Abstract
Background
Racial/ethnic differences in drug injection prevalence contribute to disparities in HIV infection rates in the U.S. between Whites, Blacks and Hispanics. We examine trends in the demographic characteristics of heroin injection drug users (IDUs) that may impact future HIV rates.
Methods
Descriptive analyses were conducted of 1) the national Treatment Episode Data Set for 1992−2004 and of the 2002−2004 baseline data from 2) CIDUS-III, a 5-city study that recruited 3,285 young IDUs, and 3) NIHU-HIT, a Chicago study of 647 young noninjecting heroin users.
Results
Between 1992 and 2004, heroin was the injected drug most often reported at admission to drug treatment. During this period, the proportion of admissions reporting injection declined 44% among Blacks but only 14% for Whites. The peak age for heroin IDUs in treatment increased 10 years for Blacks while declining over 10 years for Whites. CIDUS-III enrolled about 8 times more White (64%) than Black (8%) young IDUs despite recruiting two-thirds of the sample in cities where Blacks constituted 27%−64% of the population. Blacks comprised 53% of noninjecting heroin users in the Chicago NIHU-HIT, but only 2% of Chicago's CIDUS-III sample of heroin IDUs. Among noninjecting heroin users, Whites were more likely than Blacks to have ever injected (X2d.f.=1=17.1, p<0.001). Qualitative data supported greater resistance to injection among young Blacks than Whites.
Conclusions
Among heroin users, young Blacks are resisting injection initiation while young Whites exhibit the opposite tendency. New research should investigate reasons for this trend and its impact on the HIV epidemic and future service needs.
Keywords: injection drug use, heroin, race/ethnicity, age, HIV
1. Background
Racial/ethnic disparities in HIV infection in the United States are greatest in cases attributed to drug injection. In 2005, non-Hispanic (NH) Blacks and Hispanics respectively constituted 55% and 23% of such cases but only 12% and 15% of the US population (CDC, 2006; US Census Bureau, 2005). A recent study of 94 US metropolitan areas found that the elevated AIDS case rates for NH-Blacks compared to NH-Whites were correlated with higher drug injection rates among NH-Blacks (Cooper, et al., 2005).
Injecting drugs is closely linked to opiate use in the US, and heroin is the illicit substance most often injected (O'Donnell and Jones, 1968; Schoener, et al., 2002). Demographic characteristics of opiate users have varied historically, with middle-class White women having the highest rates at the turn of the last Century, followed by working-class urban White men in the 1920s (Brecher, 1972; Dai, 1970; Courtwright, 1982; Terry and Pellens, 1970; Pescor, 1938). By the 1940s heroin was commonly injected (O'Donnell and Jones, 1968), and shortly after World War II the U.S. experienced its first 20th century heroin epidemic (Hughes, et al., 1972), with the greatest increases in use occurring among urban Blacks and Puerto Ricans in Northeastern and Midwestern cites, and Mexicans who had immigrated to the Southwest (Ball and Chambers, 1970; Johnson, et al., 1990; Ball and Cottrell, 1965). A second epidemic in the late 1960s and 1970s was widespread but most pronounced among urban Blacks (Gfroerer and Brodsky, 1992; Agar and Reisinger, 2002; Rittenhouse, 1977; Boyle and Brunswick, 1980; Hunt and Chambers, 1976; O'Donnell, et al., 1976; Clayton and Voss, 1981; DuPont and Greene, 1973), and this cohort has been called the ”heroin injection generation” (Johnson and Golub, 2002; Golub and Johnson, 1999). During the 1980s and early 1990s a large population of heroin injectors was present but initiation rates were modest (Johnson and Golub, 2002; Hughes and Rieche, 1995). The presence of a large cohort of injection drug users (IDUs) contributed significantly to the rapid spread of HIV in the 1980s (Kinlock, et al., 1998; CDC, 2006).
Heroin use expanded again in the 1990s following increased availability of low-cost, higher-purity heroin capable of producing strong psychoactive effects through intranasal snorting (Hughes and Rieche, 1995; Chitwood, et al., 1998; Community Epidemiology Work Group, 1999). Heroin initiation occurred across racial/ethnic groups but, compared to the heroin injection generation, initiates often were better educated, more affluent, and more likely to be suburban residents (Chitwood, et al., 1998; Ouellet, et al., August 11−13, 1993; Agar and Reisinger, 2000; Spunt, 2003; SAMHSA, 2003). The demographic characteristics of this cohort and the extent to which it initiates injection will shape future HIV trends in the US. To investigate, we examined recent trends in heroin injection.
2. Methods
2.1. Data Sources
To describe patterns in the mode of heroin administration among different demographic groups between 1992 and 2004, we analyzed 3 data sources. The public Treatment Episode Data Set (TEDS) collects data from 50 states and Puerto Rico regarding the approximately 1.9 million annual admissions to public and private substance abuse treatment programs that receive state funds (SAMHSA, 2006). TEDS does not include data from facilities operated by the Federal Bureau of Prisons, the Department of Defense, or the Veterans Administration, and is not intended to represent the total national demand for substance abuse treatment. A 1997 analysis estimated that 81% of all known admissions to drug treatment were eligible for the TEDS system, and of those 83% reported data (SAMHSA, 1999). TEDS data available for our analysis were for 1992 through 2004.
