Abstract
The goal of this study was to compare the immune response and the protection capacity induced by the dengue virus 2 (DENV-2) American and Asian genotypes in Macaca fascicularis monkeys. Animals were infected with American or Asian DENV-2 strains and challenged 1 year later with a DENV-2 Asian genotype strain. The viremia and monkey antibody levels were similar for the different strains after primary and secondary infection; however, the functionality of the antibody response was different. A limited viral replication was demonstrated after the secondary infection in all the monkeys. No virus was isolated in tissue culture, while reverse transcription-PCR showed a late positive reaction in four of five challenged monkeys. The immunoglobulin M response pattern and the detection of antibodies to specific proteins by Western blotting supported the protection data. Despite the demonstration of the protective effect after homologous challenge, a strong anamnestic antibody response was observed.
Dengue fever and dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS) are caused by any of four closely related but antigenically distinct dengue virus (DENV) serotypes (DENV-1, DENV-2, DENV-3, and DENV-4). Currently, dengue fever/DHF is the most important mosquito-borne viral disease affecting humans, and an estimated 2.5 billion people live in areas at risk of epidemic transmission (14).
Infection with one of these serotypes does not provide long-lasting cross-protective immunity. In addition, preexisting antibody titers against DENV can enhance the severity of the disease during subsequent exposure to different serotypes (12, 15, 42). Important risk factors for DHF/DSS include the strain and the serotype of the virus involved, as well as the age, the immune status, the sequence of infection, and the genetic predisposition of the individual (5, 11, 28). Antibody-dependent enhancement and viral virulence are two of the major mechanisms proposed to explain DHF/DSS (20, 41). Molecular, clinical, and epidemiological studies suggest that virus genotypes and particularly certain virus mutations are of importance in the final outcome of the disease (9, 31, 37).
Among DENV-2 strains, the Asian and the American genotypes are of interest. The former has been associated with DHF/DSS during secondary heterotypic infections both in Southeast Asia and in the American regions, and the latter, demonstrated in the Americas since 1953, has been associated only with mild disease. American genotype viruses show genetic differences from Asian viruses that correlate with the reduced pathogenicity (31). Most notably, these viruses differ at amino acid envelope 390, a known virulence determinant (31); in their ability to replicate in monocyte-derived macrophages (35, 37); and in the sequence (and hence secondary RNA structure) of the 3′ untranslated region (31), which has been shown to correlate with virulence in DENV (34). It has been also proposed that American genotype viruses are less able to replicate in Aedes aegypti than viruses of Asian origin, so the latter may be more transmissible (2).
The lack of an animal model reproducing the severe DENV disease has hampered the identification of the pathogenic mechanisms implicated in the progression to DHF/DSS. However, the usefulness of the monkey model to study the immune response to DENV has been demonstrated (16-19). In spite of the fact that monkeys do not show disease symptoms, the antibody responses in monkeys are qualitatively similar to those in human patients, and they become viremic after subcutaneous inoculation with live DENV, although in many instances the antibody titers and/or duration of viremia in humans is greater (23). Currently, this model is widely employed in pathogenicity and vaccine investigations (4, 26, 32).
The implications of the molecular differences among genotypes in induced immunity have not been extensively studied. Studies with mice suggested a different humoral immune pattern after primary inoculation with the Asian and the American DENV-2 genotypes (3). However, whether the immunity induced against one genotype is able to protect against subsequent homotypic infections by strains of different genotypes is unknown.
In this study, the virological and humoral immune responses induced by the DENV-2 American and Asian genotypes in primary-inoculated Macaca fascicularis monkeys was compared. In addition, the protection after a secondary homotypic infection with the same and different genotypes of the primary infection was evaluated.
MATERIALS AND METHODS
Cells and viruses.
African green monkey kidney (Vero cells) and baby hamster kidney (BHK-21) cells were grown at 37°C in 199 medium and Eagle's minimal essential medium, respectively, both supplemented with 10% heat-inactivated fetal bovine serum (HFBS). The Aedes albopictus cell line C6/36-HT was grown at 33°C in Eagle's minimal essential medium supplemented with 10% HFBS, 1% nonessential amino acids, and 1% glutamine solution (200 mM).
DENV-2 strain A15 (isolated in Cuba during the 1981 epidemic) (27) and DENV-2 strain Jamaica (1329TVP965), both classified as Asian genotype (13, 37), and DENV-2 strain I348600, isolated in Colombia in 1986 and classified as American genotype (37), were used for the inoculation of monkeys. The passage history of these strains is shown in Table 1. Viral stocks were prepared in C6/36-HT cells, removing the supplemented culture medium of the infected cells when a cytopathic effect was observed and replacing it with fresh medium without HFBS. The supernatant was harvested when the cytopathic effect covered 80% of the monolayer, stored at −80°C, and titrated by viral plaque formation on BHK-21 cells.
TABLE 1.
Viremia in monkey sera after primary and secondary DENV-2 infections as estimated by viral isolation and RT-PCR
| Monkey | Strain used for primary inoculation | Passage historya | Viremia on the indicated day afterb:
|
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary infection
|
Secondary infection
|
|||||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||
| I | DENV-2 A15 | 4 MB, 2 C6/36 | ×, + | ×, + | ×, + | × | × | × | ||||||||||||||
| II | DENV-2 A15 | 4 MB, 2 C6/36 | × | × | ×, + | ×, + | × | × | ||||||||||||||
| III | DENV-2 A15 | 4 MB, 2 C6/36 | × | × | ×, + | ×, + | ×, + | × | ||||||||||||||
| IV | DENV-2 Jamaica | 3 M, 5 C6/36 | ×, + | ×, + | ×, + | × | ||||||||||||||||
| V | DENV-2 I348600 | ? M, 5 C6/36 | ×, + | ×, + | ×, + | × | × | × | ||||||||||||||
MB, mouse brain; M, mosquitoes; C6/36, C6/36-HT cells.
