Abstract
Though multiple islet autoantigens are recognized by T lymphocytes and autoantibodies prior to the development of type 1A (immune mediated diabetes) there is increasing evidence that autoimmunity to insulin may be central to disease pathogenesis. Evidence is strongest for the NOD mouse model where blocking immune responses to insulin prevents diabetes and insulin peptides can be utilized to induce diabetes. In man insulin gene polymorphisms are associated with disease risk, and autoantibodies and T cells reacting with multiple insulin/proinsulin epitopes are present. It is not currently clear why insulin autoimmunity is so prominent and frequent and though insulin can be used to immunologically prevent diabetes of NOD mice, insulin based preventive immunoregulation of diabetes in man is not yet possible.
Keywords: Type 1 Diabetes, Autoimmunity, Autoantigen, Insulin
Introduction
Multiple autoantigens have been implicated in type1 diabetes autoimmunity. For man, as identified with specific predictive autoantibodies there are four major target autoantigens (insulin, glutamic acid decarboxylase [GAD], IA-2 [and related IA-2beta], and the zinc transporter ZNT8). For the NOD mouse only autoantibodies to insulin have been confirmed in workshops with high specificity fluid phase radioassays and a major T cell response targets the molecule islet-specific glucose-6-phosphatase catalytic subunit-related protein (IGRP). A fundamental question is whether abnormalities in immune function result in the targeting of multiple different islet autoantigens with no fixed hierarchy or a specific autoantigen is almost always the primary target followed by intermolecular epitope spreading. If there is a primary autoantigen, such as insulin, is there a primary epitope initially recognized and essential for disease with intramolecular epitope spreading. In this short review we will highlight the immune response to insulin and in particular insulin peptide B:9–23, that we believe is a primary autoantigen of the NOD mouse, and discuss human type 1 diabetes, where though insulin is a major target autoantigen, data is lacking to assess primacy of any given autoantigenic epitope.
NOD Mouse
History of murine responses to insulin and insulin/proinsulin induced Experimental Autoimmune Diabetes
Among mouse strains, the non-obese diabetes (NOD) strain spontaneously develop autoimmune diabetes along with the development of insulin autoantibodies[1]. In the early 80’s, it was reported that even diabetes-resistant mouse strains generate insulin-reactive T cells restricted with I-Ad MHC class II molecule after immunization with porcine insulin. More recently, we reported that immunizing H-2d but not H-2b mice with insulin B chain amino acids 9 to 23 peptide (insulin B:9–23) resulted in the development of insulin autoantibodies[2]. Insulin autoantibodies were induced only when mice were immunized with insulin B:9–23 peptides, and other peptides such as insulin A chain 1 to 15 peptide failed to induce antibody production. Of note, antibodies to insulin competed with insulin but not with insulin B:9–23 peptide, and thus the antibodies are truly recognizing insulin molecules not simply the immunizing peptide. In addition, immunization with the insulin B:9–23 peptide along with Polyinosinic-polycytidylic acid (poly-IC) could induce diabetes in Balb/c mice with H-2d when transgenically expressing the costimulatory B7-1 molecule in pancreatic beta cells[3]. Thus, insulin and insulin peptides are capable of inducing immune-mediated diabetes with the appropriate MHC molecules and with engineered enhanced diabetes susceptibility.
Introduction to the NOD mouse
The NOD mouse strain was established from inbreeding of the Cataract Shionogi (CTS) strain in 1974. Lymphocytic infiltration consisting of both T and B cells into pancreatic islets called “insulitis” starts around 5 weeks age, and the majority of female NOD mice develop overt diabetes by the age of 40 weeks. Similar to man, more than 20 diabetes-susceptible and –resistant genes (idd) are found in mouse such as regions containing MHC class I and II molecules (idd1), [4] interleukin 2 (IL2) and IL21 (idd3)[5], and the costimulatory molecules (e.g. CTLA-4 and ICOS) (idd5.1)[6], which suggests that the NOD mice have multiple immune “abnormalities.” Indeed, NOD mice often develop other autoimmune disorders, for instance sialitis (lymphocytic infiltration into salivary glands) and thyroiditis.
Although B cells clearly contribute to the development of autoimmune diabetes[7], T cell transfer experiments indicate that T cells mainly mediate the disease. Multiple T cell clones reacting with islet antigens have been established from pancreatic islets, lymph nodes, and the spleen of the NOD mouse, and mice transgenic for T cell receptors (TCRs) from these clones were also generated. The islet-reactive CD4 (e.g. Wegmann’s 12-4.1[8], Haskins’s BDC2.5[9], Santamaria’s 4.1[10]) and CD8 T cell clones (e.g. Santamaria’s 8.3[11;12], Wong’s G9C8[13], DiLorenzo’s AI4[14]) can induce diabetes in immuno-compromised NOD.SCID mice without any help of B cells and other T cell populations, and mice transgenic for these islet-reactive TCRs with SCID mutation or RAG-knockout develop diabetes. Thus, anti-islet autoimmunity of the NOD mouse is promoted by T cells, and these T cell clones and TCR-transgenic mice are important tools to study antigen-specific diabetes development of the NOD mouse model.
Insulin Autoantibodies
Preceding overt hyperglycemia when most of insulin-secreting pancreatic beta cells are destroyed, NOD mice spontaneously develop insulin autoantibodies (IAA)[1]. The IAA is usually detected after 6 weeks of age and reaches a peak between 8 and 16 weeks, and mice do not necessarily express positive value of IAA when diagnosed with overt diabetes. NOD mice expressing IAA at 8 weeks of age develop diabetes earlier. Interestingly, NOD mice with transgenic TCRs targeting non-insulin antigens (CD4 BDC 2.5 and 4.1, and CD8 8.3) also have higher and earlier IAA expressions, suggesting that these mice even with limitations of T cell receptor diversity imposed by transgenes are still able to mount an impressive immune response to insulin (unpublished data, collaboration with Haskins and Santamaria). Thus, the development of insulin autoantibodies has a strong association with diabetes onset and monitoring IAA is a robust predictor of diabetes development of the NOD mice.
Insulin autoantibodies themselves do not cause the disease. However, the maternal transplacental transmission of antibodies appears to influence diabetes development. Implanting NOD embryos in pseudopregnant mothers of diabetes-resistant mouse strains suppressed the diabetes development of implanted NOD progenies[15;16].
Anti-Insulin T Cell Autoimmunity
As well as humoral autoimmune responses to insulin, NOD mice also show cellular autoimmunity to insulin. Wegmann and coworkers isolated T cells directly from pancreatic islets of NOD mice and found that the significant population of CD4 T cell clones established after stimulated with islets as antigen reacted with insulin and of the T cell clones reacting with insulin, more than 90% reacted with insulin peptide B:9–23[8]. These clones were capable of transferring diabetes into immunocompromised NOD.SCID mice and mice transgenic for T cell receptors of one of these clones (12-4.1) develop diabetes when H-2g7 homozygous[17]. Notably, these clones utilize a conserved TRAV5D-4 and TRAJ53 segment of the alpha chain with variation in the N region and no apparent conservation of the TCR beta chain[18]. Despite utilization of this dominant TCR alpha chain motif, one of the clones studied recognized insulin peptide B:9–16 and another four clones insulin B:13–23[19]. Unanue and coworkers recently found that the insulin B:9–23 peptide contains at least two binding registers, and it would be possible that T cells sharing the same conserved alpha chain recognize different epitopes contained in the insulin B:9–23 peptide[20]. On the other hand, the 2H6 T cell clone generated from pancreatic lymph nodes of the NOD mouse by Wen and coworkers also reacts with insulin B:9–23 and insulin B:12–25 peptides but suppresses diabetes via TGF-beta production[21]. It is interesting that the 2H6 cells utilize an alpha chain with the conserved TRAJ53 segment but with another Valpha segment, TRAV21.
