Abstract
The phenomenology of childhood and adolescent loss of control (LOC) eating is unknown. The authors interviewed 445 youths to assess aspects of aberrant eating. LOC was associated with eating forbidden food before the episode; eating when not hungry; eating alone; and experiencing secrecy, negative emotions, and a sense of “numbing” while eating (ps < .01). Hierarchical cluster analysis revealed a subgroup, most of whom reported LOC eating. Cluster members reported having a trigger initiate episodes, eating while watching television, and having decreased awareness regarding the amount consumed. The authors conclude that aspects of LOC eating during youth are similar to aspects of adult episodes, but a youth-specific presentation may exist. Findings may provide an intervening point to prevent excessive weight gain and eating disorders.
Keywords: binge eating, loss of control eating, children, adolescents
The prevalence of pediatric overweight has nearly tripled in recent years (Ogden et al., 2006). Overweight during youth puts individuals at high risk for becoming obese adults (Field, Cook, & Gillman, 2005; Freedman, Khan, Dietz, Srinivasan, & Berenson, 2001; Freedman et al., 2004; Guo, Wu, Chumlea, & Roche, 2002; Whitaker, Wright, Pepe, Seidel, & Dietz, 1997; Williams, 2001). Given the serious untoward medical (Adams et al., 2006; Freedman et al., 2001) and psychosocial (Puhl & Brownell, 2002; Strauss & Pollack, 2003) consequences of excess weight, overweight during childhood and adolescence is a major public health problem. Prevention and early intervention are critical to reduce the current epidemically high prevalence of pediatric overweight (Styne, 2003). Targeting behavioral factors that promote excessive weight gain may be a potential point of intervention. However, clarification of relevant behavioral factors is required before prevention efforts may be designed and implemented.
Binge eating is defined as eating a large amount of food given the context, during which a sense of lack of control over eating is experienced (American Psychiatric Association [APA], 2000). Recurrent binge eating is the hallmark behavior of binge eating disorder BED; (APA, 2000). Compared to obese adults without an eating disorder, adults with BED suffer from poorer physical health (J. G. Johnson, Spitzer, & Williams, 2001) and higher levels of eating disorder psychopathology (e.g., Masheb & Grilo, 2000; Wilfley et al., 2000) and are more likely to be diagnosed with a comorbid psychiatric disorder (e.g., Marcus, 1995; Wilfley et al., 2000; Yanovski, Nelson, Dubbert, & Spitzer, 1993). BED and subthreshold binge eating are often associated with excess body weight and obesity (de Zwaan, 2001; Yanovski et al., 1993). Not only is BED a disorder of clinical significance (Wilfley, Wilson, & Agras. 2003), but some (Sherwood, Jeffery, & Wing, 1999; Yanovski, Gormally, Leser, Gwirtsman, & Yanovski, 1994), although not all (Wadden, Foster, & Letizia, 1992), data suggest that the presence of the disorder may complicate weight loss treatment.
Binge eating, even at a subthreshold frequency, appears to be common among children (e.g., Lamerz et al., 2005; Tanofsky-Kraff et al., 2004) and adolescents (e.g., Glasofer et al., 2007; Greenfeld, Quinlan, Harding, Glass, & Bliss, 1987); prevalence estimates range from approximately 2% to 40%. Also common are reports of eating episodes during which youths experience a loss of control over their eating without consuming an unambiguously large amount of food. Studies of overweight children (Decaluwe & Braet, 2003; Morgan et al., 2002; Tanofsky-Kraff, Faden, Yanovski, Wilfley, & Yanovski, 2005) and adolescents (Berkowitz, Stunkard, & Stallings, 1993; Glasofer et al., 2007; Isnard et al., 2003) have generally found that those who report loss of control eating1 episodes, with or without unambiguously large amounts of food, have greater eating-related distress, anxiety, and depressive symptomatology and poorer self-esteem than those who do not report such episodes. Even in community-based samples, youths reporting loss of control eating are heavier and more likely to manifest disordered eating cognitions; depressive symptoms, poorer family and social functioning, and emotional stress than those without binge eating (e.g., French et al., 1997; W. G. Johnson, Rohan, & Kirk, 2002; Ledoux, Choquet, & Manfredi, 1993; Neumark-Sztainer & Hannan, 2000; Steiger, Puentes-Neuman, & Leung, 1991; Tanofsky-Kraff et al., 2004).
Loss of control eating may also promote inappropriate weight gain and thus may be a factor contributing to the current high prevalence of pediatric overweight (Ogden et al., 2006). Several prospective studies have documented that binge eating is predictive of excessive weight gain among adolescents (Field et al, 2003; Stice, Cameron, Killen, Hayward, & Taylor, 1999; Stice, Presnell, & Spangler, 2002) and of fat gain among children at high risk for adult obesity (Tanofsky-Kraff et al., 2006). The excess energy intake frequently associated with binge eating, along with the absence of compensatory behaviors, may serve as a mechanism for inappropriate weight gain, contributing to the development of obesity in at-risk children and adolescents.
Despite the substantial prevalence of loss of control eating episodes and a literature indicating accompanying psychosocial problems, the conceptualization of loss of control eating among youths has not been fully elucidated. In a community sample of adolescent boys and girls, Neumark-Sztainer and Story (1998) conducted focus groups to gain insight into how teens define the term binge eating. Without offering participants any information regarding the definition of binge eating, the authors found that responses were often unrelated to adult conceptualizations of binge eating, and almost 50% of the teen participants indicated that they were unfamiliar with or misunderstood the term (Neumark-Sztainer & Story, 1998). The authors concluded that self-reports of binge eating should be interpreted with caution and that when they are assessing eating patterns, researchers should identify specific behaviors. The results of other studies bolster this conclusion. A study of 7- to 13-year-old girls found that younger children were more likely than were older girls to report binge episodes (Maloney, McGuire, Daniels, & Specker, 1989). The authors speculated that this unexpected finding might have been due to a misunderstanding of the term binge on the part of the younger participants. Finally, multiple studies among both preadolescent and adolescent children have indicated that the presence of loss of control eating behaviors assessed via self-report measures is not concordant with the presence as assessed by interview methods (Decaluwe & Braet, 2004; Field, Taylor, Celio, & Colditz, 2004; Tanofsky-Kraff et al., 2003), suggesting that the construct of loss of control eating is not well defined or interpreted. Although structured interviews are often considered the optimal means of assessing disordered eating (Bryant-Waugh, Cooper, Taylor, & Lask, 1996; Kashubeck-West, Mintz, & Saunders, 2001; Wilfley, Schwartz, Spurrell, & Fairburn, 1997), the available methods do not systematically define the specific constructs or provide developmentally appropriate, in-depth instructions to clarify the behaviors and attitudes associated with aberrant eating.
To elucidate the construct of loss of control eating, we aimed to improve on previous studies by systematically assessing eating episodes among children and adolescents. Our overarching goal was to understand the characteristics and salience of binge and loss of control eating in children and adolescents. As recommended by Neumark-Sztainer and Story (1998), our assessment involved identifying specific constructs potentially associated with aberrant eating episodes, such as the context (e.g., eating alone) or the emotional experience (e.g., eating in response to negative affect). In doing so, we aimed to demonstrate convergent validity between loss of control eating and constructs (see the examples above) presumed to be associated with such behavior.
Developmental models of emotional regulation suggest that affect plays a central role in dysfunctional behavior (Eisenberg & Fabes, 1992). Indeed, data indicate that children prone to high emotion and low self-regulation tend to exhibit externalizing problem behaviors (e.g., Eisenberg et al., 1997, 2000). Although this model has not been utilized to examine disinhibited eating in children and adolescents specifically, adult theories suggest that binge eating occurs in response to negative emotional states (e.g., Heatherton & Baumeister, 1991; Leon, Fulkerson, Perry & Early-Zald, 1995). In describing the development of disordered eating in primarily healthy weight adolescent and young adult girls, Stice (2002) has hypothesized that overweight may lead to increased pressure to be thin, which may be experienced through negative feedback from others. In turn, body dissatisfaction ensues, and a cycle of negative affect, dieting, and binge eating manifests (Stice, 2002). Slice’s model may provide a link between developmental models and adult theories such that a potential mechanism for the relationship between negative emotions and loss of control eating in children and adolescents may be postulated: Overweight youths with high emotion and low self-regulation may be especially sensitive to negative feedback from parents and peers and, therefore, have a heightened experience of adverse affective states. Such youths may be at especially high risk for loss of control eating as an attempt to avoid experiencing negative emotions. A necessary first step in trying to further understand the nature of this relation is to systematically explore and describe loss of control eating and behavioral, physical, and emotional constructs surrounding such eating episodes in a large sample of primarily overweight children and adolescents. Furthermore, because no study has examined pediatric loss of control eating by directly comparing preadolescent (e.g., less than 12 years) to adolescent (12 to 18 years) youths or comparing boys and girls, an exploration of potential age and gender differences is warranted.
