imbalance from peripheral or central nervous lesions, calcaneus deformities are the result of the absence or reduction of triceps surae muscle power with normal or spastic tibialis anterior, extensor digitorum longus and extensor hallucis longus muscles. With the imbalance between the forces of dorsiflexion and plantar flexion of the ankle and foot, a rotation of the calcaneus to a vertical position is generated, developing what is called “paralytic pes calcaneus” [1, 2, 5–14].
The patients should be treated during childhood, because as the deformity inevitably progresses, the severity increases and no satisfactory results will be possible [1, 2].
In 1901, Whitman emphasised that muscle deficiency is more important than the deformity itself. In 1921, Hoke claimed that the difficulty the patient with this deformity encounters during ambulation is comparable to the gait of an individual with an artificial limb [1, 2].
At the final stance phase of gait, the calcaneus foot suffers loss of impulsion, with foot dorsiflexion and toe extension. This fact, associated with insufficient posterior activity of the calcaneal tendon, can cause posterior subluxation of the tibia over the talus, defining what is called retropulsion [14].
Skin ulceration may also occur as a consequence of the calcaneal prominence and abnormal support of the feet. The lack of sensibility can lead to destruction of the fat pad in areas of greater pressure, with the risk of osteomyelitis of the calcaneus [1, 7, 15, 16].
Another important effect of triceps surae muscle paralysis is the distal fibular growth inhibition and it is still possible to find narrowing of the lateral portion of the distal fibular epiphysis and valgus of the ankle joint [16–18].
In skeletally immature patients, brace treatment is effective to improve the gait, but does not reduce the calcaneus retropulsion. Therefore, the transfer of the tendons with normal muscle power to the calcaneus is one of the best treatment options [13].
One of the first descriptions of tendon transfer was from Nicoladoni in 1881, transfering the fibular tendons to the calcaneus to correct deformities [19]. In 1956, Herdon et al. showed the efficacy of tendon transfers in poliomyelitis treatment done in the early phases, attempting to prevent the establishment of the deformity or even the progression of those already present [10].
The same authors used the technique originally proposed by Peabody [10] and confirmed the efficacy of the tendon transfers in re-establishing gait with a platigrade foot and allowing the patient to stand on their toes in the equinus position. Similar results were obtained later in patients with myelomeningocele [20].
Several other techniques such as calcaneus osteotomies, with or without tendon transfers, have been described to reduce the vertical calcaneus in this deformity [21].
The treatment of the pes calcaneus with the Achilles tenodesis to the tibia in poliomyelitis patients had been successfully demonstrated since 1913 by Gallie and later by Jacobs in 1966 [13, 14].
Westin in 1967 performed 18 tenodeses to the tibia in polio patients with correction of the deformity, decreasing the gait abnormality and stimulating growth on the posterior aspect of the tibia and on the calcaneus [1, 2, 13].
In one of his cases, an unintentional suture between the Achilles tendon and the fibula was made. After 18 months, hypertrophy of the fibula was observed, associated with its growth in length [13, 14]. From these observations, tenodesis of the Achilles to the fibula was adopted as a new surgical technique. The Westin procedure aims at mechanical blocking of ankle retropulsion, improvement of the calcaneal deformity and progressive correction of the ankle valgus deformity by stimulating distal fibular growth [13, 14].
The purpose of this study was to evaluate the clinical and radiographic results of patients with paralytic calcaneus-valgus foot treated by the Westin technique.
Materials and methods
Between 1988 and 2003, 23 patients with paralytic calcaneus-valgus foot were treated with the Westin technique.
The established minimum time of follow-up was 24 months, restricting the study group to 17 patients (25 feet). The aetiology of the deformity was 11 patients from lumbar-sacral myelomeningocele sequelae (L4 to the sacral level) and 6 from late sequelae of poliomyelitis.
The mean age at the time of the surgical procedure was 8 years and 5 months, being 5 years and 10 months in the myelomeningocele patients and 14 years in poliomyelitis patients. There were eight females and nine males. Of the 25 feet, there were 13 on the right side and 12 on the left side, with 8 cases being bilateral. Functionally, 12 patients were community walkers, 4 household walkers and 1 non-walker. All patients were using braces.
Surgical indications were to block the excessive ankle dorsiflexion, decrease the retropulsion during gait, prevent skin ulcerations and improve shoe wear. Depending on the needs of each patient, associated procedures were done at the same surgical session (Table 1).
Table 1.