CD8 T cells also target insulin. Wong and coworkers generated CD8 T cell lines and clones isolated from young NOD pancreatic islets and demonstrated that the clone called G9C8 reacted with insulin B chain amino acids 15 to 23 by screening a pancreatic islet cDNA library[22]. Tetramer analysis showed that CD8 T cells recognizing insulin B:15–23 peptide are increased in younger NOD mice[23].
Not only insulin but also proinsulin, the pre-form of insulin, is recognized by T cells of NOD mice. Proinsulin amino acids B chain 24 to C peptide 36 is identified as an epitope for CD4 T cells restricted by I-Ag7[24]. Of note, only proinsulin but not insulin is expressed in thymus.
Insulin as a Primary Autoantigen
A question is whether there are essential antigens necessary for immune-mediated diabetes. Detection of insulin reactive T cells in younger NOD mice and the development of insulin autoantibodies often preceding other autoantibodies in man contributes to the hypothesis that insulin might be essential for the development of type 1 diabetes. Mice have two preproinsulin genes (ins1 and ins2), and knockout of the ins2 gene accelerate diabetes of the NOD mouse[25;26], whereas NOD mice lacking ins1 gene are protected from diabetes development but not insulitis and insulin autoantibodies[26]. These completely opposite results might be associated with the location and levels of insulin/proinsulin expression with different sequences. Namely, proinsulin 2 is expressed in the thymus regulated by autoimmune regulator gene (Aire)[27;28] and also in pancreas, whereas proinsulin 1 is exclusively expressed in the pancreas[29].
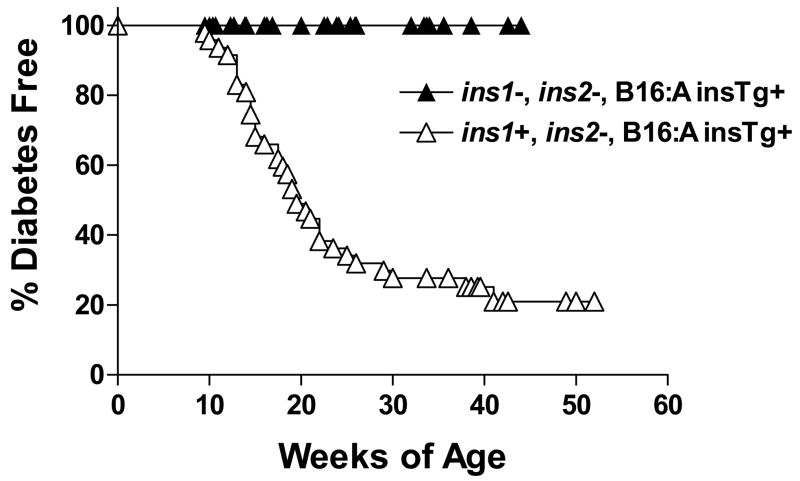
To explore whether the insulin B:9–23 peptide is essential for diabetes development of the NOD mouse, we generated NOD mice lacking both ins1 and ins2 genes. To rescue mice from hyperglycemia due to lack of insulin, we introduced a mutated insulin transgene where tyrosine at the insulin B chain 16th amino acid residue was replaced with alanine (B16:A), which does not stimulate insulin B:9–23-reactive T cell clones to proliferate[30]. NOD mice with both ins1 and ins2 knockouts and transgenic for the B16:A mutated proinsulin gene were protected from the development of anti-islet autoimmunity including insulin autoantibodies, insulitis and diabetes (Figure 1) [31]. This protection was abrogated when normal insulin B:9–23 sequence with B16:Y was provided by islet transplant or peptide immunization[32]. In addition, insulin-knockout NOD mice with the normal insulin transgene instead of the B16:A mutated insulin transgene developed insulin autoantibodies and insulitis, and thus a replacement of only a single amino acid residue restored anti-islet autoimmunity to the insulin-knockout NOD mouse.
Figure 1.
Lack of progression to diabetes of NOD mice lacking native insulin genes. Modified from Nakayama M. et al., Copyright © Nature Publishing Group from Nature 435, 2005: 220–3.
In another approach, French and Jaeckel’s groups separately investigated whether eliminating T cells reacting with proinsulin/insulin abrogates the development of islet autoimmunity of the NOD mice. They generated NOD mice transgenic for proinsulin 2 gene with MHC class II antigen promoter and found that mice are also strongly protected from diabetes development with almost no insulin-reactive T cells in periphery due to the overexpression of insulin in cells expressing MHC class II[33;34]. Moreover, Kay and coworkers reported that IGRP-reacting T cells, which usually expand in NOD mice with age, are not detected in these transgenic mice and that the immune response to IGRP is downstream of the immune response to insulin[35]. Taken together, insulin/proinsulin, especially insulin B:9–23 peptide, is mostly likely a primary autoantigen to initiate immune-mediated diabetes of the NOD mouse. It is also likely that other autoantigens contribute to diabetes development of the NOD mice and there might be other essential autoantigens.
Disease Prevention with Insulin
Various antigen-specific immunotherapies using insulin and insulin peptide have been evaluated using the NOD mouse model. Intranasal or subcutaneous administration of insulin B:9–23 peptides or an altered insulin B:9–23 delays diabetes development[36;37]. Intranasal vaccination with proinsulin DNA in combination with anti-CD40L antibody and intrathymic administration of insulin B chain prevented diabetes[38;39]. Syngeneic transplantation of hematopoietic stem cells encoding proinsulin[40] and transfer of bone marrow derived Gr-1+ myeloid cells expressing proinsulin which differentiate to dendritic cells[41] also prevented diabetes development. In terms of treating diabetes after the onset, combination therapy with anti-CD3 antibody and proinsulin 2 B24–C36 peptide reduced the recurrence of diabetes[42].
Type 1 diabetes of man
Insulin Autoantibodies
Type 1 diabetes is a chronic disease characterized by the autoimmune destruction (Type 1A) of pancreatic β-cells and severe insulin deficiency. Autoantibodies reacting with insulin, glutamic acid decarboxylase (GAD), ICA512/IA-2, I-A2 b (phogrin) and other molecules are associated with in Type 1A diabetes. The best current markers to distinguish type 1A diabetes from other forms of diabetes are the presence of anti-islet autoantibodies. Typically, autoantibodies reacting with insulin, GAD65, and I-A2 are measured. The observation that more than 90% induviduals expressing at least two of the three islet autoantibodies progress to diabetes make it possible now to predict the development of type 1A diabetes in man[43].
