Abstract
The purpose of this study was to determine if disparities exist in lifetime utilization of mental health/substance abuse services among Asian, Native Hawaiian/Other Pacific Islander (NHOPI) and white mothers. The study sample was comprised of mothers assessed to be at-risk (n=491) and not at-risk (n=218) for child maltreatment in the Hawaii Healthy Start Program study. Multiple logistic regression models were used to test the effects of predisposing, need, and enabling factors on utilization of services. Results revealed that, among mothers with depressive symptoms, compared with whites, Asians and NHOPI were significantly less likely to have received services. There were no significant racial differences in use of mental health/substance use services by other factors. These results suggest that racial disparities exist in utilization of mental health/substance abuse services among mothers with depressive symptoms. Future research is needed to identify barriers and facilitators to accessing needed services for Asian and NHOPI women.
Introduction
Mental health and substance use disorders are major public health issues that cause a tremendous amount of burden on affected individuals and society as a whole. For instance, major depressive disorder is the leading cause of disability in the USA,1 and affects nearly twice as many women as men.1–3 Although studies examining mental health among racial minorities are limited,1,4,5 collectively they show that racial minorities experience a greater disability burden from mental disorders compared to whites because of receipt of less and poorer quality of care.6–8
The annual costs of treatment of substance abuse and depression are approximately $67 billion and $44 billion, respectively.9,10 There are existing treatments that have proven to be effective for major depressive disorder and substance use disorders 1,8,9,11; however, many individuals who need treatment for these disorders do not receive it.11 Studies of substance abusing populations have also shown that racial minorities are less likely to seek treatment12 and they receive fewer services.13–15 Similarly, evidence shows that racial minorities have lower rates of health care utilization for mental disorders compared to whites because of factors such as stigma and financial costs.8,11,16,17
Most prior research has not focused on Asians and Native Hawaiian/Other Pacific Islanders (NHOPI) or has combined Asians and NHOPI in reporting findings. Asians and NHOPI are often perceived as “model minorities,” which stereotypes them as successful racial minorities compared with other racial minorities. This model minority myth perpetuates the notion that Asians and NHOPI are problem-free including not being affected with health problems, such as mental and substance use disorders or needing services to address these disorders.8
It is not too surprising, then, that there is limited knowledge about mental health and substance abuse service use among Asian and NHOPI women.18 Previous research has revealed that, overall, the Asian and NHOPI populations have a lower prevalence of substance use compared to rates of the total US population,19,20 but that rates differ among Asian and NHOPI ethnic subgroups. For example, Pacific Islanders have very high substance use rates, whereas Chinese and Southeast Asians have the lowest compared with other ethnic minorities19; hence, available data should be interpreted carefully. There is also little published research on gender-specific (e.g., NHOPI women’s utilization rates) and psychosocial correlates (e.g., social support; intimate partner violence) of depression and substance abuse among NHOPI women. Considering the cultural heterogeneity with Asian and NHOPI populations21 and that women are traditionally responsible for their children’s health22, it is vital to improve the field’s knowledge of mental health and substance abuse treatment service use among Asian and NHOPI women.
The availability of data from an experimental study of a home-based support program for families at-risk for child maltreatment provided an opportunity to assess utilization of mental health/substance abuse services by Asian and NHOPI women. The goal of the present study was to compare the prevalence of lifetime receipt of mental health/substance abuse services among women by race and to identify factors that moderated racial disparities in such service use.
Methods
This cross-sectional study used existing data from a multisite trial of the Hawaii “Healthy Start Program” (HSP) to relate maternal attributes, including race, to report lifetime use of mental health/substance abuse services. The following section describes the parent study and the conceptual model, dependent variable, independent variables, and data analysis methods for the current study.
Parent study
Data were drawn from a multisite randomized trial of HSP. The HSP’s overall aim is to “improve family functioning and, in so doing, promote child health and development and prevent child abuse”.23 (p. The HSP has two components: (1) population-based screening and assessment of families to identify those at-risk for child maltreatment; and (2) home visiting for families who are identified at-risk.24 A more detailed description of the home visiting component can be found elsewhere.24
The randomized trial, which began in 1994–1995, focused on six HSP communities on the island of Oahu. Each of the sites is a geographically defined community. The program sites were Waipahu, Diamond Head, Ewa, Waianae, Kalihi-Palama, and Kaneohe. Over time, the State increased coverage to 100% of communities. At the time the study was done, it targeted communities with greater vulnerability. Oahu is home to 80% of Hawaii’s population. Communities on the island of Oahu rather than the neighbor islands were selected to allow close monitoring of fieldwork while containing costs. The communities were different in terms of demographic characteristics. For instance, according to statistics from the 1990 United States Census, the proportions of adults lacking a high school education ranged from 17–45% among the six HSP communities, and the proportions of Native Hawaiians ranged from 7–41%.25 The at-risk families within the six HSP communities, however, were similar in most respects, including parental age, race, poverty status, education, substance use, and domestic violence.25
The screening and assessment of family risk for child maltreatment were conducted daily on all of Oahu’s civilian hospitals with obstetric units for all women residing in communities served by HSP programs. Per the usual protocol, the HSP staff screened all new mothers’ medical records at the obstetrical unit for family risk for child abuse.26 The families provided informed consent for the review of medical records at hospital registration.25 The 15 areas that were used to measure family risk included:
parents not married; unemployed partner; inadequate income; unstable housing; lack of telephone; less than high school education; inadequate emergency contacts; marital or family problems; history of abortions; abortion unsuccessfully sought or attempted; adoption sought; history of substance abuse; history of psychiatric care; history of depression; and inadequate prenatal care.26 (p.67)
If the record suggested risk or if it did not contain enough information for screening, the family was interviewed to assess each parent’s risk using Kempe’s Family Stress Checklist.27 The Family Stress Checklist assesses risk for child abuse based on ten risk factors. A family was considered to be at-risk by having one or more of the following ten risk factors on the Family Stress Checklist: (1) history of abuse as a child; (2) substance abuse, mental illness, or criminal history; (3) previous or current child protective services involvement; (4) low self-esteem, poor coping ability; (5) multiple life stressors; (6) potential for violent temper outbursts; (7) unrealistic expectations for child’s development; (8) harsh punishment of a child; (9) perceives child as being difficult or provocative; and (10) child unwanted or risk for poor bonding.25 The possible score from this Family Stress Checklist range from 0–100. Each parent was scored as 0 (no risk), 5 (mild risk) or 10 (severe risk) for each of the 10 risk factors assessed. Families were eligible for HSP home visiting if either parent had a total Family Stress Checklist score of 25 or greater and if the family was not already known to the child protective services.26 The families were eligible for the study if the mother spoke English well enough to complete study interviews (over 97% of families eligible for HSP) and if the family was willing to be enrolled in home visiting if randomly assigned to the HSP group.
