Abstract
GPR119 is a G protein-coupled receptor expressed predominantly in the pancreas (β-cells) and gastrointestinal tract (enteroendocrine cells) in humans. De-orphanization of GPR119 has revealed two classes of possible endogenous ligands, viz., phospholipids and fatty acid amides. Of these, oleoylethanolamide (OEA) is one of the most active ligands tested so far. This fatty acid ethanolamide is of particular interest because of its known effects of reducing food intake and body weight gain when administered to rodents. Agonists at the GPR119 receptor cause an increase in intracellular cAMP levels via Gαs coupling to adenylate cyclase. In vitro studies have indicated a role for GPR119 in the modulation of insulin release by pancreatic β-cells and of GLP-1 secretion by gut enteroendocrine cells. The effects of GPR119 agonists in animal models of diabetes and obesity are reviewed, and the potential value of such compounds in future therapies for these conditions is discussed.
Keywords: GPR119, oleoylethanolamide, GLP-1, anti-diabetic agents, anti-obesic agents, drug discovery
Introduction
One of the reasons for the growing public health concern over the rapidly increasing prevalence of obesity in Westernized society and in some developing countries (Stein and Colditz, 2004) is its association with the growing incidence of type II diabetes, a combination of conditions often accompanied by increased cardiovascular risk factors (Bailey, 2005). Much effort among health-care providers and pharmaceutical companies is now focused on the discovery of new treatments that alleviate this medical problem.
As part of this effort, the G-protein-coupled receptor GPR119 has recently attracted attention because of evidence from in vitro systems and animal models that its modulation may produce favourable effects on glucose homoeostasis, food intake/body weight gain and possibly also β-cell preservation. In other words, GPR119 modulators may influence parameters related to both diabetes and obesity.
The aim of this review is to summarize currently available information on the biology of GPR119, including tissue localization, possible endogenous ligands, biological functions and potential value as a therapeutic target. Literature concerning synthetic, small-molecule ligands of GPR119 has recently been reviewed by Fyfe et al. (2007a).
The GPR119 receptor
GPR119 was described by Fredriksson et al. (2003) as a class 1 (rhodopsin-type) orphan G-protein-coupled receptor having no close primary sequence relative in the human genome. Independently, GPR119 has been studied and described in the literature under various synonyms including SNORF25 (Bonini et al., 2001, 2002), RUP3 (Jones et al., 2004), GPCR2 (Takeda et al., 2002), 19AJ (Davey, 2004), OSGPR116 (Griffin, 2006) and glucose-dependent insulinotropic receptor (Chu et al., 2007b, 2007c). Isoforms of GPR119 have been identified in a number of mammalian species, including rats, mice, hamsters, chimpanzees, rhesus monkeys, cattle and dogs. Fredriksson et al. (2003) describe the rat isoform of GPR119 (accession number AY288429) as being 133 amino acids longer than the mouse and human receptors (468 vs 335 amino acids). In contrast, Bonini et al. (2001, 2002) (accession number AR240217) and Ohishi et al. (2003) give identical sequences for the rat receptor, which are 335 amino acids in length and have 96% amino-acid identity with mouse GPR119. Therefore, it appears likely that the additional C-terminal sequence reported by Fredriksson et al. (2003) may be an artefact. Phylogenetic analysis by Fredriksson et al. (2003) assigned GPR119 to a new subgroup within the bioamine receptors. In contrast, homology clustering analysis by Griffin (2006) showed the closest relatives of GPR119 to be the cannabinoid receptors.