We hypothesized that children and adolescents with loss of control eating would endorse eating in response to negative emotions and other documented characteristics of adult binge episodes: experiencing negative affect during and after eating, eating alone and in secrecy during the episodes, eating following dietary restriction, and eating rapidly or when not hungry. Because of the high prevalence of BED among obese adults seeking weight loss treatment, we also hypothesized that participants seeking weight loss treatment would be most likely to endorse loss of control eating characterized by the above constructs. Finally, drawing on the literature on adults with BED (e.g. Wilfley et al., 2003) and children with loss of control eating (e.g., Tanofsky-Kraff et al., 2004), we posited that participants who clustered together on the basis of such constructs would be heavier and more likely to experience disordered eating attitudes and cognitions compared to children who did not cluster together. To test these hypotheses in a large and diverse cohort, we carried out a multisite investigation of children’s and adolescents’ loss of control eating behaviors.
Method
Participants
Participants were children and adolescents (8–18 years) participating in nonintervention protocols or weight loss treatment studies at five research institutions between January 2004 and August 2006. For nonintervention protocols, none of the participants was undergoing weight loss treatment, and all were aware that they would not receive treatment as part of the study protocols. All youths participating in weight loss research studies were overweight (i.e., body mass index [BMI], in kilograms per square meter, of at least the 95th percentile for age and sex) or at risk for overweight (85th percentile ≥ BMI < 95th percentile for age and sex; Ogden et al., 2002) and were assessed prior to the initiation of treatment. None of the participants had developmental syndromes or delays that would preclude accurate completion of study assessments or were taking medication affecting body weight. Details regarding each location of data collection are described in the following paragraphs.
National Institute of Child Health and Human Development (NICHD)
Two groups were enrolled: overweight and nonoverweight children and adolescents (8–17 years) participating in nonintervention, metabolic studies, and adolescents (12–17 years) being assessed for a weight loss intervention study. Nonintervention participants were recruited through posted flyers; mailings to parents in the Montgomery County and Prince George’s County, Maryland, school districts; and mailings to local family physicians and pediatricians. These letters and flyers requested children and adolescents willing to participate in studies investigating hormones and growth in youths. Participants had been medication free for at least 2 weeks prior to being studied, and none had significant medical disease. Each child or adolescent had normal hepatic, renal, and thyroid function. Additional details have been reported elsewhere (Tanofsky-Kraff et al., 2004). Participants drawn from the weight loss study protocol were overweight African American and Caucasian adolescents with at least one obesity-related medical comorbidity (ClinicalTrials.gov, 2005). Recruitment and inclusion and exclusion criteria for this study have been reported (McDuffie et al., 2002).
University of Ghent
All participants (8–18 years) were overweight. Youths either were, initiating weight loss at a residential treatment program (Het Zeepreventorium, in De Haan, Belgium) or were recruited through magazine advertisements in the Ghent, Belgium, area for nonintervention studies. Advertisements requested individuals interested in participating in a study investigating excess weight gain in childhood and adolescence.
Boston University
Children and adolescents (8–18 years) who were participants in a weight loss study through the Optimal Weight for Life clinic at the Children’s Hospital Boston were enrolled. Inclusion and exclusion criteria have been described elsewhere (Glasofer et al., 2007).
University of Pittsburgh Medical Center
Children (8–12 years) were recruited from advertisements in local newspapers and letters sent to local physicians as part of a larger study soliciting mothers of overweight children. None of the mothers was actively seeking weight loss treatment for her children. Flyers were also posted throughout the Pittsburgh area, and advertisements were made on the local hospital voicemail system, in the hospital newsletter, and in two public service announcements.
Washington University in St. Louis
Adolescents (12–17 years) were recruited as part of a study examining an Internet-based weight control program. Inclusion, exclusion, and recruitment procedures have been reported (Doyle, le Grange, Goldschmidt, & Wilfley, 2007).
For all sites, participants received written explanations of the purposes, procedures, and potential hazards of the study prior to participation. Children and adolescents provided written assent, and parents gave written consent for participation. All protocols were approved by the institutional review board at each respective site.
Measures
The Eating Disorder Examination Version 12OD/C.2 EDE; (Fairburn & Cooper, 1993)
The EDE or the EDE adapted for children (Bryant-Waugh et al., 1996) was administered to each participant to assess aberrant eating. Interviewers underwent extensive training in the administration of the EDE and in the development of positive rapport with children and adolescents. The EDE’s interview-based, interactive nature allows for questions to be explained so that they are understood by each individual and so that age-related developmental differences may be addressed. Special care is taken, and examples are provided, to explain concepts such as loss of control, or the sense of being unable to stop eating once started. For example, when a participant does not readily understand the concept of loss of control, one of the standardized descriptions used is that the experience is “like a ball rolling down a hill, going faster and faster” (Tanofsky-Kraff et al., 2004, p. 55). Interviewers were trained centrally on the administration of the EDE so that the construct of loss of control eating was systematically elucidated for all participants.
On the basis of their responses to the EDE, participants were categorized as engaging in objective binge episodes (OBEs; overeating with loss of control), subjective binge episodes (SBEs; loss of control without objective overeating as assessed by the interviewer but viewed as excessive by the interviewee), objective overeating (OO; overeating without loss of control), or no episode (NE; a normal meal involving neither loss of control nor overeating) over the 28 days prior to assessment. Children and adolescents who engaged in more than one type of episode were categorized by the most pathological eating behavior described (Tanofsky-Kraff et al., 2004). OBEs were considered the most pathological, with SBEs and OOs following, respectively. NEs were the least pathological episodes for the purposes of this study. The child version differs from the adult EDE only in that its script has been edited to make it more accessible to children ages 8–14 years. Both versions generate the same four subscales: Dietary Restraint (cognitive and behavioral restriction), Eating Concern, Shape Concern, and Weight Concern, which average to create a global score.
The EDE has good internal consistency ratings, with subscale alphas ranging from .68 to .90 (Cooper, Cooper, & Fairburn, 1989), test-retest reliability with correlations of at least .70 for all subscales, and interrater reliability for all episode types (Spearman correlation coefficients of at least .70; Rizvi, Peterson, Crow, & Agras, 2000). In a sample of overweight adolescents, the EDE has shown excellent interrater reliability, with intraclass correlations ranging from .87 to .98 on the subscale and total scores (Glasofer et al., 2007). However, in one study of women with anorexia nervosa, the EDE Dietary Restraint subscale did not correlate with unobtrusively measured energy intake (Sysko, Walsh, Schebendach, & Wilson, 2005), which suggests that this scale may not be a valid indicator of actual caloric restriction. Tests of the EDE adapted for children have demonstrated good internal consistency (Cronbach’s alphas for subscales from .80 to .91), interrater reliability (Spearman rank correlations from .91 to 1.00), and discriminant validity in eating disordered samples and matched controls ages 8–14 years (Watkins, Frampton, Lask, & Bryant-Waugh, 2005). Among samples of healthy and overweight 6- to 13-year-olds (Tanofsky-Kraff et al., 2004), the child version of the EDE revealed excellent interrater reliability (intraclass correlation) for subscales (from .95 to .99, all ps < .001), and Cohen’s kappa for presence of the different eating episode categories was 1.00 (p < .001).
The Dutch version of the EDE adapted for children (Decaluwe & Braet, 2003) was designed for use in populations of Dutch youths following the recommendations of the originators of the EDE (Fairburn & Cooper, 1993) and the child version (Bryant-Waugh et al., 1996). Similar to the English version, metaphors are used to explain the construct of loss of control over eating and to ensure that: children understand the terminology. The Dutch child EDE has demonstrated excellent interrater reliability for all four subscales (correlations ranging from .91 to .99) and adequate test-rest reliability (ranging from .61 to .83; Decaluwe & Braet, 2004).
Standard Pediatric Eating Episode Interview (SPEEI)
The SPEEI was developed based upon our collective clinical experience and research in the area of pediatric overweight and disordered eating behaviors. The measure was designed and piloted during fall 2003. We compiled an exhaustive list of contextual, behavioral, physical, and emotional aspects of described eating episodes from prior work (Goossens, Braet, & Decaluwe, 2007; Levine, Ringham, Kalarchian, Wisniewski, & Marcus, 2006; Tanofsky-Kraff et al., 2004). From this list, we coded descriptions into the standardized subgroups listed in Table 1. As with the EDE, interviewers were trained centrally to provide assurance that children and adolescents understood the questions and that the constructs were accurately explicated. The SPEEI was administered following the overeating section of the EDE, and the questions were asked with regard to one episode per participant, as described above. For participants in Belgium, the interview was translated into Dutch by Lien Goossens and Caroline Braet. For most queries surrounding the behavior and physical context, a direct translation from English to Dutch was readily made. Translation of the emotional query “numb out” required discussions among sites until there was consensus that the translated terms were accurately capturing the construct.
Table 1.
