Abstract
We tested the efficacy of coronavirus-like particles (VLPs) for protecting mice against severe acute respiratory syndrome coronavirus (SCoV) infection. Coexpression of SCoV S protein and E, M and N proteins of mouse hepatitis virus in 293T or CHO cells resulted in the efficient production of chimeric VLPs carrying SCoV S protein. Balb/c mice inoculated with a mixture of chimeric VLPs and alum twice at an interval of four weeks were protected from SCoV challenge, as indicated by the absence of infectious virus in the lungs. The same groups of mice had high levels of SCoV-specific neutralizing antibodies, while mice in the negative control groups, which were not immunized with chimeric VLPs, failed to manifest neutralizing antibodies, suggesting that SCoV-specific neutralizing antibodies are important for the suppression of viral replication within the lungs. Despite some differences in the cellular composition of inflammatory infiltrates, we did not observe any overt lung pathology in the chimeric-VLP-treated mice, when compared to the negative control mice. Our results show that chimeric VLP can be an effective vaccine strategy against SCoV infection.
Keywords: SARS coronavirus, Virus-like particles, Neutralizing antibody, Mouse
Introduction
Severe acute respiratory syndrome (SARS) is a newly emerged disease caused by SARS coronavirus (SCoV). SARS originated in Southern China in 2002 and spread to five different continents causing >8000 infection and >700 deaths before its apparent eradication as a human infection in 2004 [1]. Healthcare systems in affected areas were severely stressed and additional economic costs in trade and travel were very high. It is not known if the virus will be reintroduced into the human population but ancestral coronaviruses are widely distributed in bats and are thought to have adapted to civets and then to humans in recent time periods [2], [3]. Because emerging viruses tend to reemerge as conditions change [4], it is highly desirable to develop safe and efficacious vaccines and/or antivirals to prevent SCoV infections.
All coronaviruses, including SCoV, carry four structural proteins: nucleocapsid (N) protein and three envelope proteins, namely spike (S) protein, a type I transmembrane glycoprotein; envelope (E) protein; and membrane (M) protein, which has three membrane-spanning domains. Coronavirus S protein is responsible for virus adsorption to susceptible cells through a specific virus–receptor interaction and induces membrane fusion between viral envelope and host cell membrane [5]. S protein is a main player for determining coronavirus tissue tropism, host specificity and viral pathogenicity [6], [7], [8], [9], [10], [11], [12]. Because most coronavirus neutralizing antibodies recognize S protein [1], [13], it is not surprising that most of the current SCoV vaccine candidates are either the S protein subunit itself or those carrying S protein [14], [15], [16], [17], [18], [19]. Furthermore, prophylactic administration of monoclonal antibodies directed at the SCoV S protein protects animals against subsequent SCoV challenge [20], [21], [22], [23]. These studies point out that neutralizing antibodies that recognize SCoV S protein are sufficient to prevent or decrease the morbidity and mortality associated with SCoV infection by primarily suppressing replication of the challenge virus.
Coronavirus-like particles (VLPs) are produced from the cells coexpressing the S, M, and E proteins [24]; expression of the latter two proteins are sufficient for VLP production [24]. M protein plays a central role in virus assembly, while S protein is assembled into coronavirus particles through S protein–M protein interaction [25], [26], [27], [28]. Further, interactions of the M protein with the RNA packaging signal of the viral RNA [29] and with N protein [29], [30], [31], [32] drive incorporation of the helical nucleocapsid complex, which consists of the viral genome and N protein, into virus particles. Vaccinia virus and/or alphavirus replicons have been used to express coronavirus proteins to enable generation of VLPs [33], [34], [35], while we have reported production of SCoV VLPs from 293T cells that are co-transfected with four eukaryotic pCAGGS-based expression plasmids, each of which encodes SCoV S, M, N and E proteins [36]. Others have also reported production of SCoV VLP from insect cells [37], [38] and mammalian cells [39].
During our studies of coronavirus assembly, we found an efficient production of chimeric VLPs carrying SCoV S protein and murine coronavirus (mouse hepatitis virus or MHV) M, N and E proteins from cells coexpressing those proteins. In mice immunized with the chimeric VLPs, the present study describes elicitation of antibodies that neutralized SCoV and suppressed challenged SCoV replication in the lungs. These findings suggest that the use of chimeric VLP is an effective vaccine strategy against SCoV infection.
Materials and methods
Cells and virus
Vero E6 cells, 293T cells and CHO cells were grown in Dulbecco's modified minimum essential medium (DMEM) supplemented with penicillin (100 units/ml), streptomycin (100 μg/ml), 0.2% sodium bicarbonate and 10% fetal bovine serum (FBS). The Urbani strain of SCoV was obtained from T.G. Ksiazek at the Centers for Disease Control and Prevention (Atlanta, GA), and a working stock of this virus was prepared by serially passaging a portion of the seed virus twice in Vero E6 cells. The culture fluid from infected cells was clarified by low-speed centrifugation and was filtered using a 0.45 μm filter, portioned, and frozen at −80 °C. Medium from uninfected Vero E6 cells was similarly treated and processed.
Plasmid construction
The plasmids, pCAGGS-MHV-A59/S, pCAGGS-MHV-A59/E, pCAGGS-MHV-A59/M, and pCAGGS-A59/N, were constructed by inserting the entire region of MHV structural proteins, S, E, M and N, respectively, into a chicken beta-actin promoter-based expression plasmid, pCAGGS-MCS; plasmid pMH54 [40] was obtained from Paul Masters and used as a template for PCR amplification of MHV structural genes. Construction of plasmids, pCAGGS-S expressing SCoV S protein, pCAGGS-E expressing SCoV E protein, pCAGGS-M expressing SCoV M protein, and pCAGGS-N expressing SCoV N protein, was described previously [36].
Preparation and purification of VLPs
For preparation of MHV VLPs, subconfluent 293T cell cultures in 100-mm tissue culture dishes were cotransfected with 14 μg of pCAGGS-MHV-A59/S, 0.4 μg of pCAGGS-MHV-A59/E, 3.5 μg of pCAGGS-MHV-A59/M, and 14 μg of pCAGGS-A59/N using TransIT-293 reagent (Mirus). At 3 days posttransfection, the culture media were collected, centrifuged at 1550 × g for 10 min and filtered through a 0.45-μm filter to remove cell debris. The MHV VLPs were pelleted down through 20% sucrose cushion at 26,000 rpm for 3 h by using a Beckman SW 28 rotor. After the pellets were suspended in NTE buffer (100 mM NaCl, 10 mM Tris–HCl, pH 7.0, 1 mM EDTA), the VLPs were centrifuged using a Beckman SW 28 rotor at 26,000 rpm for 3 h on a discontinuous sucrose gradient consisting of 60, 50, 30, and 20% sucrose. The VLPs at the interface of 30 and 50% sucrose were collected, diluted and further purified on a discontinuous sucrose gradient consisting of 60, 50, 30, and 20% sucrose at 26,000 rpm for 18 h. Purified and concentrated VLPs at the interface between 50 and 30% sucrose were collected, diluted and pelleted through a 20% sucrose cushion at 26,000 rpm for 2 h. The pellets were suspended in NTE buffer and kept at −80 °C until further use. For preparation of SCoV VLP, a mixture of 2.8 μg of pCAGGS-S, 13.2 μg of pCAGGS-E, 1.4 μg of pCAGGS-M, and 2.8 μg of pCAGGS-N was cotransfected into 293T cells grown on a 100-mm tissue culture plate. Chimeric VLPs were generated by transfecting 293T cells or CHO cells in a 100-mm tissue culture plate with 14 μg of pCAGGS-S, 0.4 μg of pCAGGS-MHV-A59/E, 3.5 μg of pCAGGS-MHV-A59/M, and 14 μg of pCAGGS-A59/N. SCoV VLPs and chimeric VLPs were purified using the same procedure as described for the MHV VLP purification.
Quantitation of VLP amounts
The total protein concentration of VLPs was quantitated by Bio-Rad DC protein assay according to the manufacturer's instructions (BIO-RAD, CA).