Several studies have evaluated the tissue distribution of GPR119 expression using quantitative real-time PCR or hybridization analysis. The pancreas (Figure 1a) and fetal liver have been consistently identified as major sites of mRNA expression in human tissues, with expression also being seen in the gastrointestinal tract in some studies (Bonini et al., 2001; Jones et al., 2004; Soga et al., 2005; Griffin, 2006). Bonini et al. (2001, 2002) detected GPR119 mRNA in most of the rat and mouse tissues examined, with the pancreas and gastrointestinal tract appearing as major sites of expression. In contrast to human tissues, high levels of expression were seen in many areas of the rat brain, including cerebellum, cerebral cortex, choroid plexus, dorsal root ganglion, hippocampus and hypothalamus. Jones et al. (2004) reported strong GPR119 expression in rat pancreas and hypothalamus, while rat pancreatic expression was confirmed by Soga et al. (2005). GPR119 mRNA expression in isolated pancreatic islets has been reported by Jones et al. (2004), Soga et al. (2005) and Chu et al. (2007a). By using in situ hybridization and immunofluorescent staining with a GPR119-specific antiserum (showing predominant colocalization of GPR119 with insulin), Chu et al. (2007a) concluded that β-cells are the main site of GPR119 expression in the rodent islet. However, receptor expression in a subset of α-cells or in other islet cell types could not be ruled out. Evidence of GPR119 expression in β-cell-derived insulinoma cell lines, such as HIT-T15 (Figure 1a; Chu et al., 2006, 2007a; Fyfe et al., 2006, 2007b), NIT-1, MIN6 and RIN5 (Soga et al., 2005), is consistent with the β-cell being a site of expression within the pancreatic islet. Contrary evidence has been presented by Sakamoto et al. (2006), where immunofluorescence studies with an anti-peptide antiserum revealed the pancreatic polypeptide-secreting cells as the only site of GPR119 expression in mouse and rat islets. Chu et al. (2006) have confirmed the expression of GPR119 mRNA in the colon and small intestine of mouse using an RNase protection assay and also demonstrated its presence in the mouse enteroendocrine, L-cell-derived, GLUTag cell line (Drucker et al., 1994) by northern blot. The latter finding has been independently confirmed using PCR by Fyfe et al. (2007b). Whether GPR119 is expressed in any other intestinal cell types is unknown at present.
Figure 1.
The hamster insulinoma cell line HIT-T15 as a model of insulin-secreting pancreatic β-cells (data kindly provided by Dr J White, (OSI) Prosidion). (a) Expression of GPR119 mRNA in pancreatic tissue and HIT-T15 cells, detected by reverse transcription-PCR using primers representing sequences showing 100% identity between human, rat and mouse GPR119 genes, is shown. (b) Intracellular cyclic AMP levels in HIT-T15 cells treated for 30 min with the GPR119 agonist PSN632408 are shown (Overton et al., 2006). cAMP was determined using the Perkin Elmer AlphaScreen cAMP kit.
Cells transfected with GPR119 show an increase in constitutive intracellular cAMP levels (Bonini et al., 2001; Ohishi et al., 2003; Chu et al., 2007a), implying that the receptor functions via coupling to Gαs, which leads to the stimulation of adenylate cyclase. In support of these data, potential endogenous ligands (see ‘De-orphanization of GPR119') and synthetic small-molecule agonists of GPR119 (Figure 1b; Ohishi et al., 2003; Jones et al., 2004; Fyfe et al., 2006, 2007b; Overton et al., 2006; Chu et al., 2007a) have been shown to increase cAMP concentrations in cells expressing GPR119 either endogenously or following stable or transient transfection. Furthermore, Chu et al. (2007a) have demonstrated that GPR119 exhibits poor coupling efficiency to Gαi and Gαq, indicating a selective interaction with Gαs.
De-orphanization of GPR119
The first molecule to be described as a potential endogenous ligand of GPR119 was all-trans retinoic acid (Bonini et al., 2001). Treatment of GPR119-transfected Cos-7 cells with all-trans retinoic acid was reported to produce a dose-dependent increase in intracellular cAMP (EC50=909 nM, Emax=202% of basal). However, Griffin (2006) and colleagues were unable to detect any activity for all-trans retinoic acid (concentration range 10 nM–10 μM) in a Gα16-driven reporter assay using human embryonic kidney cells transiently expressing GPR119.
A number of phospholipid molecules have been reported to act as GPR119 agonists. Bonini et al. (2002) indicated that platelet-activating factor (1-O-alkyl-2-acetyl-sn-glycero-3-phosphocholine) and lyso-platelet activating factor (1-O-alkyl-sn-glycero-3-phosphocholine) both raised cAMP levels in Chinese hamster ovary cells stably expressing GPR119. Soga et al. (2005) identified five phospholipids (the oleoyl, stearoyl and palmitoyl forms of lysophosphatidylcholine (LPC), lysophosphatidylethanolamine and lysophosphatidylinositol) that produced elevated cAMP levels in rat hepatoma cells stably expressing GPR119, but were unable to confirm the activity of lyso-platelet activating factor reported by Bonini et al. (2002). The action of oleoyl LPC as a GPR119 agonist has been confirmed in a yeast-based reporter assay by Overton et al. (2006). Moreover, LPC has been reported to stimulate insulin release from neonatal rat islet cells (Fujimoto and Metz, 1987), and a possible role for GPR119 in this effect is suggested by its β-cell localization.