Percentage of Standard Pediatric Eating Episode Interview Questions Endorsed by Eating Episode Type
| Episode type | OBE (n = 106) | SBE (n = 67) | OO (n = 106) | NE (n = 166) | χ2 | df | N | Effect size |
|---|---|---|---|---|---|---|---|---|
| Before eating episode | ||||||||
| Contextual: Meal type | ||||||||
| Breakfast | 4.7 | 6.0 | 3.8 | 3.7 | 40.3** | 12 | 442 | .18 |
| Luncha | 19.9 | 14.9 | 24.8 | 31.7 | ||||
| Dinner | 46.2 | 46.3 | 58.1 | 58.5 | ||||
| Snack | 29.2 | 32.8 | 13.3 | 6.1 | ||||
| Behavioral: Overeaten/eaten forbidden food | ||||||||
| Yes | 10.4 | 13.4 | 1.0 | 0.6 | 27.4** | 3 | 444 | .25 |
| Emotional: Emotion present | ||||||||
| Yes–negative | 32.1 | 23.9 | 10.4 | 5.4 | 38.6** | 6 | 445 | .21 |
| Yes–positive | 26.4 | 31.3 | 34.0 | 34.3 | ||||
| Behavioral: Restricting prior | ||||||||
| Yes | 22.6 | 22.4 | 16.0 | 16.9 | 2.6 | 3 | 445 | .08 |
| Emotional: Trigger | ||||||||
| Yes | 14.2 | 13.4 | 12.3 | 5.4 | 6.6 | 3 | 445 | .13 |
| Physical: Hungry | ||||||||
| Yes | 88.7 | 76.1 | 84.9 | 81.9 | 6.3 | 3 | 445 | .11 |
| Behavioral: Eating despite a lack of hunger | ||||||||
| Yes | 61.2 | 59.7 | 44.3 | 17.1 | 70.0** | 3 | 440 | .39 |
| Physical: Tired | ||||||||
| Yes | 36.8 | 34.3 | 27.4 | 21.1 | 8.2* | 3 | 445 | .14 |
| During eating episode | ||||||||
| Contextual: With whom | ||||||||
| Family | 63.8 | 55.2 | 67.6 | 72.6 | 20.8** | 6 | 441 | .17 |
| Friends | 14.3 | 23.9 | 26.7 | 20.1 | ||||
| Alone | 21.9 | 20.9 | 5.7 | 7.3 | ||||
| Contextual: Time of day | ||||||||
| Morning (until noon) | 5.7 | 10.4 | 4.7 | 7.3 | 15.4 | 12 | 443 | .11 |
| Afternoon (until 5 pm) | 38.7 | 28.4 | 37.7 | 34.8 | ||||
| Evening (until going to bed) | 50.9 | 61.2 | 56.6 | 57.3 | ||||
| Nocturnal (after going to bed) | ||||||||
| All day | 1.9 | 0.0 | 0.0 | 0.0 | ||||
| 2.8 | 0.0 | 0.9 | 0.6 | |||||
| Contextual: Celebration | ||||||||
| Yes | 29.2 | 23.9 | 36.8 | 27.4 | 4.0 | 3 | 443 | .10 |
| Emotional: Secretive | ||||||||
| Yes | 22.9 | 17.9 | 4.7 | 1.8 | 38.6** | 3 | 444 | .30 |
| motional: “Numbing” | ||||||||
| Yes | 30.2 | 34.3 | 6.6 | 5.4 | 46.7** | 3 | 445 | .35 |
| Contextual: Hiding food | ||||||||
| Yes | 13.2 | 4.5 | 2.8 | 1.2 | 18.4** | 3 | 442 | .22 |
| Behavioral: Eating quickly | ||||||||
| Yes | 47.6 | 31.3 | 28.3 | 13.3 | 43.1** | 3 | 444 | .30 |
| Behavioral: Amount compared to others | ||||||||
| More | 49.1 | 35.9 | 31.1 | 14.5 | ||||
| Less | 6.6 | 14.1 | 10.4 | 25.5 | 57.8** | 12 | 441 | .22 |
| same | 17.9 | 25.0 | 32.1 | 37.6 | ||||
| Middle (some more/some less) | 10.4 | 9.4 | 17.9 | 13.3 | ||||
| Unsure | 16.0 | 15.6 | 8.5 | 9.1 | ||||
| Contextual: Where | ||||||||
| Home | 47.2 | 38.8 | 32.4 | 49.1 | 32.5** | 12 | 439 | .17 |
| Watching televisionb | 7.5 | 16.5 | 2.9 | 1.9 | ||||
| Restaurant | 17.0 | 16.4 | 33.3 | 20.5 | ||||
| Other home | 18.9 | 13.4 | 13.3 | 17.4 | ||||
| Other | 9.4 | 14.9 | 18.1 | 11.1 | ||||
| After eating episode | ||||||||
| Emotional: Emotion present | ||||||||
| Yes–negative | 40.6 | 38.8 | 15.1 | 7.8 | 53.5** | 6 | 445 | .25 |
| Yes–positive | 3.8 | 1.5 | 6.6 | 3.0 | ||||
| Emotional: Guilt/shame | ||||||||
| Yes | 49.1 | 47.8 | 17.0 | 16.9 | 46.2** | 3 | 445 | .34 |
| Physical: Full | ||||||||
| Yes | 84.0 | 89.6 | 92.5 | 91.0 | 5.2 | 3 | 445 | .10 |
| Physical: Sick | ||||||||
| Yes | 34.0 | 26.9 | 23.6 | 14.5 | 11.6** | 3 | 445 | .18 |
Note. OBE = objective binge episode; SBE = subjective binge episode; OO = objective overeating; NE = no episode.
Two participants who reported that their episode was a brunch meal were included with the lunch group.
Participants were coded as watching television whether they were doing so in their own home or in another location.
p < .05.
p < .01.
Weight and height were measured with calibrated instruments at all sites. To standardize BMI across samples, we calculated BMI standard deviation scores (BMI z scores) according to the Centers for Disease Control and Prevention 2000 standards (Kuczmarski et al., 2002). Children and adolescents with a BMI z score of equal to or greater than 1.64 (95th percentile) were identified as overweight.
Procedure
Data were collected at a baseline visit at each site. All sites except NICHD administered the child version of the EDE regardless of age. At NICHD, adolescents (12–17 years) initiating weight loss treatment and nonintervention participants who were 14 years or older completed the standard EDE. Participants younger than 14 years in nonintervention studies were administered the child version.
At NICHD, SPEEI data were collected from all children and adolescents entering the study. At other sites, SPEEI data were obtained from participants who endorsed OBEs, SBEs, and OOs during the 1st year of data collection; subsequently, all sites queried children and adolescents describing NEs. For all sites, none of the data obtained from the SPEEI have been previously published. EDE data from Ghent and from Pittsburgh have never been published. Data from the EDE were previously published for 13 participants from the NICHD sample (Theim et al., 2007) and for all children from the Boston cohort (Eddy et al., 2007) and the St. Louis site (Doyle et al., 2007).
Data Analytic Plan
Analyses were conducted with SPSS for Windows 12.0 (SPSS, Inc., 2004). To determine convergent validity between loss of control eating and constructs proposed to describe such episodes, we used Cochran-Mantel-Haenszel summary chi-square statistics to determine the frequency of endorsed probes for each episode type (OBE, SBE, OO, and NE), stratified by location. The Cochran-Mantel-Haenszel method adjusts for site effects by estimating associations separately for each site and combining estimates of association across sites using a weighted average (Agresti, 1990). Cochran-Mantel-Haenszel statistics were calculated in SAS for Windows Version 9.0 (SAS Institute, 2003). Measures of effect size are expressed as Cramer’s V.
Episodes were clustered on the basis of episode characteristics via a hierarchical clustering algorithm (Clatworthy, Buick, Hankins, Weinman, & Horne, 2005; Hand, 1981; Krishnaiah & Kanal, 1982). The cluster analysis is identified as a method
to group entities on the basis of their similarity with respect to selected variables, so that the members of the resulting groups are as similar as possible to others within their group and as different as possible to those in other groups. (Clatworthy et al., 2005, p. 330)
Similarity between episodes was calculated with the squared Euclidean distance measure for binary data (computed as the number of discordant cases). Clusters were joined via the within-group average linkage method, which calculates mean distance between all possible inter- or intracluster pairs. Clusters are defined to make the average distance between all pairs in the cluster as small as possible. The number of clusters to retain was determined by examination of a scree plot. If further examination of the cluster characteristics revealed no meaningful differences between two clusters (e.g., the only difference was breakfast vs. lunch), the clusters were combined. The data file was split several ways, and analysis of each subgroup found a meaningful three- or four-cluster solution with one cluster representing some form of disordered eating, lending confidence to the validity of the clusters.
One-way analyses of variance were used to compare cluster subgroups on the EDE subscales and global score and BMI z score. Covariates considered were age, sex, race, socioeconomic status, and treatment status. For the EDE scores, BMI z score was also considered. Site was included as a random effect in each model. Age, race, and socioeconomic status did not significantly contribute to any model and were therefore removed. After we adjusted for other variables, site-to-site variability was minimal, so the site random effect was also removed. For two-group comparisons, effect size was expressed as a correlation, and for comparisons greater than two groups, effect size was expressed as eta-squared. Means reported were adjusted for covariates given where appropriate. Differences and associations were considered significant when significance values were less than or equal to .05.