Western blot analysis
Western blotting was performed as described previously [36]. For detection of MHV S, M and N proteins, we used anti-MHV serum, which was produced by immunizing rabbits with a purified JHM strain of MHV, kindly provided by Susan Baker, Loyola University of Chicago. For detection of SCoV S protein, a mixture of purified rabbit polyclonal anti-SCoV S protein antibody (ABGENT, cat. no. AP6000a) and polyclonal rabbit anti-SCoV S protein antibody (IMGENEX, cat. no. IMG 541) was used. SCoV N protein was detected by using rabbit polyclonal anti-SCoV N protein antibody (IMGENEX, cat. no. IMG 548), and SCoV M protein was detected by using a mixture of SCoV PUPM antibody-N-terminal (ABGENT, cat. no. AP6008a), SCoV PUPM antibody C-terminal (ABGENT, cat. no. AP6008b) and anti-SCoV M antibodies (ProSci, cat. no. 3527P and cat no. 3529P).
Colloidal Coomassie blue staining
After washing the gel with water, proteins in the gel were stained by soaking the gel with Bio-Safe Coomassie Stain (BIO-RAD) with gentle agitation for 1 h. The gel was rinsed extensively with water overnight.
Electron microscopic analysis of chimeric VLP
Carbon-coated, 200-mesh copper grids were floated on drops of chimeric VLP for 10 min. After washing the grids with water three times, negative staining was performed using 2% phosphotungstic acid (pH 7.0) for 1 min. After air drying of the grids, the sample was examined under a Philips 201 transmission electron microscope, and pictures were taken at 60 kV.
Animals
Six- to 8-week-old, female Balb/c mice (Charles River laboratory, Wilmington, MA) were housed in cages covered with barrier filters in an approval biosafety level 3 animal facility maintained by the University of Texas Medical Branch at Galveston, Texas. All of the mouse experiments were performed using experimental protocols approved by the University of Texas Medical Branch Investigational Animal Care and Use Committee; all of the experiments were carried out following National Institutes of Health and United States Department of Agriculture guidelines.
Procedures for immunization and SCoV challenge
MHV VLPs, chimeric VLPs or influenza virus vaccine were adjusted to twice their desired final concentration (μg/0.1 ml) and then mixed with an equal volume of phosphate buffered saline (PBS) or alum adjuvant (Imject alum, Pierce, cat. no. 77161). At day 0, they were administered intramuscularly (i.m.) using 1-ml tuberculin syringes (Norm-Ject, Tuttingen, Germany) and 26-g, 3/8-in. beveled needles (Becton Dickinson, cat. no. 305110). In control groups, mice were inoculated i.m. with Vero E6 cell culture fluid, a mixture of influenza vaccine and alum, or alum alone, or they were left untreated. Mice were inoculated on day 0 and, as indicated in the body of the paper a second injection was given on day 28 in most experiments. SCoV was inoculated directly into the nares of mice (40 μl) that were lightly anesthetized with isoflurane (IsoFlo; Abbott Laboratories; North Chicago, IL). Mice that were inoculated with 1 × 106 TCID50 of SCoV at day 0 to provide post-infection immunity did not undergo a second inoculation. In most of our experiments, immunized mice were challenged by intranasal (i.n.) inoculation of 1 × 106 TCID50 of SCoV at day 56 and they were euthanized at day 58, while in some experiments mice were inoculated with SCoV at day 28 and they were euthanized at day 30. Day 2 post inoculation was chosen because of reports that peak titer occurs at that time [23] and this was confirmed in our laboratory.
Titration of SCoV-specific neutralizing antibodies
Mice were anesthetized with isoflurane and then bled from the retro-orbital sinus plexus. After heat inactivation at 56 °C for 30 min, sera were stored at 4 °C. The assay for virus-specific neutralizing antibodies was performed on serial 2-fold diluted samples of each serum beginning at a dilution of 1:5 using 2% FBS-DMEM as the diluent in 96-well tissue culture plates (Falcon 3072); the final volume of the serially diluted samples in each well was 60 μl. After addition of 120 TCID50 of SCoV in 60 μl into each well, the samples were incubated for 45–60 min at room temperature. Then 100 μl of these mixtures, containing 100 TCID50 of SCoV, were transferred into duplicate wells of confluent Vero E6 cells grown in 96-well microtiter plates. After 72 h incubation, when the virus control wells exhibited advanced virus-induced CPE, the neutralizing capacity of individual serum samples was assessed by determining the presence or absence of virus-induced CPE. SCoV-specific neutralizing antibody titers were expressed as the reciprocal of the last dilution of serum that completely inhibited virus-induced CPE.
Collection of lungs, histology, immunohistochemistry, and virus titration
Two days post SCoV challenge, mice were euthanized and their lungs were removed. Lung lobes, including right middle lobe, right lower lobe, accessory lobe and left lobe, were removed and placed in 10% buffered formalin for subsequent histological examination and immunohistochemistry (IHC) as described previously [41]. For virus titration, the remaining lobes of the lungs were weighed and frozen at −80 °C before being homogenized in PBS/10% FBS solution using the TissueLyser (Qiagen; Retsch, Haan, Germany). The homogenates were then centrifuged, and SCoV titers in the clarified fluid were determined in a TCID50 assay in quadruplicate wells of Vero E6 cells in 96-well plates. Titers of virus in lung homogenates were expressed as TCID50/gram of the lungs (log10) and the minimal detectable level of virus was 2.3 log10 TCID50/g.
Formalin-fixed and paraffin-embedded tissue sections were subjected to the standard hematoxylin and eosin and IHC staining for evaluating histopathology and detecting SCoV antigen, respectively [41].
Statistical analysis
By using a statistical program Instat, (version 3, Graphpad Software, Inc., San Diego, CA), we performed the Kruskal–Wallis non-parametric analysis of variance (ANOVA) test to compare arithmetic mean SCoV lung titers and neutralizing antibody titers; undetectable virus titers were assigned a value of 1.8 (the minimal detection limit being 2.3 log10/g lung) and undetectable virus-specific neutralizing titers were assigned a value of 10.
Results
Production and characterization of chimeric VLPs
We have previously reported the successful production of SCoV VLPs from 293T cells cotransfected with four pCAGGS-based plasmids, each of which encodes SCoV S, M, N or E proteins [36] without using exogenous viruses for protein expression. In the study reported here we varied the amount of each plasmid for cotransfection and were able to generate approximately 1.3 μg of SCoV VLPs from 2 × 107 293T cells. Colloidal Coomassie blue staining and Western blot analysis identified SCoV S, N and M proteins in the purified SCoV VLPs (Fig. 1A). Likewise, transfection of four pCAGGS-based plasmids, each of which encoded MHV S, E, M or N proteins, resulted in production of MHV VLPs (Fig. 1A). After optimization, we obtained approximately 22.3 μg of purified MHV VLPs from 2 × 107 293T cells, demonstrating that the efficiency of MHV VLP production was substantially better than that of SCoV VLP production. Because M and E proteins drive VLP assembly and release [24], and coronavirus S protein is incorporated into VLPs through M–S interaction [25], [27], [28], [42], these data indicated that MHV M and E proteins resulted in more efficient VLP production than did SCoV M and E proteins.
Figure 1.
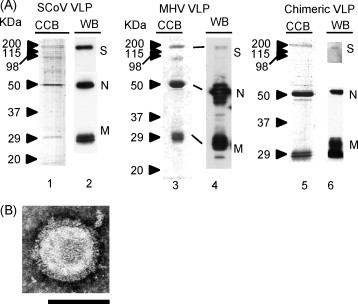
Characterization of VLPs. (A) SCoV VLPs, MHV VLPs and chimeric VLPs, all of which were produced from 293T cells, were independently purified by sucrose gradient centrifugation and 5 μg of purified VLPs were applied to each lane of SDS-PAGE. Colloidal Coomassie blue staining (CCB) and Western blot (WB) analysis of purified SCoV VLPs, MHV VLPs and chimeric VLPs are shown. (B) Negative staining of a chimeric VLP. Arrowheads indicate peplomers. Bars = 100 nm. Courtesy of Dr. Vsevolod L. Popov.