Because of the remote sequence relationship between GPR119 and the cannabinoid receptors, for which the fatty acid ethanolamide anandamide (arachidonyl ethanolamide) is an endogenous ligand, a series of related fatty acid amides was tested for agonist activity in a yeast reporter assay (Griffin, 2006; Overton et al., 2006). Although anandamide exhibited only minimal activity at GPR119, ethanolamides bearing less unsaturated fatty acid moieties showed superior activities, with oleoylethanolamide (OEA) being the most efficacious agonist tested. Treatment with OEA was shown to stimulate cAMP production in stably transfected and endogenous GPR119-expressing cell lines (Fyfe et al., 2006; Overton et al., 2006). The identification of OEA as a potential endogenous ligand for GPR119 was of particular interest, since this compound has been reported to produce a number of pharmacological effects in rodent studies, including reduction of food intake and body weight gain through activation of peroxisome proliferator-activated receptor α (Rodriguez de Fonseca et al., 2001; Fu et al., 2003), modifying feeding behaviour and motor activity through activation of the transient receptor potential vanilloid type 1 receptor (Proulx et al., 2005) and increasing fatty acid uptake by adipocytes and enterocytes through increased fatty acid translocase expression (Yang et al., 2007). It has been suggested that the reported effects of OEA on feeding may be mediated in part by GPR119 in view of the gastrointestinal localization of this receptor (Overton et al., 2006; Fyfe et al., 2007b; see ‘GPR119 agonists and obesity').
The endovanilloid compounds N-oleoyldopamine and olvanil have recently been described as GPR119 agonists with in vitro potencies similar to that of OEA (Chu et al., 2007c). These three compounds are the most potent natural GPR119 agonists reported so far, and are hence the best candidates for endogenous ligands, although they are less potent and selective than the natural ligands identified for many GPCRs. Nevertheless, they may accumulate locally at high concentrations in vivo, for instance, in the case of OEA, in the small intestine, which is known to be a site of its synthesis (Rodriguez de Fonseca et al., 2001) and also of high GPR119 expression. It is of course possible that further potential endogenous ligands remain to be identified.
GPR119 agonists and glucose homoeostasis
The expression of GPR119 in pancreatic islet β-cells led to the hypothesis that this receptor could play a role in the modulation of insulin secretion. In principle, a molecule acting via GPR119 to raise intracellular cAMP concentrations in pancreatic β-cells would be expected to potentiate glucose-stimulated insulin secretion (GSIS) in a manner analogous to that of the incretin hormones glucagon-like peptide-1 (GLP-1) and gastric inhibitory polypeptide/glucose-dependent insulinotropic peptide (GIP), which also act via Gαs-coupled, β-cell receptors (Furman et al., 2004). The insulinotropic actions of GPR119 agonists have been revealed in a number of in vitro systems. For instance, Soga et al. (2005) demonstrated that oleoyl LPC enhanced GSIS from both the perfused rat pancreas and the NIT-1 mouse β-cell line. The insulinotropic effects of oleoyl LPC were attenuated in the presence of either an adenylate cyclase inhibitor or a GPR119-selective siRNA. Lan et al. (2007) reported that oleoyl LPC potentiated GSIS by mouse pancreatic islets, in contrast to islets from GPR119-deficient mice, where no insulin secretion was seen. Chu et al. (2007a) showed enhancement of GSIS in HIT-T15 (hamster insulinoma) cells and in isolated rat and mouse islets using the selective small-molecule GPR119 agonist AR231453. No effect of this compound could be seen in islets isolated from GPR119-deficient mice.