In addition to TEDS we examined data from two recent studies of drug users in non-treatment settings. Both studies collected data from 2002 to 2004 and were examined for consistency with trend endpoints in TEDS. The Center for Disease Control and Prevention's (CDC) Third Collaborative Injection Drug Users Study (CIDUS-III) provides survey data on 3,285 young injection drug users in Baltimore, Chicago, Los Angeles, New York City, and Seattle recruited for an HIV prevention intervention trial. Methods are described in detail elsewhere (Garfein, et al., 2007). Briefly, participants were contacted through community outreach, advertising and participant referrals. According to the US Census Bureau, Whites constituted 30% to 68% of the population in the 5 study cities while Blacks constituted 27% to 64% in 3 of the 5 cities (US Census Bureau, 2000). Within cities, recruiting sites typically were in neighborhoods populated mostly by Blacks or Hispanics. Eligible persons were 15−30 years old, injected illicit drugs in the past 6 months, resided in or near the recruitment city and had no plans to leave in the following 12 months, spoke English, and agreed to HIV and hepatitis antibody testing.
The Noninjected Heroin Use, HIV and Injection Transitions Study (NIHU-HIT) enrolled 647 participants in Chicago between 2002 and 2004 for a prospective quantitative and qualitative investigation of transitions to injecting drug use and risks for infection with HIV and hepatitis B and C viruses. Participants were recruited using street outreach and respondent-driven sampling, a method useful in accessing hidden populations (Heckathorn, 1997; Lansky, et al., 2007). Using the same study sites, noninjecting heroin users were recruited concurrently with the Chicago CIDUS-III study of young IDUs, thus minimizing misrepresentations of mode of drug use. Participants were screened for recent injection stigmata (e.g., needle tracks), and heroin use was confirmed using a urine test for opiate metabolites (Biotechnostix, Canada). Eligibility criteria included age 16−30 years, current heroin use (alone or in combination with other drugs), no injection in the past 6 months, and the ability to speak English or Spanish (a detailed description of NIHU-HIT methods is available from the authors upon request).
The University of Illinois Institutional Review Board (IRB) approved the analysis of TEDS data, and the NIHU-HIT and Chicago CIDUS-III studies. CIDUS-III was also approved by IRBs at all other study sites and the CDC. CIDUS-III and NIHU-HIT participants provided written informed consent.
2.2. Quantitative Measures
We examined TEDS data for the US and the 5 primary metropolitan statistical areas (PMSAs) represented in CIDUS-III. Public TEDS files include information on demographics, substances used, and routes of drug administration. The IDU variable includes both intravenous and intramuscular injection. TEDS categorizes and recodes potential identifiers, thus all variables for the current analysis are categorical. Race and ethnicity variables were combined by the authors to create a composite variable with 4 categories: NH-Black, NH-White, Hispanic, and other. We excluded cases missing race/ethnicity information (mean proportion missing 5.6%, annual range 0.6%−7.2%).
Baseline surveys in CIDUS-III and NIHU-HIT were administered using audio computer-assisted self-interviewing (A-CASI) technology and asked participants to report race/ethnicity, age, and any history of injection.
2.3. Statistical Analysis
Descriptive analyses of proportions were used to characterize admissions reported in TEDS from 1992 through 2004. All years were examined to assess consistency in trend, though for clarity the final analysis compares 1992 and 2004. Associations of demographic and drug use characteristics with the year of admission were examined using conventional statistical tests of significance for categorical variables. However, the large size of the TEDS data series rendered virtually all differences significant. Given the size and coverage of TEDS – evidence suggests it captures two-thirds of the treatment population and over 80% of participants in the programs it targets – it is reasonable to assume that statistical significance testing becomes relatively uninformative for the purposes of this analysis (Berk, et al., 1995, Kieffer and Thompson B, 1999). Although results of statistical significance testing are reported in our tables, we primarily used descriptive methods to guide our inferences and assessed differences for their potential impact on public health, particularly regarding HIV/AIDS.
Associations between measures in the baseline CIDUS-III and NIHU-HIT data sets were examined using Pearson chi-square tests for categorical variables and t-tests for continuous measures. To maximize compatibility between our 3 data sets, we examined the subset of CIDUS-III participants who reported heroin by itself as their primary injected drug. Those who primarily injected heroin in combination with another drug were not included. No substantial differences existed in age and race/ethnicity between the subset and full sample.
TEDS and NIHU-HIT data were analyzed using SPSS 14.0 (SPSS Inc., Chicago, IL), and CIDUS-III data with SAS 9.1 (SAS Institute Inc., Cary, NC).
2.4. Qualitative Analysis
NIHU-HIT also collected qualitative data from 121 participants who were selected using criterion-based identification (e.g., injection initiators), stratified random sampling, and theoretical sampling, which selects participants believed to be knowledgeable about specific issues that are of research interest (Patton, 1990). Participants were interviewed individually in private offices by experienced staff (most interviews were conducted by the authors) using an open-ended, semi-structured interview guide to increase reliability and comparability. Interviews were audiotaped, transcribed, entered into HyperResearch 2.7 (ResearchWare Inc., Randolph, MA), and coded to identify all references to racial/ethnic dimensions of initiating drug injection. Most references to demographic differences between injecting and noninjecting heroin users resulted from asking participants to describe the heroin-use scenes in areas with which they were familiar and any changes they may have observed in those scenes. For this analysis, the coded data were searched to identify all participant statements that addressed racial/ethnic dimensions of injection initiation or avoidance.