We next tested whether coexpression of SCoV S protein and MHV E, N and M protein could result in the efficient production of chimeric VLPs which would contain high concentrations of the SCoV S protein. If SCoV S protein interacts with MHV M protein, then the robust VLP production machinery driven by MHV M and E proteins, could result in efficient chimeric VLP production. Chimeric VLP production, indeed, occurred from 293T cells that were cotransfected with plasmids, each of which expressed SCoV S protein, MHV N protein, MHV M protein or MHV E protein (Fig. 1A). Colloidal Coomassie blue staining and Western blot analysis of purified chimeric VLP showed the presence of SCoV S, MHV N and MHV M proteins in chimeric VLPs, with only a low level of host protein contamination. Negative staining of chimeric VLP revealed a typical spherical coronavirus structure with peplomers (Fig. 1B). After optimization, approximately 8.7 μg of purified chimeric VLPs was produced from 2 × 107 293T cells; the efficiency of chimeric VLP production was about 8 times better than that of SCoV VLPs.
We next tested efficiencies of chimeric VLP production from Vero and CHO cells, both of which have been used for the preparation of human vaccines [43], [44], [45], [46], [47]. By using various DNA transfection reagents and combinations of different concentrations of each plasmid for transfection, the efficiencies of chimeric VLP production from Vero cells were about 10 times lower than those from 293T cells (data not shown). We found that when we used TransIT-293, the production of chimeric VLPs from CHO cells was about one-third of those from 293T cells in repeated experiments (data not shown). Prolonged incubation of transfected 293T cells and CHO cells for more than 4 days posttransfection did not improve the accumulation of chimeric VLPs in the supernatant (data not shown).
Serum neutralizing antibody titers and lung SCoV titers in the mice immunized once with chimeric VLPs
For assessing the usefulness of chimeric VLPs as a SCoV vaccine candidate, we first tested the effects of immunization of mice with chimeric VLPs on serum neutralizing antibody production and inhibition of SCoV replication in the lung. Six- to 8-week-old female Balb/c mice were inoculated i.m. once with a mixture of 2 μg of chimeric VLPs prepared from 293T cells and PBS or 2 μg of chimeric VLP mixed with alum. As a placebo, mice were inoculated i.m. with Vero E6 cell culture fluid, while another group of mice were inoculated i.n. with 1 × 106 TCID50 of SCoV to produce solid post-infection immunity. Twenty-eight days later, the mice were bled for determining the serum neutralizing antibody titers (Fig. 2A). Subsequently, the mice were challenged i.n. with 1 × 106 TCID50 of SCoV and the lung virus titers at 2 days post SCoV challenge were determined (Fig. 2B). No SCoV-specific neutralizing antibodies were detectable in the sera of the mice inoculated i.m. with placebo. Minimal or no virus-specific neutralizing antibodies were evident in mice inoculated with chimeric VLPs mixed with PBS (mean titer 10 ± 0). The mean serum neutralizing titers for the groups of mice inoculated with live virus (70 ± 20) or chimeric VLP administered with alum (60 ± 23) were not statistically different from each other, but were statistically significantly higher (p < 0.05) than those of the mice immunized with a mixture of chimeric VLPs and PBS and the placebo group. After challenge, the mice immunized with Vero E6 cell culture fluid (placebo) or with a mixture of 2 μg chimeric VLP and PBS had high mean virus titers of 6.5 log10/lung and 5.2 log10/lung, respectively. In contrast, no virus was detectable in the lungs of the mice previously administered either live SCoV or 2 μg of chimeric VLP mixed with alum. The SCoV titers in the lungs of these mice two days post virus challenge were inversely proportional to their serum virus-neutralizing antibody titers.
Figure 2.

SCoV-specific neutralizing antibody titers of immunized mice at 28 days after immunization (A) and SCoV titers in lungs of mice 2 days after intranasal challenge with 1 × 106 TCID50 of SCoV at day 28 (B). (A) Mean SCoV-specific neutralizing antibody titers of the mice at 28 days after i.n. inoculation of SCoV or i.m. inoculation of placebo (medium from Vero E6 cells) or 2 μg chimeric VLP suspended in PBS or alum are shown. The lengths of the bars indicate mean virus-specific serum neutralizing antibody titers. The vertical dashed line demarks the minimal antibody detection level in this assay (i.e., 10). (B) Mice were independently inoculated i.m. with placebo (medium from Vero E6 cells), a mixture of 2 μg chimeric VLP and PBS or a mixture of 2 μg chimeric VLP and alum or i.n. with 1 × 106 TCID50 of infectious SCoV. After 28 days, these mice were challenged with 1 × 106 TCID50 of SCoV. Two days later, mice were sacrificed and the virus titers in the lungs were determined as shown in the graph. The lengths of the bars indicate mean pulmonary virus titers in each indicated group (log10/lung). The vertical dashed line denotes the minimal virus detection level in this assay (i.e., 2.3 log10/lung). Number of animals/group = 5.
Effects of chimeric VLP amounts on neutralizing antibody titers and inhibition of challenged SCoV replication in the lungs
To study the immunogenicity of chimeric VLPs, three groups of mice were inoculated i.m. with 0.5, 1, or 2 μg mixed with alum. Other groups of mice received a mixture of 2 μg of chimeric VLPs and PBS, 2 μg of MHV VLPs and alum, 1 μg of Influenza A virus vaccine and alum, Vero E6 cell culture fluid, live SCoV, or alum alone, or the mice received no treatment. Mean neutralizing titers at 28 days post inoculation in mice receiving 0.5, 1, or 2 μg chimeric VLPs with alum were 20 ± 10, 84 ± 75, and 110 ± 60, respectively (Fig. 3A). In the absence of alum, 2 μg chimeric VLPs induced a lower but significant neutralizing antibody response of 12.5 ± 5. The mice infected with SCoV had the neutralizing titer of 70 ± 20. The mice inoculated with 2 μg of MHV VLP had no detectable virus-specific neutralizing antibodies, demonstrating that MHV S protein did not elicit neutralizing antibodies against SCoV. The neutralizing antibody titers at 28 days post inoculation were not investigated in the groups of mice inoculated with Influenza vaccine and alum, alum alone, or in those receiving no treatment.
Figure 3.
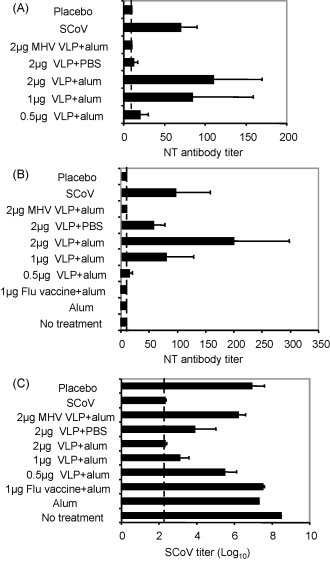
SCoV-specific neutralizing serum antibody titers in the immunized mice and SCoV titers in lungs of mice 2 days after intranasal challenge with SCoV at day 56. On day 0, mice were either left untreated or were inoculated i.n. with 1 × 106 TCID50 of SCoV or injected i.m. with placebo (medium from Vero E6 cells), a mixture of 2 μg MHV VLPs and PBS, a mixture of 2 μg chimeric VLP and PBS, a mixture of 2 μg chimeric VLP and alum, a mixture of 1 μg chimeric VLP and alum, a mixture of 0.5 μg chimeric VLP and alum, a mixture of 1 μg influenza virus vaccine and alum, or alum alone. (A) The graph represents virus-specific serum neutralizing antibody titers at 28 days post inoculation. Number of animals/group = 5. (B) At 56 days blood samples were collected, and then the mice, excluding those inoculated with live SCoV and left untreated, were re-inoculated with the same material. The graph represents virus-specific, serum-neutralizing antibody titers at 56 days after initial inoculation. The vertical dashed lines in (A) and (B) denote the minimal antibody detection level in this assay (1/10 dilution). (C) Mice were inoculated with 1 × 106 TCID50 of SCoV at day 56. After 2 days, mice were euthanized, and the lung virus titers were determined. The vertical dashed line in (C) denotes the minimal virus detection level in this assay (2.3 log10 TCID50/g lung). The data from two independent experiments were combined and are represented in (B) and (C). The number of mice used for (B) and (C) were: 7 for placebo, SCoV, and 2 μg chimeric VLP with PBS; 6 for 2 μg chimeric VLP with alum; 5 for MHV VLP with alum and 1 μg chimeric VLP with alum; 4 for 0.5 μg chimeric VLP with alum; and 3 for all other groups.