The presence of GPR119 in the enteroendocrine GLUTag cell line noted above (Chu et al., 2006; Fyfe et al., 2007b) suggests that intestinally expressed receptor may also be involved in glucose homoeostasis via the modulation of incretin hormone release. GLUTag cells are known to secrete the incretin hormone GLP-1, and they respond to the signals controlling GLP-1 release in a similar manner to primary intestinal L cells (Brubaker et al., 1998). Small-molecule GPR119 agonists have been shown to elevate cAMP levels and stimulate GLP-1 secretion from GLUTag cells. Moreover, they increase plasma GLP-1 levels acutely when administered to rodents (Chu et al., 2006; Fyfe et al., 2007b). Furthermore, a small-molecule GPR119 agonist has been reported to stimulate the release of both GLP-1 and GIP in wild-type, but not GPR119-deficient, mice (Chu et al., 2007b). This result suggests that GPR119 may be expressed in GIP-secreting K cells, but this has not yet been demonstrated directly. Hence, GPR119 agonists might exert a twofold effect in lowering blood glucose, acting directly at the pancreatic β-cell to promote GSIS and, indirectly, via the enteroendocrine cells, by stimulating the release of the incretin hormones GLP-1 and GIP, which are powerful anti-hyperglycaemic agents (Drucker, 2001; Meier et al., 2002a; Gromada et al., 2004). It should be noted that, while part of the mechanism of GLP-1-dependent blood glucose lowering may depend on a direct insulinotropic effect on the β-cell, GLP-1 also exerts its actions by suppressing meal-associated glucagon secretion and regulating delivery of food to the gut by reducing gastric motility (see reviews by Holst and Deacon, 2005; Holst, 2006; Drucker, 2006, 2007).
Several studies have reported that small-molecule GPR119 agonists can suppress glucose excursions when administered during oral glucose tolerance tests in both normoglycaemic and hyperglycaemic rodent models (Ohishi et al., 2003; Jones et al., 2004; Chu et al., 2006, 2007a; Fyfe et al., 2007b). The anti-hyperglycaemic actions of GPR119 agonists were lost in GPR119-deficient mice (Chu et al., 2007a). The ability of GPR119 agonists to improve glycaemic control was reduced following either intraperitoneal or intravenous administration of glucose (Chu et al., 2007a; Fyfe et al., 2007b). This implies that little of the effect seen in the oral glucose tolerance test may be achieved by direct stimulation of GSIS at the pancreatic β-cell, and suggests incretin mediation of the response.
GPR119 agonists and obesity
As noted above, the idea that GPR119 modulation might provide the basis for an anti-obesity therapy was first suggested by the effects of its endogenous ligand, OEA, on feeding and body weight (Overton et al., 2006). Lan et al. (2007), however, reported that OEA was able to suppress food intake to a similar extent in both wild-type and GPR119-deficient mice. Nevertheless, as OEA is a relatively non-selective and low-potency GPR119 agonist, it is conceivable that its GPR119-specific effects would be masked in such a model.
The demonstration that GPR119 agonists stimulate the release of GLP-1 lends further credence to these agents having an effect on body weight, since GLP-1 is known to cause gastric deceleration and increase satiety, phenomena that lead to reduced caloric intake and weight loss in both animal models and human subjects (Meier et al., 2002b; Zander et al., 2002; Nielsen 2005). Possibly as a result of their effects on GLP-1 secretion, selective small-molecule GPR119 agonists inhibit gastric emptying and suppress food intake upon acute dosing to rats, with no indication of drug-induced malaise or conditioned taste aversion (Fyfe et al., 2006, 2007b; Overton et al., 2006). The hypophagic actions of GPR119 agonists lead to reduced weight gain, fat pad masses and plasma leptin/triglyceride levels when administered sub-chronically in rodent models of obesity (Fyfe et al., 2006, 2007b; Overton et al., 2006). The testing of potent, selective agonists for food intake and body weight effects in GPR119-deficient mouse models has not been reported so far.
Possible applications to drug discovery
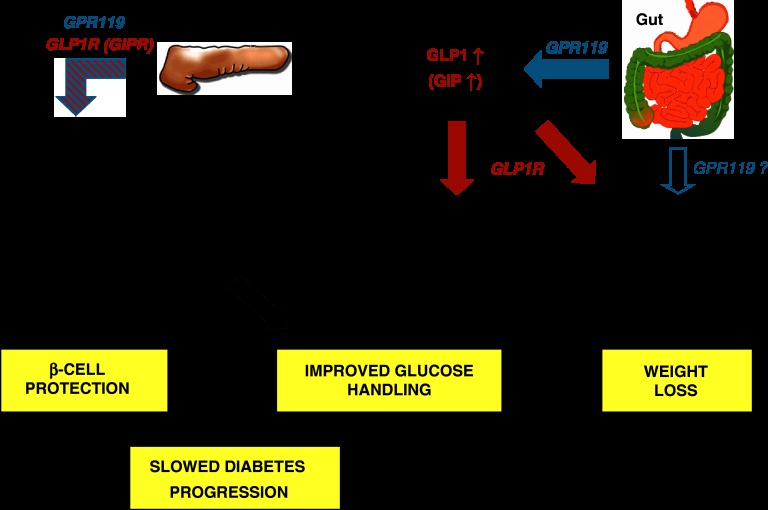
Current publicly available data on the effects of GPR119 agonists in animal models indicate that they could prove valuable agents for the treatment of type 2 diabetes and obesity by improving glucose homoeostasis while concurrently limiting food intake and body weight gain. Although the details of their mechanism of action are not yet understood fully, it appears that their ability to stimulate GLP-1 secretion from intestinal L-cells may be important for these observed effects, as summarized in Figure 2.