3. Results
3.1. TEDS Data: 1992−2004
Race/ethnicity, gender, and referral sources at admission to publicly-funded drug treatment programs were largely stable between 1992 and 2004, but the proportion of admissions age 40 years and older increased from 21.6% to 34.6% (data not shown). The largest changes in primary substance of abuse were for marijuana/hashish (from 6.1% to 15.9%) and methamphetamine (from 1.0% to 7.0%). The prevalence of drug injection among all admissions remained nearly constant from 1992 to 2004 (range 13.1%−14.0%). However, the racial/ethnic characteristics of IDUs changed, with declines among NH-Blacks (11.0% to 6.6%) and Hispanics (27.0% to 17.3%), and an increase among NH-Whites (12.4% to 14.8%).
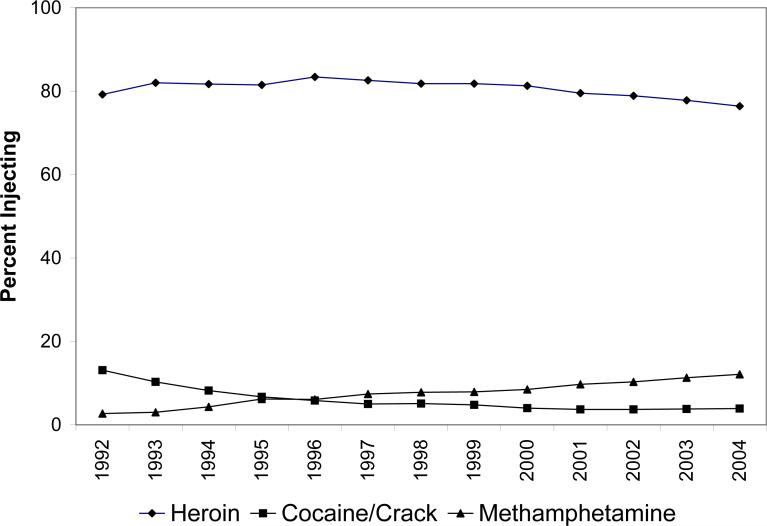
Heroin was the primary injected drug in both 1992 and 2004 (79.2% and 76.4%, respectively) and for all years during that period (Figure 1). Admissions for primary cocaine injection decreased from 13.1% to 3.9%, while methamphetamine admissions increased from 2.7% to 12.1%. Compared to 1992, NH-White IDU admissions were less likely in 2004 to inject heroin (73.2% vs. 69.3%) and cocaine (14.3% vs. 4.2%), but more likely to inject methamphetamine (4.5% vs. 16.0%). NH-Black IDU admissions also injected cocaine less often in 2004, but more often reported heroin (77.6% vs. 91.9%) rather than another stimulant. In both periods, approximately 93% of Hispanic IDUs primarily injected heroin.
Figure 1.
Top 3 Most Frequently Injected Primary Substances Among Admissions to Publicly Funded Treatment Programs in the United States: Treatment Episodes Data Set, 1992 through 2004.
Because heroin users constitute the largest number of injection admissions, we examined TEDS for trends in heroin use. The proportion of admissions citing heroin as their primary drug increased from 11.3% in 1992 to 14.3% in 2004. Table 1 describes selected demographic and drug use characteristics for primary heroin admissions during this period. NH-Whites increased as a proportion of such admissions, from 43.0% to 49.0%, while NH-Blacks and Hispanics decreased. Self-referral was the primary source of treatment entry in both periods, though less so in 2004. Previous treatment episodes were common and declined over time, though the large proportions of missing cases in 2004 warrant caution. Planned methadone treatment at the time of admission decreased from 57.2% to 30.0% during this period and the trend was similar for all racial/ethnic groups. Age distributions changed sharply, however, with a decline of 36% in the 30−39 year old age group and increases of 49% for those aged 40 years and older, and 18% for those 29 years and younger. Notably, by 2004 there was an 84% increase in NH-Whites age 29 years and younger, and a 78% increase in NH-Blacks 40 years and older.
Table 1.
