Abstract
Serotonin (5-HT) has been implicated in the pathogenesis of pulmonary arterial hypertension (PAH). We hypothesized that plasma 5-HT would be elevated in PAH related to associated conditions.
We performed a prospective cohort study of 21 patients with PAH undergoing initial right heart catheterization and 6 healthy controls.
Platelet-free plasma 5-HT levels were similar in patients with idiopathic PAH, PAH related to associated conditions, and healthy controls. Higher 5-HT levels correlated with increased six-minute walk distance (r = 0.55, p = 0.04).
These data suggest that plasma 5-HT levels are normal in PAH. Plasma 5-HT may therfore not be a useful biomarker in this condition.
Keywords: 5-hydroxytryptamine, Cohort, Pulmonary arterial hypertension, Serotonin, Six-minute walk testing
Introduction
Serotonin (5-HT) is a potent pulmonary vasoconstrictor and platelet aggregator that has been implicated in the pathophysiology of pulmonary arterial hypertension (PAH). Most human circulating 5-HT is stored in platelets, while only platelet-free plasma 5-HT has potent vascular activity. Two previous studies (N=16 each) have shown increased plasma 5-HT levels in patients with idiopathic PAH (IPAH) [1, 2]. In addition, a 5-HT promoter polymorphism has been associated with the risk of PAH in one population, although this association was not seen in another population [3-5]. We therefore hypothesized that plasma 5-HT levels would be significantly elevated in PAH related to associated conditions (APAH).
Methods
We performed a prospective cohort study of patients with PAH undergoing initial right heart catheterization at our center beginning in November 2001. We excluded patients already receiving targeted PAH treatment. We also included age- and gender-matched healthy controls. The Columbia University Institutional Review Board approved the study.
A bionutritionist counseled subjects to avoid 5-HT-rich foods, alcohol and coffee for 48 hours before phlebotomy; subjects recorded foods eaten during this period. No subjects received anti-platelet agents. After an overnight fast, blood was withdrawn using minimal tourniquet technique and suction. Blood was immediately centrifuged for 10 minutes at 200 × g at room temperature to obtain platelet-rich plasma, and then at 4500 × g for 10 minutes at 4°C to obtain platelet-free plasma. Plasma was stored at −80°C until analysis by ELISA (IBL, Hamburg, Germany). Cross-reactivity with related substances (e.g., 5-HIAA, DL-tryptophan, and melatonin) has been reported to be ≤ 0.12%. Results were read from a standard curve. The threshold of detection was 0.01 nmol/L.
Data were summarized by mean ± standard deviation, median and interquartile range, or frequency (percentage). Kruskal-Wallis tests, Wilcoxon rank sum and signed rank tests, and Spearman's correlation coefficients were used. Sixteen APAH patients and 6 controls provided more than 95% power to detect the differences in plasma 5-HT observed in previous studies [1, 2].
Results
We enrolled 28 PAH patients and 8 controls; 21 patients and 6 controls were compliant with dietary restrictions and comprised the final study sample (Table). Two PAH patients had collagen vascular disease, 3 had HIV, 5 had congenital cardiac shunts (2 repaired), 6 had portopulmonary hypertension, and 5 had IPAH.
Table.
Demographic and clinical characteristics
| Variable | IPAH (n=5) |
APAH (n=16) |
Controls (n=6) |
p value |
|---|---|---|---|---|
| Age, years | 45 ± 19 | 41 ± 12 | 34 ± 5 | 0.20 |
| Female, n (%) | 4 (80%) | 15 (94%) | 4 (67%) | 0.24 |
| Race/Ethnicity, n (%) | 0.56 | |||
| White/Non-Hispanic | 4 (80%) | 8 (50%) | 6 (100%) | |
| White/Hispanic | 0 (0%) | 3 (19%) | 0 (0%) | |
| Black/Non-Hispanic | 0 (0%) | 3 (19%) | 0 (0%) | |
| Black/Hispanic | 0 (0%) | 1 (6%) | 0 (0%) | |
| Asian/Non-Hispanic | 1 (20%) | 1 (6%) | 0 (0%) | |
| Body mass index, kg/m2 | 30 ± 8 | 26 ± 6 | 25 ± 5 | 0.47 |
| NYHA class, n (%) | 0.15 | |||
| II | 0 (0%) | 4 (25%) | ||
| III | 4 (80%) | 12 (75%) | ||
| IV | 1 (20%) | 0 | ||
| Mean right atrial pressure, mm Hg | 8 ± 3 | 9 ± 6 | 0.53 | |
| Mean pulmonary artery pressure, mm Hg | 63 ± 12 | 58 ± 14 | 0.48 | |
| Pulmonary vascular resistance, dynes·sec·cm−5 |
1467 ± 832 | 1425 ± 753 | 0.90 | |
| Cardiac index, liters/min/m2 | 1.7 ± 0.3 | 2.0 ± 0.7 | 0.39 | |
| Oxygen consumption at peak exercise, ml/min/kg |
9.6 ± 0.6 | 11.0 ± 4.5 | 1.0 | |
| Six-minute walk distance, meters | 364 ± 146 | 341 ± 122 | 0.80 |
Data are presented as mean ± sd and frequency (percentage). NYHA: New York Heart Association.