Surgical procedures associated with Westin’s tenodesis
| Associated procedures | Number of feet |
|---|---|
| Osteotomy of the calcaneus | 8 |
| Transfer of the anterior tibial tendon to the calcaneus | 6 |
| Transfer of the short fibular tendon to the calcaneus | 3 |
| Triple arthrodesis of the foot | 2 |
| Subtalar arthrodesis | 1 |
| Talectomy | 1 |
| Steindler | 1 |
| Total | 17 |
Source: M.R.-ISCMSP
Radiographically, the anteroposterior and lateral views of the ankle and foot were done in a weight-bearing position and the axial view of the calcaneus pre- and postoperatively. On the lateral view of the ankle and foot, the tibiocalcaneal angle was measured (normal values: 70–80°) pre- and postoperatively [14].
Clinical and radiographic aspects were considered in the evaluation of results. A satisfactory result comprised gait improvement, better adaptation to shoes or braces, decrease of the retropulsion and the increase of the tibiocalcaneal angle. The subjective opinion of the parents or carers about the results was also recorded as satisfied or unsatisfied.
The mean follow-up period was 6 years and 6 months, with a maximum of 11 years and 8 months, being 6 years and 1 month in the myelomeningocele patients and 7 years and 4 months in the polio patients.
Of the eight bilateral cases, four were operated on at the same and four at separate sessions. All patients were immobilised in short leg casts with ankles in a neutral position for 6 weeks, without weight bearing. After the cast removal, physiotherapy was initiated.
For data analysis, the Pearson correlation coefficient to quantitative variables and Fisher’s test for the qualitative parameters were used with the software EpiInfo 6 v6.04.
Results
Global data analysis demonstrated that, radiographically, there was a mean increase of 15.3° of the tibiocalcaneal angle between the pre- and postoperative measurements; this was statistically significant (P=0.0003).
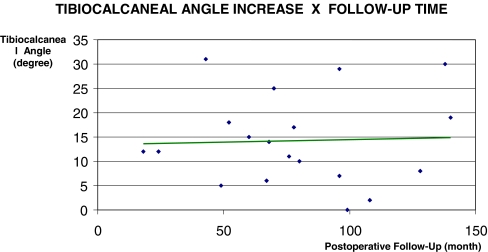
The correlation between the follow-up time and the increase in the tibiocalcaneal angle showed a low correlation coefficient (r=0.04). The dispersion diagram for this analysis presents a horizontal least-squares line (Fig. 1), which means that the increase of the tibiocalcaneal angle is not related to a longer follow-up time.
Fig. 1.
Graph analysis of the tibiocalcaneal angle increase in relation to the postoperative follow-up time in patients with valgus paralytic pes calcaneus treated with the Westin technique
Clinically, 16 patients (94.2%) reported improvement and satisfaction with the treatment. Only one (5.8%) patient’s parents reported being dissatisfied with the results. All patients presented plantigrade feet, with better adaptation to the braces and no footwear complaints after surgery. Concerning retropulsion, 16 patients (94.2%), 23 feet (92%) showed a reduction in retropulsion and only one patient (5.8%), 2 feet (8%), maintained the preoperative condition. Regarding the use of postoperative braces, 15 patients no longer need them and 2 patients continued to wear braces.
If the results were evaluated according to the aetiology, the increase in the tibiocalcaneal angle was significant only for the myelomeningocele patients (P=0.0001) (Table 2) compared to those with polio (P=0.053).
Table 2.
Mean values of the pre- and postoperative tibiocalcaneal angle
| Tibiocalcaneal angle | Degrees |
|---|---|
| Preoperative mean | 53.12 |
| Postoperative mean | 68.04 |
| Mean increase | 15.32 |
Source: M.R.-ISCMSP
In the evaluation of the qualitative results (satisfaction and retropulsion), the Fisher’s test could not distinguish between the two groups because of the small number of patients.
Regarding the complications, there were two cases (8%) with rupture of the tenodesis that were successfully repaired, and there were no other complications. There were no cases of pressure sores or skin problems.
In this group of patients, six had residual deformities requiring other surgical procedures later (Table 3).
Table 3.
Associated procedures to the Westin technique in patients with valgus paralytic pes calcaneus
| Procedures | Number of feet |
|---|---|
| Transfer of the anterior tibial tendon to the calcaneus | 3 |
| Dwyer osteotomy of the calcaneus | 2 |
| Lateral column lengthening (Evans) | 1 |
| Subtalar arthroresis (Pisani technique) | 1 |
| Triple arthrodesis of the foot | 1 |
| Posterior-medial release of the foot | 1 |
| Total | 9 |
Source: M.R.-ISCMSP
Discussion
In 1913, Gallie started the surgical treatment of pes calcaneus using tenodesis of the calcaneal tendon to the tibia in patients with poliomyelitis. Jacobs in 1966 reported three cases treated with the same technique, but did not reach conclusions about the efficacy of the procedure because of the short follow-up period. Neither of these authors mentioned the presence of the ankle valgus or the improvement of the calcaneus deformity [13, 14, 20].