The sample of at-risk families was selected at the time of the HSP assessment. The families who were identified as at-risk for abuse were offered program services, and program participation was voluntary. After an eligible family was identified, a staff member described both the HSP and the study and obtained a signed, informed consent from the mother to participate.25 Of the 897 eligible at-risk families, 81% were willing to enroll in home visiting and in the study, less than 1% were willing to enroll in home visiting but did not want to be in the study, and the remainder declined home visiting. The percent of families willing to enroll in the HSP was comparable to rates before the study. Compared to those refusing home visiting, enrollees were slightly younger and were more likely to be at very high risk for child maltreatment, to have given birth prematurely, and to have completed their assessment of risk in the hospital rather than by the telephone (23% of the participants and 44% of the nonparticipants were assessed by the telephone).26
Research staff conducted a baseline maternal interview within a month after the baby’s birth (in 1994–1995), with the first wave of data collection ending in 1998–1999. Of those providing consent, 94% of the eligible at-risk families completed the baseline interview: intervention (n=373) and controls (n=311). Trained research staff independent of the HSP collected data from at-risk families at their homes at baseline, when the child was 1, 2, and 3 years old, and when the child was in first grade.
When children in the at-risk sample were in first grade, an addition comparison group of not-at-risk families was assembled (n=440 families). This random sample was drawn from the cohort of families of newborns who had screened negative for risk of child maltreatment in the study communities at the time that the at-risk families were screened and assessed. The not-at-risk sample was stratified by birth weight, gender, and parity within each HSP community. There were 19 families who were deemed ineligible to participate because of language barriers or child’s death, 82 families who could not be located, 116 families who refused, and 223 families who were enrolled and followed when the children were in grade 1.
Mothers in the study received monetary remuneration for the completion of interviews. They received $25 for the baseline interview and $30 for the grade 1 follow-up interview.
Funding for this study were provided by the Robert Wood Johnson Foundation (18303), the Annie E. Casey Foundation (94-4041), the David and Lucile Packard Foundation (93-6051, 94-7957, 97-8058, and 98-3448), the Hawaii State Department of Health (99-29-J), the US Maternal and Child Health Bureau (R40 MC 00029, formerly MCJ-240637 and R40MC00123, formerly MCJ-240838), the National Institute of Mental Health, Epidemiological Center for Early Risk Behaviors (P30MH38725), and the National Institute of Mental Health (R01 MH60733). The study was approved by the Hawaii Department of Health Research Review Committee and by the institutional review boards of The Johns Hopkins University School of Medicine and the six hospitals where families were assessed and enrolled into the study.
Response rates of parent study
Overall, follow-up interviews when the children were in grade 1 were obtained for 770 families; of these, 709 were interviews with the child’s biological mother. The overall response rates were 80% (547/684) for the at-risk sample and 53% (223/421) for the not-at-risk sample. Within the at-risk sample, response rates were 78% (243/311) for the control group and 82% (304/373) for the intervention group.
The racial distributions for the at-risk Grade 1 sample were 14% white, 26% Asian, 32% NHOPI, and 28% with no primary affiliation or other. The racial distributions for the not-at-risk Grade 1 sample were 13% white, 42% Asian, 15% NHOPI, and 30% with no primary affiliation or other.
Within the sample of at-risk mothers, those with vs. without an interview did not differ by race or age. Within the sample of not-at-risk mothers, those with vs. without an interview did not differ by age but did differ by race (p=0.01). The following proportions of not-at-risk mothers had completed the interview: 64% whites, 44% Asians, 63% NHOPI, and 55% with no primary racial affiliation/other.
Conceptual model
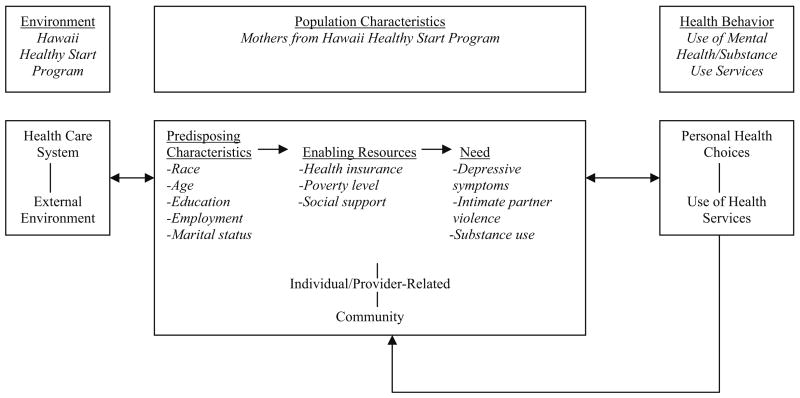
The Andersen and Aday Behavioral Model and Access to Care (Fig. 1) was used to guide variable selection for measuring racial disparities.28 It is important first to identify whether racial disparities in service use are present after controlling for service need, defined here as depressive symptoms, substance use, and/or intimate partner violence. Then, one tests for interactions of predisposing and enabling variables with race. Previous studies have used this model to examine mental health services use by Asians and NHOPI,29 rates/predictors of inpatient psychiatric care,30 and depression and substance use as predictors of utilization.31,32
Figure 1.
An adaptation of the Andersen & Aday Behavioral Model and Access to Care. Adapted from Anderson28
Dependent variable
The study’s dependent variable, lifetime use of residential/outpatient mental health/substance abuse services (yes/no), is a health behavior.33 Each mother was asked, “Have you ever stayed overnight in a hospital/treatment center for substance use/emotional problems?” If no, she was asked, “Did you ever want/need to stay overnight in a treatment center for substance use/emotional problems?” Each mother was also asked, “Have you ever in your life received outpatient help/treatment for substance use/emotional problems?” If no, she was asked, “Did you ever want/need outpatient help/treatment for substance use/emotional problems?” These questions combined both mental health and substance abuse services; hence, this study was unable to separate these two types of services as distinct outcomes.
Independent variables
The baseline independent variables included the environment (study group) and predisposing characteristics (race, age, education, marital status, and employment). The race categories included Asian, NHOPI, white, and no primary racial affiliation/other. In terms of age, there was no difference in the prevalence of utilization of mental health/substance abuse services among mothers who were 19 years old or younger, 20–25, and 26–34 (20%, 20% and 21%, respectively); however, 30% of mothers who were 35 years and older reported utilizing such services. The following analyses, therefore, treated age as a binary variable (34 years old or younger and 35 years old or older).
The education categories included less than a high school education, a high school education, and some college, a college education or graduate education. Maternal employment in the past 12 months was treated as a binary variable (yes and no). Marital status was also treated as a binary variable (married or living together and single, separated, divorced, or widowed).
The enabling resources included health insurance, household poverty level, and social support. The current health insurance categories included private health insurance, public health insurance, and no health insurance. The household poverty level, which was determined using the federal poverty level guidelines, was treated as a binary variable (above household poverty level and below household poverty level).