Anti-insulin antibodies are present for years before the development of Type 1A diabetes. Palmer and coworkers[44] found the presence of anti-insulin antibodies in patients with new-onset type 1A diabetes prior to the administration of exogenous insulin. The BABYDIAB project reported autoantibodies can be detected as early as nine months of age in offspring of diabetes parents[45;46]. Children who had high affinity IAA almost always progress to expression of multiple islet autoantibodies and insulin autoantibodies are usually the first autoantibody to appear in young children developing type 1 diabetes[1;46]. This is particularly true for infants less than 1 year of age[1]. Achenbach and coworkers have analyzed the affinity of anti-insulin autoantibodies for children followed prospectively in the BabyDiab study. A high percentage of the children who went on to develop multiple anti-islet autoantibodies or to progress to diabetes express high affinity autoantibodies (>109 l/mol). In addition the high risk, high affinity autoantibodies differed from the autoantibodies of children who failed to develop additional autoantibodies (remained IAA positive only) or had transient insulin autoantibodies in that the majority reacted well with proinsulin[46]. All high-affinity IAAs required conservation of human insulin A chain residues 8–13 and were reactive with proinsulin[46]. Isotypes of insulin autoantibodies have been evaluated in the BabyDiab study and in studies from Finland [47;48] with the observation that a broader response to insulin (including IgG3 autoantibodies) and strong IgG1 responses is associated with a somewhat greater risk of progression to diabetes.
Levels of insulin autoantibodies appear to be regulated over long periods of time in prediabetic first-degree relatives. The levels of antibodies correlate inversely with the age at which type 1 diabetes develops. Thus levels greater than 2000 nU/ml are almost exclusively found in patients who progress to type 1A diabetes prior to age 5, and less than half of individuals developing type 1A diabetes after age 15 have levels of anti-insulin autoantibodies distinguished from controls.
High levels of such antibodies are to some extent associated with DR4 and DQ8[49]. Relatives, who only express anti-insulin autoantibodies infrequently progress to overt diabetes [46], but a high proportion of anti-insulin autoantibody-positive, ICA-negative relatives under the age of 10 convert to ICA positivity.
Insulin/Proinsulin Reactive T cells
The phenotype of autoreactive T-cells of patients has been studied. These cells can be distinguished from those of control subjects by their coexpression of CD25 and CD134 and whether they are naïve or memory T cells[50]. Autoantigen-specific T-cells that recognize multiple GAD65- and preproinsulin-derived peptides and coexpressed CD25 (+) CD134 (+) were confined to patients and pre-diabetic probands. The coexpression of CD25 and the costimulatory molecule CD134 on memory T-cells provides a novel marker for type 1 diabetes-associated T-cell immunity.
Insulin epitope recognized by autoreactive T cells
In an effort to obtain access to pancreatic lymph node and intra-islet T cells we have initiated a program where cadaveric organ donors are screened in real time for the expression of anti-islet autoantibodies. Approximately 1/300 of such donors expressed multiple anti-islet autoantibodies. In a recent screening of organ donors for risk markers of type 1 diabetes, 6 cases were single insulin autoantibody positive and one were quadruple positive in 1, 507 donors in the age-group of 25–60 years[51]. It is predicted that pancreas from such individuals expressing multiple islet autoantibodies will harbor relevant T cell clones. Oligoclonal expanded T cells from prancreatic lymph node of diabetic subjects with DR4 recognized the insulin A: 1–15 epitope restricted by DR4 but not from normal control subjects. These results identify insulin-reactive, clonally expanded T cells from the site of autoinflammatory drainage in type 1 diabetics[52].
Many putative epitopes of proinsulin/insulin have been identified (table 1). Since insulin peptide B: 9–23 may be a primary autoantigen of the NOD mouse and its amino acid sequence is identical in mice and in humans, B: 9–23 may play important role in man. Alleva and coworkers have generated insulin B: 9–23 reactive cell lines from PBMCs by short time stimulation with peptide and IL-2 from recent-onset type 1 diabetic patients but didn’t find peptide reactivity in controls[53]. T cell epitope mapping of insulin was studied by using serial overlapping peptides in Japanese patients with type 1A diabetes[54]. All epitopes recognized by T cells were identified in the B-chain of insulin. B9–23, B4–18, and B12–26 were identified in some patients while most frequent epitope were B10–24 region, B1–15 and B11–25 regions.
Table 1.
Preproinsulin/Insulin epitopes with diabetes specific immune response.
| Epitope | Sequence | HLA | CD4/CD8 | Source of T cell | Identified method | Reference |
|---|---|---|---|---|---|---|
| PPI 73–90 (C17-A1) | GAGSLQP LALEGSL QKRG | DR4 | CD4 | PBMCs | ? | [55] PNAS. 1998 March 31; 95(7): 3833–3838 |
| PPI 33–47 (B9–23) | SHLVEAL YLVCGER G | DQ8 | CD4 | PBMCs | Interferon-γ enzyme –linked immunospot, 3H-thymidine proliferation | [53] J Clin Invest. 2001 January 15; 107(2): 173–180 |
| PPI 35–51 (B11–27) | LVEALYL VCGERGF FYT | CD4 | PBMCs | ELISA assay, 3H-thymidine proliferation | [56] Diabetologia 2004 Mar;47(3):439–50 | |
| PPI 48–60 (B24-C4) | FFYTPKT RREAED | DR3 | CD4 | PBMCs | 3H-thymidine proliferation, Tetramer analysis | [57] Mol.Med. 1995 Sep;1(6):625–33, [50] J Autoimmun. 2005 Nov;25(3):235–43 |
| PPI 57–73 (C13-C29) | GGGPGA GSLQPLA LEGS | CD4 | PBMCs | ELISA assay, 3H-thymidine proliferation | [56] Diabetologia 2004 Mar;47(3):439–50 | |
| PPI 90–104 (A1–15) | GIVEQCC TSICSLY Q | DR4 | CD4 | Pancreatic LN, PBMCs | IL13 ELISA assay, 3H-thymidine proliferation | [52] Nature 2005 May 12; 435: 224–228, [58] J.Exp.Med.2005 Oct 31; 202(9): 1191–1197 |
| PPI 2–10 | ALWMRL LPL | A2 | CD8 | PBMCs | IFN-γ ELISPOT | [59] Diabetes. 2007 Mar;56(3):613–21. |
| PPI 34–42(B10–18) | HLVEALY LV | A2 | CD8 | PBMCs | HLA-A2insB10–18 tetramer staining; IFN-γ ELISPOT assay | [60] P NAS. 2005 December20; 102(51): 18425–18430. [61] PNAS 2005; 102:10581–6. |
| PPI 41–50(B17–26) | LVCGERG FFY | A1 | CD8 | PBMCs | IFN-γ ELISPOT assay | [61]PNAS 2005; 102:10581–6. |
| PPI 42–51(B18–27) | VCGERGF FYT | A2/B 8 | CD8 | PBMCs | IFN-γ ELISPOT assay | [61] PNAS 2005; 102:10581–6. [59] Diabetes. 2007 Mar;56(3):613–21. |
| PPI 44–51(B20–27) | VCGERGF FYT | B8 | CD8 | PBMCs | IFN-γ ELISPOT assay | [61]PNAS 2005; 102:10581–6. |
| PPI46–54(B 22–30) | LYLVCGE RG | A24 | CD8 | PBMCs | CTL activities assay | [62] Diabetes Res Clin Pract. 2001 Mar;51(3):173–9 |
| PPI 49–57(B25-C1) | FYTPKTR RE | B8 | CD8 | PBMCs | IFN-γ ELISPOT assay | [61]PNAS 2005; 102:10581–6. |
Multiple independent studies identify the insulin B: 10–18 epitope as a target of autoreactive CD8 T cells with extremely high binding affinity for HLA-A2[60;61;63;64]. Panels of 8- to 11-mer peptide within proinsulin region 28–64 were recognized by PBMCs[63]. Four proinsulin peptides (41–50, 42–51, 44–51 and 49–57) were recognized by a high percentage of HLA-A1 and -A3; HLA-A1, -A2, -B8, and -B18; HLA-A1 and -B8; and HLA-B8 diabetic patients, respectively. Proinsulin 49–57 and 51–61peptides located within a region overlapping the B chain and C peptide. None of those peptides were recognized by PBMCs from insulin-treated type 2 diabetes patients or control individuals. Of note, T cells recognize insulin B10–18 differently in type 1A diabetes both at disease onset and after longer disease duration, but not in nondiabetic controls and type 2 diabetes[61]. Insulin B9–18, B10–18 and A12–20 were also recognized by cells from a HLA-A2 transgenic humanized mouse model[63].