Seventy-three participants (10 from Ghent, 38 from Boston, 22 from Pittsburgh, and 3 from St. Louis) with NEs were not administered the SPEEI during the 1st year of the study and were thus not included in the present study. Few differences were found between participants with NEs who were administered the SPEEI and those who were not. After site was accounted for, no differences were found with regard to age, sex, or BMI z score between children with NEs who were and were not administered the SPEEI. However, compared to NE participants who were queried, those who were not queried were more likely to be participating in a weight loss treatment study, 37.3% versus 69.9%; χ2(3, N = 239) = 6.9, p = .01.
Results
Data were collected from 445 children and adolescents (M = 13.1 years, SD = 2.6); 195 were participants from Bethesda, Maryland; 114 were from Ghent, Belgium; 81 were from Boston, Massachusetts; 47 were from Pittsburgh, Pennsylvania; and 8 were from St. Louis, Missouri. Seventy percent (n = 312) of the sample was overweight (BMI z score ≥ 1.64). Of the overweight children and adolescents, 189 (60.6%) were initiating weight loss treatment. Participant demographics by site are described in Table 2.
Table 2.
participant Demographics by Site
| Variable | Bethesda, MD (n = 195) | Ghent, Belgium (n = 114) | Boston, MA (n = 81) | Pittsburgh, PA (n = 47) | St. Louis, MO (n = 8) |
|---|---|---|---|---|---|
| Mean (SD) age in years | 14.0 (2.5) | 14.0 (2.6) | 12.1 (2.3) | 10.4 (1.4) | 14.5 (1.9) |
| Gender (% female) | 56.9 | 66.7 | 53.1 | 68.1 | 75.0 |
| Race (%) | |||||
| African American | 29.7 | 0.0 | 28.4 | 40.4 | 37.5 |
| Asian | 3.1 | 0.0 | 1.2 | 0.0 | 0.0 |
| Caucasian | 60.0 | 100.0 | 60.0 | 59.6 | 62.5 |
| Hispanic | 1.5 | 0.0 | 9.9 | 0.0 | 0.0 |
| Other | 5.6 | 0.0 | 0.0 | 0.0 | 0.0 |
| Median SES a | 2 | 4 | 3 | 4 | 3 |
| Mean (SD) BMI z-score | 1.3 (1.2) | 2.1 (0.4) | 2.4 (0.3) | 2.1 (0.4) | 2.1 (0.5) |
| Overweight (%) | 46.2 | 85.1 | 96.3 | 87.2 | 75.0 |
| treatment seeking (%) | 14.9 | 70.2 | 100.0 | 0.0 | 100.0 |
Note. SES = socioeconomic status; BMI = body mass index.
Socioeconomic status was measured by the Hollingshead (1975) index. Lower scores on a scale of 1 to 5 indicate higher SES.
Twenty-four percent of participants reported OBEs, 15% endorsed SBEs, 24% described OOs, and 37% reported NEs. Groups did not differ with regard to sex, χ2(3, N = 445) = 2.0, p = .56; race, χ2(3, N = 445) = 3.6, p = .31; or socioeconomic status, F = 0.6, p = .65. Youths with OOs (M = 14.0 years, SD = 2.3) were significantly older than those reporting SBEs (M = 12.3 years, SD = 2.8) and NEs (M = 13.0 years, SD = 2.5), F(3, 444) = 6.3, p < .01. After sex and treatment status were controlled, OBE youths (BMI z score, M = 2.0, SD = 0.7) were heavier than participants with OOs (M = 1.6, SD = 1.0) or NEs (M = 1.6, SD = 1.1), and SBE youths (M = 2.0, SD = 0.7) were heavier than participants with NEs, F(3, 427) = 4.8, p < .01; η2 = .03. Those with OBEs were more likely to be involved in a weight loss treatment study than those in other groups, OBE = 58.5%, SBE = 34.3%, OO = 48.1%, NE = 37.3%; χ2(3, N = 445) = 15.2, p < .01.
On the basis of data from the EDE, the prevalence and frequency of compensatory behaviors were low. Twenty-four participants (5.4%) reported engaging in a compensatory behavior at least one time over the past month, 10 of whom also reported OBEs. The most commonly reported behavior was excessive exercise (n = 19), with an average, of 4.1 (SD = 3.4) episodes in the past month. Four participants reported self-induced vomiting in the past month, with a mean of 3.1 (SD = 2.4) episodes. Only 1 participant met criteria for bulimia nervosa (through use of appetite suppressants). All results remained the same when this participant was removed from the data set.
Of the 445 children and adolescents who completed the SPEEI, 95% of cases had complete data. Among the 28 incomplete cases, the most common missing data were where the episode took place, the amount of food the participant consumed compared to others, and with whom the participant was eating. Compared to cases with complete data, those with missing data had significantly lower scores on the EDE Eating Concern subscale (M = 0.46, SD = 0.68, vs. M = 0.25, SD = 0.34, respectively, p = .01) and were more likely to be participants from NICHD (n = 15) than Ghent (no missing data; p = .03). Only participants with complete data were included in the cluster analyses since all variables from the SPEEI are nominal, thus precluding the use of normal-theory-based likelihood methods for imputation of missing data. Furthermore, when cluster analyses are used, it is assumed that the population consists of heterogeneous subgroups that have not been identified, so the appropriate subgroup for calculating summary statistics is unknown. Although one method for using all available data has been described for cluster analyses (Everitt, Landau, & Leese, 2001), this approach is not clearly superior to excluding data and was less robust when applied to the present data set.2 However, as a conservative measure, we included the participants with missing data in the nonclustered sample for the analyses of variance.
Convergent Validity of Binge and Loss of Control Eating
Significant differences among responses were revealed on the basis of episode type (see Table 1). Compared to youths endorsing OO and NE, greater percentages of participants with OBEs and SBEs reported that the episode began after consumption of a “forbidden” food, χ2(3, N = 444) = 27.4, p < .01; that they experienced a negative emotion before eating, χ2 (6, N = 445) = 38.6, p < .01; that they ate despite a lack of hunger, χ2(3, N = 445) = 70.0, p < .01; and that the episode was a snack as opposed to a meal, χ2(12, N = 442) = 403, p < .01. These individuals also were more likely to report eating alone, χ2(6, N = 442) = 20.8, p < .01; and experiencing secrecy regarding eating, χ2 (3, N = 444) = 38.6, p < .01. Furthermore, participants with OBEs and SBEs were more likely to endorse experiencing a sense of “numbing out” while eating, χ2(3, N = 445) = 47.7, p < .01. After eating, greater percentages of youths with OBEs and SBEs reported experiencing a negative emotion, χ2(6, N = 445) = 53.5, p < .01; including feelings of shame and guilt, χ2(3, N = 445) = 46.2, p < .01. Compared to all other groups, youths describing OBEs were more likely to report hiding the food being eaten, χ2(3, N = 442) = 18.4,p < .01; eating quickly, χ2(3, N = 444) = 43.1, p < .01; eating more food than others, χ2(12, N = 441) = 57.8, p < .01; and feeling physically sick after the meal, χ2(3, N = 445) = 11.6, p < .01. SBE participants were more likely to eat while watching television compared to other groups, χ2(12, N = 439) = 38.2, p < .01.
Hierarchical cluster analysis revealed a small but cohesive subgroup of participants (3% of the sample; n = 15), 87% of whom had reported engaging in an OBE or SBE (disordered eating cluster; see Table 3). Five participants from the cluster were from NICHD, 5 were from Ghent, 4 were from Boston, and 1 was from Washington University. Most (87%) were adolescents (ages 12.7–17.7 years). Behaviors that were reported by this group included having an event (e.g., an argument) trigger the episode, eating alone, and eating while watching television. Additionally, the disordered eating cluster described the episode as a snack and reported eating despite a lack of hunger, experiencing secrecy and a sense of numbing out while eating, and experiencing negative emotions before and after eating, including feelings of shame and guilt. The disordered eating cluster also reported being unsure of how much they were eating. Seventy-five percent of these youths were participating in a weight loss treatment study, 80% were overweight, 80% were female, and 93% were Caucasian. According to their EDE interviews, 47% (95% confidence interval = 21%–73%) of these participants met full or subthreshold frequency criteria (on average, at least four OBEs or eight SBEs per month) for Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; APA, 2000) BED, compared to 6% (95% confidence interval = 4%–9%) for the rest of the sample (p < .001, Fisher’s exact test). After the contributions of sex, BMI z score, and treatment status were accounted for, compared to the rest of the sample, the disordered eating cluster had greater EDE Eating Concern, F(l, 444) = 8.2,p < .01, r = .34; Shape Concern, F(2,444) = 3.9,p = .05, r = .31; and global, F(l, 445) = 5.8, p < .05, r = .31, scores than the rest of the sample (see Figure 1). However, no differences were found with regard to EDE Dietary Restraint, F(1, 427) = 1.1, p = .3, r = .20; or Weight Concern, F(1, 426) = 1.8, p = .2, r = .23, subscales (see Figure 1). BMI z scores did not differ between the disordered eating cluster group (BMI z score, M = 1.8, SD = 0.60) and the rest of the participants (BMI z score, M = 1.8, SD = 0.96), F(1, 427) = 0.0, p = 1.0, r = .10.