×, positive by RT-PCR; +, positive by viral isolation. Days of inoculation and challenge were considered day zero.
Supernatants from C6/36-HT cells infected with the aforementioned strains and supernatant from noninfected cells as mock antigen were employed as antigens for enzyme-linked immunosorbent assay (ELISA), Western blotting (WB), and plaque reduction neutralization test (PRNT). The PRNT was also performed with strains DENV-1 Jamaica (isolated in 1977), DENV-3 116/00 (isolated during the 2000 Cuban outbreak), and DENV-4 Dominica (isolated in 1981).
The standard DENV strains DENV-1 Hawaii, DENV-2 New Guinea C, DENV-3 H87, and DENV-4 H241, grown in suckling mouse brain and extracted by the sucrose-acetone method, were used for the hemagglutination inhibition (HAI) assay (8). This DENV-2 stock was also employed for immunoglobulin M (IgM) capture ELISA.
Strains DENV-1 Jamaica, DENV-2 Jamaica, DENV-2 I348600, and DENV-4 Dominica were donated by the late Robert Shope.
Monkey inoculation.
Five adult Macaca fascicularis monkeys seronegative for DENV were used in this study. The animals were inoculated twice by the subcutaneous route at an interval of 1 year. Monkeys I, II, and III were primarily inoculated in the left arm with 4 log10 PFU of the DENV-2 A15 strain, monkey IV with the DENV-2 Jamaica strain, and monkey V with the DENV-2 I348600 strain (Table 1). One year later, all monkeys were secondarily inoculated with 4 log10 PFU of the DENV-2 A15 strain. After the first and the second viral inoculations, blood samples were collected daily for 10 days to detect viremia and to evaluate the generation of specific antibodies over time. For serological studies, three additional blood samples were taken at days 15, 30, and 60.
Before each handling, animals were anesthetized intramuscularly with Ketamine hydrochloride. The maintenance and care of experimental animals complied with the Cuban guidelines for the humane use of laboratory animals.
Viremia detection.
Viral isolation was performed by inoculating 100 μl of undiluted serum onto Vero cells grown in 24-well plates, shaking the plates for 1 h at 37°C, and then centrifuging the plates as previously described (22, 38). Fresh supplemented medium was added to the wells, and after 7 days of incubation, cells were tested by an indirect immunofluorescence technique using monoclonal antibodies (MAbs) specific for DENV (21). Samples were subjected to three blind passages in the same cell culture before being considered negative.
The presence of viral RNA was assessed by qualitative RNA reverse transcription-PCR (RT-PCR). RNA was extracted from 250 μl of serum samples using the Trizol procedure according to the manufacturer's instructions (Gibco-BRL). RT and cDNA amplification were performed as previously described (30, 40).
Serological studies.
The anti-DENV antibodies developed after virus inoculations were evaluated by ELISA, PRNT, HAI, and WB.
The anti-DENV IgG antibodies in each individual serum sample were titrated by ELISA against the three DENV-2 strains. Maxisorp 96-well plates were coated with MAb 4G2 (ATCC), which recognizes the flavivirus E protein (22). Three washes with phosphate-buffered saline containing 0.05% Tween 20 (Merck, Germany) were completed after each step of the ELISA. Plates were blocked with 2% bovine serum albumin and then incubated overnight at 4°C with a saturating concentration of DENV antigen and the mock antigen in separate wells. Twofold-diluted serum samples were incubated 1 h at 37°C with either the DENV or the mock antigen. Anti-monkey IgG-peroxidase conjugate (Sigma) diluted 1/10,000 was incubated for 1 h at 37°C. H2O2-ortho-phenylenediamine was added as the substrate solution and left for 30 min. Optical densities (OD) were measured at 492 nm. A dilution of serum was considered positive when the ratio of the OD with DENV antigen to that with mock antigen was 2 or higher.
Anti DENV-2 IgM antibodies were determined by an IgM capture ELISA. Maxisorp 96-well plates were coated with affinity-purified anti-human IgM developed in goat serum (Sigma). Once plates were blocked with 2% bovine serum albumin, 1/10-diluted monkey serum samples were incubated for 2 h at room temperature in four wells of the plate. A saturated concentration of DENV-2 was added and left overnight at 4°C in two of the four wells, and in the other two wells a mock antigen preparation was added as a negative antigen control. Later, 1/2,000-diluted anti-DENV-2 hyperimmune mouse ascitic fluid was incubated for 1 h at 37°C, followed by a similar incubation with 1/4,000-diluted anti-mouse Ig-peroxidase conjugate (Amersham, United Kingdom). As the substrate solution, H2O2-ortho-phenylenediamine was added and left for 30 min. A serum sample was considered positive when the ratio of the OD with DENV antigen to that with mock antigen was 2 or higher.
The PRNT was performed with BHK-21 cells as described by Morens et al. (33) with some modifications (1). The serum dilution that resulted in a 50% reduction of plaque count, as determined by probit analysis, was considered the end point titer. The HAI test was performed as described earlier (8). The sera were treated with acetone and adsorbed with goose erythrocytes. HAI antibody titers were estimated as the highest serum dilution which resulted in the complete inhibition of hemagglutination produced by 8 hemagglutinating units of DENV.