Social support was assessed using the Maternal Social Support Index.34,35 The Maternal Social Support Index consisted of 18 items that were distributed among the following seven domains: (1) help with daily tasks, (2) satisfaction with visits from kin, (3) help with crises, (4) emergency child care, (5) satisfaction with communication from male partner, (6) satisfaction with communication from another support person, and (7) community involvement. The Maternal Social Support Index has been successfully used with Asian and NHOPI women.36
The need factors included depressive symptoms, problem alcohol use, illicit drug use, and intimate partner violence. Depressive symptoms were assessed using the Center for Epidemiologic Studies—Depression (CES-D) scale. The CES-D scale is a 20-item, self-reported instrument that assesses the level of depressive symptomatology in the past week.37 Each item receives a score of 0, 1, 2, or 3 based on the frequency of occurrence with a higher score indicating more occurrence of the particular symptom, thus, the total CES-D score can range from 0–60. Previous research has employed a cutoff score of 16 or greater to designate an individual as depressed.38,39 Thus, the following analyses defined a score of 16 or greater as positive for depression. The CES-D scale has been used and validated with Asian40,41 and Native Hawaiian adults.42–47 The internal consistencies (Cronbach alpha) for the CES-D scale was 0.87, which was comparable to the original scale’s reliability.37
Problem alcohol use was assessed using the CAGE. CAGE is a short test developed to screen for alcoholism or covert drinking problems. An interviewer administered the CAGE, which asks: (1) Have you ever felt you should Cut down on your drinking?; (2) Have people Annoyed you by criticizing your drinking?; (3) Have you ever felt bad or Guilty about your drinking?; and (4) Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (Eye opener)?48 CAGE items are scored a 0 or 1 and a total score of 2+ is seen as an indication of an alcohol problem or alcoholism. Problem alcohol use was defined as ever CAGE positive and have drank in the past year (yes or no). The study did not collect information about the respondent’s lifetime experience with problem alcohol use.
Illicit drug use was categorized as (1) no, never used illicit drugs, (2) yes, used illicit drugs in the past but not currently, and, (3) yes, used illicit drugs in the past and in the past 12 months. Interviewers asked the respondents, “Which of these have you ever used without a doctor’s prescription, ever in your life, even once?” Some examples of illicit drugs included marijuana, methamphetamines, cocaine, and heroin.
Intimate partner violence was assessed with the Conflict Tactics Scale-2, a revised version of the Conflict Tactics Scale.49 The respondents were asked, “How often did this happen in the past 12 months?” The following three Conflict Tactics Scale-2 subscales were included in the survey: (1) psychological aggression; (2) physical assault; and (3) sexual coercion. All eight psychological aggression items, all 12 physical assault items, and three of the seven sexual coercion items were included in the survey. The Conflict Tactics Scale50,51 and the Conflict Tactics Scale-252,53 have been used and validated with Asians and NHOPI. The following analyses include mothers’ lifetime experience with intimate partner violence. The internal consistencies (Cronbach alpha) for the psychological aggression, physical assault, and sexual coercion Conflict Tactics Scale-2 subscales in this sample were 0.82, 0.90, and 0.57, respectively; the psychological aggression and physical assault scales were comparable to the original scales’ reliabilities.49
Data analysis
Stata version 9.054, was used to analyze the data. The analysis was limited to biological mothers because data on race were not available for other primary caregivers. Descriptive statistics were calculated to estimate population parameters. Bivariate analysis (for each explanatory variable), likelihood ratio test for each factor, exploratory data analysis for potential effect modification, and multiple logistic regressions were performed. In terms of effect modification, potential interactions between race and need factors (depressive symptoms, substance use, and intimate partner violence) were explored first. Then, potential interactions between race and predisposing and enabling variables were explored. An interaction effect was included in the final multivariate model if it was found to be statistically significant (p<0.05). The multivariate model included race, risk status for child maltreatment, variables that were found to be significant in the bivariate analyses (p<0.05), variables that were supported by previous research to be significantly associated with mental health/substance abuse services, and significant interactions between race and other variable(s) (p<0.05).
Results
Sample description
There were 709 mothers in this study including 491 that were identified to be at-risk and 218 assessed to be not-at-risk for child maltreatment (see Table 1). The study sample comprised of 13.7% whites, 30.8% Asians, and 26.9% NHOPI. The remaining mothers reported no primary racial affiliation or other. The study sample’s age range was 14–43 years old.
Table 1.
Maternal characteristics when children were in grade 1 (n=709)
| Characteristic | Total # (%) |
|---|---|
| Risk for child maltreatment | |
| At-risk | 491 (69.3) |
| Not at-risk | 218 (30.7) |
| At-risk: Study group assignment | |
| Controls | 218 (30.8) |
| Intervention | 273 (38.5) |
| Race | |
| White | 97 (13.7) |
| Asian | 218 (30.8) |
| Native Hawaiian/Other Pacific Islander | 191 (26.9) |
| No primary racial affiliation/other | 203 (28.6) |
| Age (at baseline) | |
| ≤19 | 148 (20.9) |
| 20–25 | 229 (32.4) |
| 26–34 | 260 (36.7) |
| 35+ | 71 (10.0) |
| Marital status | |
| Married/living together | 404 (57.0) |
| Single/separated/divorced/widowed | 305 (43.0) |
| Current health insurance | |
| None | 62 (8.8) |
| Public | 223 (31.7) |
| Private | 419 (59.5) |
| Education | |
| Less than high school | 93 (13.1) |
| High school | 221 (31.2) |
| Some college or more | 394 (55.7) |
| Employment (in past 12 months) | |
| No | 139 (19.6) |
| Yes, 1+ job | 570 (80.4) |
| Household poverty level | |
| Under | 237 (34.0) |
| Above | 460 (66.0) |
| Social support: help with daily tasks | |
| 0 | 37 (5.7) |
| 1–2 | 60 (9.3) |
| 3–5 | 167 (25.8) |
| 6+ | 384 (59.3) |
| Social support: help with crises | |
| 0 | 17 (2.4) |
| 1–2 | 155 (21.9) |
| 3–5 | 315 (44.4) |
| 6+ | 222 (31.3) |
| Social support: emergency child care | |
| 0–1 | 91 (12.8) |
| 2+ | 618 (87.2) |
| Social support: regular talks with another person | |
| No | 71 (10.0) |
| Yes | 638 (90.0) |
| Social support: satisfaction with visits from kin | |
| No relatives | 121 (17.1) |
| 1+ relatives and more/less often | 166 (23.4) |
| 1+ relatives and it is about right | 422 (59.5) |
| Social support: satisfaction with communication from a male partner | |
| Dissatisfied/very dissatisfied | 51 (7.2) |
| Satisfied | 320 (45.1) |
| Very satisfied | 222 (31.3) |
| No current partner or in past 12 months | 116 (16.4) |
| Social support: attend religious services a month | |
| No religious group | 358 (50.5) |
| Attend once per month | 61 (8.6) |
| Attend more than once per month | 290 (40.9) |
| Social support: how active in voluntary groups | |
| No membership in group | 526 (74.2) |
| Not active or fairly active | 71 (10.0) |
| Very active | 112 (15.8) |
| Depressive symptoms | |
| No (CES-D<16) | 505 (71.6) |
| Yes (CES-D≥16) | 200 (28.4) |
| Any illicit drug use | |
| No | 315 (44.5) |
| Yes in past, but not currently/in past 12 months | 347 (49.1) |
| Yes in past and currently/in past 12 months | 45 (6.4) |
| Problem alcohol use (in past 12 months) | |
| No | 645 (91.0) |
| Yes | 64 (9.0) |
| Intimate partner violence (IPV) | |
| No IPV ever | 111 (15.8) |
| Some IPV ever | 525 (74.9) |
| No partner in past 12 months | 65 (9.3) |
| IPV: any psychological aggression | |
| No | 117 (16.8) |
| Yes | 516 (73.9) |
| No partner in past 12 months | 65 (9.3) |
| IPV: any physical assault | |
| No | 446 (63.9) |
| Yes | 187 (26.8) |
| No partner in past 12 months | 65 (9.3) |
| IPV: any sexual coercion | |
| No | 565 (80.4) |
| Yes | 73 (10.4) |
| No partner in past 12 months | 65 (9.2) |
Total for each variable does not always equal 709 because there were nonresponses for some variables. Total does not always equal to 100% due to rounding
CES-D Center for Epidemiologic Studies—Depression
Over half of the mothers were married to or living with a partner. Most of the mothers had health insurance, but over a third lived below the household poverty level and a fifth were unemployed in the past year. Thirteen percent of the mothers had less than a high school education. Furthermore, most mothers reported having some family members or friends helping them in most areas of social support, but a majority of the mothers reported having no membership or not being active or fairly active in voluntary groups.