Patients with APAH did not have elevated plasma 5-HT levels compared to controls (Figure 1; p = 0.51). Patients with IPAH also had 5-HT levels similar to those of controls. In fact, only 1 PAH patient had an elevated platelet-free plasma serotonin level (kit manufacturer's upper limit of normal [97.5th percentile] = 1.3 nmol/L). There were no differences in plasma 5-HT levels between individual APAH diagnoses and controls (p > 0.15). When we analyzed all PAH patients regardless of diet restrictions (therefore potentially increasing plasma 5-HT levels), we still found no difference between PAH patients and controls (mean 5-HT level = 0.81, 0.65, and 0.63 nmol/L for APAH (n=19), IPAH (n=9), and controls, respectively, p = 0.63).
Figure 1.
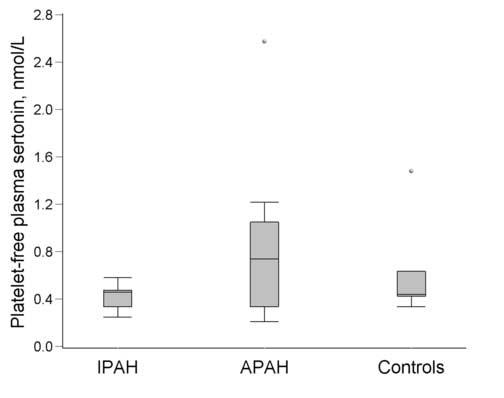
Platelet-free plasma serotonin levels for IPAH, APAH, and controls: median (line) and interquartile range (box). Whiskers are 1.5x the interquartile range. Filled circles are outliers.
There was an inverse association between the 5-HT level and right atrial pressure of borderline significance (r = −0.44, p = 0.09) and a direct association between 5-HT and the six-minute walk distance (r = 0.55, p = 0.04), but no associations with other indicators of disease severity.
Discussion
We found that patients with APAH and IPAH had plasma 5-HT levels that were similar to those of healthy controls. These results differ from those of previous studies in which PAH was associated with dramatically higher 5-HT levels (>30 nmol/L) [1, 2]. There are a number of possible explanations for these discrepant findings.
First, we specifically focused on patients with APAH, whereas prior studies predominantly included patients with IPAH. Of note, however, 5-HT levels were also normal in patients with IPAH in our study.
Second, the patients in the current study may have differed from those of prior studies. Hemodynamics in our study were similar to those in previous studies, making substantial differences in the stage of disease unlikely [1, 2]. Also, higher levels of 5-HT, if anything, were associated with milder PAH and better exercise capacity in our study. Our patients were ethnically heterogeneous compared to those in prior studies, which could explain the disparate findings.
Third, our sample size for APAH was equal to those of the prior studies that showed elevated 5-HT levels, and we had more than adequate power to detect the dramatic elevations in 5-HT previously seen. Therefore, the small sample size does not account for our findings.
Finally, it is possible that differences in laboratory assays or technique explain our findings in comparison to previous work. The highly sensitive nature of assessing platelet-free plasma serotonin has led to studies showing great variation in plasma 5-HT levels [6-10]. We tried to take extensive precautions to prevent such variability. In addition, although we used an ELISA assay rather than the radioenzymatic assay used in prior studies, it is unlikely that this explains the log difference in 5-HT levels for PAH patients between studies.
Our results and the previous studies of plasma 5-HT levels in PAH should be interpreted cautiously. Our finding of normal plasma 5-HT levels in PAH does not necessarily discount an important role for 5-HT in PAH. 5-HT production in the small pulmonary arteries may still have significant paracrine effects, inviting potential medical interventions such as selective serotonin reuptake inhibitors [11-13]. However, in contrast to previously published studies, our data suggest that the platelet-free plasma level of 5-HT may be normal in patients with PAH and hence may not be an adequate disease biomarker. Future investigation of the serotonergic pathway in PAH should continue to focus on the local pulmonary vascular action of 5-HT.
Acknowledgements
The authors wish to thank May Huang, MS and the staff of the Irving Center for Clinical Research staff at Columbia University for their assistance with this study.