Using enzyme-linked immunosorbent spot assays (ELISPOT), Peakman and coworkers identified proinsulin specific peptides (C13-C32, C19-A3 and C22-A5) to which PBMCs from diabetics and controls differentially respond. Diabetic patients respond with a pro-inflammatory phenotype with an IFN-γ response; whereas controls react to islet autoantigens with the production of IL-10 alone which suggests these cells may have a regulatory role[65].
Trials of Prevention Utilizing Insulin
It is now possible to predict type 1A diabetes in man as mentioned above and prevent it in animal models[66]. Thus there is a strong impetus to develop therapies for prevention in man with the creation of TrialNet and the Immune Tolerance Network by the National Institutes of Health. TrialNet is an expansion of the DPT-1 (Diabetes Prevention Trial) network, but with an emphasis not only on trials for diabetes prevention but also on trials to prevent further destruction of islet beta cells in patients with type 1A diabetes.
DPT-1 tested if insulin administered either both intravenously and subcutaneously or orally could prevent the development of diabetes in healthy, islet antibody-positive relatives of patients with type 1 diabetes assessed to have a high risk of developing type 1 diabetes. Subcutaneous injection of insulin did not slow progression, nor overall did oral insulin. For a subgroup of relatives in the oral trial with high levels of insulin autoantibodies there was a significant delay in progression (approximately 4.5 years)[67]. Further studies to explore the potential role of oral insulin in delaying diabetes in relatives similar to those in the subgroup with higher IAA levels is on going[68].
A trial of intranasal insulin with 38 individuals at risk for type 1 diabetes from Melbourne Pre-Diabetes Family Study suggest that intranasal insulin induces immune changes consistent with mucosal tolerance to insulin and it does not accelerate loss of β-cell function[69].
It is hypothesized that the amount of insulin that could be administered subcutaneously in man was below the relative amount needed for protection in NOD mice. With the use of insulin B chain or insulin peptides such as an altered peptide ligand of insulin B chain, B9–23, larger amounts can be administered without risk of inducing hypoglycemia. The company Neurocrine has produced an altered peptide ligand of insulin B: 9–23, with alanine replacing amino acids 16 and 19(NBI-6024) [53]. A randomized placebo controlled trail of NBI-6024 failed to preserve beta cell secretion in patients with new onset diabetes.
Insulin Autoimmune Syndrome
The insulin autoimmune syndrome (IAS) also named Hirata syndrome is characterized by severe spontaneous hypoglycemia without evidence of exogenous insulin administration, high levels of total serum immunoreactive insulin, and the presence of a high titer of anti insulin antibody. IAS has been reported mainly in Japan and so far only 27 IAS cases have been described from outside of Asia. Polyclonal IAS is essentially confined to DR4-positive individuals with DRB1*0406[70;71]. The extremely low prevalence of IAS among Caucasians may be explained by the low prevalence of DRB1*0406 in this population. Even less commonly, monoclonal insulin autoantibodies are responsible for the insulin autoimmune syndrome, without the DRB1*0406 association. Case reports identified monoclonal insulin autoantibodies in IAS patients with HLA-DRB1*0401, DRB1*0403, and DRB1*0404.
Insulin Allergy
Since the introduction of human insulin, insulin allergy occurs in less than 1% of diabetic patients treated with insulin. In these patients, different methods have been used for the treatment of insulin allergy such as oral antihistaminics, desensitization[72] and use of different insulin or insulin formulations. Allergic reactions range in severity from erythema and pruritus to life-threatening anaphylaxis. Allergic reactions to insulin usually occur within a few hours after an injection and are usually due to a local or systemic type I IgE-mediated hypersensitivity reaction[73]. IgG(4)-mediated allergic reaction to glargine insulin is also reported[74]. For delayed hypersensitivity reactions, administration of insulin with small amount of glucocorticoid in the same injection is a consideration[75].
Conclusion
There is no doubt that autoimmunity directed at insulin is a major component of the pathogenesis of type 1 diabetes of man and the NOD mouse model. In the NOD model we hypothesize that recognition of the insulin B:9–23 peptide by a non-stringent conserved Valpha and Jalpha T cell receptor combination (TRAV 5D-4*04, TRAJ53) enhances the probability of anti-insulin autoimmunity given the NOD’s penchant for autoimmunity[76]. At present, we are directly testing the potential crucial contribution of the Jalpha 53 sequence by creating NOD mice lacking the Jalpha 53(TRAJ53) segment. With the marked MHC restriction of type 1 diabetes of man, we believe that a dominant peptide will also be important for human diabetes. Human diabetes may of course be more heterogeneous than our mouse models. If however there is similar to the NOD crucial peptide determinants of disease (e.g. proinsulin/insulin), preventing such an immune response will hopefully lead to the safe prevention of type 1 diabetes.