Table 3.
Common Factors Among Disordered Eating Cluster (n =15)
| Loss of control eating (OBEs or SBEs) associated with some or all of the following: | |
| 1. | Eating following negative emotions and/or a triggering event |
| 2. | Eating despite a lack of hunger |
| 3. | Eating occurs during or is initiated by a snack |
| 4. | Eating alone, in some cases while watching television |
| 5. | Feelings of secrecy with regard to episode |
| 6. | A sense of “numbing” while eating and being unsure of how much food is being ingested |
| 7. | Negative emotions following eating, specifically shame and guilt |
Note. OBE = objective binge episode; SBE = subjective binge episode.
Figure 1.
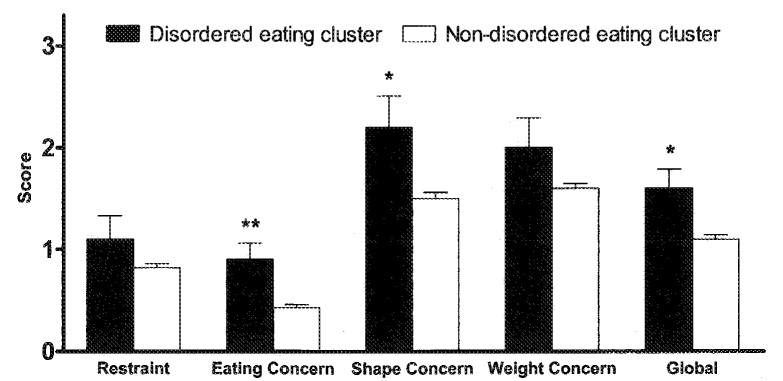
Eating Disorder Examination subscales and global score by disordered eating cluster (n = 15) and nondisordered eating (n = 430) cluster. Error bars represent standard errors of the mean, *p ≤ .05. **p < .01.
Post Hoc Analyses by Age, Sex, and Treatment Status
The data were analyzed separately for younger (12 years or younger; n = 156) and older (older than 12 years; n = 289) participants. On the basis of chi-square analyses, compared to younger children reporting OOs and NEs, younger children with OBEs and SBEs were more likely to report the following behaviors with regard to their episodes: eating despite a lack of hunger, χ2(3, N = 156) = 29.5, p < .01; eating quickly, χ2(3, N = 152) = 9.7, p < .05; and consuming more than others, χ2(12, N = 154) = 34.0, p < .01. Specific to the younger children was the likelihood of reporting feeling sick after eating, χ2(3, N = 156) = 11.6, p < .01. Similar to the older participants, younger children endorsed all of the emotion-related probes other than having an event trigger the episode. Hierarchical cluster analysis including only the younger children revealed a somewhat different set of characteristics from results generated by the entire sample. These 15 children, 12 of whom endorsed OBEs or SBEs, tended to report that the episode took place at a home other than their own and in the afternoon and that they were eating more than others. Similar to the cluster for the entire group, younger children also reported experiencing a negative emotion and a trigger occurring prior to the episode, eating in secret, and feeling numb.
An analysis of the data was also conducted separately for boys (n = 177) and girls (n = 268). Chi-square frequencies did not differ considerably by sex compared to findings of the entire sample, although boys with OBEs (78.4%) and SBEs (70.0%) were just as likely as those with OOs (68.1%) or NEs (60.3%) to be overweight, χ2(3, N = 177) = 2.2, p = .54. Among the boys, there were no reported differences by episode type with regard to experiencing a trigger prior to or feeling sick after the episode (ps > .10). Cluster analyses revealed a distinct subgroup of boys (n = 10), of whom 4 reported an OBE or SBE. These boys were likely to endorse being alone and watching television while eating. They were also likely to report that the episode was a snack and being unsure of how much they were eating. Other than experiencing a negative emotion prior to the episode, unlike the rest of the sample, this subgroup of boys did not endorse any other emotional experiences during their episode.
In a third set of analyses, we examined youths participating in weight loss studies (n = 198) and nonintervention participants (n = 247) separately. Chi-square analyses based on treatment status differed little from those for the entire sample. However, for participants in weight loss studies, there were no significant differences based on episode type regarding where the episode took place or whether they felt sick after the episode. Weight loss study participants with OBEs were more likely to feel full after eating, χ2(3, N = 198) = 10.6, p = .01. For nonintervention children and adolescents, there were no significant differences between episode type and feeling secretive about eating, hiding their food, or the amount they were eating compared to others. By contrast, non-treatment participants with OBEs were more likely to report feeling physically hungry before their episode, χ2(3, N = 247) = 7.8, p = .05. Cluster analyses for the weight loss treatment participants and nonintervention children and adolescents each identified a subgroup of 5 participants, all of whom were included in the cluster generated from the entire sample. As expected, these youths were very similar to the cluster from the entire sample. However, the weight loss treatment cluster was also likely to report hiding their food, eating more than others, and feeling sick afterward. The nontreatment cluster was additionally likely to report that their episode was in the afternoon and associated with feeling tired. Both groups differed from the entire sample in that they were likely to report eating quickly.
Discussion
In this multisite investigation, we found that children and adolescents who engaged in loss of control eating episodes endorsed aspects of disordered eating that were generally reflective of the adult criteria for BED (APA, 2000). Youths endorsing loss of control eating episodes also tended to report an experience of numbing while eating. Moreover, a cohesive subset of individuals (disordered eating cluster) who reportedly had engaged in at least line episode of loss of control eating in the past month may represent a characterization of disordered eating specific to children and adolescents. Although these individuals did not differ from the rest of the sample with regard to BMI z score, they reported significantly higher Eating Concern, Shape Concern, and global EDE scores compared to the rest of the sample.
Our findings regarding children and adolescents appear to mirror those reported for adult samples in several respects. To our knowledge, there are no data regarding the prevalence of dieting among obese adults in Europe; however, U.S. data indicate that approximately 70% and 63% of obese women and men, respectively, report trying to lose weight (Bish et al., 2005). In our sample, approximately 60% of overweight girls and 65% of overweight boys were participating in weight loss treatment studies. With regard to loss of control eating, a number of items endorsed by participants with OBEs and SBEs were similar to the criteria for BED described in the DSM-IV-TR—in particular, “eating large amounts of food when not feeling physically hungry; eating alone because of being embarrassed by how much one is eating; and feeling disgusted with oneself, depressed, or very guilty after overeating” (APA, 2000, p. 787). Tills finding suggests that when loss of control eating is carefully described and contextual, behavioral, physical, and emotional aspects are articulated, youths who eat while experiencing loss of control share many characteristics with adults who engage in similar behaviors. The experience of numbing, which we found to be common among children and adolescents with OBEs and SBEs, is not one of the specific DSM-IV-TR criteria for BED but is described in adults with BED. The Associated Features and Disorders section of the DSM-IV-TR for BED specifically states that some “individuals describe a dissociative quality to the binge episodes (feeling ‘numb’ or ‘spaced out’)” (APA, 2000, p. 786). The term alexithymia, defined as cognitive-emotional deficits such as the inability to identify and express emotions and affect as well as an avoidance in coping with conflicts or articulating emotions (Sifneos, 1996), has been shown to be elevated in adults with BED (Pinaquy, Chabrol, Simon, Louvet, & Barbe, 2003). In our sample, participants used the terms numb out, zone out, blank out, paralyzed, and stunned to represent this construct. One hypothesis that may explain such findings is that children and adolescents are unaware of their emotional experiences, particularly with regard to the experience of loss of control over eating (Tanofsky-Kraff et al., 2007). Indeed, it has been posited that because youths are often not cognizant of their emotional experiences during eating episodes, they may find it difficult to understand and report them (Maloney, McGuire, & Daniels, 1988). Alternatively, it is possible that alexithymia, while associated with BED in adults, is a central component of loss of control eating problems among youths. This potentially supports escape theory, which views binge eating as a motivated attempt to escape aversive self-awareness or emotional distress (Heatherton & Baumeister, 1991).
Within our sample, there was a subset of participants who appeared to share a number of common features in addition to the endorsement of OBEs and SBEs. This disordered eating cluster not only reported experiences similar to those described by adults with BED but also represented approximately 3% of the entire sample, an estimate that is comparable to the prevalence rate of BED described in overweight adults when assessed by structured clinical interview (APA, 2000; Spitzer et al., 1993). Notably, almost half of these participants met either full or subthreshold criteria for DSM-IV-TR BED. Similar to child and adolescent presentations of other Axis I disorder classifications (e.g., Axelson et al., 2006; Dopheide, 2006; Stewart et al., 2007), children with binge eating problems may share many of the aspects specific to BED in adults but vary with regard to the frequency, intensity, and emphasis of particular symptoms.