In addition, sera collected 30 days after the first and second virus inoculations were tested by WB to determine the protein specificity of the antibodies elicited. Supernatant from DENV-infected Vero cells was mixed with the sample buffer (without β-mercaptoethanol) for sodium dodecyl sulfate-polyacrylamide gel electrophoresis and heated for 5 min at 80°C as previously described (7). The mixture was loaded onto a 10% polyacrylamide gel; electrophoresis and blotting were assessed as described previously (29, 44). After blocking with 5% skim milk for 1 h at room temperature, the nitrocellulose membrane was cut to strips and incubated overnight at 4°C with 1/50-diluted monkey sera. DENV-2 proteins were identified with MAbs and polyclonal antibodies: MAb 3H5 and 4G2 (anti-E Flaviviridae family; ATCC) to the E protein, MAb 2H2 to the PrM/M protein (10), MAb 8H8 to the core protein (C) (36), murine polyclonal antiserum to the recombinant DENV-2 nonstructural 3 protein (NS3), and DENV-2 hyperimmune mouse ascitic fluid. Finally, the strips were incubated with a 1/1,000 dilution of goat anti-monkey IgG-peroxidase conjugate (Sigma) or goat anti-mouse IgG-peroxidase conjugate (Amersham) as control strips for 1 h at 37°C. Bands were visualized using H2O2-3,3-diaminobenzidine tetrahydrochloride as the substrate.
RESULTS
Development of viremia.
The mean viremia duration after primary infection as estimated by viral isolation was 2.6 days for monkeys inoculated with strain A15 and 3 days for monkeys inoculated with strain Jamaica or I348600 (Table 1). Using RT-PCR, nucleic acid that was assumed to represent viremia was detected. According to RT-PCR, the mean viremia duration in animals inoculated with strain A15 was 5.3 days, while viremia lasted 3 and 5 days in monkeys inoculated with strain Jamaica or I348600, respectively (Table 1). The onset of viremia was first detected at days 2 and 3 by RT-PCR and virus isolation, respectively. The positive RT-PCR at day 1 was not assumed to indicate viremia.
After secondary infection no virus was isolated in any of the studied samples. A positive RT-PCR was observed late for all the animals with the exception of monkey III.
Antibody response.
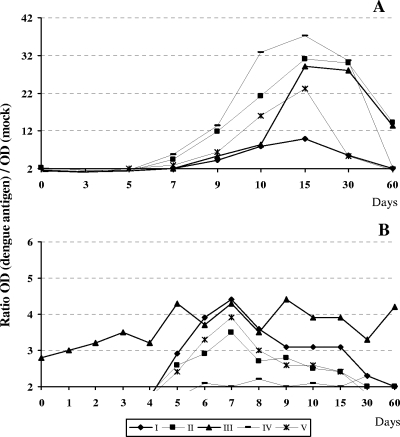
Specific IgM antibodies were detected in monkeys I, II, III, and IV at days 7 to 60 after primary inoculation. However, specific IgM antibodies were negative at day 30 in serum from monkey V. Peak IgM levels were attained at day 15 after primary infection, and the levels were similar among monkeys with the exception of monkey I, which showed a lower value. After secondary infection, anti-DENV IgM antibodies were detected at day 5 or 6, lasting between 15 and 60 days (Fig. 1). In contrast to the case for the primary infection, very low levels of IgM antibodies were detected in all animals after secondary infection. It was noteworthy that monkey III was still positive for IgM antibodies 1 year after the primary infection and in addition remained positive 60 days after the secondary infection.
FIG. 1.
Kinetics of IgM antibodies after primary (A) and secondary (B) infections. After challenge, days were renumbered, starting at 1. Values were considered positive when the ratio of the OD with DENV antigen to that with mock antigen was 2 or higher.
After primary infection, high titers of anti-DENV-2 specific IgG antibodies were observed in all monkeys, with maximum levels at between 15 and 60 days (Fig. 2). After secondary infection, the antibody titers showed a fast increase, reaching plateau levels at between 6 and 15 days.
FIG. 2.
Kinetics of IgG antibodies induced after primary and secondary infections as detected by ELISA. Kinetics of specific antibodies to strain A15 (⧫), strain Jamaica (▴), and strain I348600 (▪) are shown. After challenge, days were renumbered, starting at 0. Arrows indicate the days of primary and secondary infections.
HAI antibodies to DENV-2 showed the highest titers at day 15 after primary infection (Table 2). A wider cross-reactivity to DENV-1, -3, and -4 was observed in sera from monkeys inoculated with strain A15. In contrast, strains Jamaica and I348600 induced cross-reactive antibodies only to DENV-4. Cross-reactive antibodies decreased quickly, while DENV-2-specific antibodies were maintained over time. After secondary infection, both homologous and heterologous antibodies rapidly increased in all the animals; however, while the former remained elevated, the latter decreased by day 60.
TABLE 2.