Acknowledgments
This work is supported by grants from the National Institutes of Health (DK32083, DK55969, DK62718, AI50864, DK32493, DK064605), the Diabetes Endocrine Research Center grant from the National Institute of Diabetes and Digestive and Kidney Diseases (P30 DK57516), the American Diabetes Association, the Juvenile Diabetes Foundation (JDRF1-2006-16), and the Children’s Diabetes Foundation. L.Z is supported by ADA postdoctoral fellowship (7-06-MN-17). M.N. is supported by an advanced postdoctoral fellowship from the Juvenile Diabetes Foundation (JDRF10-2006-51).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Yu L, Robles DT, Abiru N, Kaur P, Rewers M, Kelemen K, Eisenbarth GS. Early expression of antiinsulin autoantibodies of humans and the NOD mouse: evidence for early determination of subsequent diabetes. Proc Natl Acad Sci USA. 2000;97:1701–1706. doi: 10.1073/pnas.040556697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abiru N, Maniatis AK, Yu L, Miao D, Moriyama H, Wegmann D, Eisenbarth GS. Peptide and MHC specific breaking of humoral tolerance to native insulin with the B:9–23 peptide in diabetes prone and normal mice. diab. 2001;50:1274–1281. doi: 10.2337/diabetes.50.6.1274. [DOI] [PubMed] [Google Scholar]
- 3.Moriyama H, Wen L, Abiru N, Liu E, Yu L, Miao D, Gianani R, Wong FS, Eisenbarth GS. Induction and acceleration of insulitis/diabetes in mice with a viral mimic (polyinosinic-polycytidylic acid) and an insulin self-peptide. Proc Natl Acad Sci U S A. 2002;99:5539–5544. doi: 10.1073/pnas.082120099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hattori M, Buse JB, Jackson RA, Glimcher L, Dorf ME, Minami M, Makino S, Moriwaki K, Korff M, Kuzuya H, Imura H, Seidman JG, Eisenbarth GS. The NOD mouse: recessive diabetogenic gene within the major histocompatibility complex. Science. 1986;231:733–735. doi: 10.1126/science.3003909. [DOI] [PubMed] [Google Scholar]
- 5.Podolin PL, Wilusz MB, Cubbon RM, Pajvani U, Lord CJ, Todd JA, Peterson LB, Wicker LS, Lyons PA. Differential glycosylation of interleukin 2, the molecular basis for the NOD Idd3 type 1 diabetes gene? Cytokine. 2000;12:477–482. doi: 10.1006/cyto.1999.0609. [DOI] [PubMed] [Google Scholar]
- 6.Hill NJ, Lyons PA, Armitage N, Todd JA, Wicker LS, Peterson LB. NOD Idd5 locus controls insulitis and diabetes and overlaps the orthologous CTLA4/IDDM12 and NRAMP1 loci in humans. diab. 2000;49:1744–1747. doi: 10.2337/diabetes.49.10.1744. [In Process Citation] [DOI] [PubMed] [Google Scholar]
- 7.Serreze DV, Chapman HD, Varnum DS, Hanson MS, Reifsnyder PC, Scott DR, Fleming SA, Leiter EH, Shultz LD. B lymphocytes are essential for the initiation of T cell-mediated autoimmune diabetes: analysis of a new “speed-congenic” stock of NOD. Igunull mice. J Exp Med. 1996;184:2049–2053. doi: 10.1084/jem.184.5.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8*.Daniel D, Gill RG, Schloot N, Wegmann D. Epitope specificity, cytokine production profile and diabetogenic activity of insulin-specific T cell clones isolated from NOD mice. Eur J Immunol. 1995;25:1056–1062. doi: 10.1002/eji.1830250430. Wegmann and coworkers isolated T cells directly from islets of NOD mice stimuated with “islets” as antigen and discovered responses to insulin for the majority of CD4 T cells, and for insulin responsive T cells, >90% recognized insulin peptide B:9–23. [DOI] [PubMed] [Google Scholar]
- 9.Haskins K, Portas M, Bradley B, Wegmann D, Lafferty K. T-lymphocyte clone specific for pancreatic islet antigen. Diabetes. 1988;37:1444–1448. doi: 10.2337/diab.37.10.1444. [DOI] [PubMed] [Google Scholar]
- 10.Verdaguer J, Schmidt D, Amrani A, Anderson B, Averill N, Santamaria P. Spontaneous autoimmune diabetes in monoclonal T cell nonobese diabetic mice. J Exp Med. 1997;186:1663–1676. doi: 10.1084/jem.186.10.1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nagata M, Santamaria P, Kawamura T, Utsugi T, Yoon J-W. Evidence for the role of CD8+ cytotoxic T cells in the destruction of pancreatic β-cells in nonobese diabetic mice. J Immunol. 1994;152:2042–2050. [PubMed] [Google Scholar]
- 12.Lieberman SM, Evans AM, Han B, Takaki T, Vinnitskaya Y, Caldwell JA, Serreze DV, Shabanowitz J, Hunt DF, Nathenson SG, Santamaria P, DiLorenzo TP. Identification of the {beta} cell antigen targeted by a prevalent population of pathogenic CD8+ T cells in autoimmune diabetes. Proc Natl Acad Sci USA. 2003;100:8384–8388. doi: 10.1073/pnas.0932778100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong FS, Visintin I, Wen L, Flavell RA, Janeway CA. CD8 T cell clones from young nonobese diabetic (NOD) islets can transfer rapid onset of diabetes in NOD mice in the absence of CD4 cells. J Exp Med. 1996;183:67–76. doi: 10.1084/jem.183.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lieberman SM, Takaki T, Han B, Santamaria P, Serreze DV, DiLorenzo TP. Individual nonobese diabetic mice exhibit unique patterns of CD8+ T cell reactivity to three islet antigens, including the newly identified widely expressed dystrophia myotonica kinase. J Immunol. 2004;173:6727–6734. doi: 10.4049/jimmunol.173.11.6727. [DOI] [PubMed] [Google Scholar]
- 15.Greeley SA, Katsumata M, Yu L, Eisenbarth GS, Moore DJ, Goodarzi H, Barker CF, Naji A, Noorchashm H. Elimination of maternally transmitted autoantibodies prevents diabetes in nonobese diabetic mice. Nat Med. 2002;8:399–402. doi: 10.1038/nm0402-399. [DOI] [PubMed] [Google Scholar]
- 16.Kagohashi Y, Udagawa J, Abiru N, Kobayashi M, Moriyama K, Otani H. Maternal factors in a model of type 1 diabetes differentially affect the development of insulitis and overt diabetes in offspring. Diabetes. 2005;54:2026–2031. doi: 10.2337/diabetes.54.7.2026. [DOI] [PubMed] [Google Scholar]
- 17.Jasinski JM, Yu L, Nakayama M, Li MM, Lipes MA, Eisenbarth GS, Liu E. Transgenic insulin (B:9–23) T-cell receptor mice develop autoimmune diabetes dependent upon RAG genotype, H-2g7 homozygosity, and insulin 2 gene knockout. Diabetes. 2006;55:1978–1984. doi: 10.2337/db06-0058. [DOI] [PubMed] [Google Scholar]