Demographic, Treatment Referral and Drug Use Characteristics by Race/Ethnicity of Primary Heroin Admissions to Publicly Funded Treatment Programs: Treatment Episodes Data Set, 1992 and 2004.
| Variable |
Total |
Non-Hispanic White |
Non-Hispanic Black |
Hispanic |
||||
|---|---|---|---|---|---|---|---|---|
| |
1992 n=163,099 %* |
2004 n=254,535 % |
1992 n=70,193 % |
2004 n=124,638 % |
1992 n=41,700 % |
2004 n=61,287 % |
1992 n=47,039 % |
2004 n=62,075 % |
| Race/Ethnicity | ||||||||
| Non-Hispanic White | 43.0** | 49.0 | -- | -- | -- | -- | -- | -- |
| Non-Hispanic Black | 25.6 | 24.1 | -- | -- | -- | -- | -- | -- |
| Hispanic | 28.8 | 24.4 | -- | -- | -- | -- | -- | -- |
| Other |
2.6 |
2.6 |
-- |
-- |
-- |
-- |
-- |
-- |
| Sex | ||||||||
| Male | 65.6 | 68.1 | 62.4 | 64.0 | 64.0 | 64.7 | 71.6 | 80.0 |
| Female | 34.3 | 31.8 | 37.5 | 36.0 | 35.9 | 35.2 | 28.4 | 20.0 |
| Missing |
0.1 |
<0.1 |
0.1 |
<0.1 |
0.1 |
<0.1 |
<0.1 |
<0.1 |
| Age | ||||||||
| ≤20 | 2.2 | 4.8 | 2.0 | 8.2 | 2.3 | 0.4 | 2.5 | 2.3 |
| 21−29 | 23.3 | 25.2 | 22.5 | 36.9 | 18.2 | 5.8 | 28.7 | 20.7 |
| 30−39 | 47.3 | 30.1 | 50.4 | 25.9 | 43.9 | 31.7 | 45.7 | 36.8 |
| 40−49 | 22.4 | 28.8 | 21.9 | 21.3 | 28.4 | 42.5 | 17.9 | 30.4 |
| ≥50 | 4.4 | 11.0 | 2.9 | 7.5 | 6.4 | 19.5 | 4.8 | 9.5 |
| Missing |
0.4 |
0.2 |
0.3 |
0.2 |
0.7 |
0.2 |
0.3 |
0.3 |
| Age at First Use | ||||||||
| ≤20 | 56.6 | 45.6 | 55.1 | 46.1 | 57.7 | 46.5 | 57.9 | 44.8 |
| 21−29 | 30.8 | 25.7 | 30.8 | 26.4 | 30.4 | 28.1 | 31.0 | 22.8 |
| 30−39 | 9.4 | 11.6 | 10.7 | 11.8 | 8.5 | 14.3 | 8.3 | 8.9 |
| 40−49 | 1.3 | 2.9 | 1.5 | 3.1 | 1.2 | 3.7 | 1.2 | 1.9 |
| ≥50 | 0.2 | 0.4 | 0.2 | 0.3 | 0.2 | 0.5 | 0.2 | 0.3 |
| Missing |
1.7 |
13.7 |
1.7 |
12.3 |
2.0 |
7.0 |
1.3 |
21.2 |
| Source of Referral | ||||||||
| Self | 67.3 | 56.5 | 71.0 | 58.6 | 58.3 | 50.4 | 69.1 | 58.0 |
| Alcohol/Drug Care Provider | 12.3 | 15.6 | 11.4 | 15.6 | 15.4 | 15.2 | 11.3 | 16.4 |
| Other Health Provider | 4.2 | 4.8 | 3.9 | 5.3 | 6.1 | 5.2 | 3.1 | 3.5 |
| School | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | <0.1 | 0.1 | 0.1 |
| Employer | 0.6 | 0.3 | 0.5 | 0.2 | 1.1 | 0.3 | 0.4 | 0.3 |
| Community | 3.2 | 5.7 | 3.1 | 5.3 | 3.5 | 7.4 | 2.9 | 5.1 |
| Court/Criminal | 10.2 | 14.4 | 7.8 | 12.4 | 13.2 | 19.2 | 11.4 | 13.3 |
| Missing |
2.1 |
2.7 |
2.2 |
2.5 |
2.2 |
2.2 |
1.7 |
3.3 |
| Previous Treatment Episodes | ||||||||
| Yes | 68.4 | 61.0 | 72.3 | 62.3 | 61.5 | 61.9 | 68.3 | 57.9 |
| No | 21.9 | 17.8 | 17.1 | 17.5 | 29.3 | 23.3 | 22.8 | 13.2 |
| Missing |
9.7 |
21.2 |
10.6 |
20.3 |
9.2 |
14.8 |
8.9 |
29.0 |
| Planed use of Methadone | ||||||||
| Yes | 57.2 | 30.0 | 56.6 | 27.8 | 48.1 | 27.7 | 65.4 | 36.1 |
| No | 41.3 | 66.8 | 41.0 | 67.8 | 50.7 | 69.5 | 34.2 | 63.0 |
| Missing |
1.5 |
3.2 |
2.4 |
4.4 |
1.2 |
2.8 |
0.3 |
1.0 |
| Usual Route of Use | ||||||||
| Oral | 1.2 | 1.6 | 1.6 | 1.7 | 1.1 | 1.3 | 0.7 | 1.8 |
| Smoking | 1.4 | 2.2 | 1.6 | 2.2 | 1.7 | 2.0 | 0.8 | 2.1 |
| Inhalation | 18.8 | 30.6 | 9.5 | 17.4 | 33.6 | 60.2 | 20.3 | 29.1 |
| Injection | 73.5 | 58.0 | 82.0 | 70.9 | 58.5 | 32.6 | 73.6 | 55.9 |
| Other | 0.6 | 0.7 | 0.5 | 0.8 | 1.1 | 0.7 | 0.4 | 0.5 |
| Missing |
4.4 |
6.9 |
4.8 |
6.9 |
4.0 |
3.1 |
4.3 |
10.6 |
| Daily Use | ||||||||
| Yes | 79.0 | 71.8 | 78.0 | 70.3 | 75.1 | 74.4 | 83.3 | 72.0 |
| No | 16.1 | 21.0 | 16.4 | 22.5 | 20.1 | 21.8 | 12.3 | 17.2 |
| Missing | 5.0 | 7.2 | 5.6 | 7.1 | 4.8 | 3.8 | 4.4 | 10.8 |
Percentages may not sum to 100 due to rounding.