HAI antibody titers in serum samples collected after primary and secondary DENV-2 infections
| Strain used in HAI test | Monkey | Reciprocal HAI antibody titera on the indicated day after:
|
||||||
|---|---|---|---|---|---|---|---|---|
| Primary infection
|
Secondary infection
|
|||||||
| 10 | 15 | 60 | 0 | 5 | 10 | 60 | ||
| DENV-1 Hawaii | I | <10 | 40 | <10 | <10 | 10 | 80 | 20 |
| II | <10 | 20 | 10 | <10 | 20 | 40 | <10 | |
| III | <10 | 40 | 10 | <10 | 20 | 80 | 10 | |
| IV | <10 | <10 | <10 | <10 | <10 | 20 | 10 | |
| V | <10 | <10 | 10 | <10 | 20 | 80 | 10 | |
| DENV-2 New Guinea C | I | <10 | 20 | 20 | 40 | 160 | 1,280 (32) | 320 |
| II | <10 | 160 | 80 | 40 | 320 | 320 (8) | 80 | |
| III | 20 | 160 | 80 | 80 | 320 | 2,560 (32) | 160 | |
| IV | 80 | 160 | 40 | 40 | 320 | 640 (16) | 320 | |
| V | 40 | 40 | 40 | 40 | 320 | 2,560 (64) | 160 | |
| DENV-3 H87 | I | <10 | <10 | <10 | <10 | 10 | 80 | 40 |
| II | <10 | 10 | <10 | <10 | 20 | 40 | 10 | |
| III | <10 | 20 | <10 | <10 | 20 | 160 | 20 | |
| IV | <10 | <10 | <10 | <10 | 10 | 40 | 20 | |
| V | <10 | <10 | <10 | <10 | 40 | 160 | 20 | |
| DENV-4 H241 | I | 10 | 20 | 10 | <10 | 20 | 160 | 20 |
| II | <10 | 80 | 20 | <10 | 40 | 80 | 20 | |
| III | <10 | 80 | 40 | 10 | 40 | 160 | 40 | |
| IV | <10 | 20 | <10 | <10 | 20 | 80 | 20 | |
| V | <10 | 20 | <10 | <10 | 40 | 320 | 20 | |
Data represent the reciprocal HAI antibody titers estimated as the highest serum dilution that resulted in the complete inhibition of hemagglutination produced by 8 hemagglutinating units. Values in parentheses indicate the fold increase in the homologous titer at day 10 following challenge with respect to the titer detected at the day of challenge (day 0).
Low titers of anti-DENV-2 neutralizing antibodies were detected at day 60 after primary inoculation (Table 3). It was noteworthy that neutralizing antibodies generated in monkeys first inoculated with strain A15 did not recognize strain Jamaica, with the exception of monkey I. After secondary infection, an increase in anti-DENV-2 neutralizing antibodies was observed. Monkeys infected twice with strain A15 showed similar neutralizing-antibody titers to the three strains. However, the neutralizing-antibody titers in sera from animals first infected with strain Jamaica or I348600 were lower against strain A15. After primary and secondary infections, neutralizing antibodies to DENV-1, -3, and -4 were not found.
TABLE 3.
Neutralizing antibodies to DENV-2 strains in sera collected after primary and secondary DENV-2 infections
| Strain used in PRNT | Monkey | Reciprocal neutralizing antibody titera on the indicated day after:
|
||||
|---|---|---|---|---|---|---|
| Primary infection, 60b | Secondary infection
|
|||||
| 0 | 5 | 10 | 60 | |||
| DENV-2 A15 | I | 24 | 54 | 640 | 200 (3.7) | 150 |
| II | 25 | 28 | 350 | 190 (6.7) | 56 | |
| III | 50 | 92 | 500 | 250 (2.7) | 150 | |
| IV | 100 | 25 | 98 | 200 (8) | 230 | |
| V | 17 | 25 | 240 | 720 (28.8) | 130 | |
| DENV-2 Jamaica | I | 35 | 160 | 340 | 180 (0.06) | 300 |
| II | <10 | 11 | 250 | 500 (45.4) | 150 | |
| III | <10 | <10 | 260 | 1,100 (110) | 230 | |
| IV | 17 | 200 | 1,200 | 1,900 (9.5) | 1,500 | |
| V | 45 | 150 | 1,200 | 2,500 (16.6) | 300 | |
| DENV-2 I348600 | I | 35 | 35 | 190 | 210 (6) | 270 |
| II | 11 | 26 | 360 | 400 (15.3) | 96 | |
| III | 33 | 33 | 440 | 600 (18) | 210 | |
| IV | 12 | 36 | 1,100 | 1,100 (30.5) | 140 | |
| V | 16 | 78 | 100 | 660 (8.4) | 38 | |
Data represent the reciprocal neutralizing antibody titers as detected by the PRNT, estimated by probit analysis, which reduced the number of plaques by 50% compared with the viral control. Values in parentheses indicate the fold increase in the titer at day 10 following the challenge with respect to the titer detected at the day of challenge (day 0).
No neutralizing antibody titers were detected prior to day 60.
It was remarkable that HAI and neutralizing-antibody titers to the homologous serotype increased more than four times between the sera collected at days 0 and 10 after virus challenge (Tables 2 and 3).
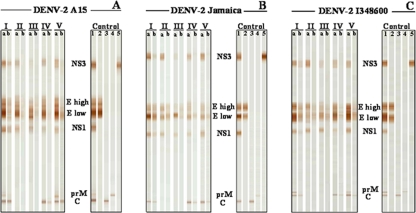
After primary infection, antibodies to both structural and nonstructural DENV proteins were detected by WB (Fig. 3). Sera recognized the envelope (E) protein and the nonstructural proteins NS1 and NS3 of the three DENV-2 strains independent of the strain used in the inoculation, with the exception of monkey III, for which the signal detected to NS3 was very slight after primary infection and absent after secondary infection. The antibody levels to the nonstructural proteins after secondary infection were lower than those after the first inoculation.
FIG. 3.
WB analysis of serum antibody responses against DENV-2 proteins in monkeys after primary and secondary infections. A, B, and C represent antibodies to strains DENV-2 A15, Jamaica, and I348600, respectively. Individual strips were used for testing serum collected 30 days after primary (a) and secondary (b) infections for each monkey (I to V). Control strips: 1, anti DENV-2 hyperimmune mouse ascitic fluid; 2, MAb 3H5/4G2; 3, MAb 8H8; 4, MAb 2H2; 5, polyclonal antibodies to recombinant DENV-2 NS3 protein.