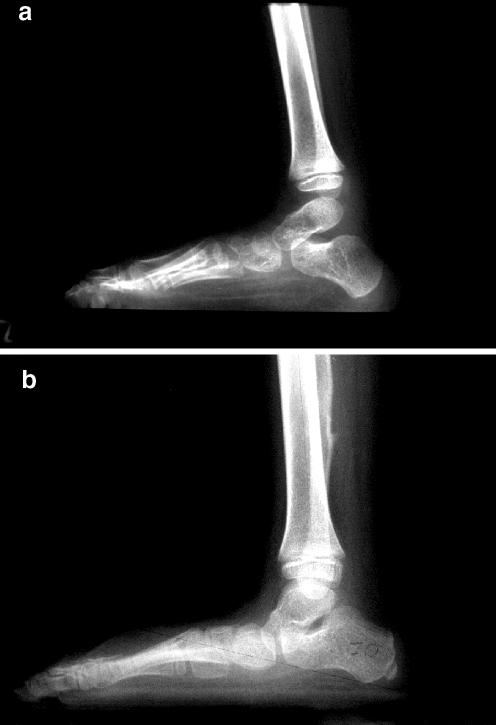
Until 1967, Westin performed tenodesis of the Achilles tendon to the tibia and started to perform the calcanealfibular tenodesis after the observation of a case in which this technique was done inadvertently. Eighteen months postoperatively in this case, he noticed hypertrophy and overgrowth of the fibula epiphysis in addition to the decrease of the retropulsion during gait and the improvement of the vertical calcaneus. In 1988, Westin et al. presented the results of 66 calcaneofibular tenodeses in polio patients with calcaneus-valgus feet. All patients showed clinical and radiographic improvement using the tibiocalcaneal angle as a parameter, but they stressed the possibility of overcorrection or the forthcoming equinus deformity of the foot (38%), especially related to young patients at the time of the surgery. Although the mean age of our myelomeningocele patients was 5 years and 10 months and after a follow-up of a little over 6 years, overcorrection was not found (Figs. 2, 3). No equinus deformity occurred. Although we had two patients with more than 80° of increase of the tibiocalcaneal angle, clinically the results are very similar to the originals from Westin et al. [13, 14].
Fig. 2.
D.S.S., 9-year-old female, myelomeningocele sequelae, right pes calcaneus, radiographic evaluation. a Preoperative; b postoperative
Fig. 3.
M.C.F.S., 15-year-old female, myelomeningocele sequelae, bilateral pes calcaneus, clinical aspects. a Preoperative; b) and c postoperative
We could not find any statistical analysis in the literature concerning the Westin procedure and the increase of the tibiocalcaneal angle with the time of follow-up. In our study, that increase was statistically significant (P=0.0003), but no correlation between the time of follow-up and the increase of the tibiocalcaneal angle was observed.
Figure 1 demonstrates the horizontal least-squares line in the dispersion graph that correlates follow-up time and angle increase, demonstrating a low correlation coefficient between these two parameters. Therefore, the increase in the tibiocalcaneal angle is not related to a longer postoperative follow-up time in our patients.
The radiographic results were statistically significant only for the myelomeningocele patients (P=0.0001). For those with polio, the number was too small (six patients) to compare, but if simulated with nine patients, the results become significant.
Clinical results were not statistically significant, and no difference could be established between the two aetiological groups.
None of the patients in the study showed elongation of the transferred Achilles tendon as reported by Dias [18], who reported this complication in 30% of his patients.
The transfer of the anterior tibial tendon to the calcaneus is the classic option for treating pes calcaneus. This technique has been used as an isolated procedure by several authors with good results, with regard to the decrease of the calcaneus inclination and prevention of the deformity. On the other hand, none of the authors obtained improvement or prevention of the valgus deformity of the ankle [1, 2, 5, 12, 13, 15, 20, 23–25]. It should be remembered that both procedures can be associated, the anterior tibial tendon transfer and the Westin tenodesis, since both have different principles and effects.
Considering only the patients with poliomyelitis, we could not correlate statistically the increase in the tibiocalcaneal angle and the clinical improvement. We demonstrated that all patients were satisfied after the surgical treatment with a better gait and a decrease of the retropulsion. Therefore, our results allow us to recommend the procedure clinical grounds.
Our study showed satisfactory results with the Westin tenodesis, clinically and radiographically, in the myelomeningocele patients, being a good option to treat paralytic pes calcaneus, with no influence of the follow-up time on the results.