At day 28, these mice, except for those untreated and those that had been inoculated with live SCoV, were boosted with the same material. Then the neutralizing antibody titers at day 56 were determined (Fig. 3B). Mice injected with chimeric VLPs and alum had no increase in titer at the lowest dose, but 1- and 2-μg doses resulted in marked booster responses. Animals receiving the highest dose developed titers of 200 ± 97.7, while those infected with SCoV had the neutralizing titer of 97 ± 60. A second inoculation of a mixture of 2 μg chimeric VLPs with PBS efficiently boosted median neutralizing antibody titers to 57 ± 21, which was higher than the titer following 0.5 μg of chimeric VLP mixed with alum (15 ± 5.7). No neutralizing antibodies were detected at the lowest dilution tested in groups receiving MHV VLP, influenza vaccine and alum, alum alone, or placebo or in those left untreated.
All mice were challenged i.n. with live SCoV on day 56 and sacrificed 2 days later. As expected, maximal pulmonary virus titers were detected in the groups of mice inoculated with placebo (6.9 log10 ±0.7), MHV VLPs (6.2 log10 ±0.4), influenza vaccine and alum (7.5 ± 0.1), alum alone (7.3 ± 0), and in those left untreated (8.5 ± 0) (Fig. 3C). Partial protection was obtained in groups of mice inoculated twice with 0.5 μg chimeric VLP mixed with alum (5.5 log10 ±0.6), 2 μg chimeric VLPs and PBS (3.9 log10 ±1.1) or 1 μg chimeric VLPs mixed with alum (3.1 log10 ±0.5). Notably, no virus was detectable in the lungs of any of the mice given live virus i.n. or two doses of 2 μg chimeric VLP mixed with alum. The mean lung virus titers for the latter two groups were statistically different from the mean pulmonary SCoV titer seen in the placebo control group when these means were compared using a non-parametric ANOVA test (both p values being <0.01). Overall, the virus levels in these animals generally correlated inversely with those of SCoV-specific neutralizing antibodies present in the sera of the mice.
Histopathological examination and IHC of the lungs of the immunized mice after SCoV challenge
Histopathological examination of the groups of mice that neither produced neutralizing antibodies nor suppressed SCoV replication in the lungs (i.e., mice treated with Vero E6 cell culture fluid, inoculated with a mixture of influenza virus vaccine and alum, and with alum alone, as well as those left untreated), revealed moderate interstitial pneumonia (Fig. 4A and B). The bronchial epithelium appeared to be the main affected target with prominent cellular cytoplasmic swelling and blebbing. Extensive accumulation of cellular debris and necrotic epithelial cells, accompanied by inflammatory infiltrates, occurred in some bronchioles (Fig. 4A). We also observed a moderate infiltration of mononuclear cells around peribronchiolar and perivascular regions of infected tissues and a mild-to-moderate thickening of the bronchiolar interstitial tissues and alveolar walls with mononuclear cell infiltration (Fig. 4B). IHC staining demonstrated the presence of SCoV N protein within bronchiolar epithelial cells, but not within cells of alveolar lining (Fig. 4C). In contrast to the prominent pathology and viral replication in the lungs of the control animals, mild interstitial pneumonia was found, upon viral challenge, in the mice previously immunized with mixtures of either chimeric VLP and PBS, or chimeric VLP and alum, and in those infected with live SCoV (Fig. 4D, E, G, H). Specifically, cytopathology, i.e., swelling and blebbing, was rarely observed in bronchiolar epithelial cells, despite the presence of some desquamated cells within the airway lumen. Additionally, the thickening of bronchiolar interstitial tissues and the alveolar wall and cellular infiltration were less prominent when compared with those of the control groups. There was no big difference in the lung pathology between mice inoculated with VLP and PBS and those inoculated with VLP and alum. We noticed that inflammatory mononuclear cells seemed to be the main, if not only, cellular component of the cellular infiltrates around the peribronchiolar and perivascular regions of mice initially primed with live SCoV.
Figure 4.
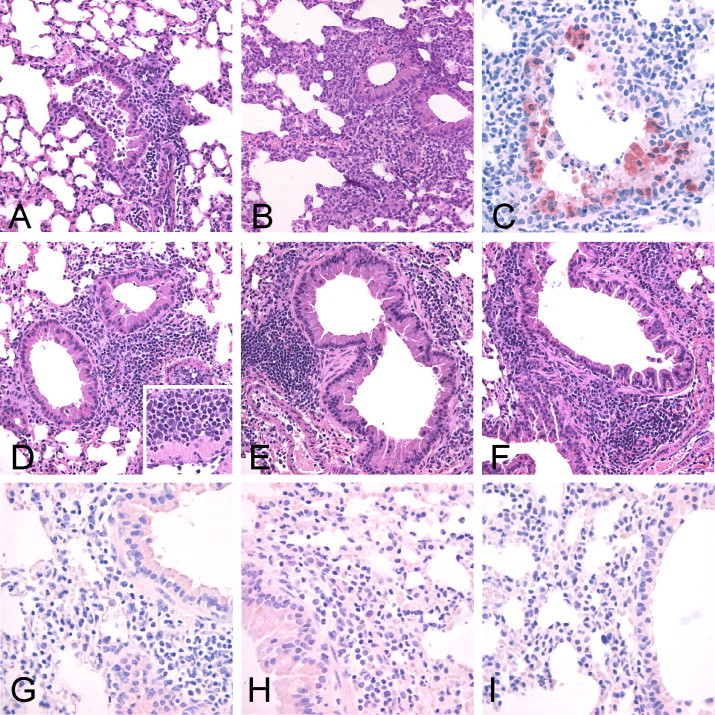
Lung histopathology and immunohistochemistry of the control placebo and immunized mice at 2 days post SCoV challenge. Mice (n = 5 for all groups) were inoculated with VeroE6 cell culture fluids twice at days 0 and 28 (A–C), immunized with a mixture of chimeric VLPs and PBS at days 0 and 28 (D and G), chimeric VLPs and alum (E and H) at days 0 and 28, or live SCoV at day 0 only (F and I). These mice were challenged with SCoV at day 56 and sacrificed at day 58. (A) Bronchiolar epithelial cells showed swelling and blebbing of the luminal cytoplasm, and extensive cellular debris comprised of necrotic epithelium and inflammatory cells in the airway lumen. Moderate peribronchiolar mononuclear inflammatory cell infiltrates are also present (hematoxylin and eosin staining) (magnification, ×200). (B) Thickening of the bronchiolar interstitial tissues and alveolar walls with mononuclear cell infiltration (magnification, ×200). (C) SCoV N antigen was distributed in bronchiolar epithelial cells, as determined by immunohistochemistry (magnification, ×400). (D–F) Bronchiolar epithelial cells showed rare swelling and blebbing of the luminal cytoplasm, and the rare presence of cellular debris in airways (magnification, ×200). The peribronchiolar mononuclear, neutrophil and eosinophil infiltrates (D, inset) (magnification, ×400). (G–I) SCoV antigens were not detected by immunohistochemistry in the lungs of these mice (magnification, ×400).
In addition to inflammatory mononuclear cells, we observed the infiltration of neutrophils and eosinophils around the bronchioles and blood vessels of mice inoculated with a mixture of chimeric VLPs and PBS and that of chimeric VLPs and alum (Fig. 4D and E); counting of the infiltrating cells at the five fields of each mouse's lung tissues revealed that infiltrating eosinophils represented 13.2 ± 9.6% and 22.2 ± 9.9% of all the infiltrating cells in mice inoculated with a mixture of chimeric VLP and PBS and in those inoculated with chimeric VLP and alum, respectively. In contrast, infiltrating eosinophils represented merely 1.42 ± 1.42%, 0%, 0% and 0.77 ± 0.33% of all infiltrating cells in mice inoculated, respectively, with Vero E6 cell culture fluid, a mixture of influenza virus vaccine and alum, alum alone, and in those left untreated.