Partially influenced by the large size of the TEDS dataset, all comparisons of interest between 1992 and 2004 are statistically significant at <0.0001, except for sex comparison among NH-Blacks (p=0.023).
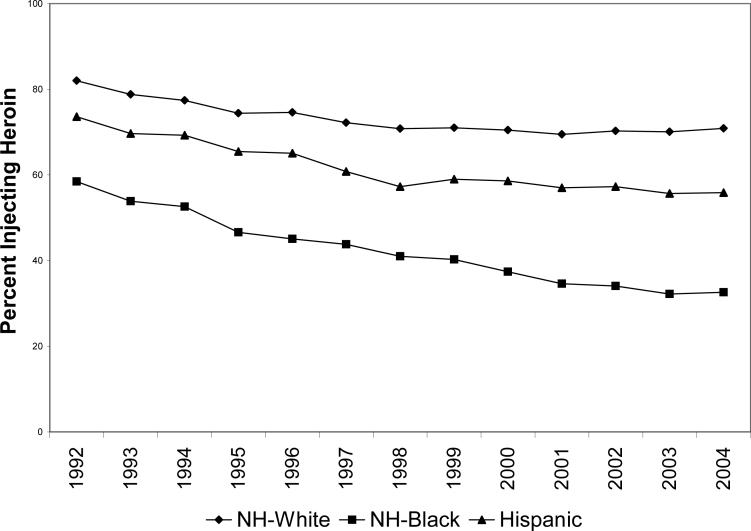
The primary route of heroin administration also changed sharply between 1992 and 2004, with inhalation increasing 63% and injection falling 21%. Injection declined more among NH-Blacks (44%) than among NH-Whites (14%) and Hispanics (24%), a trend that was consistent throughout this period (Figure 2). Of note, the proportion of heroin IDU admissions 29 years and younger decreased for NH-Blacks (8.0% vs. 6.4%) and Hispanics (29.3 vs. 27.4%) but increased substantially for NH-Whites (21.7% vs. 45.0%).
Figure 2.
Racial/Ethnic Distribution of Injection Among Primary Heroin Admissions to Publicly Funded Treatment Programs in the United States: Treatment Episodes Data Set, 1992 and 2004.
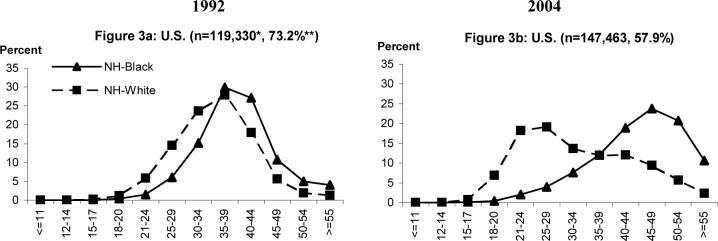
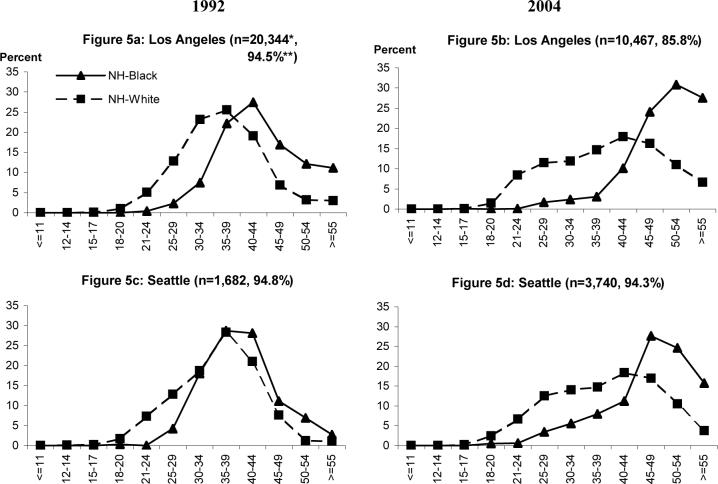
We examined age trends among primary heroin IDU admissions for the US (Figure 3), and the 5 PMSAs represented in CIDUS-III (Figures 4 and 5) (data for Hispanics not shown). Age distributions for the US were similar in 1992 for NH-Black and NH-White primary heroin IDU admissions, peaking at about 35−39 years (Figure 3a). By 2004, NH-Black IDUs were older (peak 45−49 years), while NH-White IDUs were younger (peak 21−29 years) (Figure 3b). Hispanics peaked at age 30−34 years in 1992 and 35−39 years in 2004.
Figure 3.