The mean total CES-D score was 12 (range: 0–55); 28.4% of mothers scored positive for depressive symptoms. Nearly 45% of mothers reported never using illicit drugs, 49.1% reported past use only, and 6.4% reported past and current use. Nine percent of mothers had problem alcohol use in the past year. Nearly 16% of mothers experienced no intimate partner violence, 73.9% any psychological aggression, 26.8% any physical assault, and 10.4% any sexual coercion.
A correlation matrix (not shown) revealed that the “need” factors were not highly correlated. Furthermore, the mean variance inflation factor for the “need” factors was 1.04, an indication of low collinearity among the items.
Type of care
Overall, 21% (n=151) of the mothers reported lifetime receipt of outpatient or inpatient mental health/substance abuse services. Of the 151 who received mental health/substance abuse services, 20 (13%) mothers received both inpatient and outpatient services, 125 (83%) used only outpatient services, and six (4%) used only inpatient services.
In terms of types of care, 13% of the mothers reported receiving only professional care, 3% only nonprofessional care, and 6% both professional and nonprofessional care (Table 2). Among mothers who did not report utilizing any mental health/substance abuse services, less than 10% had stated that they had “ever wanted or needed services”; therefore, because of this small number, this variable was not examined as an outcome.
Table 2.
“Ever Utilized” and “Never Used but Wanted or Needed” mental health/substance use services, by type of care (n=709)
| Type of care | Ever utilized # (%) | Never used but wanted/needed # (%) |
|---|---|---|
| Professional onlya | 91 (12.8) | 42 (5.9) |
| Non-professional onlyb | 19 (2.7) | 11 (1.6) |
| Both professional and non-professional | 41 (5.8) | 16 (2.2) |
| Any care (professional and/or nonprofessional) | 151 (21.3) | 69 (9.7) |
| None | 558 (78.7) | 640 (90.3) |
| Total | 709 (100.0) | 709 (100.0) |
“Professional” included: (1) community mental health center/other outpatient mental health clinic; (2) professional care (e.g., psychologist, psychiatrist, social worker, or family counselor not part of service/clinic already mentioned); (3) partial hospitalization; (4) emergency room; and (5) family doctor
“Nonprofessional” included: (1) in-home therapist/counselor/family preservation worker; (2) any other kind of counselor; (3) support group; (4) priest/minister/rabbi; (5) healer/kahuna/spiritualist; and (6) acupuncturist/chiropractor/naturopath
Bivariate analyses in utilization of mental health/substance abuse services
Bivariate analyses revealed that race was significantly associated with use of mental health/substance abuse services. Compared with white mothers, Asian (unadjusted odds ratio [OR]=0.43 [95% confidence interval {CI}=0.25, 0.76]) and NHOPI (unadjusted OR=0.53 [95% CI=0.30, 0.93]) were significantly less likely to have received services.
Bivariate analyses also showed that use of mental health/substance abuse treatment services did not significantly differ by risk for child maltreatment or study group or by two predisposing characteristics—age and education. However, other predisposing characteristics and enabling resources were found to be significantly associated with service use. Specifically, compared with mothers who were married or living with a partner, mothers who were single/separated/divorced/widowed were significantly more likely to have used services (unadjusted OR=2.30 [95% CI=1.59, 3.31]). In addition, mothers who had public health insurance (vs. private; unadjusted OR=1.71 [95% CI=1.17, 2.49]), been unemployed in the past 12 months (vs. having one or more jobs; unadjusted OR=1.59 [95% CI=1.04, 2.44]), and were living under the household poverty level (unadjusted OR=1.64 [95% CI=1.13, 2.38]) were also significantly more likely to have used services.
In terms of social support, mothers who had help with one or more daily tasks were less likely to ever receive services compared with mothers who had no help (unadjusted OR=0.92 [95% CI=0.86, 0.99]). Furthermore, for each additional person a mother could count on in time of crises, the unadjusted OR increased by 2% (95% CI=1.00, 1.05). However, having emergency child care, having regular talks with another person, attending religious services, and involvement in voluntary groups did not play a significant role in use of services. Furthermore, satisfaction with the number of visits from kin did not play a significant role in ever utilizing services among mothers who said they see one or more relatives a week. Mothers who reported seeing no relatives, however, were significantly more likely to ever utilize services compared with mothers who reported seeing at least one relative per week and were satisfied with the number of visits (unadjusted OR=1.74 [95% CI=1.10, 2.76]). Finally, mothers who reported being dissatisfied or very dissatisfied with communication from their male partner compared with mothers who reported being very satisfied were significantly more likely to have used services (unadjusted OR=2.86 [95% CI=1.44, 5.71]), but there was no significant difference among mothers who reported being satisfied.
All of the need factors were found to play significant roles in the bivariate analyses. In particular, mothers who were positive for depression were significantly more likely to have used services (unadjusted OR: 2.56 [95% CI=1.76, 3.73]). Mothers who reported illicit drug use in the past, regardless of current use, were significantly more likely to have utilized services compared with mothers who never had illicit drug use. The unadjusted OR for those with past illicit drug use but no current use was 2.92 (95% CI=1.92, 4.45); the unadjusted OR for those with past and current use was 6.20 (95% CI=3.13, 12.27). Mothers with vs. without problem alcohol use in the past year were significantly more likely to have received services (unadjusted OR=2.44 [95% CI=1.42, 4.21]).