Discussion
The present study tested the efficacy of immunization of mice with chimeric VLPs for elicitation of anti-SCoV-neutralizing antibodies, suppression of SCoV replication in the lungs, and SCoV-mediated lung cytopathology. Although various strategies for SCoV vaccines, including expression of SCoV S protein in other viruses [18], [48], [49], inactivated SCoV particles [50], [51], [52], [53], DNA vaccines [17], [54], recombinant S protein [55], [56] and other approaches [57], [58], have been reported, to our knowledge this is the first report testing VLPs propagated in mammalian cells as SCoV vaccine candidates. It appears that chimeric VLPs produced from mammalian cells in this study were more immunogenic than were SCoV VLPs produced by using a baculovirus-expression system [38]; immunization of the mice four times with 100 μg of the baculovirus-derived SCoV VLPs in each immunization elicited neutralizing antibody titers that were no longer higher than those obtained in the present study. Use of inactivated SCoV as a SCoV vaccine is a similar vaccine strategy that was explored in the present study. Others reported that immunizing mice twice with 1 μg of double-inactivated SCoV with alum elicited high titers of neutralizing antibodies [50]. A major negative aspect of the use of inactivated SCoV vaccines is that extreme care must be taken to completely inactivate infectious SCoV in the vaccine preparations. In contrast, a VLP-based vaccine strategy eliminates this safety concern.
Accumulated data suggest the importance of the compatibility of the S protein endodomain (or a cytoplasmic tail) and M protein for assembly of S protein into coronavirus or VLPs [40], [59], [60]; in past reports, S protein assembly occurred if these two regions are derived from the same virus, but not from different coronaviruses. Accordingly, we were surprised to find the efficient production of chimeric VLPs carrying SCoV S protein and MHV-derived N, M and E proteins. The present data suggest that the endodomain of SCoV S protein interacted efficiently with MHV M protein and assembled into VLPs. The endodomain of coronavirus S proteins has two partially overlapping sub-regions, a N-terminal, ∼18-residue-long, cysteine-rich region and a C-terminal, ∼27-residue-long, charge-rich region (Fig. 5 ). MHV lacking the very C-terminal 12-amino-acid segment of the S protein endodomain is viable and replicates well in cell culture, suggesting that the removal of 12 carboxy-terminal residues does not inhibit interactions between the mutant S protein and the M protein [25], [26]. In contrast, replication is severely impaired in MHV mutants lacking the very C-terminal 22 amino acids or 25 amino acids of the S protein endodomain, i.e., constituting the majority of the charge-rich region [26]. Furthermore, a single point mutation of a charged amino acid to alanine in the charge-rich region of the endodomain has no detectable effect on the incorporation of a heterologous protein containing MHV S endodomain into virions, whereas mutants containing multiple charged residues-to-alanine significantly reduce the incorporation of the protein into virions [26]. These data suggest that the charge-rich region of the endodomain plays a key role in the selective inclusion of the S protein into the virion. We noted that there were 6 charged residues between the transmembrane domain and the C-terminal 12 amino acids in both SCoV and MHV, while only 3 charged residues are found in feline infectious peritonitis virus (FIPV) (Fig. 5). FIPV S protein is not assembled into VLPs or viruses that carry MHV M, N and E proteins [25]. Accordingly, the presence of the same number of charged residues at the region of the endodomain, which is considered to be important for S protein assembly into virus particles, in both SCoV and MHV implies that both viruses had a similar structure in this portion of the endodomain, allowing them to interact with MHV M protein.
Figure 5.
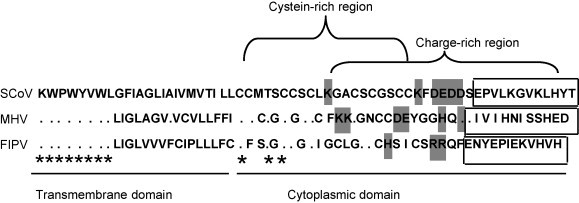
Amino acid sequences of endodomains of SCoV, MHV and FIPV. A CLUSTALW alignment [80] of the carboxy-terminus of S protein sequences of SCoV (strain Urbani, GenBank accession no. AY278741), MHV (strain A59, GenBank accession no. NC_001846), and FIPV (GenBank accession no. AY994055). The transmembrane domain, cytoplasmic domain, cystein-rich region, and charge-rich region are indicated. Charge-residues in the membrane proximal region are shaded. Twelve residues near C-terminal region are in boxes. Asterisks represent identical residues.
Inoculation of mice with a mixture of chimeric VLPs and alum, but not that of MHV VLPs and alum, induced antibodies that neutralized SCoV (Fig. 3). The lack of heterologous protection confirmed that the SCoV S protein is the relevant constituent of the chimeric VLPs. As has been observed in other VLP systems [61], [62], the particles themselves are immunogenic after 1 or 2 injections and provided protection when challenge was carried out after the second i.m. injection of only 2 μg. Addition of alum adjuvant enhanced induction of neutralizing antibodies, and indeed titers reached those post-infection after two injections of 2 μg. All VLP groups had significant protection as evidenced by reduction in lung viral titers 2 days after virulent virus challenge, the optimum time to detect replication in the Balb/c mouse [23]. Higher neutralizing antibody titers correlated with lower virus content, and the 2 μg plus alum groups had no detectable virus. Overall, our data were in agreement with past reports revealing the importance of SCoV-specific neutralizing antibodies, most of which recognize S protein, for curbing SCoV replication in the lung [21], [63], [64], [65], [66], [67].
Immunization of mice with Venezuelan equine encephalitis virus replicon particles encoding SCoV N protein induced an enhanced immunopathology, that included infiltrating eosinophils in the lungs, following SCoV challenge [68], implying the possibility that a SCoV vaccine lacking N protein expression may be desirable, as it would reduce the potential risk of immunopathological changes primed by immunization. In this regard, chimeric VLPs carrying MHV N protein or those lacking N protein (unpublished data) could eliminate the possible induction of SCoV N protein-induced immunopathology. The efficient production of chimeric VLP from CHO cells as we report in this study is promising as a new strategy for preparing VLP-based SCoV vaccine from mammalian cells; its suitability for preparing large quantities of VLP-based vaccine against SCoV remains to be determined. Further improvements of chimeric VLP production, e.g., codon-optimization of the SCoV S gene and MHV N, M and E genes in the expression plasmids and development of an inexpensive transfection reagent and/or procedure, would be required for the substantial enhancement of chimeric VLP production.
Accumulated data suggest that antibodies against the FIPV S protein fail to protect cats from FIPV challenge and enhance virus replication in the host through antibody-dependent enhancement (ADE) [69], [70], [71], [72], [73]. It has been reported that antibodies that neutralize most human SCoV isolates enhance entry of a SCoV isolate from the civet in the cell culture level [74], but it is unclear whether ADE occurs in animals that are immunized with SCoV vaccine candidates. We did not observe signs of ADE in our study; the mice that were immunized with chimeric VLPs or initially inoculated with SCoV efficiently suppressed challenged SCoV replication. S protein in chimeric VLPs was derived from a SCoV Urbani strain, which was also used as the challenge virus, and VLPs induced antibodies that readily neutralized SCoV in vitro. In this regard, it is worth noting that immunization of mice with a Venezuelan equine encephalitis virus replicon carrying S protein of the Urbani strain showed only limited protection against heterologous SCoV that contained S gene from the human GD03 isolate [68].