Age Distribution of Primary Heroin Injecting Admissions to Publicly Funded Treatment Programs in the United States: Treatment Episodes Data Set, 1992 and 2004. *Samples exclude cases missing information on age. Proportion missing <0.5%. ** Percentage injecting of total heroin admissions.
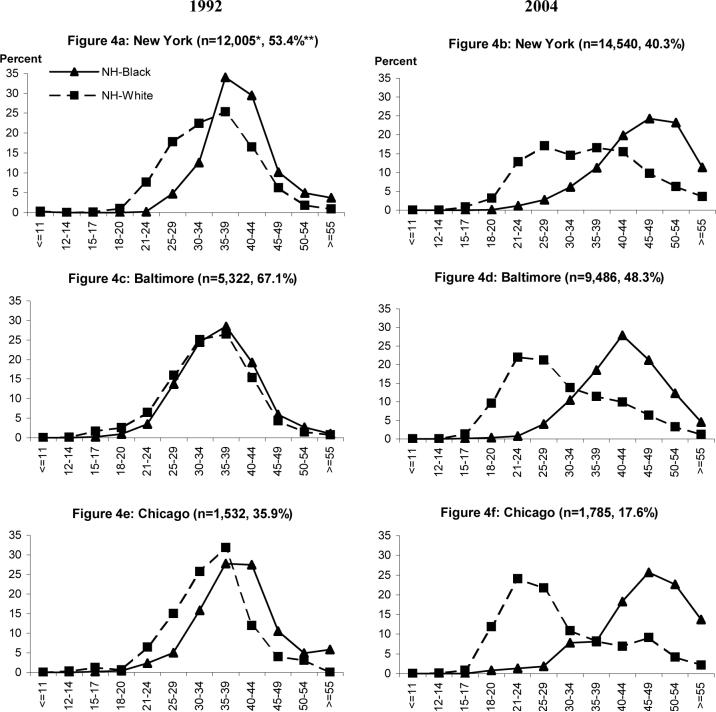
Figure 4.
Age Distribution of Primary Heroin Injecting Admissions to Publicly Funded Treatment Programs in Selected East Coast and Midwest Primary Metropolitan Statistical Areas: Treatment Episodes Data Set, 1992 and 2004. *Samples exclude cases missing information on age. Proportion missing <0.5%. ** Percentage injecting of total heroin admissions.
Figure 5.
Age Distribution of Primary Heroin Injecting Admissions to Publicly Funded Treatment Programs in Selected West Coast Primary Metropolitan Statistical Areas: Treatment Episodes Data Set, 1992 and 2004. *Samples exclude cases missing information on age. Proportion missing <0.5%. ** Percentage injecting of total heroin admissions.
The East Coast and Midwestern PMSAs experienced sizeable declines in injection among heroin admissions during this period: New York, from 53.4% to 40.3%, Baltimore, from 67.1% to 48.3%, and Chicago, from 35.9% to 17.6% (Figures 4a, 4b for New York, 4c, 4d for Baltimore, and 4e, 4f for Chicago). While NH-Blacks declined markedly as a proportion of heroin IDU admissions in these PMSAs (26.2% to 14.4%, 72.3% to 42.4%, and 65.9% to 34.7% respectively), NH-Whites increased in Baltimore (27.1% to 55.1%) and Chicago (from 21.3% to 47.8%), and Hispanics increased in New York (40.2% to 49.8%). The peak age group in 1992 of heroin injectors was 35−39 for both NH-Black and NH-White admissions in these 3 PMSAs. In 2004, peak age of NH-Blacks was 10 years greater in New York and Chicago, and 5 years greater in Baltimore. In contrast, NH-White IDU admissions were younger in 2004, with peaks of 21−24 years in Baltimore and Chicago, and 25−29 years in New York (with a near-peak of 35−39 years). The age distributions of Hispanics in New York, Baltimore, and Chicago generally flattened between 1992 and 2004, with increases in both younger and older age groups.
Injection was far more common among heroin admissions in the West Coast PMSAs for both time periods: Los Angeles, 94.5% and 85.8% (Figures 5a, 5b) and Seattle, 94.8% and 94.3% (Figures 5c, 5d). In 1992 the peak age of heroin IDU admissions was 35−39 years for all groups in Seattle and NH-Whites in Los Angeles. NH-Black IDUs in Los Angeles were slightly older (40−44 years) and Hispanics slightly younger (30−34 years). By 2004 both PMSAs saw increases of 10 years in the peak age group of NH-Black and Hispanic heroin IDU admissions but only 5 years for NH-Whites. In both West Coast PMSAs, the proportion of NH-White IDUs 18−29 years old was stable.
3.2. CIDUS-III Study: 2002−2004
CIDUS-III data represent a concerted attempt to recruit young IDUs age 15−30 years in 5 geographically diverse cities. Table 2 provides racial/ethnic distributions of CIDUS-III participants and population census data (US Census Bureau, 2000) for the 5 study locations. Though study sites typically were in neighborhoods where NH-Whites were not the majority, the study enrolled 8 times more NH-White than NH-Black young IDUs (64.0% vs.7.7%). In the cities with the largest proportions of Black residents, Baltimore (64%) and Chicago (37%), the proportion of NH-Whites to NH-Blacks remained large: 76.2% vs. 11.7% and 75.0% vs. 2.5%, respectively. Heroin was the drug most often injected for the entire sample (71.7%) and at each site. However, at West Coast sites 26.9% to 35.6% of participants mostly injected methamphetamine/amphetamine, while almost none did so at the other sites.