Lastly, compared with mothers who reported having no lifetime experience with intimate partner violence, mothers who reported having past and/or current experience with intimate partner violence (e.g., psychological aggression, physical assault, or sexual coercion) were significantly more likely to have received services (unadjusted OR=3.16 [95% CI=1.40, 7.15]). Additionally, compared with mothers who reported having no lifetime experience with physical assault, mothers who reported having any lifetime experience with physical assault (unadjusted OR=1.78 [95% CI=1.18, 2.67]) were significantly more likely to have received services. Compared with mothers who reported having no lifetime experience with sexual coercion, mothers who reported having any lifetime experience with sexual coercion (unadjusted OR: 2.51 [95% CI=1.49, 4.24]) were significantly more likely to have received services.
Racial disparities in utilization of mental health/substance abuse services
Table 3 shows the results of the final multivariate logistic regression model. There were no significant differences in receipt of mental health/substance abuse services by risk for child maltreatment. Mothers who were 34 years old or younger compared with those who were 35 years old or older were significantly less likely to have received services (adjusted OR=0.40 [95% CI=0.21, 0.77]). There were no significant differences by marital status and health insurance; however, mothers with a high school education compared with some college or more were significantly less likely to have received services (adjusted OR=0.59 [95% CI=0.35, 0.98]). Mothers who lived below the household poverty level compared with above the household poverty level were significantly more likely to have received services (adjusted OR=1.73 [95% CI=1.02, 2.93]). In terms of social support, for each additional person a mother could count on in time of crises, the adjusted OR increased by 4% (95% CI=1.01, 1.07). Mothers who reported past use of illicit drugs were significantly more likely to have received mental health/substance abuse services. Specifically, the adjusted OR for past illicit drug use but not current illicit drug use was 2.62 (95% CI=1.63, 4.23), and the adjusted OR for past and current illicit drug use was 5.18 (95% CI=2.32, 11.59). Problem alcohol use and experience with psychological aggression or physical assault were not found to be significantly associated with use of services. Additionally, mothers with experience with sexual coercion compared with no experience with sexual coercion were significantly more likely to have received services (adjusted OR=2.27 [95% CI=1.19, 4.32]).
Table 3.
Prevalence of utilization and multivariate analyses for mental health/substance abuse services (n=709)
| Variable | Prevalence # (%) | OR (95% CI) |
|---|---|---|
| Risk for child maltreatment | ||
| Not at-riska (n=218) | 38 (17.4) | 1.00 (Reference) |
| At-risk (n=491) | 113 (23.0) | 1.21 (0.70, 2.10) |
| Age | ||
| 35+a (n=71) | 21 (29.6) | 1.00 (Reference) |
| <35 (n=637) | 130 (20.4) | 0.40 (0.21, 0.77)* |
| Marital status | ||
| Married/living togethera (n=438) | 97 (22.2) | 1.00 (Reference) |
| Single/divorced/separated/widowed) (n=267) | 103 (38.6) | 1.60 (0.98, 2.61) |
| Health care insurance | ||
| Privatea (n=419) | 80 (19.1) | 1.00 (Reference) |
| Public (n=223) | 64 (28.7) | 1.05 (0.61, 1.82) |
| None (n=62) | 7 (11.3) | 0.42 (0.17, 1.05) |
| Education | ||
| Some college or morea (n=394) | 93 (23.6) | 1.00 (Reference) |
| High school (n=221) | 38 (17.2) | 0.59 (0.35, 0.98)** |
| Less than high school (n=93) | 20 (21.5) | 0.52 (0.27, 1.02) |
| Household poverty level | ||
| Abovea (n=460) | 86 (18.7) | 1.00 (Reference) |
| Under (n=237) | 65 (27.4) | 1.73 (1.02, 2.93)** |
| Social support: help with crises (continuous) | 1.04 (1.01, 1.07)** | |
| 0 (n=17) | 12 (32.4) | |
| 1–2 (n=60) | 18 (30.0) | |
| 3–5 (n=315) | 34 (20.4) | |
| 6+ (n=222) | 51 (23.0) | |
| Illicit drug use | ||
| Noa (n=315) | 36 (11.4) | 1.00 (Reference) |
| Yes in past, but not currently/in past 12 months (n=347) | 97 (27.4) | 2.62 (1.63, 4.23)* |
| Yes in past and currently/in past 12 months (n=45) | 20 (44.4) | 5.18 (2.32, 11.59)* |
| Problem alcohol use | ||
| Noa (n=639) | 170 (26.5) | 1.00 (Reference) |
| Yes (n=64) | 30 (46.9) | 1.41 (0.73, 2.70) |
| Any psychological aggression | ||
| Noa (n=117) | 18 (15.4) | 1.00 (Reference) |
| Yes (n=515) | 150 (29.1) | 0.78 (0.42, 1.44) |
| No partner in past 12 months (n=65) | 26 (40.0) | 1.41 (0.63, 3.18) |
| Any physical assault | ||
| Noa (n=446) | 76 (17.0) | 1.00 (Reference) |
| Yes (n=187) | 50 (26.7) | 1.13 (0.68, 1.89) |
| No partner in past 12 months (n=65) | 22 (33.9) | b |
| Any sexual coercion | ||
| Noa (n=565) | 138 (24.4) | 1.00 (Reference) |
| Yes (n=72) | 35 (48.6) | 2.27 (1.19, 4.32)** |
| No partner in past 12 months (n=65) | 26 (40.0) | b |
| Interaction: depressive symptoms and race | ||
| Depressive symptoms (no; n=505) | ||
| Whitea (n=76) | 16 (21.1) | 1.00 (Reference) |
| Asian (n=163) | 23 (14.1) | 1.01 (0.46, 2.22) |
| Native Hawaiian/Other Pacific Islander (n=121) | 13 (10.7) | 0.73 (0.30, 1.77) |
| No primary racial affiliation/other (n=145) | 31 (21.4) | 1.41 (0.67, 2.96) |
| Depressive symptoms (yes; n=200) | ||
| Whitea (n=21) | 13 (61.9) | 1.00 (Reference) |
| Asian (n=55) | 11 (20.0) | 0.18 (0.05, 0.66)* |
| Native Hawaiian/Other Pacific Islander (n=68) | 21 (30.9) | 0.25 (0.07, 0.84)** |
| No primary racial affiliation/other (n=56) | 22 (39.3) | 0.41 (0.12, 1.40) |
Results represent the final model with interactions and adjusted OR (95% CI) for the association between the variable and outcome (lifetime use of mental health/substance abuse services vs. no lifetime use of mental health/substance abuse services)
Statistically significant at p≤0.01
Statistically significant at p≤0.05
Reference group
Dropped due to collinearity
There was a significant interaction between race and depressive symptoms. Among mothers with depressive symptoms or identified to be positive for depression, the adjusted ORs for lifetime receipt of mental health/substance abuse services for Asians was 0.18 (95% CI=0.05, 0.66) and NHOPI was 0.25 (95% CI=0.07, 0.84) compared with whites. Among mothers who were identified negative for depression, no racial differences were found.