Subbarao et al. reported mild and focal peribronchiolar mononuclear inflammatory infiltrates and SCoV antigens in bronchiolar epithelial cells in the lungs of BALB/c mice at 2 days post SCoV inoculation [23]. Staining with SCoV monoclonal antibody to N protein, we also found SCoV antigen within bronchiolar epithelial cells after challenge of unimmunized mice. Consistent with the SCoV titers in the lungs, no viral antigen was detected in the lungs of the mice inoculated with chimeric VLPs. The absence of SCoV antigen in the lungs of VLP-immunized mice or mice pre-exposed to live virus, as indicated by the results of IHC staining (Fig. 4B), strongly argue for the efficacy of chimeric VLPs in protecting against SARS-CoV infection. SCoV-induced histopathological changes that were detected in unimmunized mice in our study appeared to be similar or slightly more severe, especially with respect to the changes in the bronchioles, than those described in the report of Subbarao et al. [23]. After SCoV challenge, the mice immunized with chimeric VLPs showed mixed peribronchiolar inflammatory infiltrates and a slight thickening of the peribronchiolar interstitium and alveolar walls. These lesions in immunized mice were milder than seen in unimmunized mice, demonstrating the effects of chimeric VLP immunization in suppressing SCoV-induced cytopathological changes in the lungs. The mice immunized with a mixture of chimeric VLP and alum had higher neutralizing antibody titers than did those immunized with a mixture of the chimeric VLP and PBS, while both groups of the mice showed similar levels of SCoV-induced lung cytopathology, suggesting neither alum nor neutralizing antibody titers were sole determinant of the severity of inflammatory responses. Possible cellular immune responses against chimeric VLP proteins were suggested by the observation that the mice inoculated with a mixture of chimeric VLPs and PBS and that of chimeric VLPs and alum, but not other groups of mice, showed infiltration of neutrophils and eosinophils around the bronchioles and blood vessels. In contrast, it has been reported that immunization of mice with a mixture of inactivated SCoV with adjuvant MF59 primary elicited humoral immune response [75]. Further investigation, using not only Balb/c mice but also other SCoV susceptible mice [41], [76], [77] and other animal models [78], [79], will be necessary to evaluate the implications and impact of cellular immune activities, including pulmonary infiltration of neutrophils and eosinophils, as well as the utility of chimeric VLPs as a SCoV vaccine.
Acknowledgments
We thank Dr. Vsevolod L. Popov and other members of the Electron Microscopy Laboratory and University of Texas Medical Branch for their excellent support for electron microscopy. We also thank Susan Baker for anti-MHV serum, Robert Atmar for statistics analysis and Bob Couch for valuable suggestions and discussion.
This work was supported by National Institutes of Health Service Contract AI 65298 and grants AI29984 and AI72493. NI was supported by a fellowship for long-term overseas research for young investigators sponsored by the Ministry of Education, Culture, Sports, Science and Technology, Japan.
References
- 1.Peiris J.S., Guan Y., Yuen K.Y. Severe acute respiratory syndrome. Nat Med. 2004;10(12 Suppl):S88–S97. doi: 10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vijaykrishna D., Smith G.J., Zhang J.X., Peiris J.S., Chen H., Guan Y. Evolutionary insights into the ecology of coronaviruses. J Virol. 2007;81(8):4012–4020. doi: 10.1128/JVI.02605-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Song H.D., Tu C.C., Zhang G.W., Wang S.Y., Zheng K., Lei L.C. Cross-host evolution of severe acute respiratory syndrome coronavirus in palm civet and human. Proc Natl Acad Sci U S A. 2005;102(7):2430–2435. doi: 10.1073/pnas.0409608102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peters C.J. Emerging viral diseases. In: Knipe D., Howley P., editors. Fields Virology. 5th ed. Lippincott Williams and Wilkins; Philadelphia: 2007. pp. 605–625. [Google Scholar]
- 5.Masters P.S. The molecular biology of coronaviruses. Adv Virus Res. 2006:193–292. doi: 10.1016/S0065-3527(06)66005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li W., Zhang C., Sui J., Kuhn J.H., Moore M.J., Luo S. Receptor and viral determinants of SARS-coronavirus adaptation to human ACE2. EMBO J. 2005;24(8):1634–1643. doi: 10.1038/sj.emboj.7600640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thackray L.B., Holmes K.V. Amino acid substitutions and an insertion in the spike glycoprotein extend the host range of the murine coronavirus MHV-A59. Virology. 2004;324(2):510–524. doi: 10.1016/j.virol.2004.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Navas S., Weiss S.R. Murine coronavirus-induced hepatitis: JHM genetic background eliminates A59 spike-determined hepatotropism. J Virol. 2003;77(8):4972–4978. doi: 10.1128/JVI.77.8.4972-4978.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casais R., Dove B., Cavanagh D., Britton P. Recombinant avian infectious bronchitis virus expressing a heterologous spike gene demonstrates that the spike protein is a determinant of cell tropism. J Virol. 2003;77(16):9084–9089. doi: 10.1128/JVI.77.16.9084-9089.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gallagher T.M., Buchmeier M.J. Coronavirus spike proteins in viral entry and pathogenesis. Virology. 2001;279(2):371–374. doi: 10.1006/viro.2000.0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanchez C.M., Izeta A., Sanchez-Morgado J.M., Alonso S., Sola I., Balasch M. Targeted recombination demonstrates that the spike gene of transmissible gastroenteritis coronavirus is a determinant of its enteric tropism and virulence. J Virol. 1999;73(9):7607–7618. doi: 10.1128/jvi.73.9.7607-7618.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phillips J.J., Chua M.M., Lavi E., Weiss S.R. Pathogenesis of chimeric MHV4/MHV-A59 recombinant viruses: the murine coronavirus spike protein is a major determinant of neurovirulence. J Virol. 1999;73(9):7752–7760. doi: 10.1128/jvi.73.9.7752-7760.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holmes K.V. SARS-associated coronavirus. N Engl J Med. 2003;348(20):1948–1951. doi: 10.1056/NEJMp030078. [DOI] [PubMed] [Google Scholar]
- 14.Zhong X., Yang H., Guo Z.F., Sin W.Y., Chen W., Xu J. B-cell responses in patients who have recovered from severe acute respiratory syndrome target a dominant site in the S2 domain of the surface spike glycoprotein. J Virol. 2005;79(6):3401–3408. doi: 10.1128/JVI.79.6.3401-3408.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang S., Chou T.H., Sakhatskyy P.V., Huang S., Lawrence J.M., Cao H. Identification of two neutralizing regions on the severe acute respiratory syndrome coronavirus spike glycoprotein produced from the mammalian expression system. J Virol. 2005;79(3):1906–1910. doi: 10.1128/JVI.79.3.1906-1910.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keng C.T., Zhang A., Shen S., Lip K.M., Fielding B.C., Tan T.H. Amino acids 1055 to 1192 in the S2 region of severe acute respiratory syndrome coronavirus S protein induce neutralizing antibodies: implications for the development of vaccines and antiviral agents. J Virol. 2005;79(6):3289–3296. doi: 10.1128/JVI.79.6.3289-3296.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang Z.Y., Kong W.P., Huang Y., Roberts A., Murphy B.R., Subbarao K. A DNA vaccine induces SARS coronavirus neutralization and protective immunity in mice. Nature. 2004;428(6982):561–564. doi: 10.1038/nature02463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bisht H., Roberts A., Vogel L., Bukreyev A., Collins P.L., Murphy B.R. Severe acute respiratory syndrome coronavirus spike protein expressed by attenuated vaccinia virus protectively immunizes mice. Proc Natl Acad Sci U S A. 2004;101(17):6641–6646. doi: 10.1073/pnas.0401939101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buchholz U.J., Bukreyev A., Yang L., Lamirande E.W., Murphy B.R., Subbarao K. Contributions of the structural proteins of severe acute respiratory syndrome coronavirus to protective immunity. Proc Natl Acad Sci U S A. 2004;101(26):9804–9809. doi: 10.1073/pnas.0403492101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sui J., Li W., Roberts A., Matthews L.J., Murakami A., Vogel L. Evaluation of human monoclonal antibody 80R for immunoprophylaxis of severe acute respiratory syndrome by an animal study, epitope mapping, and analysis of spike variants. J Virol. 2005;79(10):5900–5906. doi: 10.1128/JVI.79.10.5900-5906.