Table 2.
Racial/Ethnic Characteristics of 15−30 Year Old Drug Injectors in the CIDUS-III Study and Population Census Data From the Study's 5 Recruitment Locations.*
|
Location and Data Source** |
Non-Hispanic Black |
Non-Hispanic White |
Hispanic |
|---|---|---|---|
|
Total CIDUS-III (n=3,285) |
7.7 |
64.0 |
16.8 |
|
Total Primary Heroin Injectors in CIDUS-III (n=2,252) |
5.9 |
70.3 |
14.6 |
| Baltimore | |||
| PMSA, 2000 US Census | 27.4 | 66.3 | 2.0 |
| City, 2000 US Census | 64.3 | 31.0 | 1.7 |
| CIDUS-III Primary Recruitment Site, 2000 US Census | 75.8 | 19.9 | 1.2 |
| Total CIDUS-III (n=977) | 11.7 | 76.2 | 1.8 |
| Heroin Injectors in CIDUS-III (n=692) |
9.9 |
79.8 |
1.6 |
| Chicago | |||
| PMSA 2000 US Census | 18.9 | 58.0 | 17.1 |
| City 2000 US Census | 36.8 | 31.3 | 26.0 |
| CIDUS-III Primary Recruitment Site 2000 US Census@ | 95.3 | 2.0 | 2.2 |
| Total CIDUS-III (n=796) | 2.5 | 75.0 | 17.8 |
| Heroin Injectors in CIDUS-III (n=763) |
2.0 |
76.0 |
17.3 |
| Los Angeles | |||
| PMSA 2000 US Census | 9.8 | 31.1 | 44.6 |
| City 2000 US Census | 11.3 | 29.7 | 46.5 |
| CIDUS-III Primary Recruitment Site 2000 US Census | 7.5 | 41.8 | 38.7 |
| Total CIDUS-III (n=540) | 11.9 | 50.7 | 15.9 |
| Heroin Injectors in CIDUS-III (n=230) |
10.3 |
64.6 |
9.4 |
| New York | |||
| PMSA 2000 US Census | 24.6 | 39.6 | 25.1 |
| City 2000 US Census | 26.6 | 35.0 | 27.0 |
| CIDUS-III Primary Recruitment Site 2000 US Census | 27.6 | 1.4 | 74.7 |
| Total CIDUS-III (n=383) | 5.5 | 17.5 | 70.8 |
| Heroin Injectors in CIDUS-III (n=228) |
6.1 |
23.3 |
62.3 |
| Seattle | |||
| PMSA 2000 US Census | 4.4 | 76.3 | 5.2 |
| City 2000 US Census | 8.4 | 67.9 | 5.3 |
| CIDUS-III Primary Recruitment Site 2000 US Census | 20.0 | 46.2 | 7.2 |
| Total CIDUS-III (n=589) | 5.5 | 70.9 | 5.9 |
| Heroin Injectors in CIDUS-III (n=339) | 3.3 | 73.4 | 6.6 |
CIDUS-III recruitment sites are defined by zip codes for neighborhoods where research field stations were located, Participants were recruited using multiple strategies including community outreach and respondent driven sampling.
2000 Census Data were derived from the US Census Bureau (US Census Bureau, 2000).
In Chicago, the CIDUS-III study was conducted from three different field sites, in neighborhoods where NH-Whites were not the majority. The field site that recruited most study participants is presented in the table.
Table 3 presents selected baseline demographic and drug use characteristics for primary heroin injectors. All cities except New York enrolled far more NH-Whites than NH-Blacks and Hispanics. In addition, NH-Blacks were significantly older than NH-Whites (mean age 26 vs. 23 years, p<0.0001).
Table 3.
Demographic and Drug Use Characteristics of 15−30 Year Old Primary Heroin Injectors in the CIDUS-III Study.
|
Variable |
Total (n=2,252) %* |
Baltimore (n=692) % |
Chicago (n=763) % |
Los Angeles (n=230) % |
New York (n=228) % |
Seattle (n=339) % |
|---|---|---|---|---|---|---|
| Race/Ethnicity | ||||||
| Non-Hispanic White | 70.3 | 79.8 | 76.0 | 64.6 | 23.3 | 73.4 |
| Non-Hispanic Black | 5.9 | 9.9 | 2.0 | 10.3 | 6.1 | 3.3 |
| Hispanic | 14.6 | 1.6 | 17.3 | 9.4 | 62.3 | 6.6 |
| Other/Mixed |
9.2 |
8.7 |
4.7 |
15.7 |
8.3 |
16.7 |
| Sex | ||||||
| Male | 67.5 | 67.2 | 65.8 | 67.4 | 74.1 | 67.3 |
| Female |
32.6 |
32.8 |
34.2 |
32.6 |
25.9 |
32.7 |
| Age | ||||||
| 15−20 | 19.7 | 20.7 | 19.4 | 24.8 | 8.8 | 22.4 |
| 21−25 | 46.2 | 44.4 | 51.4 | 47.4 | 41.2 | 41.0 |
| 26−30 | 34.1 | 35.0 | 29.2 | 27.8 | 50.0 | 36.6 |
| Mean years (s.d.) |
24(3.5) |
24(3.6) |
24(3.4) |
23(3.6) |
25(3.4) |
24(3.7) |
| Age at First Injection | ||||||
| 15−20 | 68.5 | 67.6 | 63.1 | 86.8 | 59.9 | 76.1 |
| 21−25 | 24.8 | 24.7 | 27.9 | 12.8 | 32.6 | 21.2 |
| 26−30 | 6.7 | 7.7 | 9.1 | 0.4 | 7.5 | 2.7 |
| Mean years (s.d.) | 19(3.8) | 19(3.7) | 20(3.7) | 17(3.2) | 20(3.8) | 17.9(3.7) |
Percentages may not sum to 100 due to rounding.