Discussion
This study addressed the field’s limited understanding of the lifetime prevalence of utilization of mental health and substance abuse services by Asian and NHOPI women in the USA. About one-fifth of mothers reported receiving services, which is similar to the National Comorbidity Survey Replication’s finding that the 1-year prevalence of use of services for mental health or alcohol/drug use among the adult population in the USA was 18%.55
This study also sought to identify racial disparities in mothers’ utilization of mental health or substance abuse treatment services. Among mothers who screened positive for depression, Asians and NHOPI were significantly less likely to have ever received mental health/substance abuse services compared with whites—This dispels the Model Minority Myth by revealing that Asians and NHOPI are not “better off” and health care disparities do exist. The CES-D scale is often used as a screening tool to identify persons at risk for depression. The study finding demonstrates that, among those who have demonstrated a need for such services, Asian and NHOPI mothers are less likely to access services to address their need. These results are consistent with previous research17,56 but extend the field’s understanding by providing separate estimates for Asian and NHOPI women. Factors that may help explain this study finding include clinician bias (e.g., underdiagnosis in Asians and NHOPI because they are “problem-free”),6,8,11 stigma,6,8,11,17,57 loss of face,11,57 financial cost,11 limited English,6,8,11 different cultural expressions and perceptions of problems,6,8,11 availability and accessibility of services,8,57 and lack of culturally appropriate services.6,8,11,16–18,57 Further research is needed to identify factors related to the underutilization of mental health/substance abuse services among depressed Asian and NHOPI mothers.
Furthermore, this study also identified factors that were significantly associated with receipt of services for mothers overall. For example, the predisposing characteristics, age (being 34 years old or younger compared with 35+ years old), and education (having a high school education compared with some college or more) were significantly associated with not having received services. The enabling resources, household poverty level (living under compared with above), and social support (having person[s] they can count on in time of crises) were significantly associated with having received services. The need factors, illicit drug use (past and/or current use compared with no use) and experience with sexual coercion (lifetime experience compared with none), were also significantly associated with having received services.
Strengths
The study’s findings add to the literature on the prevalence of mental health/substance abuse services and identification of the “need” factors that are associated with the utilization of mental health/substance abuse services among Asian and NHOPI women. Another strength of this study was that validated and widely used instruments were used to assess the “need” factors during the follow-up interviews with the HSP study participants.
Limitations and recommendations for future research
These results should be interpreted with the following limitations in mind. First, data collection methods combined use of mental health and substance abuse treatment as a single variable. These services are different in nature, and it is possible that there are different barriers and facilitators to treatment seeking for mental health vs. substance abuse services; therefore, it is suggested that future research separate the mental health services questions from the substance abuse services questions to better examine these possibilities. Second, the temporal sequence could not be established. Third, although the outcome was derived from self-reported data, it is unclear whether having medical records data would have provided a more accurate assessment of receipt of mental health or substance abuse treatment services. It is possible that the study underestimated use of services from nonprofessional providers. Unfortunately, a review of participants’ medical records for lifetime utilization of services was not feasible. Fourth, the study had a small sample size for certain subgroups. For instance, the study could not examine differences between mothers who reported that they wanted or needed mental health or substance abuse services compared with mothers who did not report that they wanted or needed such services. The study results also strongly encourage the need for additional research with a larger sample size because of the significant racial differences found among those with depressive symptoms.
Fifth, reporting bias for substance use or intimate partner violence may be present if respondents preferred not to report unfavorable experiences for reasons such as stigma or shame. Sixth, because the study’s inclusion criteria included English proficiency, the study’s findings cannot be generalized to those with limited English proficiency; however, very few families were ineligible for the study because of limited English proficiency. Lastly, although the HSP survey used some of the terminology for the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) diagnostic criteria of substance dependence and abuse, the respondents were not specifically asked whether these symptoms/experiences (e.g., withdrawal, tolerance) had occurred in the “past 12 months,” which must be specified to meet DSM-IV criteria for a diagnosis of substance abuse or dependence.58
Implications for Behavioral Health
Studies have documented the consequences of untreated mental health/substance use disorders. Asian and NHOPI women, in particular, have the highest prevalence of suicide among those 65 years old or older compared to their counterparts in other racial groups.59,60 The results presented in this study highlight the urgent need to develop strategies to reduce health care disparities among Asian and NHOPI. One might reason that service use would not differ by race in Hawaii because there is no majority racial group. The study results strongly suggest otherwise—This is consistent with the literature that there are racial disparities in health care use.16,61 Further research is needed to recognize the barriers and facilitators to treatment seeking for mental health/substance abuse services. It is also crucial to consider the role of culture in influencing an Asian and NHOPI woman’s decision to seek needed treatment.
Effective treatments exist and may significantly decrease society’s economic burden,9 but the challenge is twofold: (1) to dispel the misperception that all Asians and NHOPI are the same and, therefore, have similar experiences with mental health/substance use disorders; and (2) to reevaluate the nation’s mental health/substance use health care system’s current ability to provide care to Asian and NHOPI women.
Acknowledgments
V.M. Ta conceived of the study, conducted and synthesized analyses, and contributed to the main draft of the manuscript. H.S. Juon provided technical expertise in the area of Asian and Pacific Islander health and statistical guidance. A.C. Gielen provided technical expertise in the area of intimate partner violence and assisted with synthesizing analyses. D. Steinwachs provided technical expertise in the area of mental health. A. Duggan was the principal investigator of the parent study and provided background knowledge of the data source. All authors helped to conceptualize ideas, interpret findings, and review drafts of the manuscript.
Work for this publication were supported by the National Institute of Drug Abuse (NIDA) University of California San Francisco Treatment Research Center Grant (P50 DA09253) and the NIDA Training Grant (T32 DA07250); the federal Maternal and Child Health Bureau (R40 MC 00029; formerly MCJ 240637) and R40MC00123 (formerly MCJ 240838); the Robert Wood Johnson Foundation (18303); the Annie E. Casey Foundation (94-4041); the David and Lucile Packard Foundation (93-6051, 94-7957, 97-8058, and 98-3448); the Hawaii State Department of Health (99-29-J), and National Institute of Health (R01MH60733).
The original dissertation research was conducted at The Johns Hopkins University Bloomberg School of Public Health, Department of Health Policy and Management, 624 N. Broadway, Baltimore, MD 21205. Final editing for this manuscript was conducted at the University of California, San Francisco/San Francisco General Hospital, 1001 Potrero Ave., Ward 21, San Francisco, CA 94110.
Contributor Information
Hee-soon Juon, Department of Health, Behavior & Society, School of Public Health, The Johns Hopkins University, 624 N. Broadway, Room 712, Baltimore, MD, 21205, USA. Telephone: +1-410-6145410. Fax: +1-410-6142797. Email: hjuon@jhsph.edu.