Figure 2.
Proposed mechanisms of GPR119 agonist action. See text for further explanation.
Modulation of the GLP-1 receptor has attracted much attention as a means of improving glycaemic control in type 2 diabetes patients (see reviews from Holst and Deacon, 2005; Drucker, 2006, 2007; Holst, 2006). Such treatments have the advantage of minimizing the risk of hypoglycaemia, since the actions of GLP-1 are glucose-dependent and diminish as blood glucose levels are normalized. As GLP-1 is rapidly rendered inactive by the dipeptidyl peptidase IV enzyme, current approaches fall into two classes: (a) injection of an ‘incretin mimetic', that is, a peptidic GLP-1 receptor agonist resistant to degradation by dipeptidyl peptidase IV and (b) inhibition of dipeptidyl peptidase IV to preserve endogenous GLP-1 in its active form. While treatment with dipeptidyl peptidase IV inhibitors appears to have no effect on body weight, the injectable incretin mimetics have been demonstrated to produce weight loss in addition to their effects on glycaemic control (Nielsen, 2005). This combination of actions could be of particular therapeutic value, since weight loss is known to be beneficial in the control of type II diabetes and is difficult to achieve during treatment with many other glucose-lowering agents (Bailey, 2005). Using a GPR119 agonist to stimulate secretion of endogenous GLP-1 may provide a third approach, giving improved glycaemic control and associated weight loss through an oral dosing regime. The ability of GPR119 agonists to elicit GIP secretion (Chu et al., 2007b) could be of limited therapeutic value during the initial stages of treatment, since type 2 diabetic patients are generally GIP-resistant (Nauck et al., 1993). However, it has recently been reported that β-cell responsiveness to GIP is enhanced with improving blood glucose control (Højberg et al., 2007), so one could envisage GIP secretion gaining more pharmacological importance as chronic treatment with a GPR119 agonist progresses.
Administration of GLP-1 or one of its mimetics has been shown to promote the preservation or expansion of β-cell mass and to delay the development of diabetes in animal models (Brubaker and Drucker, 2004), although not yet in human subjects. This effect may be partly the result of improved glycaemic control. However, elevated intracellular cAMP levels have been shown to protect β-cells from 2-deoxy-D-ribose-induced oxidative damage (Koh et al., 2005) and lipid-induced apoptosis (Kwon et al., 2004). As GPR119 agonists raise cAMP levels in the β-cell, there is potential for these agents to exert a beneficial effect on disease progression beyond what could be achieved by improving glucose homoeostasis alone. The concomitant increase in circulating GLP-1, itself capable of raising β-cell cAMP levels, might contribute to such an effect.
Much progress has been made in the discovery of potent, selective, small-molecule agonists of GPR119 with drug-like properties and oral activity in appropriate animal models (Fyfe et al., 2007a), of which one, APD668, has so far entered into the clinic (Mealy and Lupone, 2006). The value of GPR119 agonists as a new class of therapeutics for type II diabetes and associated obesity is therefore likely to be determined within the next few years.
Acknowledgments
We express our gratitude to our many colleagues at (OSI) Prosidion and OSI Pharmaceuticals Inc. who have contributed to the GPR119 project. Particularly we thank Dr Jim McCormack, VP, Research, and Dr Martin Procter, Senior Director, Chemistry, for their guidance and encouragement.
Glossary
- GIP
gastric inhibitory polypeptide/glucose-dependent insulinotropic peptide
- GLP-1
glucagon-like peptide-1
- GSIS
glucose-stimulated insulin secretion
- LPC
lysophosphatidylcholine (1-alkyl-sn-glycero-3-phosphocholine)
- OEA
oleoylethanolamide
Footnotes
Conflict of interest
The authors state no conflict of interest
(OSI) Prosidion is the diabetes and obesity business unit of OSI Pharmaceuticals Inc. and is operated by Prosidion Ltd, a wholly owned subsidiary of OSI Pharmaceuticals Inc.