The disordered eating cluster did not differ from the rest of the sample with regard to BMI z score. The lack of a BMI difference may be a consequence of our sample, which oversampled for overweight children and adolescents. Studies of overweight youths often do not demonstrate differences in body size between individuals who do and do not binge eat (Berkowitz et al., 1993; Decaluwe & Braet, 2003; Goossens et al., 2007; Isnard et al., 2003; Tanofsky-Kraff, Faden, Yanovski, Wilfley, & Yanovski, 2005). Although the disordered eating cluster had higher mean EDE Eating Concern and Shape Concern subscale scores and global scores than the rest of the sample, these scores were not within a clinically abnormal range (e.g., means of 2.0 and 4.0, respectively, in one sample of overweight adolescents with full-syndrome BED; Glasofer et al., 2007), and they did not differ on the Dietary Restraint or Weight Concern subscales. Although the lack of findings with regard to the Dietary Restraint subscale is consistent with some studies of overweight adolescents (e.g., Glasofer et al., 2007), weight concern is typically a hallmark construct associated with and predictive of eating disorders (Killen et al., 1994, 1996). Future studies examining the general psychological and social functioning of youths who present with a constellation of behaviors and emotions similar to our disordered eating cluster are required to determine whether our findings may serve as a foundation on which to base development of a youth-specific presentation of binge eating. Until such time, our findings should be considered preliminary given the small number of participants who clustered together.
In post hoc analyses, we found that younger children (12 years or younger) with OBEs and SBEs tended to endorse fewer of the qualitative queries than the older participants. Nevertheless, it is notable that the younger children with loss of control eating in our sample reported all but one criterion (food seeking as a reward—which was not included in the present study) of Marcus and Kalarchian’s (2003) proposed Criteria A (characterization of a binge episode) and B (associations with binge episodes) for BED among children younger than 14 years. Thus, our data bolster the recommendation for a separate set of criteria in middle childhood youths. As is observed for pediatric obesity treatment (Epstein, Valoski, Wing, & McCurley, 1994), in which weight loss appears to be more easily achieved during middle childhood than during adolescence, identifying and intervening with individuals who manifest binge eating behaviors during middle childhood might result in a more promising prognosis.
Boys with OBEs and SBEs in our sample endorsed many of the same aspects of aberrant eating as their female counterparts. However, on the basis of cluster analyses, unlike the girls, only 40% of this group endorsed an OBE or SBE, and these boys were less likely to endorse many of the emotional aspects associated with their eating episodes. Our findings support some (Tanofsky, Wilfley, Spurrell, Welch, & Brownell, 1997; Tanofsky-Kraff et al., 2007), but not all (Masheb & Grilo, 2006), data suggesting that men and boys may be less likely than women and girls to report eating in response to negative affect.
Our findings support the notion that loss of control eating is identifiable by interview methods when contextual, behavioral, physical, and, most salient, emotional aspects are explicated and assessed. Given that a third of the participants in the disordered eating cluster were from the Ghent site, findings may be generalized not only to youths in the U.S. but also to non-English-speaking children and adolescents. Collectively, the sample was enriched for overweight, which suggests that our findings may be most relevant to heavier youths. Further, as more than half of the clustered participants were adolescent girls initiating weight loss treatment, these youths may be at greatest risk for disordered eating involving loss of control eating behaviors in the absence of compensatory behaviors. We recommend that providers treating such individuals not only screen for loss of control eating but carefully assess all circumstances surrounding the episodes with queries similar to those developed for the SPEEI. These youths may require a more specialized treatment for disturbed eating in addition to weight loss. Nevertheless, a third of our disordered eating cluster was not involved in weight loss treatment, and 20% of these participants were not overweight. On the basis of responses to the SPEEI, the descriptive differences of OBEs and SBEs between treatment and nontreatment children were few. Moreover, although more weight loss treatment participants were identified in the disordered eating cluster, the percentages of children and adolescents with loss of control eating did not differ on the basis of treatment status. The implication is that although participating in weight loss treatment may be associated with a higher risk for a constellation of disordered eating behaviors, identifying and intervening with individuals who are not in weight loss programs but endorse loss of control eating may prevent excessive weight gain and the onset of full-syndrome eating disorders.
Strengths of the present investigation are the large sample; the inclusion of racially, ethnically, and geographically diverse youths from multiple research facilities; and the use of measured height and weight. An additional asset is the use of structured clinical interviews to assess disordered eating behaviors, attitudes, and the specific qualitative aspects surrounding aberrant eating episodes. A primary limitation of the present study is the delayed inclusion of queries for participants with NEs about their described eating episode. Despite this disadvantage, the inclusion of a control group of children and adolescents describing nonaberrant eating offers an important comparison to those with such episodes. A possible shortcoming of our study is that we did not include a measure of participants’ eating behaviors based on parent report. Although asking parents for collateral information might have provided useful corroborative data, it is unclear whether parents are able to accurately report their children’s eating behaviors (W. G. Johnson, Grieve, Adams, & Sandy, 1999; Steinberg et al.. 2004; Tanofsky-Kraff, Yanovski, & Yanovski, 2005). Finally, our collective sample was not recruited in a truly population-based fashion. Even among the nonintervention children and adolescents, families opted to participate and thus might have been more health conscious than the general population, which potentially limits the external generalizability of the study. Studies to document the prevalence and characteristics of disturbed eating in community-based samples of youths are therefore needed.
We conclude that many aspects of pediatric loss of control eating are similar to those of adults but that a youth-specific syndrome may exist at a prevalence rate comparable to adult eating disorders. The present study may provide a foundation on which to develop evidence-based criteria building on a unique presentation of binge eating among youths. Moreover, our data may help to clarify the findings that reported loss of control eating is predictive of excessive weight gain and full-syndrome eating disturbance, and they may serve as a basis for the design of appropriate interventions to prevent these outcomes.
Acknowledgments
This work was supported by National Institute of Child Health and Human Development Grant ZO1 HD-00641 and a supplement from the National Center on Minority Health and Health Disparities to Jack A. Yanovski; special research funds from Ghent University to Caroline Braet; National Institute of Mental Health Grant 5F31MH071019 and a Charles H. Hood Foundation grant to Kamryn T. Eddy; Family-Based Treatment of Severe Pediatric Obesity Grant HD38425 and Pittsburgh Obesity/Nutrition Research Center Grant DK46204 to Marsha D. Marcus; and a Washington University Longer Life Foundation grant, National Institute of Mental Health Grant K24 MH070446, National Heart, Lung, and Blood Institute Grant T32 HL007456, and National Institute of Child Health and Human Development Grant R01 HD036904 to Denise E. Wilfley.
Footnotes
The phrase loss of control is used throughout to indicate both binge and loss of control eating in children and adolescents. When referring only to episodes that include a large amount of food with loss of control, we use the term binge.
Using this method, we identified 5 patients in the disordered eating cluster, all of whom were in the cluster of the original analysis. Further analysis of the 10 cases assigned to the original disordered eating cluster showed that these cases were very similar to the 5 cases using the full sample. The only differences found were that these cases were less likely than the other 5 in the original analysis cluster to have an emotional trigger but were more likely to be unsure of the amount eaten. To determine the better approach, we compared the original 10 participants to both the 5-case cluster from the entire sample and the rest of the nonclustered participants. With respect to the percentage of participants endorsing each construct, we found that the 10 cases in the original cluster were more similar to the other 5 youths in the disordered eating cluster (Pearson r = .51) than to the rest of the sample (r = .23). Thus, we believe that the presented analysis is more appropriate than including all cases.the contribution to the similarity between two [patients] that would have been provided by a variable whose value is missing is equal to the weighted mean of the contributions provided by the variables for which the values have been observed. (Everitt et al., 2001. p. 53)
Contributor Information
Marian Tanofsky-Kraff, National Institute of Child Health and Human Development and Uniformed Services University of the Health Sciences.
Lien Goossens, Ghent University.
Kamryn T. Eddy, Boston University
Rebecca Ringham, University of Pittsburgh Medical Center.
Andrea Goldschmidt, Washington University School of Medicine.
Susan Z. Yanovski, National Institute of Child Health and Human Development and National Institute of Diabetes and Digestive and Kidney Diseases
Caroline Braet, Ghent University.
Marsha D. Marcus, University of Pittsburgh Medical Center
Denise E. Wilfley, Washington University School of Medicine
Cara Olsen, Uniformed Services University of the Health Sciences.
Jack A. Yanovski, National Institute of Child Health and Human Development
References
- Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. New England Journal of Medicine. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- Agresti A. Testing conditional independence. In: Agresti A, editor. Categorical data analyses. New York: Wiley; 1990. pp. 230–232. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. text rev. Washington, DC: Author; 2000. [Google Scholar]
- Axelson D, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, et al. Phenomenology of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry. 2006;63:1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- Berkowitz R, Stunkard AJ, Stallings VA. Binge-eating disorder in obese adolescent girls. Annals of the New York Academy of Sciences. 1993;699:200–206. doi: 10.1111/j.1749-6632.1993.tb18850.x. [DOI] [PubMed] [Google Scholar]
- Bish CL, Blanck HM, Serdula MK, Marcus M, Kohl HW, Khan LK. Diet and physical activity behaviors among Americans trying to lose weight: 2000 Behavioral Risk Factor Surveillance System. Obesity Research. 2005;13:596–607. doi: 10.1038/oby.2005.64. [DOI] [PubMed] [Google Scholar]
- Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the Eating Disorder Examination with children: A pilot study. International Journal of Eating Disorders. 1996;19:391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Clatworthy J, Buick D, Hankins M, Weinman J, Home R. The use and reporting of cluster analysis in health psychology: A review. British Journal of Health Psychology. 2005;10:329–358. doi: 10.1348/135910705X25697. [DOI] [PubMed] [Google Scholar]
- ClinicalTrials.gov. Safety and efficacy of Xenical in children and adolescents with obesity-related diseases. 2005 Retrieved January 24, 2006 from http://www.clinicaltrials.gov/et/show/NCT00001723.