Andrea C. Gielen, Department of Health, Behavior & Society, Center for Injury Research and Policy, School of Public Health, The Johns Hopkins University, 624 N. Broadway, Room 557, Baltimore, MD, 21205, USA. Telephone: +1-410-9552397. Fax: +1-410-6142797. Email: agielen@jhsph.edu.
Donald Steinwachs, Department of Health Policy and Management, Health Services Research and Development Center, School of Public Health, The Johns Hopkins University, 624 N. Broadway, Room 652, Baltimore, MD, 21205, USA. Telephone: +1-410-9556562. Fax: +1-410-9550470. Email: dsteinwa@jhsph.edu
Anne Duggan, Department of Pediatrics, School of Medicine, The Johns Hopkins University, 1620 McElderry St, Rm 203 Reed Hall, Baltimore, MD, 21205, USA. Telephone: +1-410-6140912. Fax: +1-410-6145431. Email: aduggan@jhmi.edu.
References
- 1.US Department of Health and Human Services. Healthy people 2010: Mental health and mental disorders. [Accessed March 9, 2005]; Available at: http://www.healthypeople.gov/document/html/volume2/18mental.htm.
- 2.Ingram R, Scott W, Siegle G. Depression: social and cognitive aspects. In: Millon TBP, Davis R, editors. Oxford Textbook of Psychopathology. New York, NY: Oxford University; 1999. pp. 203–226. [Google Scholar]
- 3.National Institute of Mental Health. Women and depression. [Accessed December 17, 2004]; Available at: http://www.nimh.nih.gov/publicat/depresfact.cfm.
- 4.Johnson CD, Misra D. Mental health. In: Misra D, editor. Women’s Health Data Book: A Profile of Women’s Health in the United States. 3. Washington, DC: Jacobs Institute of Women’s Health and The Henry J. Kaiser Family Foundation; 2001. pp. 104–117. [Google Scholar]
- 5.Institute of Medicine. Introduction and literature review. In: Smedley BD, Stith AY, Nelson AR, editors. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003. pp. 29–79. [PubMed] [Google Scholar]
- 6.Good MD, James C, Good BI, et al. The culture of medicine and racial, ethnic, and class disparities in healthcare. In: Smedley BD, Stith AY, Nelson AR, editors. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: The National Academies Press; 2003. pp. 594–625. [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality. 2004 National Healthcare Disparities Report. AHRQ Publication No. 05-0014. Rockville, MD: Agency for Healthcare Research and Quality; 2004. [Google Scholar]
- 8.US Department of Health and Human Services. Mental Health: Culture, Race, and Ethnicity—A Supplement to Mental Health: A Report of the Surgeon General. Inventory No. SMA-01-3613. Rockville: Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2001. [Google Scholar]
- 9.National Institute on Drug Abuse. [Accessed September 27, 2005];NIDA InfoFacts: Drug Addiction Treatment Methods. Available at: http://www.nida.nih.gov/infofacts/treatmeth.html.
- 10.Greenberg PE, Stiglin LE, Finkelstein SN, et al. The economic burden of depression in 1990. The Journal of Clinical Psychiatry. 1993;54(11):405–418. [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services. [Accessed January 24, 2005];The Fundamentals of Mental Health and Mental Illness. Available at: http://www.surgeongeneral.gov/library/mentalhealth/home.html.
- 12.Longshore D, Hsieh SC, Anglin MD, et al. Ethnic patterns in drug abuse treatment utilization. Journal of Mental Health Administration. 1992;19(3):268–277. doi: 10.1007/BF02518991. [DOI] [PubMed] [Google Scholar]
- 13.Grella CE, Stein JA. Impact of program services on treatment outcomes of patients with comorbid mental and substance use disorders. Psychiatric Services. 2006;57(7):1007–1015. doi: 10.1176/appi.ps.57.7.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells K, Klap R, Koike A, et al. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. The American Journal of Psychiatry. 2001;158(12):2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt L, Greenfield T, Mulia N. Unequal treatment: racial and ethnic disparities in alcoholism treatment services. Alcohol Research and Health. 2006;29(1):49–54. [PMC free article] [PubMed] [Google Scholar]
- 16.Chow JC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. American Journal of Public Health. 2003;93(5):792–797. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herrick CA, Brown HN. Underutilization of mental health services by Asian-Americans residing in the United States. Issues in Mental Health Nursing. 1998;19(3):225–240. doi: 10.1080/016128498249042. [DOI] [PubMed] [Google Scholar]
- 18.Ro M. Moving forward: addressing the health of Asian American and Pacific Islander women. American Journal of Public Health. 2002;92(4):516–519. doi: 10.2105/ajph.92.4.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Substance Abuse and Mental Health Services Administration. Asian/Pacific Islander Americans and Substance Abuse. Prevention Alert. 7. Vol. 5. Rockville: U.S. Department of Health & Human Services. Substance Abuse and Mental Health Services Administration; 2002. [Google Scholar]
- 20.Substance Abuse and Mental Health Services Administration. Office of Applied Studies, National Opinion Research Center. [Accessed September 30, 2005];Prevalence of Substance Use Among Racial & Ethnic subgroups in the US. Available at: http://oas.samhsa.gov/NHSDA/Ethnic/ethn1001.htm.