DISCUSSION
It is accepted that a primary infection with one DENV serotype induces long-term protective immunity to reinfection with the homologous serotype (42). However, the huge resurgence of illness caused by DENV in the tropical and subtropical areas of the world has been characterized by the increased movement of DENV, including genotypes, among countries and by a rise in DENV diversity and hyperendemic transmission. In this context, individuals would be secondarily infected by the same serotype, including similar or different genotypes. Few studies have focused on this issue and particularly on the virological and immunological responses associated with homologous secondary infections. Taking into account that monkeys provide the closest model of human DENV infection, Macaca fascicularis monkeys were used to compare the immunogenicities and the homotypic protective capacities associated with three DENV-2 strains clustered in the American and Asian genotypes.
After primary infection, all the animals inoculated either with the American or Asian DENV-2 strains developed viremia with comparable durations. Similar durations of viremia have been previously reported by Halstead et al. (16) in monkeys inoculated with DENV-2 strains.
Recent studies suggested that DENV-2 strains of the American genotype have a lower replication capacity in Aedes aegypti mosquitoes than strains of the Asian genotype (4). Although the onset and duration of viremia were similar for the American and Asian genotypes, we cannot exclude the presence of differences between them because the viral load was not studied. Nevertheless, even if differences in viral load among the strains after primary infection in monkeys were possible, the similar durations of viremia suggest that they were not significant. However, the American genotype strain was able to induce viremia during the primary infection, in contrast to the results reported by Kochel et al. (26). Those authors could not demonstrate viremia by cell culture inoculation in six Aotus nancymae monkeys inoculated with 4 log10 PFU of a DENV-2 American strain (26).
The analysis of the antibody response during the primary infection confirmed the immunogenic properties of the three DENV-2 strains studied. The kinetics of anti-DENV IgM in infected monkeys has not been widely studied. IgM antibodies developed in all infected animals after primary infection, and the antibody levels induced were similar between genotypes. The titers of HAI antibodies, similar to previous observations, were usually higher and detected earlier in response to the homologous virus than to the other three serotypes after primary infection (16). The HAI antibody response induced by each strain after primary infection was different in the cross-reactive capacity to serotypes 1 and 3. Our results were similar to previous reports that showed prominent crossing of antisera to DENV-2 with DENV-4 antigens (18).
The widest cross-serotype reactivity noted for anti-DENV-2 A15 sera (as estimated by HAI assay) and also the rapid decrease over time of these cross-reactive antibodies were remarkable. Whether these observations are related to a higher pathogenic capacity of this strain is not known; however, it is important to mention that this strain was isolated during an epidemic in which more than 10,000 DHF/DSS cases, mostly with a secondary heterotypic infection, were reported (13). The DENV-2 A15 strain shows several amino acid differences in the E protein compared to the DENV-2 I348600 and Jamaica strains (M.G. Guzmán and D. Rosario, unpublished data). It is known that the E glycoprotein represents the dominant virus antigen involved in virus attachment, virus-specific membrane fusion in acid pH endosomes and the induction of the protective immune response, including HAI and neutralizing antibodies (6, 39).
After primary infection, low levels of homologous neutralizing antibodies were detected late in all animals. Previous studies showed earlier and higher neutralizing activity in Aotus nancymae monkeys primarily infected with either DENV-2 American or Asian genotype strains. In addition, low levels of neutralizing antibodies to the Asian strain were reported in sera from monkeys inoculated with the American strain (26). Based on the development of viremia and on the rapid increase of HAI antibodies in all monkeys, it was expected that neutralizing antibodies would also be detected at this time. This atypical behavior in the neutralizing antibody kinetics could not be matched with individual viral load because it was not possible to quantify viremia. Nevertheless, neutralizing antibodies were detected in all animals at day 60 after primary infection with either American or Asian DENV-2 strains, suggesting a similar behavior among the inoculated monkeys. It has been postulated that the development of neutralizing antibodies depends on the virus replication levels and on the time required for antibody maturation (24). Similar results were obtained when mice were inoculated with several DENV-2 genotypes (3). The possibility of a technical mistake is minimal because all samples were tested simultaneously by PRNT; however, it is important to consider the limits of the DENV neutralization assay in detecting low antibody levels.
The absence of neutralizing antibodies against DENV-2 strain Jamaica in sera collected from two monkeys inoculated with DENV-2 strain A15 support previous studies with mice. The preliminary studies could not demonstrate any neutralization activity against an Asian DENV-2 strain (isolated during the 1997 Cuban DHF/DSS epidemic) in sera collected from mice immunized with the A15 strain (3). The explanation for this finding remains unclear, but although both strains belong to the same genotype, the A15 strain is closest to old Asian strains, while the Cuban 1997 and Jamaica strains are closest to new Asian strains. Differences in the amino acid sequences of the E protein may be related to this finding.
Previously, Halstead et al. (16) studied the virological and immunological responses in monkeys challenged with homologous virus. That approach focused on viral challenge up to 6 months after primary infection (16). Our study is the first in which immune animals were challenged with homologous virus of different genotypes and, in addition, the long-term homologous protection at 1 year was evaluated.
After secondary infection, no virus was isolated in tissue culture. Comparable results have been previously obtained after homologous challenge in DENV-1 and DENV-2 immune monkeys and in individuals immunized with attenuated DENV-1 and DENV-2 vaccines (19, 25).
The analysis by WB of the monkey sera collected after primary and secondary infections corroborated the viremia observations. After primary infection all sera strongly reacted with the structural and nonstructural proteins, and after secondary infection the signal to nonstructural proteins decreased, indicating that the virus replication was quite limited. The sera collected from the monkey with a negative RT-PCR (monkey III) showed lower levels of anti-NS3 antibodies. A possible role in the pathogenic mechanisms of the T-cell and humoral responses to NS3 epitopes has been suggested (45, 46). Previous observations also showed an increase in the morbidity and mortality of mice immunized with NS3 protein after virus challenge (R. Ramirez et al., unpublished data).