- Cooper Z, Cooper PJ, Fairburn CG. The validity of the Eating Disorder Examination and its subscales. British Journal of Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- Decaluwe V, Braet C. Prevalence of binge-eating disorder in obese children and adolescents seeking weight-loss treatment. International Journal of Obesity Related Metabolic Disorders. 2003;27:404–409. doi: 10.1038/sj.ijo.0802233. [DOI] [PubMed] [Google Scholar]
- Decaluwe V, Braet C. Assessment of eating disorder psychopathology in obese children and adolescents: Interview versus self-report questionnaire. Behaviour Research and Therapy. 2004;42:799–811. doi: 10.1016/j.brat.2003.07.008. [DOI] [PubMed] [Google Scholar]
- de Zwaan M. Binge eating disorder and obesity. International Journal of Obesity Related Metabolic Disorders. 2001;25 Suppl. 1:S51–S55. doi: 10.1038/sj.ijo.0801699. [DOI] [PubMed] [Google Scholar]
- Dopheide JA. Recognizing and treating depression in children and adolescents. American Journal of Health Systems Pharmacotherapy. 2006;63:233–243. doi: 10.2146/ajhp050264. [DOI] [PubMed] [Google Scholar]
- Doyle AC, le Grange D, Goldschmidt A, Wilfley DE. Psychosocial and physical impairment in overweight adolescents at high risk for eating disorders. Obesity. 2007;15(1):145–154. doi: 10.1038/oby.2007.515. [DOI] [PubMed] [Google Scholar]
- Eddy KT, Tanofsky-Kraff M, Thompson-Brenner H, Herzog DB, Brown TA, Ludwig DS. Eating disorder pathology among overweight treatment-seeking youth: Clinical correlates and cross-sectional risk models. Behaviour Research and Therapy. 2007;45:2360–2371. doi: 10.1016/j.brat.2007.03.017. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA. Emotion, regulation, and the development of social competence. In: Clark MS, editor. Review of personality and social psychology: Vol. 14. Emotion and social behavior. Newbury Park, CA: Sage; 1992. pp. 119–150. [Google Scholar]
- Eisenberg N, Fabes RA, Shepard S, Murphy BC, Guthrie IK, Jones S, et al. Contemporaneous and longitudinal prediction of children’s social functioning from regulation and emotionality. Child Development. 1997;68:642–664. [PubMed] [Google Scholar]
- Eisenberg N, Guthrie IK, Fabes RA, Shepard S, Losoya S, Murphy BC, et al. Prediction of elementary school children’s externalizing problem behaviors from attentional and behavioral regulation and negative emotionality. Child Development. 2000;71:1367–1382. doi: 10.1111/1467-8624.00233. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychology. 1994;13:373–383. doi: 10.1037//0278-6133.13.5.373. [DOI] [PubMed] [Google Scholar]
- Everitt BS, Landau S, Leese M, et al. Cluster analysis. 4th ed. New York: Oxford University Press; 2001. [Google Scholar]
- Fairburn C, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating, nature, assessment and treatment. 12th ed. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Field AE, Austin SB, Taylor CB, Malspeis S, Rosner B, Rockett HR, et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112:900–906. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obesity Research. 2005;13(1):163–169. doi: 10.1038/oby.2005.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field AE, Taylor CB, Celio A, Colditz GA. Comparison of self-report to interview assessment of bulimic behaviors among preadolescent and adolescent girls and boys. International Journal of Eating Disorders. 2004;35:86–92. doi: 10.1002/eat.10220. [DOI] [PubMed] [Google Scholar]
- Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics. 2001;108:712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Inter-relationships among childhood BMI, childhood height, and adult obesity: The Bogalusa Heart Study. International Journal of Obesity Related Metabolic Disorders. 2004;28:10–16. doi: 10.1038/sj.ijo.0802544. [DOI] [PubMed] [Google Scholar]
- French SA, Story M, Neumark-Sztainer D, Downes B, Resnick M, Blum R. Ethnic differences in psychosocial and health behavior correlates of dieting, purging, and binge eating in a population-based sample of adolescent females. International Journal of Eating Disorders. 1997;22:315–322. doi: 10.1002/(sici)1098-108x(199711)22:3<315::aid-eat11>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Glasofer DR, Tanofsky-Kraff M, Eddy KT, Yanovski SZ, Theim KR, Mirch MC, et al. Binge eating in overweight treatment-seeking adolescents. Journal of Pediatric Psychology. 2007;32(1):95–105. doi: 10.1093/jpepsy/jsl012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goossens L, Braet C, Decaluwe V. Loss of control over eating in obese youngsters. Behaviour Research and Therapy. 2007;45:1–9. doi: 10.1016/j.brat.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Greenfeld D, Quinlan DM, Harding P, Glass E, Bliss A. Eating behavior in an adolescent population. International Journal of Eating Disorders. 1987;6:99–111. [Google Scholar]
- Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. American Journal of Clinical Nutrition. 2002;76:653–658. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- Hand D. Discrimination and classification. New York: Wiley; 1981. [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hollingshead A. Four factor index of social status. New Haven, CT: Yale University; 1975. [Google Scholar]
- Isnard P, Michel G, Frelut ML, Vila G, Falissard B, Naja W, et al. Binge eating and psychopathology in severely obese adolescents. International Journal of Eating Disorders. 2003;34:235–243. doi: 10.1002/eat.10178. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Spitzer RL, Williams JB. Health problems, impairment and illnesses associated with bulimia nervosa and binge eating disorder among primary care and obstetric gynaecology patients. Psychological Medicine. 2001;31:1455–1466. doi: 10.1017/s0033291701004640. [DOI] [PubMed] [Google Scholar]
- Johnson WG, Grieve FG, Adams CD, Sandy J. Measuring binge eating in adolescents: Adolescent and parent versions of the Questionnaire of Eating and Weight Patterns. International Journal of Eating Disorders. 1999;26:301–314. doi: 10.1002/(sici)1098-108x(199911)26:3<301::aid-eat8>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Johnson WG, Rohan KJ, Kirk AA. Prevalence and correlates of binge eating in White and African American adolescents. Eating Behaviors. 2002;3(2):179–189. doi: 10.1016/s1471-0153(01)00057-5. [DOI] [PubMed] [Google Scholar]
- Kashubeck-West S, Mintz LB, Saunders KJ. Assessment of eating disorders in women. The Counseling Psychologist. 2001;29:662–694. [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, et al. Weight concerns influence the development of eating disorders: A 4-year prospective study. Journal of Consulting and Clinical Psychology. 1996;64:936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel KF, Hammer LD, et al. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: A three-year prospective analysis. International Journal of Eating Disorders. 1994;16:227–238. doi: 10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Krishnaiah PR, Kanal LN. Handbook of statistics: Vol. 2. Classification, pattern recognition and reduction of dimensionality. Amsterdam: Elsevier; 1982. [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC growth charts for the United States: Methods and development. Vital Health Statistics. 2002;11(246):1–190. [PubMed] [Google Scholar]
- Lamerz A, Kuepper-Nybelen J, Bruning N, Wehle C, Trost-Brinkhues G, Brenner H, et al. Prevalence of obesity, binge eating, and night eating in a cross-sectional field survey of 6-year-old children and their parents in a German urban population. Journal of Child Psychology and Psychiatry. 2005;46:385–393. doi: 10.1111/j.1469-7610.2004.00363.x. [DOI] [PubMed] [Google Scholar]
- Ledoux S, Choquet M, Manfredi R. Associated factors for self-reported binge eating among male and female adolescents. Journal of Adolescence. 1993;16(1):75–91. doi: 10.1006/jado.1993.1006. [DOI] [PubMed] [Google Scholar]
- Leon GR, Fulkerson JA, Perry CL, Early-Zald MB. Prospective analysis of personality and behavioral vulnerabilities and gender influences in the later development of disordered eating. Journal of Abnormal Psychology. 1995;104:140–149. doi: 10.1037//0021-843x.104.1.140. [DOI] [PubMed] [Google Scholar]
- Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus MD. Overeating among seriously overweight children seeking treatment: Results of the children’s eating disorder examination. International Journal of Eating Disorders. 2006;39:135–140. doi: 10.1002/eat.20218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney MJ, McGuire JB, Daniels SR. Reliability testing of a children’s version of the Eating Attitude Test. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:541–543. doi: 10.1097/00004583-198809000-00004. [DOI] [PubMed] [Google Scholar]
- Maloney MJ, McGuire J, Daniels SR, Specker B. Dieting behavior and eating attitudes in children. Pediatrics. 1989;84:482–489. [PubMed] [Google Scholar]