- 21.Reeves T, Bennett C. The Asian and Pacific Islander Population in the United States: March 2002. Current Population Reports. Washington, DC: U.S. Census Bureau; 2005. pp. 20–540. [Google Scholar]
- 22.Walsh D, Sorensen G, Leonard L. Gender, Health, and Cigarette Smoking. In: Amick BI, Levine S, Tarlov A, et al., editors. Society and Health. New York, NY: Oxford University Press; 1995. pp. 131–171. [Google Scholar]
- 23.Duggan A, Fuddy L, Burrell L, et al. Randomized trial of a statewide home visiting program to prevent child abuse: impact in reducing parental risk factors. Child Abuse & Neglect. 2004;28(6):623–643. doi: 10.1016/j.chiabu.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 24.Duggan A, McFarlane E, Fuddy L, et al. Randomized trial of a statewide home visiting program: impact in preventing child abuse and neglect. Child Abuse & Neglect. 2004;28(6):597–622. doi: 10.1016/j.chiabu.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Duggan A, Windham A, McFarlane E, et al. Hawaii’s healthy start program of home visiting for at-risk families: evaluation of family identification, family engagement, and service delivery. Pediatrics. 2000;105(1 Pt 3):250–259. [PubMed] [Google Scholar]
- 26.Duggan AK, McFarlane EC, Windham AM, et al. Evaluation of Hawaii’s healthy start program. Future Child. 1999;9(1):66–90. discussion 177–178. [PubMed] [Google Scholar]
- 27.Kempe H. Child Abuse and Neglect: The Family and the Community. Cambridge, MA: Ballinger Publishing Company; 1976. [Google Scholar]
- 28.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health & Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 29.Harada N, Kim L. Use of mental health services by older Asian and Pacific Islander Americans. In: Padgett DK, editor. Handbook on Ethnicity, Aging, and Mental Health. Westport, CT: Greenwood Press; 1995. pp. 185–202. [Google Scholar]
- 30.Goldston DB, Reboussin BA, Kancler C, et al. Rates and predictors of aftercare services among formerly hospitalized adolescents: a prospective naturalistic study. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(1):49–56. doi: 10.1097/00004583-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 31.de Boer AG, Wijker W, de Haes HC. Predictors of health care utilization in the chronically ill: a review of the literature. Health Policy. 1997;42(2):101–115. doi: 10.1016/s0168-8510(97)00062-6. [DOI] [PubMed] [Google Scholar]
- 32.Booth BM, Staton M, Leukefeld C. Substance use health services research. Substance Use & Misuse. 2001;36(6–7):673–685. doi: 10.1081/ja-100104084. [DOI] [PubMed] [Google Scholar]
- 33.Andersen R, Newman J. Societal and individual determinants of medical care utilization in the United States. Milbank Quarterly. 1973;51:95–124. [PubMed] [Google Scholar]
- 34.Pascoe JM, Ialongo NS, Horn WF, et al. The reliability and validity of the maternal social support index. Family Medicine. 1988;20(4):271–276. [PubMed] [Google Scholar]
- 35.Pascoe JM, French J. The reliability and validity of the Maternal Social Support Index for primiparous mothers: a brief report. Family Medicine. 1990;22(3):228–230. [PubMed] [Google Scholar]
- 36.McCurdy K. Can home visitation enhance maternal social support? American Journal of Community Psychology. 2001;29(1):97–112. doi: 10.1023/A:1005201530070. [DOI] [PubMed] [Google Scholar]
- 37.Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 38.Windham AM, Rosenberg L, Fuddy L, et al. Risk of mother-reported child abuse in the first 3 years of life. Child Abuse & Neglect. 2004;28(6):645–667. doi: 10.1016/j.chiabu.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 39.Furukawa T, Hirai T, Kitamura T, et al. Application of the center for epidemiologic studies depression scale among first-visit psychiatric patients: a new approach to improve its performance. Journal of Affective Disorders. 1997;46(1):1–13. doi: 10.1016/s0165-0327(97)00079-7. [DOI] [PubMed] [Google Scholar]
- 40.Ying YW, Lee PA, Tsai JL, et al. The conception of depression in Chinese American college students. Cultural Diversity & Ethnic Minority Psychology. 2000;6(2):183–195. doi: 10.1037/1099-9809.6.2.183. [DOI] [PubMed] [Google Scholar]
- 41.Chung H, Teresi J, Guarnaccia P, et al. Depressive symptoms and psychiatric distress in low income Asian and Latino primary care patients: prevalence and recognition. Community Mental Health Journal. 2003;39(1):33–46. doi: 10.1023/a:1021221806912. [DOI] [PubMed] [Google Scholar]
- 42.Kaholokula JK, Haynes SN, Grandinetti A, et al. Biological, psychosocial, and sociodemographic variables associated with depressive symptoms in persons with type 2 diabetes. Journal of Behavioral Medicine. 2003;26(5):435–458. doi: 10.1023/a:1025772001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grandinetti A, Kaholokula JK, Crabbe KM, et al. Relationship between depressive symptoms and diabetes among Native Hawaiians. Psychoneuroendocrinology. 2000;25(3):239–246. doi: 10.1016/s0306-4530(99)00047-5. [DOI] [PubMed] [Google Scholar]
- 44.Prescott CA, McArdle JJ, Hishinuma ES, et al. Prediction of major depression and dysthymia from CES-D scores among ethnic minority adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(5):495–503. doi: 10.1097/00004583-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 45.Yuen NY, Nahulu LB, Hishinuma ES, et al. Cultural identification and attempted suicide in Native Hawaiian adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(3):360–367. doi: 10.1097/00004583-200003000-00019. [DOI] [PubMed] [Google Scholar]
- 46.Yuen N, Andrade N, Nahulu L, et al. The rate and characteristics of suicide attempters in the Native Hawaiian adolescent population. Suicide & Life-Threatening Behavior. 1996;26(1):27–36. [PubMed] [Google Scholar]
- 47.Nahulu LB, Andrade NN, Makini GK, Jr, et al. Psychosocial risk and protective influences in Hawaiian adolescent psychopathology. Cultural Diversity & Mental Health. 1996;2(2):107–114. [PubMed] [Google Scholar]
- 48.Ewing JA. Detecting alcoholism. The CAGE questionnaire. The Journal of the American Medical Association. 1984;252(14):1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 49.Straus M, Hamby S, McCoy S, et al. The revised conflict tactics scales (CTS2): development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. [Google Scholar]
- 50.Yick AG, Shibusawa T, Agbayani-Siewert P. Partner violence, depression, and practice implications with families of Chinese descent. Journal of Cultural Diversity. 2003;10(3):96–104. [PubMed] [Google Scholar]
- 51.Hicks MH, Li Z. Partner violence and major depression in women: a community study of Chinese Americans. Journal of Nervous and Mental Disease. 2003;191(11):722–729. doi: 10.1097/01.nmd.0000095124.05023.e1. [DOI] [PubMed] [Google Scholar]
- 52.Lau Y. Does pregnancy provide immunity from intimate partner abuse among Hong Kong Chinese women? Social Science & Medicine. 2005;61(2):365–377. doi: 10.1016/j.socscimed.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 53.Alvi S, Schwartz MD, DeKeseredy W, et al. Victimization and attitudes towards woman abuse of impoverished minority women. Western Criminology Review. 2005;6(1):1–11. [Google Scholar]
- 54.Stata Statistical Software: Release 9.0. College Station, TX: Stata Corporation; 2005. [computer program] Version. [Google Scholar]
- 55.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 56.Matsuoka J, Breaux C, Ryujin D. National utilization of mental health services by Asian Americans/Pacific Islanders. Journal of Community Psychology. 1997;25(2):141–145. [Google Scholar]
- 57.Kim-Goh M, Yamamoto J, Suh C. Characteristics of Asian/Pacific Islander psychiatric patients in a public mental health system. Asian American and Pacific Islander Journal of Health. 1994;2(2):125–132. [PubMed] [Google Scholar]
- 58.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, DSM-IV. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 59.Liang SL. Overcoming Stigma in Asian American Mental Health. [Accessed November 10, 2004]; Available at: http://www.medscape.com/viewarticle/491353_print.
- 60.National Center for Injury Prevention and Control. WISQARS Injury Mortality Reports, 2000–2002. [Accessed July 30, 2006]; Available at: http://webappa.cdc.gov/sasweb/ncipc/mortrate10.html.
- 61.Byrd W, Clayton L. Racial and ethnic disparities in healthcare: a background and history. In: Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine of the National Academies; 2003. pp. 455–527. [PubMed] [Google Scholar]