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenough T.C., Babcock G.J., Roberts A., Hernandez H.J., Thomas W.D., Jr., Coccia J.A. Development and characterization of a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody that provides effective immunoprophylaxis in mice. J Infect Dis. 2005;191(4):507–514. doi: 10.1086/427242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sui J., Li W., Murakami A., Tamin A., Matthews L.J., Wong S.K. Potent neutralization of severe acute respiratory syndrome (SARS) coronavirus by a human mAb to S1 protein that blocks receptor association. Proc Natl Acad Sci U S A. 2004;101(8):2536–2541. doi: 10.1073/pnas.0307140101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Subbarao K., McAuliffe J., Vogel L., Fahle G., Fischer S., Tatti K. Prior infection and passive transfer of neutralizing antibody prevent replication of severe acute respiratory syndrome coronavirus in the respiratory tract of mice. J Virol. 2004;78(7):3572–3577. doi: 10.1128/JVI.78.7.3572-3577.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vennema H., Godeke G.J., Rossen J.W., Voorhout W.F., Horzinek M.C., Opstelten D.J. Nucleocapsid-independent assembly of coronavirus-like particles by co-expression of viral envelope protein genes. EMBO J. 1996;15(8):2020–2028. doi: 10.1002/j.1460-2075.1996.tb00553.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bosch B.J., de Haan C.A., Smits S.L., Rottier P.J. Spike protein assembly into the coronavirion: exploring the limits of its sequence requirements. Virology. 2005;334(2):306–318. doi: 10.1016/j.virol.2005.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ye R., Montalto-Morrison C., Masters P.S. Genetic analysis of determinants for spike glycoprotein assembly into murine coronavirus virions: distinct roles for charge-rich and cysteine-rich regions of the endodomain. J Virol. 2004;78(18):9904–9917. doi: 10.1128/JVI.78.18.9904-9917.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Haan C.A., Smeets M., Vernooij F., Vennema H., Rottier P.J. Mapping of the coronavirus membrane protein domains involved in interaction with the spike protein. J Virol. 1999;73(9):7441–7452. doi: 10.1128/jvi.73.9.7441-7452.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nguyen V.P., Hogue B.G. Protein interactions during coronavirus assembly. J Virol. 1997;71(12):9278–9284. doi: 10.1128/jvi.71.12.9278-9284.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Narayanan K., Makino S. Cooperation of an RNA packaging signal and a viral envelope protein in coronavirus RNA packaging. J Virol. 2001;75(19):9059–9067. doi: 10.1128/JVI.75.19.9059-9067.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuo L., Masters P.S. Genetic evidence for a structural interaction between the carboxy termini of the membrane and nucleocapsid proteins of mouse hepatitis virus. J Virol. 2002;76(10):4987–4999. doi: 10.1128/JVI.76.10.4987-4999.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Narayanan K., Maeda A., Maeda J., Makino S. Characterization of the coronavirus M protein and nucleocapsid interaction in infected cells. J Virol. 2000;74(17):8127–8134. doi: 10.1128/jvi.74.17.8127-8134.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sturman L.S., Holmes K.V., Behnke J. Isolation of coronavirus envelope glycoproteins and interaction with the viral nucleocapsid. J Virol. 1980;33(1):449–462. doi: 10.1128/jvi.33.1.449-462.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Narayanan K., Chen C.J., Maeda J., Makino S. Nucleocapsid-independent specific viral RNA packaging via viral envelope protein and viral RNA signal. J Virol. 2003;77(5):2922–2927. doi: 10.1128/JVI.77.5.2922-2927.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maeda J., Maeda A., Makino S. Release of coronavirus E protein in membrane vesicles from virus-infected cells and E protein-expressing cells. Virology. 1999;263(2):265–272. doi: 10.1006/viro.1999.9955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baudoux P., Carrat C., Besnardeau L., Charley B., Laude H. Coronavirus pseudoparticles formed with recombinant M and E proteins induce alpha interferon synthesis by leukocytes. J Virol. 1998;72(11):8636–8643. doi: 10.1128/jvi.72.11.8636-8643.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huang C., Ito N., Tseng C.T., Makino S. Severe acute respiratory syndrome coronavirus 7a accessory protein is a viral structural protein. J Virol. 2006;80(15):7287–7294. doi: 10.1128/JVI.00414-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mortola E., Roy P. Efficient assembly and release of SARS coronavirus-like particles by a heterologous expression system. FEBS Lett. 2004;576(1–2):174–178. doi: 10.1016/j.febslet.2004.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lu X., Chen Y., Bai B., Hu H., Tao L., Yang J. Immune responses against severe acute respiratory syndrome coronavirus induced by virus-like particles in mice. Immunology. 2007;122:496–502. doi: 10.1111/j.1365-2567.2007.02676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang Y., Yang Z.Y., Kong W.P., Nabel G.J. Generation of synthetic severe acute respiratory syndrome coronavirus pseudoparticles: implications for assembly and vaccine production. J Virol. 2004;78(22):12557–12565. doi: 10.1128/JVI.78.22.12557-12565.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuo L., Godeke G.J., Raamsman M.J., Masters P.S., Rottier P.J. Retargeting of coronavirus by substitution of the spike glycoprotein ectodomain: crossing the host cell species barrier. J Virol. 2000;74(3):1393–1406. doi: 10.1128/jvi.74.3.1393-1406.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tseng C.T., Huang C., Newman P., Wang N., Narayanan K., Watts D.M. Severe acute respiratory syndrome coronavirus infection of mice transgenic for the human Angiotensin-converting enzyme 2 virus receptor. J Virol. 2007;81(3):1162–1173. doi: 10.1128/JVI.01702-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Opstelten D.J., Raamsman M.J., Wolfs K., Horzinek M.C., Rottier P.J. Envelope glycoprotein interactions in coronavirus assembly. J Cell Biol. 1995;131(2):339–349. doi: 10.1083/jcb.131.2.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Azizi A., Anderson D.E., Ghorbani M., Gee K., Diaz-Mitoma F. Immunogenicity of a polyvalent HIV-1 candidate vaccine based on fourteen wild type gp120 proteins in golden hamsters. BMC Immunol. 2006;7:25. doi: 10.1186/1471-2172-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Argentini C., Giuseppetti R., D’Ugo E., La Sorsa V., Tritarelli E., Orobello S. A pre-S/S CHO-derived hepatitis B virus vaccine protects woodchucks from WHV productive infection. Vaccine. 2005;23(28):3649–3656. doi: 10.1016/j.vaccine.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 45.Baruch D.I., Gamain B., Miller L.H. DNA immunization with the cysteine-rich interdomain region 1 of the Plasmodium falciparum variant antigen elicits limited cross-reactive antibody responses. Infect Immun. 2003;71(8):4536–4543. doi: 10.1128/IAI.71.8.4536-4543.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Monath T.P., Soike K., Levenbook I., Zhang Z.X., Arroyo J., Delagrave S. Recombinant, chimeric live, attenuated vaccine (ChimeriVax) incorporating the envelope genes of Japanese encephalitis (SA14-14-2) virus and the capsid and nonstructural genes of yellow fever (17D) virus is safe, immunogenic and protective in non-human primates. Vaccine. 1999;17(15–16):1869–1882. doi: 10.1016/s0264-410x(98)00487-3. [DOI] [PubMed] [Google Scholar]
- 47.Yasuda A., Kimura-Kuroda J., Ogimoto M., Miyamoto M., Sata T., Sato T. Induction of protective immunity in animals vaccinated with recombinant vaccinia viruses that express PreM and E glycoproteins of Japanese encephalitis virus. J Virol. 1990;64(6):2788–2795. doi: 10.1128/jvi.64.6.2788-2795.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kapadia S.U., Rose J.K., Lamirande E., Vogel L., Subbarao K., Roberts A. Long-term protection from SARS coronavirus infection conferred by a single immunization with an attenuated VSV-based vaccine. Virology. 2005;340(2):174–182. doi: 10.1016/j.virol.2005.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen Z., Zhang L., Qin C., Ba L., Yi C.E., Zhang F. Recombinant modified vaccinia virus Ankara expressing the spike glycoprotein of severe acute respiratory syndrome coronavirus induces protective neutralizing antibodies primarily targeting the receptor binding region. J Virol. 2005;79(5):2678–2688. doi: 10.1128/JVI.79.5.2678-2688.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Spruth M., Kistner O., Savidis-Dacho H., Hitter E., Crowe B., Gerencer M. A double-inactivated whole virus candidate SARS coronavirus vaccine stimulates neutralising and protective antibody responses. Vaccine. 2006;24(5):652–661. doi: 10.1016/j.vaccine.2005.08.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tang L., Zhu Q., Qin E., Yu M., Ding Z., Shi H. Inactivated SARS-CoV vaccine prepared from whole virus induces a high level of neutralizing antibodies in BALB/c mice. DNA Cell Biol. 2004;23(6):391–394. doi: 10.1089/104454904323145272. [DOI] [PubMed] [Google Scholar]