- Marcus MD. Introduction—binge eating: Clinical and research directions. Addictive Behaviors. 1995;20:691–693. doi: 10.1016/0306-4603(95)00103-4. [DOI] [PubMed] [Google Scholar]
- Marcus MD, Kalarchian MA. Binge eating in children and adolescents. International Journal of Eating Disorders. 2003;34 Suppl:S47–S57. doi: 10.1002/eat.10205. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Binge eating disorder: A need for additional diagnostic criteria. Comprehensive Psychiatry. 2000;41(3):159–162. doi: 10.1016/S0010-440X(00)90041-5. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. International Journal of Eating Disorders. 2006;39:141–146. doi: 10.1002/eat.20221. [DOI] [PubMed] [Google Scholar]
- McDuffie JR, Calis KA, Uwaifo GI, Sebring NG, Fallon EM, Hubbard VS, et al. Three-month tolerability of orlistat in adolescents with obesity-related comorbid conditions. Obesity Research. 2002;10:642–650. doi: 10.1038/oby.2002.87. [DOI] [PubMed] [Google Scholar]
- Morgan C, Yanovski S, Nguyen T, McDuffie J, Sebring N, Jorge M, et al. Loss of control over eating, adiposity, and psychopathology in overweight children. International Journal of Eating Disorders. 2002;31:430–441. doi: 10.1002/eat.10038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Hannan PJ. Weight-related behaviors among adolescent girls and boys: Results from a national survey. Archives of Pediatric and Adolescent Medicine. 2000;154:569–577. doi: 10.1001/archpedi.154.6.569. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Story M. Dieting and binge eating among adolescents: What do they really mean? Journal of the American Dietetic Association. 1998;98:446–450. doi: 10.1016/S0002-8223(98)00101-1. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- Pinaquy S, Chabrol H, Simon C, Louvet JP, Barbe P. Emotional eating, alexithymia, and binge-eating disorder in obese women. Obesity Research. 2003;11:195–201. doi: 10.1038/oby.2003.31. [DOI] [PubMed] [Google Scholar]
- Puhl R, Brownell K. Stigma, discrimination, and obesity. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- Rizvi SL, Peterson CB, Crow SJ, Agras WS. Test-retest reliability of the Eating Disorder Examination. International Journal of Eating Disorders. 2000;28:311–316. doi: 10.1002/1098-108x(200011)28:3<311::aid-eat8>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS for Windows Version 9.0 [computer software] Gary. NC: Author; 2003. [Google Scholar]
- Sherwood NE, Jeffery RW, Wing RR. Binge status as a predictor of weight loss treatment outcome. International Journal of Obesity Related Metabolic Disorders. 1999;23:485–493. doi: 10.1038/sj.ijo.0800846. [DOI] [PubMed] [Google Scholar]
- Sifneos PE. Alexithymia: Past and present. American Journal of Psychiatry. 1996;153 Suppl. 7:137–142. doi: 10.1176/ajp.153.7.137. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Yanovski S, Wadden T, Wing R, Marcus MD, Stunkard A, et al. Binge eating disorder: Its further validation in a multisite study. International Journal of Eating Disorders. 1993;13:137–153. [PubMed] [Google Scholar]
- SPSS, Inc. SPSS for Windows 12.0 [computer software] Chicago: Author; 2004. [Google Scholar]
- Steiger H, Puentes-Neuman G, Leung FY. Personality and family features of adolescent girls with eating symptoms: Evidence for restricter/binger differences in a nonclinical population. Addictive Behaviors. 1991;16:303–314. doi: 10.1016/0306-4603(91)90023-b. [DOI] [PubMed] [Google Scholar]
- Steinberg E, Tanofsky-Kraff M, Cohen ML, Elberg J, Freedman RJ, Semega-Janneh M, et al. Comparison of the child and parent forms of the Questionnaire on Eating and Weight Patterns in the assessment of children’s eating-disordered behaviors. International Journal of Eating Disorders. 2004;36:183–194. doi: 10.1002/eat.20022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SE, Rosario MC, Brown TA, Carter AS, Leckman JF, Sukhodolsky D, et al. Principal components analysis of obsessive-compulsive disorder symptoms in children and adolescents. Biological Psychiatry. 2007;61:285–291. doi: 10.1016/j.biopsych.2006.08.040. [DOI] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. Journal of Consulting and Clinical Psychology. 1999;67:967–974. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychology. 2002;21:131–138. [PubMed] [Google Scholar]
- Strauss RS, Pollack HA. Social marginalization of overweight children. Archives of Pediatric and Adolescent Medicine. 2003;157:746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- Styne DM. A plea for prevention. American Journal of Clinical Nutrition. 2003;78:199–200. doi: 10.1093/ajcn/78.2.199. [DOI] [PubMed] [Google Scholar]
- Sysko R, Walsh TB, Schebendach J, Wilson GT. Eating behaviors among women with anorexia nervosa. American Journal of Clinical Nutrition. 2005;82:296–301. doi: 10.1093/ajcn.82.2.296. [DOI] [PubMed] [Google Scholar]
- Tanofsky MB, Wilfley DE, Spurrell EB, Welch R, Brownell KD. Comparison of men and women with binge eating disorder. International Journal of Eating Disorders. 1997;21:49–54. doi: 10.1002/(sici)1098-108x(199701)21:1<49::aid-eat6>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, et al. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117:1203–1209. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Faden D, Yanovski SZ, Wilfley DE, Yanovski JA. The perceived onset of dieting and loss of control eating behaviors in overweight children. International Journal of Eating Disorders. 2005;38:112–122. doi: 10.1002/eat.20158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Morgan CM, Yanovski SZ, Marmarosh C, Wilfley DE, Yanovski JA. Comparison of assessments of children’s eating-disordered behaviors by interview and questionnaire. International Journal of Eating Disorders. 2003;33:213–224. doi: 10.1002/eat.10128. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Theim KR, Yanovski SZ, Bassett AM, Burns NP, Ranzenhofer LM, et al. Validation of the Emotional Eating Scale adapted for use in children and adolescents (EES-C) International Journal of Eating Disorders. 2007;40:232–240. doi: 10.1002/eat.20362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating disordered behaviors, body fat, and psychopathology in overweight and normal weight children. Journal of Consulting and Clinical Psychology. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Yanovski JA. Comparison of child interview and parent reports of children’s eating disordered behaviors. Eating Behaviors. 2005;6:95–99. doi: 10.1016/j.eatbeh.2004.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theim KR, Tanofsky-Kraff M, Salaita CG, Haynos AF, Mirch MC, Ranzenhofer LM, et al. Children’s descriptions of the foods consumed during loss of control eating episodes. Eating Behaviors. 2007;8:258–265. doi: 10.1016/j.eatbeh.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, Foster GD, Letizia KA. Response of obese binge eaters to treatment by behavior therapy combined with very low calorie diet. Journal of Consulting and Clinical Psychology. 1992;60:808–811. doi: 10.1037//0022-006x.60.5.808. [DOI] [PubMed] [Google Scholar]
- Watkins B, Frampton I, Lask B, Bryant-Waugh R. Reliability and validity of the child version of the Eating Disorder Examination: A preliminary investigation. International Journal of Eating Disorders. 2005;38:183–187. doi: 10.1002/eat.20165. [DOI] [PubMed] [Google Scholar]
- Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. New England Journal of Medicine. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Friedman MA, Dounchis JZ, Stein RI, Welch RR, Ball SA. Comorbid psychopathology in binge eating disorder: Relation to eating disorder severity at baseline and following treatment. Journal of Consulting and Clinical Psychology. 2000;68:641–649. [PubMed] [Google Scholar]
- Wilfley DE, Schwartz MB, Spurrell EB, Fairburn CG. Assessing the specific psychopathology of binge eating disorder patients: Interview or self-report? Behaviour Research and Therapy. 1997;35:1151–1159. [PubMed] [Google Scholar]
- Wilfley D, Wilson G, Agras W. The clinical significance of binge eating disorder. International Journal of Eating Disorders. 2003;34 Suppl.:S96–S106. doi: 10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]
- Williams S. Overweight at age 21: The association with body mass index in childhood and adolescence and parents’ body mass index. A cohort study of New Zealanders born in 1972–1973. International Journal of Obesity Related Metabolic Disorders. 2001;25:158–163. doi: 10.1038/sj.ijo.0801512. [DOI] [PubMed] [Google Scholar]
- Yanovski SZ, Gormally JF, Leser MS, Gwirtsman HE, Yanovski JA. Binge eating disorder affects outcome of comprehensive very-low-calorie diet treatment. Obesity Research. 1994;2:205–212. doi: 10.1002/j.1550-8528.1994.tb00049.x. [DOI] [PubMed] [Google Scholar]
- Yanovski SZ, Nelson JE, Dubbert BK, Spitzer RL. Association of binge eating disorder and psychiatric comorbidity in obese subjects. American Journal of Psychiatry. 1993;150:1472–1479. doi: 10.1176/ajp.150.10.1472. [DOI] [PubMed] [Google Scholar]