References
- Bailey CJ. Drugs on the horizon for diabesity. Curr Diab Rep. 2005;5:353–359. doi: 10.1007/s11892-005-0093-1. [DOI] [PubMed] [Google Scholar]
- Bonini JA, Borowsky BE, Adham N, Boyle N, Thompson TO.2001DNA encoding SNORF25 receptorUS patent 6,221,660-B1.
- Bonini JA, Borowsky BE, Adham N, Boyle N, Thompson TO.2002Methods of identifying compounds that bind to SNORF25 receptorsUS patent 6,468,756-B1.
- Brubaker PL, Drucker DJ. Minireview: glucagon-like peptides regulate cell proliferation and apoptosis in the pancreas, gut and central nervous system. Endocrinology. 2004;145:2653–2659. doi: 10.1210/en.2004-0015. [DOI] [PubMed] [Google Scholar]
- Brubaker PL, Schloos J, Drucker DJ. Regulation of glucagon-like peptide-1 synthesis and secretion in the GLUTag enteroendocrine cell line. Endocrinology. 1998;139:4108–4114. doi: 10.1210/endo.139.10.6228. [DOI] [PubMed] [Google Scholar]
- Chu Z, Carroll C, Gutierrez V, Lucman A, Moloney M, Gao H, et al. 2007bAR231453 mediates improved glycaemic control exclusively via GDIR/GPR119 Keystone Symposium. Diabetes: Molecular Genetics, Signalling Pathways and Integrated PhysiologyKeystone, Colorado, USA, 14–19 January 2007, abstract 117.
- Chu Z, Jones R, Chen R, Carroll C, Gutierrez V, Lucman A, et al. 2007cNovel lipid amide activators of GDIR/GPR119 and their role in glucose homeostasis Keystone Symposium. Diabetes: Molecular Genetics, Signalling Pathways and Integrated PhysiologyKeystone, Colorado, USA, 14–19 January 2007, abstract 230.
- Chu Z-L, Jones RM, He H, Carroll C, Gutierrez V, Lucman A, et al. A role for β-cell-expressed GPR119 in glycemic control by enhancing glucose-dependent insulin release. Endocrinology. 2007a;148:2601–2609. doi: 10.1210/en.2006-1608. [DOI] [PubMed] [Google Scholar]
- Chu Z-L, Leonard JN, Al-Shamma HA, Jones RM.2006Combination therapy for the treatment of diabetes and conditions related thereto and for the treatment of conditions ameliorated by increasing a blood GLP-1 levelInternational Patent Publication WO 2006/076231.
- Davey J. G-protein-coupled receptors: new approaches to maximise the impact of GPCRs in drug discovery. Expert Opin Ther Targets. 2004;8:165–170. doi: 10.1517/14728222.8.2.165. [DOI] [PubMed] [Google Scholar]
- Drucker DJ. Development of glucagon-like peptide-1-based pharmaceuticals as therapeutic agents for the treatment of diabetes. Curr Pharmaceut Des. 2001;7:1399–1412. doi: 10.2174/1381612013397401. [DOI] [PubMed] [Google Scholar]
- Drucker DJ. The biology of incretin hormones. Cell Metab. 2006;3:153–165. doi: 10.1016/j.cmet.2006.01.004. [DOI] [PubMed] [Google Scholar]
- Drucker DJ. The role of gut hormones in glucose homeostasis. J Clin Invest. 2007;117:24–32. doi: 10.1172/JCI30076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drucker DJ, Jin T, Asa SL, Young TA, Brubaker PL. Activation of proglucagon gene transcription by protein kinase-A in a novel mouse enterondocrine cell line. Mol Endocrinol. 1994;8:1646–1655. doi: 10.1210/mend.8.12.7535893. [DOI] [PubMed] [Google Scholar]
- Fredriksson R, Höglund PJ, Gloriam DEI, Lagerstrom MC, Schiöth HB. Seven evolutionarily conserved human rhodopsin G protein-coupled receptors lacking close relatives. FEBS Lett. 2003;554:381–388. doi: 10.1016/s0014-5793(03)01196-7. [DOI] [PubMed] [Google Scholar]