- 18.Simone E, Daniel D, Schloot N, Gottlieb P, Babu S, Kawasaki E, Wegmann D, Eisenbarth GS. T cell receptor restriction of diabetogenic autoimmune NOD T cells. Proc Natl Acad Sci USA. 1997;94:2518–2521. doi: 10.1073/pnas.94.6.2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abiru N, Wegmann D, Kawasaki E, Gottlieb P, Simone E, Eisenbarth GS. Dual overlapping peptides recognized by insulin peptide B:9–23 reactive T cell receptor AV13S3 T cell clones of the NOD mouse. J Autoimmun. 2000;14:231–237. doi: 10.1006/jaut.2000.0369. [DOI] [PubMed] [Google Scholar]
- 20.Levisetti MG, Suri A, Petzold SJ, Unanue ER. The insulin-specific T cells of nonobese diabetic mice recognize a weak MHC-binding segment in more than one form. J Immunol. 2007;178:6051–6057. doi: 10.4049/jimmunol.178.10.6051. [DOI] [PubMed] [Google Scholar]
- 21*.Du W, Wong FS, Li MO, Peng J, Qi H, Flavell RA, Sherwin R, Wen L. TGF-beta signaling is required for the function of insulin-reactive T regulatory cells. J Clin Invest. 2006;116:1360–1370. doi: 10.1172/JCI27030. CD4 T cells reacting with insulin peptide B:9–23 can both cause and prevent diabetes, and a T cell receptor transgenic recapitulates protection dependent upon TGFbeta. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong FS, Karttunen J, Dumont C, Wen L, Visintin I, Pilip IM, Shastri N, Pamer EG, Janeway CAJ. Identification of an MHC class I-restricted autoantigen in type 1 diabetes by screening an organ-specific cDNA library. Nat Med. 1999;5:1026–1031. doi: 10.1038/12465. [DOI] [PubMed] [Google Scholar]
- 23.Trudeau JD, Kelly-Smith C, Verchere CB, Elliott JF, Dutz JP, Finegood DT, Santamaria P, Tan R. Prediction of spontaneous autoimmune diabetes in NOD mice by quantification of autoreactive T cells in peripheral blood. J Clin Invest. 2003;111:217–223. doi: 10.1172/JCI16409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen W, Bergerot I, Elliott JF, Harrison LC, Abiru N, Eisenbarth GS, Delovitch TL. Evidence that a peptide spanning the B-C junction of proinsulin is an early autoantigen epitope in the pathogenesis of type 1 diabetes. J Immunol. 2001;167:4926–4935. doi: 10.4049/jimmunol.167.9.4926. [DOI] [PubMed] [Google Scholar]
- 25.Thebault-Baumont K, Dubois-LaForgue D, Krief P, Briand JP, Halbout P, Vallon-Geoffroy K, Morin J, Laloux V, Lehuen A, Carel JC, Jami J, Muller S, Boitard C. Acceleration of type 1 diabetes mellitus in proinsulin 2-deficient NOD mice. J Clin Invest. 2003;111:851–857. doi: 10.1172/JCI16584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moriyama H, Abiru N, Paronen J, Sikora K, Liu E, Miao D, Devendra D, Beilke J, Gianani R, Gill RG, Eisenbarth GS. Evidence for a primary islet autoantigen (preproinsulin 1) for insulitis and diabetes in the nonobese diabetic mouse. Proc Natl Acad Sci U S A. 2003;100:10376–10381. doi: 10.1073/pnas.1834450100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pugliese A, Brown D, Garza D, Zeller M, Redondo MJ, Eisenbarth GS, Patel DD, Ricordi C. Self-Antigen Presenting Cells Expressing Islet Cell Molecules in Human Thymus and Peripheral Lymphoid Organs: Phenotypic Characterization and Implications for Immunological Tolerance and Type 1 Diabetes. J Clin Invest. 2001;107:555–564. doi: 10.1172/JCI10860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson MS, Venanzi ES, Klein L, Chen Z, Berzins SP, Turley SJ, von Boehmer H, Bronson R, Dierich A, Benoist C, Mathis D. Projection of an immunological self shadow within the thymus by the aire protein. Science. 2002;298:1395–1401. doi: 10.1126/science.1075958. [DOI] [PubMed] [Google Scholar]
- 29.Chentoufi AA, Polychronakos C. Insulin expression levels in the thymus modulate insulin-specific autoreactive T-cell tolerance: the mechanism by which the IDDM2 locus may predispose to diabetes. diab. 2002;51:1383–1390. doi: 10.2337/diabetes.51.5.1383. [DOI] [PubMed] [Google Scholar]
- 30.Alleva DG, Gaur A, Jin L, Wegmann D, Gottlieb PA, Pahuja A, Johnson EB, Motheral T, Putnam A, Crowe PD, Ling N, Boehme SA, Conlon PJ. Immunological Characterization and Therapeutic Activity of an Altered-Peptide Ligand, NBI-6024, Based on the Immunodominant Type 1 Diabetes Autoantigen Insulin B-Chain (9–23) Peptide. diab. 2002;51:2126–2134. doi: 10.2337/diabetes.51.7.2126. [DOI] [PubMed] [Google Scholar]
- 31*.Nakayama M, Abiru N, Moriyama H, Babaya N, Liu E, Miao D, Yu L, Wegmann DR, Hutton JC, Elliott JF, Eisenbarth GS. Prime role for an insulin epitope in the development of type 1 diabetes in NOD mice. Nature. 2005;435:220–223. doi: 10.1038/nature03523. Mutating the insulin peptide B:9–23 from tyrosine to alanine at position B16 prevents development of diabetes of NOD mice and almost all insulitis and insulin autoantibodies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nakayama M, Beilke JN, Jasinski JM, Kobayashi M, Miao D, Li M, Coulombe MG, Liu E, Elliott JF, Gill RG, Eisenbarth GS. Priming and effector dependence on insulin B:9–23 peptide in NOD islet autoimmunity. J Clin Invest. 2007;117:1835–1843. doi: 10.1172/JCI31368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.French MB, Allison J, Cram DS, Thomas HE, Dempsey-Collier M, Silva A, Georgiou HM, Kay TW, Harrison LC, Lew AM. Transgenic expression of mouse proinsulin II prevents diabetes in nonobese diabetic mice. diab. 1996;46:34–39. doi: 10.2337/diab.46.1.34. [DOI] [PubMed] [Google Scholar]
- 34.Jaeckel E, Lipes MA, von Boehmer H. Recessive tolerance to preproinsulin 2 reduces but does not abolish type 1 diabetes. Nat Immunol. 2004;5:1028–1035. doi: 10.1038/ni1120. [DOI] [PubMed] [Google Scholar]
- 35*.Krishnamurthy B, Dudek NL, McKenzie MD, Purcell AW, Brooks AG, Gellert S, Colman PG, Harrison LC, Lew AM, Thomas HE, Kay TW. Responses against islet antigens in NOD mice are prevented by tolerance to proinsulin but not IGRP. J Clin Invest. 2006;116:3258–3265. doi: 10.1172/JCI29602. Direct demonstration that eliminating immune response to islet target IGRP does not prevent diabetes of NOD mice, while eliminating insulin response both prevents diabetes and targeting of IGRP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Daniel D, Wegmann DR. Protection of nonobese diabetic mice from diabetes by intranasal or subcutaneous administration of insulin peptide B-(9–23) Proc Natl Acad Sci USA. 1996;93:956–960. doi: 10.1073/pnas.93.2.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kobayashi M, Abiru N, Arakawa T, Fukushima K, Zhou H, Kawasaki E, Yamasaki H, Liu E, Miao D, Wong FS, Eisenbarth GS, Eguchi K. Altered B:9 23 insulin, when administered intranasally with cholera toxin adjuvant, suppresses the expression of insulin autoantibodies and prevents diabetes. J Immunol. 2007;179:2082–2088. doi: 10.4049/jimmunol.179.4.2082. [DOI] [PubMed] [Google Scholar]