An anamnestic antibody response was observed during the secondary infection. A different IgM antibody pattern was observed after secondary infection. All the monkeys secondarily infected exhibited an earlier increase, lower levels, and shorter duration of the IgM response than those with primary infection. Similar IgM kinetics after challenge have been correlated with protection in animals immunized with recombinant proteins (3a). In the early phase of the infection, high-affinity IgM could be produced by non-class-switched IgM B cells having memory functions (43), which could also explain the different behavior of monkey IV. In addition, the low viral replication levels demonstrated during the secondary infection could lead to a limited availability of specific antigens to naive B cells and hence to a lower IgM antibody response.
The homologous and heterologous HAI antibodies were increased after secondary infection, but the DENV-2-specific titers were at least twice higher. No differences in terms of IgM, IgG, and HAI antibodies depending on the viral genotype of the primary infection were identified. However, the monkeys inoculated with strains I348600 and Jamaica showed lower neutralizing antibody titers against strain A15. The greater divergence in the genomic sequence of strain A15 could explain its lower recognition.
According to previous reports, the evaluation of the sequential administration of different DENV serotypes in monkeys has shown solid protection after homologous challenge (16). The lack of detectable viremia with a secondary HAI response was classified as partial protection, while the lack of detectable viremia with an absent or transient HAI response was considered evidence of solid protection (16). In contrast to the previous observations, we could not demonstrate sterile immunity in the animals studied after homologous virus challenge 1 year after the primary infection. According to the protection patterns proposed by Halstead et al. (16), the low viral replication (as detected by RT-PCR) and, even more, the strong anamnestic response demonstrated by the significant increase in the antibody titers after challenge suggest a pattern of partial rather than solid protection in our animals.
The implications of these interesting observations are of importance in terms of disease and vaccination and deserve careful studies. Perhaps the differences in the response observed after secondary infection compared to the previous report by Halstead et al. (16) are a function of the long interval before homologous virus challenge (1 year after primary infection) or the animal species employed here. In order to evaluate the half-life of the immunity induced after a DENV-2 infection, experiments providing homologous challenge at 3 and 6 months and testing with other animal species should also be performed.
In summary, the main conclusions of this study are that (i) even when the three strains induced similar viremia and antibody levels after primary and secondary infections, the functionalities of such antibody responses were different, and (ii) there was protection after homologous challenge although a strong anamnestic antibody response occurred.
Acknowledgments
We thank Olaf Horstick (TDR) for his help in the review of the manuscript. We also thank Roberto Fernández and Omar Fuentes (Tropical Medicine Institute Pedro Kourí) for their useful comments regarding biosafety and entomological control and Karelia Cozme (Center for Genetic Engineering and Biotechnology) for her contributions to the animal studies.
This investigation received financial support from the Cuban Program for Dengue Vaccine Development.
Footnotes
Published ahead of print on 19 December 2007.
REFERENCES
- 1.Alvarez, M., R. Rodriguez-Roche, L. Bernardo, L. Morier, and M. G. Guzman. 2005. Improved dengue virus plaque formation on BHK21 and LLCMK2 cells: evaluation of some factors. Dengue Bull. 29:1-9. [Google Scholar]
- 2.Armstrong, P. M., and R. Rico-Hesse. 2001. Differential susceptibility of Aedes aegypti to infection by the American and Southeast Asian genotypes of dengue type 2 virus. Vector Borne Zoonotic Dis. 1:159-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernardo, L., A. Yndart, S. Vazquez, L. Morier, and M. G. Guzman. 2005. Antibody responses to Asian and American genotypes of dengue 2 virus in immunized mice. Clin. Diagn. Lab. Immunol. 12:361-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3a.Bernardo, L., L. Hermida, J. Martin, M. Alvarez, I. Prado, C. López, R. Martínez, R. Rodríguez-Roche, A. Zulueta, L. Lazo, D. Rosario, G. Guillén, and M. G. Gúzman. Anamnestic antibody response after viral challenge in monkeys immunized with dengue 2 recombinant fusion proteins. Arch. Virol., in press. [DOI] [PubMed]