Funded by NIH HL67771, HL072739, HL082895, and RR00645.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Herve P, Launay JM, Scrobohaci ML, Brenot F, Simonneau G, Petitpretz P, Poubeau P, Cerrina J, Duroux P, Drouet L. Increased plasma serotonin in primary pulmonary hypertension. Am J Med. 1995;99:249–254. doi: 10.1016/s0002-9343(99)80156-9. [DOI] [PubMed] [Google Scholar]
- 2.Kereveur A, Callebert J, Humbert M, Herve P, Simonneau G, Launay JM, Drouet L. High plasma serotonin levels in primary pulmonary hypertension. Effect of long-term epoprostenol (prostacyclin) therapy. Arterioscler Thromb Vasc Biol. 2000;20:2233–2239. doi: 10.1161/01.atv.20.10.2233. [DOI] [PubMed] [Google Scholar]
- 3.Eddahibi S, Humbert M, Fadel E, Raffestin B, Darmon M, Capron F, Simonneau G, Dartevelle P, Hamon M, Adnot S. Serotonin transporter overexpression is responsible for pulmonary artery smooth muscle hyperplasia in primary pulmonary hypertension. J Clin Invest. 2001;108:1141–1150. doi: 10.1172/JCI12805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Machado RD, Koehler R, Glissmeyer E, Veal C, Suntharalingam J, Kim M, Carlquist J, Town M, Elliott CG, Hoeper M, Fijalkowska A, Kurzyna M, Thomson JR, Gibbs SR, Wilkins MR, Seeger W, Morrell NW, Gruenig E, Trembath RC, Janssen B. Genetic association of the serotonin transporter in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2006;173:793–797. doi: 10.1164/rccm.200509-1365OC. [DOI] [PubMed] [Google Scholar]
- 5.Willers ED, Newman JH, Loyd JE, Robbins IM, Wheeler LA, Prince MA, Stanton KC, Cogan JA, Runo JR, Byrne D, Humbert M, Simonneau G, Sztrymf B, Morse JA, Knowles JA, Roberts KE, McElroy JJ, Barst RJ, Phillips JA., 3rd Serotonin transporter polymorphisms in familial and idiopathic pulmonary arterial hypertension. Am J Respir Crit Care Med. 2006;173:798–802. doi: 10.1164/rccm.200509-1361OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gustafsson BI, Tommeras K, Nordrum I, Loennechen JP, Brunsvik A, Solligard E, Fossmark R, Bakke I, Syversen U, Waldum H. Long-term serotonin administration induces heart valve disease in rats. Circulation. 2005;111:1517–1522. doi: 10.1161/01.CIR.0000159356.42064.48. [DOI] [PubMed] [Google Scholar]
- 7.Gijsman HJ, Verkes RJ, Schouten-Verhagen JC, Schoemaker RC, Van Gerven JM, De Rijk RH, Van Kempen GM. Estimation of plasma serotonin using isopycnic centrifugation. Hum Psychopharmacol. 2000;15:417–421. doi: 10.1002/1099-1077(200008)15:6<417::AID-HUP210>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 8.Lechin F, van der Dijs B, Orozco B, Lechin M, Lechin AE. Increased levels of free serotonin in plasma of symptomatic asthmatic patients. Ann Allergy Asthma Immunol. 1996;77:245–253. doi: 10.1016/S1081-1206(10)63263-2. [DOI] [PubMed] [Google Scholar]
- 9.Paez X, Hernandez L. Plasma serotonin monitoring by blood microdialysis coupled to high-performance liquid chromatography with electrochemical detection in humans. J Chromatogr B Biomed Sci Appl. 1998;720:33–38. doi: 10.1016/s0378-4347(98)00417-4. [DOI] [PubMed] [Google Scholar]
- 10.Rothman RB, Redmon JB, Raatz SK, Kwong CA, Swanson JE, Bantle JP. Chronic treatment with phentermine combined with fenfluramine lowers plasma serotonin. Am J Cardiol. 2000;85:913–915. doi: 10.1016/s0002-9149(99)00896-6. A910. [DOI] [PubMed] [Google Scholar]
- 11.Eddahibi S, Guignabert C, Barlier-Mur AM, Dewachter L, Fadel E, Dartevelle P, Humbert M, Simonneau G, Hanoun N, Saurini F, Hamon M, Adnot S. Cross talk between endothelial and smooth muscle cells in pulmonary hypertension. Critical role for serotonin-induced smooth muscle hyperplasia. Circulation. 2006;113:1857–1864. doi: 10.1161/CIRCULATIONAHA.105.591321. [DOI] [PubMed] [Google Scholar]
- 12.Kawut SM, Horn EM, Berekashvili KK, Lederer DJ, Widlitz AC, Rosenzweig EB, Barst RJ. Selective serotonin reuptake inhibitor use and outcomes in pulmonary arterial hypertension. Pulm Pharmacol Ther. 2006;19:370–374. doi: 10.1016/j.pupt.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Serotonin Transporter Inhibitor Escitalopram in Pulmonary Hypertension. http://clinicaltrials.gov/ct/show/NCT00190333. Accessed on: December 10, 2006.