References
- 1.Menelaus MB, Barwood SA, Graham HK (1998) In: Menelaus’ orthopaedic management of spina bifida cystica, 3rd edn. WB Saunders Co. Ltd, p 107–127
- 2.Bliss DG, Menelaus MB (1986) The results of transfer of tibialis anterior to the heel in patients who have a myelomeningocele. J Bone Jt Surg Am 68:1258–1264 [PubMed]
- 3.Bradley GW, Coleman SS (1981) Treatment of calcaneocavus deformity. J Bone Jt Surg Am 63:1159–1166 [PubMed]
- 4.Coleman SS (1983) Complex foot deformities in children. Lea & Febiger, pp 167–191
- 5.Fernandez FR, Fernandez SA, Colon C, Ramirez N, Alegria M, Clinton R (1992) Transfer of the tibialis anterior for calcaneus deformity in myelodysplasia. J Bone Jt Surg Am 73:1038–1041 [PubMed]
- 6.Mitchell GP (1977) Posterior displacement osteotomy of the calcaneus. J Bone Jt Surg Br 59:223–235 [DOI] [PubMed]
- 7.Cholmeley JA (1953) Elmslie’s operation for the calcaneus foot. J Bone Jt Surg Br 35:46 [DOI] [PubMed]
- 8.Fraser RK, Hoffman EB (1992) Calcaneus deformity in the ambulant patient with myelomeningocele. J Bone Jt Surg Am 73:994–997 [DOI] [PubMed]
- 9.Frawley PA, Broughton NS, Menelaus MB (1998) Incidence and type of hindfoot deformities in patients with low-level spina bifida. J Pediatr Orthop 18:312–313 [DOI] [PubMed]
- 10.Herndon CH, Strong JM, Heyman CH (1956) Transposition of tibialis anterior in the treatment of paralytic talipes calcaneus. J Bone Jt Surg Am 38:751–760 [PubMed]
- 11.Stevens PM, Toomey E (1988) Fibular-Achilles tenodesis for paralytic ankle valgus. J Pediatr Orthop 8:169–175 [PubMed]
- 12.Stott NS, Zionts LE, Gronley JK, Perry J (1996) Tibialis anterior transfer for calcaneal deformity a postoperative gait analysis. J Pediatr Orthop 16:792–798 [DOI] [PubMed]
- 13.Westin GW (1965) Tendon transfers about the foot, ankle, and hip in the paralyzed lower extremity. J Bone Jt Surg Am 47:1430–1443 [PubMed]
- 14.Westin GW, Dingeman RD, Gausewitz SH (1988) The results of tenodesis of tendon Achilles to the fibula for paralytic pes calcaneus. J Bone Jt Surg Am 70:320–328 [PubMed]
- 15.Beaty LH, Canale ST, Roach JW, Dias LS, Drennan JC, Banta JV, Lubicky JP, Carroll NC, Lindseth RE (1990) Orthopaedic aspects of myelomeningocele. J Bone Jt Surg Am 72:626–630 [PubMed]
- 16.Sharrard WJ (1967) Paralytic deformity in the lower limb. J Bone Jt Surg Br 49:731–747 [PubMed]
- 17.Dias LS (1983) In: Myelomeningocele, orthopaedic treatment. Williams and Wilkins, p 168
- 18.Dias LS (1985) Valgus deformity of ankle joint. Pathogenesis of fibular shortening. J Pediatr Orthop 5:176–180 [PubMed]
- 19.Carrol NC (1987) Assessment and management of the lower extremity in myelodysplasia. Orthop Clin North Am 18:709–724 [PubMed]
- 20.Banta JV, Sutherland DH, Wyatt M (1981) Anterior tibial transfer to the os calcis with Achilles tenodesis for calcaneal deformity in myelomeningocele. J Pediatr Orthop 1:125–130 [DOI] [PubMed]
- 21.Warner WC (2002) In: Campbell’s Operative Orthopaedics, 10th edn. Mosby Inc., pp 1211–1279
- 22.Renington RD, Schork MA (1970) In: Statistics with applications to the biological and health sciences. Prentice Hall Inc., New Jersey, p 418
- 23.Georgiadis GM, Aronson DD (1990) Posterior transfer of the anterior tibial tendon in children who have a myelomeningocele. J Bone Jt Surg Am 72:392–398 [PubMed]
- 24.Hayes JT, Gross HP, Dow S (1964) Surgery for paralytic defects secondary to myelomeningocele and myelodysplasia. J Bone Jt Surg Am 46:1577–1597 [PubMed]
- 25.Jacobs JT (1966) Achilles tenodesis for paralytic calcaneocavus foot. Clin Orthop Rel Res 47:143–149 [PubMed]