- 38.Every AL, Kramer DR, Mannering SI, Lew AM, Harrison LC. Intranasal vaccination with proinsulin DNA induces regulatory CD4+ T cells that prevent experimental autoimmune diabetes. J Immunol. 2006;176:4608–4615. doi: 10.4049/jimmunol.176.8.4608. [DOI] [PubMed] [Google Scholar]
- 39.Cetkovic-Cvrlje M, Gerling IC, Muir A, Atkinson MA, Elliott JF, Leiter EH. Retardation or acceleration of diabetes in NOD/Lt mice mediated by intrathymic administration of candidate β-cell antigens. diab. 1997;46:1975–1982. doi: 10.2337/diab.46.12.1975. [DOI] [PubMed] [Google Scholar]
- 40.Steptoe RJ, Ritchie JM, Harrison LC. Transfer of hematopoietic stem cells encoding autoantigen prevents autoimmune diabetes. J Clin Invest. 2003;111:1357–1363. doi: 10.1172/JCI15995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Steptoe RJ, Ritchie JM, Jones LK, Harrison LC. Autointmune diabetes is suppressed by transfer of proinsulin-encoding Gr-1(+) myeloid progenitor cells that differentiate in vivo into resting dendritic cells. diab. 2005;54:434–442. doi: 10.2337/diabetes.54.2.434. [DOI] [PubMed] [Google Scholar]
- 42.Bresson D, Togher L, Rodrigo E, Chen YL, Bluestone JA, Herold KC, von Herrath M. Anti-CD3 and nasal proinsulin combination therapy enhances remission from recent-onset autoimmune diabetes by inducing Tregs. Journal of Clinical Investigation. 2006;116:1371–1381. doi: 10.1172/JCI27191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Achenbach P, Warncke K, Reiter J, Williams AJ, Ziegler AG, Bingley PJ, Bonifacio E. Type 1 diabetes risk assessment: improvement by follow-up measurements in young islet autoantibody-positive relatives. Diabetologia. 2006;49:2969–2976. doi: 10.1007/s00125-006-0451-9. [DOI] [PubMed] [Google Scholar]
- 44.Palmer JP, Asplin CM, Clemons P, Lyen K, Tatpati O, Raghu PK, Paquette TL. Insulin antibodies in insulin-dependent diabetics before insulin treatment. Science. 1983;222:1337–1339. doi: 10.1126/science.6362005. [DOI] [PubMed] [Google Scholar]
- 45.Hummel M, Bonifacio E, Schmid S, Walter M, Knopff A, Ziegler AG. Brief communication: Early appearance of islet autoantibodies predicts childhood type 1 diabetes in offspring of diabetic parents. Annals of Internal Medicine. 2004;140:882–886. doi: 10.7326/0003-4819-140-11-200406010-00009. [DOI] [PubMed] [Google Scholar]
- 46*.Achenbach P, Koczwara K, Knopff A, Naserke H, Ziegler AG, Bonifacio E. Mature high-affinity immune responses to (pro)insulin anticipate the autoimmune cascade that leads to type 1 diabetes. J Clin Invest. 2004;114:589–597. doi: 10.1172/JCI21307. High affinity anti-insulin autoantibodies predict development of diabetes in children followed from birth and are usually the first autoantibody to develop. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Achenbach P, Warncke K, Reiter J, Naserke HE, Williams AJ, Bingley PJ, Bonifacio E, Ziegler AG. Stratification of type 1 diabetes risk on the basis of islet autoantibody characteristics. diab. 2004;53:384–392. doi: 10.2337/diabetes.53.2.384. [DOI] [PubMed] [Google Scholar]
- 48.Hoppu S, Ronkainen MS, Kimpimaki T, Simell S, Korhonen S, Ilonen J, Simell O, Knip M. Insulin autoantibody isotypes during the prediabetic process in young children with increased genetic risk of type 1 diabetes. Pediatr Res. 2004;55:236–242. doi: 10.1203/01.PDR.0000100905.41131.3F. [DOI] [PubMed] [Google Scholar]
- 49.Redondo MJ, Babu S, Zeidler A, Orban T, Yu L, Greenbaum C, Palmer JP, Cuthbertson D, Eisenbarth GS, Krischer JP, Schatz D. Specific human leukocyte antigen DQ influence on expression of antiislet autoantibodies and progression to type 1 diabetes. J Clin Endocrinol Metab. 2006;91:1705–1713. doi: 10.1210/jc.2005-1695. [DOI] [PubMed] [Google Scholar]
- 50.Oling V, Marttila J, Ilonen J, Kwok WW, Nepom G, Knip M, Simell O, Reijonen H. GAD65- and proinsulin-specific CD4+ T-cells detected by MHC class II tetramers in peripheral blood of type 1 diabetes patients and at-risk subjects. J Autoimmun. 2005;25:235–243. doi: 10.1016/j.jaut.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 51.In’t VP, Lievens D, De Grijse J, Ling Z, van der AB, Pipeleers-Marichal M, Gorus F, Pipeleers D. Screening for insulitis in adult autoantibody-positive organ donors. Diabetes. 2007;56:2400–2404. doi: 10.2337/db07-0416. [DOI] [PubMed] [Google Scholar]
- 52.Kent SC, Chen Y, Bregoli L, Clemmings SM, Kenyon NS, Ricordi C, Hering BJ, Hafler DA. Expanded T cells from pancreatic lymph nodes of type 1 diabetic subjects recognize an insulin epitope. Nature. 2005;435:224–228. doi: 10.1038/nature03625. [DOI] [PubMed] [Google Scholar]
- 53.Alleva DG, Crowe PD, Jin L, Kwok WW, Ling N, Gottschalk M, Conlon PJ, Gottlieb PA, Putnam AL, Gaur A. A disease-associated cellular immune response in type 1 diabetics to an immunodominant epitope of insulin. J Clin Invest. 2001;107:173–180. doi: 10.1172/JCI8525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Higashide T, Kawamura T, Nagata M, Kotani R, Kimura K, Hirose M, Inada H, Niihira S, Yamano T. T cell epitope mapping study with insulin overlapping peptides using ELISPOT assay in Japanese children and adolescents with type 1 diabetes. Pediatr Res. 2006;59:445–450. doi: 10.1203/01.pdr.0000200803.72985.3c. [DOI] [PubMed] [Google Scholar]
- 55.Congia M, Patel S, Cope AP, De Virgiliis S, Sonderstrup G. T cell epitopes of insulin defined in HLA-DR4 transgenic mice are derived from preproinsulin and proinsulin. Proc Natl Acad Sci USA. 1998;95:3833–3838. doi: 10.1073/pnas.95.7.3833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Durinovic-Bello I, Schlosser M, Riedl M, Maisel N, Rosinger S, Kalbacher H, Deeg M, Ziegler M, Elliott J, Roep BO, Karges W, Boehm BO. Pro- and anti-inflammatory cytokine production by autoimmune T cells against preproinsulin in HLA-DRB1*04, DQ8 Type 1 diabetes. diabetol. 2004;47:439–450. doi: 10.1007/s00125-003-1315-1. [DOI] [PubMed] [Google Scholar]