- 52.Xiong S., Wang Y.F., Zhang M.Y., Liu X.J., Zhang C.H., Liu S.S. Immunogenicity of SARS inactivated vaccine in BALB/c mice. Immunol Lett. 2004;95(2):139–143. doi: 10.1016/j.imlet.2004.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.He Y., Zhou Y., Siddiqui P., Jiang S. Inactivated SARS-CoV vaccine elicits high titers of spike protein-specific antibodies that block receptor binding and virus entry. Biochem Biophys Res Commun. 2004;325(2):445–452. doi: 10.1016/j.bbrc.2004.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Woo P.C., Lau S.K., Tsoi H.W., Chen Z.W., Wong B.H., Zhang L. SARS coronavirus spike polypeptide DNA vaccine priming with recombinant spike polypeptide from Escherichia coli as booster induces high titer of neutralizing antibody against SARS coronavirus. Vaccine. 2005;23(42):4959–4968. doi: 10.1016/j.vaccine.2005.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.He Y., Li J., Heck S., Lustigman S., Jiang S. Antigenic and immunogenic characterization of recombinant baculovirus-expressed severe acute respiratory syndrome coronavirus spike protein: implication for vaccine design. J Virol. 2006;80(12):5757–5767. doi: 10.1128/JVI.00083-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Czub M., Weingartl H., Czub S., He R., Cao J. Evaluation of modified vaccinia virus Ankara based recombinant SARS vaccine in ferrets. Vaccine. 2005;23(17–18):2273–2279. doi: 10.1016/j.vaccine.2005.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kuate S., Cinatl J., Doerr H.W., Uberla K. Exosomal vaccines containing the S protein of the SARS coronavirus induce high levels of neutralizing antibodies. Virology. 2007 doi: 10.1016/j.virol.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee J.S., Poo H., Han D.P., Hong S.P., Kim K., Cho M.W. Mucosal immunization with surface-displayed severe acute respiratory syndrome coronavirus spike protein on Lactobacillus casei induces neutralizing antibodies in mice. J Virol. 2006;80(8):4079–4087. doi: 10.1128/JVI.80.8.4079-4087.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haijema B.J., Volders H., Rottier P.J. Switching species tropism: an effective way to manipulate the feline coronavirus genome. J Virol. 2003;77(8):4528–4538. doi: 10.1128/JVI.77.8.4528-4538.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Godeke G.J., de Haan C.A., Rossen J.W., Vennema H., Rottier P.J. Assembly of spikes into coronavirus particles is mediated by the carboxy-terminal domain of the spike protein. J Virol. 2000;74(3):1566–1571. doi: 10.1128/jvi.74.3.1566-1571.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Noad R., Roy P. Virus-like particles as immunogens. Trends Microbiol. 2003;11(9):438–444. doi: 10.1016/s0966-842x(03)00208-7. [DOI] [PubMed] [Google Scholar]
- 62.Grgacic E.V., Anderson D.A. Virus-like particles: passport to immune recognition. Methods. 2006;40(1):60–65. doi: 10.1016/j.ymeth.2006.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.ter Meulen J., Bakker A.B., van den Brink E.N., Weverling G.J., Martina B.E., Haagmans B.L. Human monoclonal antibody as prophylaxis for SARS coronavirus infection in ferrets. Lancet. 2004;363(9427):2139–2141. doi: 10.1016/S0140-6736(04)16506-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Du L., Zhao G., He Y., Guo Y., Zheng B.J., Jiang S. Receptor-binding domain of SARS-CoV spike protein induces long-term protective immunity in an animal model. Vaccine. 2007;25(15):2832–2838. doi: 10.1016/j.vaccine.2006.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Du L., He Y., Wang Y., Zhang H., Ma S., Wong C.K. Recombinant adeno-associated virus expressing the receptor-binding domain of severe acute respiratory syndrome coronavirus S protein elicits neutralizing antibodies: implication for developing SARS vaccines. Virology. 2006;353(1):6–16. doi: 10.1016/j.virol.2006.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bisht H., Roberts A., Vogel L., Subbarao K., Moss B. Neutralizing antibody and protective immunity to SARS coronavirus infection of mice induced by a soluble recombinant polypeptide containing an N-terminal segment of the spike glycoprotein. Virology. 2005;334(2):160–165. doi: 10.1016/j.virol.2005.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roberts A., Thomas W.D., Guarner J., Lamirande E.W., Babcock G.J., Greenough T.C. Therapy with a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody reduces disease severity and viral burden in golden Syrian hamsters. J Infect Dis. 2006;193(5):685–692. doi: 10.1086/500143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Deming D., Sheahan T., Heise M., Yount B., Davis N., Sims A. Vaccine efficacy in senescent mice challenged with recombinant SARS-CoV bearing epidemic and zoonotic spike variants. PLoS Med. 2006;3(12):e525. doi: 10.1371/journal.pmed.0030525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vennema H., de Groot R.J., Harbour D.A., Dalderup M., Gruffydd-Jones T., Horzinek M.C. Early death after feline infectious peritonitis virus challenge due to recombinant vaccinia virus immunization. J Virol. 1990;64(3):1407–1409. doi: 10.1128/jvi.64.3.1407-1409.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Perlman S., Dandekar A.A. Immunopathogenesis of coronavirus infections: implications for SARS. Nat Rev Immunol. 2005;5(12):917–927. doi: 10.1038/nri1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Weiss R.C., Scott F.W. Antibody-mediated enhancement of disease in feline infectious peritonitis: comparisons with dengue hemorrhagic fever. Comp Immunol Microbiol Infect Dis. 1981;4(2):175–189. doi: 10.1016/0147-9571(81)90003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Olsen C.W., Corapi W.V., Ngichabe C.K., Baines J.D., Scott F.W. Monoclonal antibodies to the spike protein of feline infectious peritonitis virus mediate antibody-dependent enhancement of infection of feline macrophages. J Virol. 1992;66(2):956–965. doi: 10.1128/jvi.66.2.956-965.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Corapi W.V., Olsen C.W., Scott F.W. Monoclonal antibody analysis of neutralization and antibody-dependent enhancement of feline infectious peritonitis virus. J Virol. 1992;66(11):6695–6705. doi: 10.1128/jvi.66.11.6695-6705.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang Z.Y., Werner H.C., Kong W.P., Leung K., Traggiai E., Lanzavecchia A. Evasion of antibody neutralization in emerging severe acute respiratory syndrome coronaviruses. Proc Natl Acad Sci U S A. 2005;102(3):797–801. doi: 10.1073/pnas.0409065102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kong W.P., Xu L., Stadler K., Ulmer J.B., Abrignani S., Rappuoli R. Modulation of the immune response to the severe acute respiratory syndrome spike glycoprotein by gene-based and inactivated virus immunization. J Virol. 2005;79(22):13915–13923. doi: 10.1128/JVI.79.22.13915-13923.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McCray P.B., Jr., Pewe L., Wohlford-Lenane C., Hickey M., Manzel L., Shi L. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J Virol. 2007;81(2):813–821. doi: 10.1128/JVI.02012-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rockx B., Sheahan T., Donaldson E., Harkema J., Sims A., Heise M. Synthetic reconstruction of zoonotic and early human severe acute respiratory syndrome coronavirus isolates that produce fatal disease in aged mice. J Virol. 2007;81(14):7410–7423. doi: 10.1128/JVI.00505-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Roberts A., Vogel L., Guarner J., Hayes N., Murphy B., Zaki S. Severe acute respiratory syndrome coronavirus infection of golden Syrian hamsters. J Virol. 2005;79(1):503–511. doi: 10.1128/JVI.79.1.503-511.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Martina B.E., Haagmans B.L., Kuiken T., Fouchier R.A., Rimmelzwaan G.F., Van Amerongen G. Virology: SARS virus infection of cats and ferrets. Nature. 2003;425(6961):915. doi: 10.1038/425915a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Thompson J.D., Higgins D.G., Gibson T.J. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 1994;22(22):4673–4680. doi: 10.1093/nar/22.22.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]