- 4.Blaney, J. E., Jr., C. T. Hanson, K. A. Hanley, B. R. Murphy, and S. S. Whitehead. 2004. Vaccine candidates derived from a novel infectious cDNA clone of an American genotype dengue virus type 2. BMC Infect. Dis. 4:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bravo, J. R., M. G. Guzman, and G. P. Kouri. 1987. Why dengue haemorrhagic fever in Cuba? 1. Individual risk factors for dengue haemorrhagic fever/dengue shock syndrome (DHF/DSS). Trans. R. Soc. Trop. Med. Hyg. 81:816-820. [DOI] [PubMed] [Google Scholar]
- 6.Chen, Y., T. Maguire, and R. M. Marks. 1996. Demonstration of binding of dengue virus envelope protein to target cells. J. Virol. 70:8765-8772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Churdboonchart, V., N. Bhamarapravati, S. Peampramprecha, and S. Sirinavin. 1991. Antibodies against dengue viral proteins in primary and secondary dengue hemorrhagic fever. Am. J. Trop. Med. Hyg. 44:481-493. [DOI] [PubMed] [Google Scholar]
- 8.Clarke, D. H., and J. Casals. 1958. Techniques for hemagglutination and hemagglutination-inhibition with arthropod-borne viruses. Am. J. Trop. Med. Hyg. 7:561-573. [DOI] [PubMed] [Google Scholar]
- 9.Cologna, R., and R. Rico-Hesse. 2003. American genotype structures decrease dengue virus output from human monocytes and dendritic cells. J. Virol. 77:3929-3938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falconar, A. K. 1999. Identification of an epitope on the dengue virus membrane (M) protein defined by cross-protective monoclonal antibodies: design of an improved epitope sequence based on common determinants present in both envelope (E and M) proteins. Arch. Virol. 144:2313-2330. [DOI] [PubMed] [Google Scholar]
- 11.Gubler, D. J. 1998. Dengue and dengue hemorrhagic fever. Clin. Microbiol. Rev. 11:480-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guzman, M. G., M. Alvarez, R. Rodriguez, D. Rosario, S. Vazquez, L. Valdes, M. V. Cabrera, and G. Kouri. 1999. Fatal dengue hemorrhagic fever in Cuba, 1997. Int. J. Infect. Dis. 3:130-135. [DOI] [PubMed] [Google Scholar]
- 13.Guzman, M. G., V. Deubel, J. L. Pelegrino, D. Rosario, M. Marrero, C. Sariol, and G. Kouri. 1995. Partial nucleotide and amino acid sequences of the envelope and the envelope/nonstructural protein-1 gene junction of four dengue-2 virus strains isolated during the 1981 Cuban epidemic. Am. J. Trop. Med. Hyg. 52:241-246. [DOI] [PubMed] [Google Scholar]
- 14.Guzman, M. G., and G. Kouri. 2002. Dengue: an update. Lancet Infect. Dis. 2:33-42. [DOI] [PubMed] [Google Scholar]
- 15.Halstead, S. B. 1970. Observations related to pathogensis of dengue hemorrhagic fever. VI. Hypotheses and discussion. Yale J. Biol. Med. 42:350-362. [PMC free article] [PubMed] [Google Scholar]
- 16.Halstead, S. B., J. Casals, H. Shotwell, and N. Palumbo. 1973. Studies on the immunization of monkeys against dengue. I. Protection derived from single and sequential virus infections. Am. J. Trop. Med. Hyg. 22:365-374. [DOI] [PubMed] [Google Scholar]
- 17.Halstead, S. B., and N. E. Palumbo. 1973. Studies on the immunization of monkeys against dengue. II. Protection following inoculation of combinations of viruses. Am. J. Trop. Med. Hyg. 22:375-381. [DOI] [PubMed] [Google Scholar]
- 18.Halstead, S. B., H. Shotwell, and J. Casals. 1973. Studies on the pathogenesis of dengue infection in monkeys. I. Clinical laboratory responses to primary infection. J. Infect. Dis. 128:7-14. [DOI] [PubMed] [Google Scholar]
- 19.Halstead, S. B., H. Shotwell, and J. Casals. 1973. Studies on the pathogenesis of dengue infection in monkeys. II. Clinical laboratory responses to heterologous infection. J. Infect. Dis. 128:15-22. [DOI] [PubMed] [Google Scholar]
- 20.Halstead, S. B., and P. Simasthien. 1970. Observations related to the pathogenesis of dengue hemorrhagic fever. II. Antigenic and biologic properties of dengue viruses and their association with disease response in the host. Yale J. Biol. Med. 42:276-292. [PMC free article] [PubMed] [Google Scholar]
- 21.Henchal, E. A., M. K. Gentry, J. M. McCown, and W. E. Brandt. 1982. Dengue virus-specific and flavivirus group determinants identified with monoclonal antibodies by indirect immunofluorescence. Am. J. Trop. Med. Hyg. 31:830-836. [DOI] [PubMed] [Google Scholar]
- 22.Hermida, L., L. Bernardo, J. Martin, M. Alvarez, I. Prado, C. Lopez, L. Sierra Bde, R. Martinez, R. Rodriguez, A. Zulueta, A. B. Perez, L. Lazo, D. Rosario, G. Guillen, and M. G. Guzman. 2006. A recombinant fusion protein containing the domain III of the dengue-2 envelope protein is immunogenic and protective in nonhuman primates. Vaccine 24:3165-3171. [DOI] [PubMed] [Google Scholar]
- 23.Innis, B. 1997. Antibody responses to dengue virus infection, p. 221-243. In D. Gubler and G. Kuno (ed.), Dengue and dengue haemorrhagic fever. CAB International, New York, NY.
- 24.Janeway, C., and P. Travers. 1994. Host defense against infection, 1st ed. Blackwell Scientific Publications, London, United Kingdom.