- Fu J, Gaetani S, Oveisi F, Lo Verme J, Serrani A, Rodriguez de Fonseca F, et al. Oleoylethanolamide regulates feeding and body weight through activation of the nuclear receptor PPAR-α. Nature. 2003;425:90–93. doi: 10.1038/nature01921. [DOI] [PubMed] [Google Scholar]
- Fujimoto WY, Metz SA. Phasic effects of glucose, phospholipase A2 and lysophospholipids on insulin secretion. Endocrinology. 1987;120:1750–1757. doi: 10.1210/endo-120-5-1750. [DOI] [PubMed] [Google Scholar]
- Furman B, Pyne N, Flatt P, O'Harte F. Targeting beta-cell cyclic 3′5′ adenosine monophosphate for the development of novel drugs for treating type 2 diabetes mellitus. A review. J Pharm Pharmacol. 2004;56:1477–1492. doi: 10.1211/0022357044805. [DOI] [PubMed] [Google Scholar]
- Fyfe M, Overton H, White J, Jones R, Sorensen RV, Reynet C. Discovery of novel, orally active, synthetic GPR119 agonists as potential agents for treatment of obesity and associated metabolic disorders. Diabetes. 2006;55 Suppl 1:346-OR. [Google Scholar]
- Fyfe M, White J, Widdowson P, Overton H, Reynet C. GPR119 agonists are potential novel oral agents for the treatment of diabesity. Diabetes. 2007b;56 Suppl 1:532-P. [Google Scholar]
- Fyfe MCT, Overton HA, Procter MJ, Reynet C, White JR. New nonpeptide-binding GPCRs as targets for diabetes and the metabolic syndrome. Annu Rep Med Chem. 2007a;42:133–149. [Google Scholar]
- Griffin G.2006Methods for identification of modulators of OSGPR116 activityUS patent 7,083,933-B1.
- Gromada J, Brock B, Schmitz O, Rorsman P. Glucagon-like peptide-1: regulation of insulin secretion and therapeutic potential. Basic Clin Pharmacol Toxicol. 2004;95:252–262. doi: 10.1111/j.1742-7843.2004.t01-1-pto950502.x. [DOI] [PubMed] [Google Scholar]
- Højberg PV, Vilsbøll T, Knop FK, Bache M, Madsbad S, Krarup T, et al. Four weeks of near-normalization of blood glucose restores the insulin response to GIP and improves the insulin response to GLP-1 in patients with type 2 diabetes. Diabetes. 2007;56 Suppl 1:1455-P. [Google Scholar]
- Holst JJ. Glucagon-like peptide-1: from extract to agent. The Claude Bernard Lecture, 2005. Diabetologia. 2006;49:253–260. doi: 10.1007/s00125-005-0107-1. [DOI] [PubMed] [Google Scholar]
- Holst JJ, Deacon CF. Glucagon-like peptide-1 mediates the therapeutic actions of DPP-IV inhibitors. Diabetologia. 2005;48:612–615. doi: 10.1007/s00125-005-1705-7. [DOI] [PubMed] [Google Scholar]
- Jones RM, Semple G, Fioravanti B, Pereira G, Calderon I, Uy J, et al. 20041,2,3-trisubstituted aryl and heteroaryl derivatives as modulators of metabolism and the prophylaxis and treatment of disorders related thereto such as diabetes and hyperglycaemiaInternational Patent Publication WO 2004/065380.
- Koh G, Suh KS, Chon S, Oh S, Woo JT, Kim SW, et al. Elevated cAMP level attenuates 2-deoxy-D-ribose induced oxidative damage in pancreatic beta-cells. Arch Biochem Biophys. 2005;438:70–79. doi: 10.1016/j.abb.2005.03.018. [DOI] [PubMed] [Google Scholar]
- Kwon G, Pappan KL, Marshall CA, Schaffer JE, McDaniel ML. cAMP dose-dependently prevents palmitate-induced apoptosis by both protein kinase A and cAMP-guanine nucleotide exchange factor-dependent pathways in β-cells. J Biol Chem. 2004;279:8938–8945. doi: 10.1074/jbc.M310330200. [DOI] [PubMed] [Google Scholar]
- Lan H, Vassileva G, Corona A, Liu L, Baker H, Golovko A, et al. 2007Mice lacking GPR119 maintain metabolic homeostasis Keystone Symposium. Diabetes: Molecular Genetics, Signalling Pathways and Integrated PhysiologyKeystone, Colorado, USA, 14–19 January 2007, abstract 253.