- 57.Rudy G, Stone N, Harrison LC, Colman PG, McNair P, Brusic V, French MB, Honeyman MC, Tait B, Lew AM. Similar peptides from two β cell autoantigens, proinsulin and glutamic acid decarboxylase, stimulate T cells of individuals at risk for insulin-dependent diabetes. Mol Med. 1995;1:625–633. [PMC free article] [PubMed] [Google Scholar]
- 58.Mannering SI, Harrison LC, Williamson NA, Morris JS, Thearle DJ, Jensen KP, Kay TW, Rossjohn J, Falk BA, Nepom GT, Purcell AW. The insulin A-chain epitope recognized by human T cells is posttranslationally modified. J Exp Med. 2005;202:1191–1197. doi: 10.1084/jem.20051251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mallone R, Martinuzzi E, Blancou P, Novelli G, Afonso G, Dolz M, Bruno G, Chaillous L, Chatenoud L, Bach JM, van Endert P. CD8+ T-cell responses identify beta-cell autoimmunity in human type 1 diabetes. Diabetes. 2007;56:613–621. doi: 10.2337/db06-1419. [DOI] [PubMed] [Google Scholar]
- 60.Pinkse GG, Tysma OH, Bergen CA, Kester MG, Ossendorp F, van Veelen PA, Keymeulen B, Pipeleers D, Drijfhout JW, Roep BO. Autoreactive CD8 T cells associated with beta cell destruction in type 1 diabetes. Proc Natl Acad Sci USA. 2005;102:18425–18430. doi: 10.1073/pnas.0508621102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Toma A, Haddouk S, Briand JP, Camoin L, Gahery H, Connan F, Dubois-LaForgue D, Caillat-Zucman S, Guillet JG, Carel JC, Muller S, Choppin J, Boitard C. Recognition of a subregion of human proinsulin by class I-restricted T cells in type 1 diabetic patients. Proc Natl Acad Sci USA. 2005;102:10581–10586. doi: 10.1073/pnas.0504230102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kimura K, Kawamura T, Kadotani S, Inada H, Niihira S, Yamano T. Peptide-specific cytotoxicity of T lymphocytes against glutamic acid decarboxylase and insulin in type 1 diabetes mellitus. Diabetes Res Clin Pract. 2001;51:173–179. doi: 10.1016/s0168-8227(00)00225-4. [DOI] [PubMed] [Google Scholar]
- 63.Hassainya Y, Garcia-Pons F, Kratzer R, Lindo V, Greer F, Lemonnier FA, Niedermann G, Van Endert PM. Identification of naturally processed HLA-A2--restricted proinsulin epitopes by reverse immunology. Diabetes. 2005;54:2053–2059. doi: 10.2337/diabetes.54.7.2053. [DOI] [PubMed] [Google Scholar]
- 64.Pinkse GG, Boitard C, Tree TI, Peakman M, Roep BO. HLA class I epitope discovery in type 1 diabetes: independent and reproducible identification of proinsulin epitopes of CD8 T cells--report of the IDS T Cell Workshop Committee. Ann N Y Acad Sci. 2006;1079:19–23. doi: 10.1196/annals.1375.003. [DOI] [PubMed] [Google Scholar]
- 65.Arif S, Tree TI, Astill TP, Tremble JM, Bishop AJ, Dayan CM, Roep BO, Peakman M. Autoreactive T cell responses show proinflammatory polarization in diabetes but a regulatory phenotype in health. Journal of Clinical Investigation. 2004;113:451–463. doi: 10.1172/JCI19585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wasserfall CH, Atkinson MA. Autoantibody markers for the diagnosis and prediction of type 1 diabetes. Autoimmun Rev. 2006;5:424–428. doi: 10.1016/j.autrev.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 67.Schatz DA, Bingley PJ. Update on major trials for the prevention of type 1 diabetes mellitus: the American Diabetes Prevention Trial (DPT-1) and the European Nicotinamide Diabetes Intervention Trial (ENDIT) J Pediatr Endocrinol Metab. 2001;14 (Suppl 1):619–622. doi: 10.1515/jpem.2001.14.s1.619. [DOI] [PubMed] [Google Scholar]
- 68.Skyler JS, Krischer JP, Wolfsdorf J, Cowie C, Palmer JP, Greenbaum C, Cuthbertson D, Rafkin-Mervis LE, Chase HP, Leschek E. Effects of oral insulin in relatives of patients with type 1 diabetes: The Diabetes Prevention Trial--Type 1. Diab care. 2005;28:1068–1076. doi: 10.2337/diacare.28.5.1068. [DOI] [PubMed] [Google Scholar]
- 69.Harrison LC, Honeyman MC, Steele CE, Stone NL, Sarugeri E, Bonifacio E, Couper JJ, Colman PG. Pancreatic beta-cell function and immune responses to insulin after administration of intranasal insulin to humans at risk for type 1 diabetes. Diab care. 2004;27:2348–2355. doi: 10.2337/diacare.27.10.2348. [DOI] [PubMed] [Google Scholar]
- 70.Uchigata Y, Kuwata S, Tsushima T, Tokunaga K, Miyamoto M, Tsuchikawa K, Hirata Y, Juji T, Omori Y. Patients with Graves’ disease who developed insulin autoimmune syndrome (Hirata disease) possess HLA-Bw62/Cw4/DR4 carrying DRB1*0406. J Clin Endocrinol Metab. 1993;77:249–254. doi: 10.1210/jcem.77.1.8325948. [DOI] [PubMed] [Google Scholar]
- 71.Uchigata Y, Tokunaga K, Nepom G, Bannai M, Kuwata S, Dozio N, Benson EA, Ronningen KS, Spinas GA, Tadokoro K. Differential immunogenetic determinants of polyclonal insulin autoimmune syndrome (Hirata’s disease) and monoclonal insulin autoimmune syndrome. Diabetes. 1995;44:1227–1232. doi: 10.2337/diab.44.10.1227. [DOI] [PubMed] [Google Scholar]
- 72.Eapen SS, Connor EL, Gern JE. Insulin desensitization with insulin lispro and an insulin pump in a 5-year-old child. Ann Allergy Asthma Immunol. 2000;85:395–397. doi: 10.1016/S1081-1206(10)62554-9. [DOI] [PubMed] [Google Scholar]
- 73.Wonders J, Eekhoff EM, Heine R, Bruynzeel DP, Rustemeyer T. [Insulin allergy: background, diagnosis and treatment] Insulineallergie; achtergrond, diagnostiek en behandeling. Ned Tijdschr Geneeskd. 2005;149:2783–2788. [PubMed] [Google Scholar]
- 74.Madero MF, Sastre J, Carnes J, Quirce S, Herrera-Pombo JL. IgG(4)-mediated allergic reaction to glargine insulin. Allergy. 2006;61:1022–1023. doi: 10.1111/j.1398-9995.2006.01117.x. [DOI] [PubMed] [Google Scholar]
- 75.Yokoyama H, Fukumoto S, Koyama H, Emoto M, Kitagawa Y, Nishizawa Y. Insulin allergy; desensitization with crystalline zinc-insulin and steroid tapering. Diabetes Res Clin Pract. 2003;61:161–166. doi: 10.1016/s0168-8227(03)00114-1. [DOI] [PubMed] [Google Scholar]
- 76.Homann D, Eisenbarth GS. An immunologic homunculus for type 1 diabetes. J Clin Invest. 2006;116:1212–1215. doi: 10.1172/JCI28506. [DOI] [PMC free article] [PubMed] [Google Scholar]