- 25.Kanesa-thasan, N., W. Sun, G. Kim-Ahn, S. Van Albert, J. R. Putnak, A. King, B. Raengsakulsrach, H. Christ-Schmidt, K. Gilson, J. M. Zahradnik, D. W. Vaughn, B. L. Innis, J. F. Saluzzo, and C. H. Hoke, Jr. 2001. Safety and immunogenicity of attenuated dengue virus vaccines (Aventis Pasteur) in human volunteers. Vaccine 19:3179-3188. [DOI] [PubMed] [Google Scholar]
- 26.Kochel, T. J., D. M. Watts, A. S. Gozalo, D. F. Ewing, K. R. Porter, and K. L. Russell. 2005. Cross-serotype neutralization of dengue virus in Aotus nancymae monkeys. J. Infect. Dis. 191:1000-1004. [DOI] [PubMed] [Google Scholar]
- 27.Kouri, G., P. Mas, M. G. Guzman, M. Soler, A. Goyenechea, and L. Morier. 1983. Dengue hemorrhagic fever in Cuba, 1981: rapid diagnosis of the etiologic agent. Bull. Pan Am. Health Organ. 17:126-132. [PubMed] [Google Scholar]
- 28.Kouri, G. P., M. G. Guzman, and J. R. Bravo. 1987. Why dengue haemorrhagic fever in Cuba? 2. An integral analysis. Trans. R. Soc. Trop. Med. Hyg. 81:821-823. [DOI] [PubMed] [Google Scholar]
- 29.Laemmli, U. K. 1970. Cleavage of structural protein during assembly of the head of bacteriphage T4. Nature 227:680-685. [DOI] [PubMed] [Google Scholar]
- 30.Lanciotti, R. S., C. H. Calisher, D. J. Gubler, G. J. Chang, and A. V. Vorndam. 1992. Rapid detection and typing of dengue viruses from clinical samples by using reverse transcriptase-polymerase chain reaction. J. Clin. Microbiol. 30:545-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leitmeyer, K. C., D. W. Vaughn, D. M. Watts, R. Salas, I. Villalobos de Chacon, C. Ramos, and R. Rico Hesse. 1999. Dengue virus structural differences that correlate with pathogenesis. J. Virol. 73:4738-4747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Monath, T. P., G. A. Myers, R. A. Beck, M. Knauber, K. Scappaticci, T. Pullano, W. Tad Archambault, J. Catalan, C. Miller, Z. X. Zhang, S. Shin, K. Pugachev, K. Draper, I. S. Levenbook, and F. Guirakhoo. 2005. Safety testing for neurovirulence of novel live, attenuated flavivirus vaccines: infant mice provide an accurate surrogate for the test in monkeys. Biologicals 33:131-144. [DOI] [PubMed] [Google Scholar]
- 33.Morens, D. M., S. B. Halstead, P. M. Repik, R. Putvatana, and N. Raybourne. 1985. Simplified plaque reduction neutralization assay for dengue viruses by semimicro methods in BHK-21 cells: comparison of the BHK suspension test with standard plaque reduction neutralization. J. Clin. Microbiol. 22:250-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Proutski, V., E. A. Gould, and E. C. Holmes. 1997. Secondary structure of the 3′ untranslated region of flaviviruses: similarities and differences. Nucleic Acids Res. 25:1194-1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pryor, M. J., J. M. Carr, H. Hocking, A. D. Davidson, P. Li, and P. J. Wright. 2001. Replication of dengue virus type 2 in human monocyte-derived macrophages: comparisons of isolates and recombinant viruses with substitutions at amino acid 390 in the envelope glycoprotein. Am. J. Trop. Med. Hyg. 65:427-434. [DOI] [PubMed] [Google Scholar]
- 36.Pupo Antunez, M., H. Rodriguez, S. Vazquez, J. C. Vilaseca, M. Alvarez, A. Otero, and G. Guzman. 1997. Monoclonal antibodies raised to the dengue-2 virus (Cuban: A15 strain) which recognize viral structural proteins. Hybridoma 16:347-353. [DOI] [PubMed] [Google Scholar]
- 37.Rico Hesse, R., L. M. Harrison, R. A. Salas, D. Tovar, A. Nisalak, C. Ramos, J. Boshell, M. T. de Mesa, R. M. Nogueira, and A. T. da Rosa. 1997. Origins of dengue type 2 viruses associated with increased pathogenicity in the Americas. Virology 230:244-251. [DOI] [PubMed] [Google Scholar]
- 38.Rodriguez-Roche, R., M. Alvarez, M. G. Guzman, L. Morier, and G. Kouri. 2000. Comparison of rapid centrifugation assay with conventional tissue culture method for isolation of dengue 2 virus in C6/36-HT cells. J. Clin. Microbiol. 38:3508-3510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roehrig, J. T., R. A. Bolin, and R. G. Kelly. 1998. Monoclonal antibody mapping of the envelope glycoprotein of the dengue 2 virus, Jamaica. Virology 246:317-328. [DOI] [PubMed] [Google Scholar]
- 40.Rosario, D., M. Alvarez, J. Diaz, R. Contreras, R. Rodriguez, S. Vazquez, and M. G. Guzman. 1998. Polymerase chain reaction for rapid detection and serotyping of dengue virus in clinical samples. Rev. Panam. Salud Publica 4:1-5. [DOI] [PubMed] [Google Scholar]
- 41.Rosen, L. 1986. The pathogenesis of dengue haemorrhagic fever. A critical appraisal of current hypotheses. S. Afr. Med. J. Suppl. 1986:40-42. [PubMed] [Google Scholar]
- 42.Sabin, A. B. 1952. Research on dengue during World War II. Am. J. Trop. Med. Hyg. 1:30-50. [DOI] [PubMed] [Google Scholar]
- 43.Shi, Y., K. Agematsu, H. D. Ochs, and K. Sugane. 2003. Funtional analysis of human memory B-cell subpopulations: IgD+CD27+ B cells are crucial in secondary immune response by producing high affinity IgM. Clin. Immunol. 108:128-137. [DOI] [PubMed] [Google Scholar]
- 44.Towbin, H., Staehelin, T., and J. Golden. 1979. Electrophoretic transfer of protein from polyacrylamide gel to nitrocellulose sheets: procedure and some applications. Proc. Natl. Acad. Sci. USA 76:4350-4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zivna, I., S. Green, D. W. Vaughn, S. Kalayanarooj, H. A. Stephens, D. Chandanayingyong, A. Nisalak, F. A. Ennis, and A. L. Rothman. 2002. T cell responses to an HLA-B*07-restricted epitope on the dengue NS3 protein correlate with disease severity. J. Immunol. 168:5959-5965. [DOI] [PubMed] [Google Scholar]
- 46.Zivny, J., M. DeFronzo, W. Jarry, J. Jameson, J. Cruz, F. A. Ennis, and A. L. Rothman. 1999. Partial agonist effect influences the CTL response to a heterologous dengue virus serotype. J. Immunol. 163:2754-2760. [PubMed] [Google Scholar]