- Mealy NE, Lupone B. Endocrine disorders. Drugs Future. 2006;31:719–750. [Google Scholar]
- Meier JJ, Gallwitz B, Schmidt WE, Nauck MA. Glucagon-like peptide 1 as a regulator of food intake and body weight: therapeutic perspectives. Eur J Pharmacol. 2002b;440:269–279. doi: 10.1016/s0014-2999(02)01434-6. [DOI] [PubMed] [Google Scholar]
- Meier JJ, Nauck MA, Schmidt WE, Gallwitz B. Gastric inhibitory polypeptide: the neglected incretin revisited. Regul Peptides. 2002a;107:1–13. doi: 10.1016/s0167-0115(02)00039-3. [DOI] [PubMed] [Google Scholar]
- Nauck MA, Heimesaat MM, Orskov C, Holst JJ, Ebert R, Creutzfeld W. Preserved incretin activity of glucagon-like peptide 1 [7–36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type 2 diabetes mellitus. J Clin Invest. 1993;91:301–307. doi: 10.1172/JCI116186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen LL. Incretin mimetics and DPP-IV inhibitors for the treatment of type 2 diabetes. Drug Discov Today. 2005;10:703–710. doi: 10.1016/S1359-6446(05)03460-4. [DOI] [PubMed] [Google Scholar]
- Ohishi T, Takasaki J, Matsumoto M, Saito T, Kamohara M, Soga T, et al. 2003Method of screening remedy for diabetesEur Patent Application EP 1338651-A1.
- Overton HA, Babbs AJ, Doel SM, Fyfe MCT, Gardner LS, Griffin G, et al. Deorphanization of a G protein-coupled receptor for oleoylethanolamide and its use in the discovery of small-molecule hypophagic agents. Cell Metab. 2006;3:167–175. doi: 10.1016/j.cmet.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Proulx K, Cota D, Castaneda TR, Tschop MH, D'Alessio DA, Tso P, et al. Mechanisms of oleoylethanolamide (OEA)-induced changes in feeding behaviour and motor activity. Am J Physiol Regul Integr Comp Physiol. 2005;289:R729–R737. doi: 10.1152/ajpregu.00029.2005. [DOI] [PubMed] [Google Scholar]
- Rodriguez de Fonseca FR, Navarro M, Gomez R, Escuredo L, Nava F, Fu J, et al. An anorexic lipid mediator regulated by feeding. Nature. 2001;414:209–212. doi: 10.1038/35102582. [DOI] [PubMed] [Google Scholar]
- Sakamoto Y, Inoue H, Kawakami S, Miyawaki K, Miyamoto T, Mizuta K, et al. Expression and distribution of GPR119 in the pancreatic islets of mice and rats: predominant localization in pancreatic polypeptide-secreting PP-cells. Biochem Biophys Res Commun. 2006;351:474–480. doi: 10.1016/j.bbrc.2006.10.076. [DOI] [PubMed] [Google Scholar]
- Soga T, Ohishi T, Matsui T, Saito T, Matsumoto M, Takasaki J, et al. Lysophosphatidylcholine enhances glucose-dependent insulin secretion via an orphan G-protein-coupled receptor. Biochem Biophys Res Commun. 2005;326:744–751. doi: 10.1016/j.bbrc.2004.11.120. [DOI] [PubMed] [Google Scholar]
- Stein CJ, Colditz GA. The epidemic of obesity. J Clin Endocrinol Metab. 2004;89:2522–2525. doi: 10.1210/jc.2004-0288. [DOI] [PubMed] [Google Scholar]
- Takeda S, Kadowaki S, Haga T, Takaesu H, Mitaku S. Identification of G protein-coupled receptor genes from the human genome sequence. FEBS Lett. 2002;520:97–101. doi: 10.1016/s0014-5793(02)02775-8. [DOI] [PubMed] [Google Scholar]
- Yang Y, Chen M, Georgeson KE, Harmon CM. Mechanism of oleoylethanolamide on fatty acid uptake in small intestine after food intake and body weight reduction. Am J Physiol Regul Integr Comp Physiol. 2007;292:R235–R241. doi: 10.1152/ajpregu.00270.2006. [DOI] [PubMed] [Google Scholar]
- Zander M, Madsbad S, Madsen JL, Holst JJ. Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and β-cell function in type 2 diabetes: a parallel-group study. Lancet. 2002;359:824–830. doi: 10.1016/S0140-6736(02)07952-7. [DOI] [PubMed] [Google Scholar]