3.3. NIHU-HIT Study: 2002−2004
Of the 647 young noninjecting heroin users in Chicago's NIHU-HIT over half (52.9%) were NH-Black, with the remainder split between Hispanics (23.8%) and NH-Whites (21.0%). Here, too, NH-Blacks were significantly older than NH-Whites (mean age 27 vs. 22 years, p<0.0001). Most (81.3%) participants reported ever feeling addicted to heroin and nearly half used it daily. Daily and less frequent users were similar in race/ethnicity. Compared to NH-Blacks, NH-Whites were more likely to report having ever injected (X2d.f.=1=17.1, p<0.0001).
Racial/ethnic trends in heroin administration were mentioned by 30 of the 121 respondents who completed qualitative interviews. None said NH-Blacks were more likely than NH-Whites and Hispanics to inject. Of the 3 respondents who suggested no differences, all spoke in generalities rather than recounting specific observations, which suggests their comments were not grounded in experience. In contrast, 22 respondents said NH-Whites were more likely than NH-Blacks to inject and 10 said the same about Hispanics (responses were not mutually exclusive). The following comments typified these assessments and were chosen for variation in the race/ethnicity, gender and age of the speakers.
Case 1
NH-Black female, 30: “I'd seen shooting . . . the older generation. [Black] people in my age bracket and younger snorted. . . . A young White person will shoot. . . All my White friends shoot and I don't know why.”
Case 2
NH-Black male, 29: “Most of the [Black] people I see shooting up are like older people that's been shooting like since the '70's. I haven't run across too many younger people that shoot heroin. I might even say that suburban White kids might shoot heroin more than the Black kids.”
Case 3
NH-Black female, 24: “Most Black people don't like needles. So nah, people don't graduate to that. . . . I just never, never, in my 5 years that I've been getting high, I never heard of a Black person using needles.”
Case 4
NH-White male, 24: “I think more Black people snort than White . . . most of the people I know turn to shooting, and most . . . are White . . . a lot of Black people, even older ones, they tend to snort. It seems like they're scared of the risk.”
Case 5
NH-White female, 21: “A lot of the White people my age, they shoot it [heroin]. . . . I think a lot of the Black people, they are kind of afraid of the needle.”
Case 6
Hispanic female, 29: “Not too many people that I know inject it. The people that I did meet were Caucasian, and I don't know where these people [come from], cause I live around a Black neighborhood . . . . But the ones that I do know that inject are . . . . mostly Latin. But I know that's rare, I know that a lot of Latins just snort.”
4. Discussion
This study examined national substance abuse treatment data (TEDS) and two research studies, one of young injection drug users (CIDUS-III) and one of young noninjecting heroin users (NIHU-HIT). A striking finding in our analysis is the substantial decline in young NH-Black heroin injectors entering treatment and enrolling in research studies. As an example of the latter, NH-Blacks were only 12% of Baltimore's CIDUS-III sample despite constituting 64% of the city's population (US Census Bureau, 2000). In comparison, the ALIVE study begun in the late 1980's in Baltimore recruited a sample that was 95% African-American (Vlahov, et al., 1991). More recently, the proportion of Whites in Baltimore's second and third Risk Evaluation and Assessment of Community Health (REACH) studies of 15−30 year old IDUs, increased from 31% in 1997−1999 (Fuller, et al., 2001) to 71% in 2000−2002 (Havens, et al., 2006) using similar recruiting methods. The latter study recruited young noninjecting drug users simultaneously with IDUs, and the non-IDU sample was 78% Black. In Chicago NH-Blacks comprised over half the heroin snorters in NIHU-HIT but only 2% of the IDUs in CIDUS-III, despite both studies recruiting concurrently at the same locations.
Studies conducted elsewhere also support these findings. Some report that Blacks have declined as a proportion of subjects in studies of IDUs (Friedman, et al., 1999; Sherman, et al., 2005; Garfein, et al., 1998) and are less likely to be newer (<7 years) or recently transitioned (≤2 ye ars) injectors (Des Jarlais, et al., 1999; Fuller, et al., 2002). In New York City, Black heroin snorters were less likely to have ever injected or to resume or initiate injecting (Neaigus, et al., 2006; Neaigus, et al., 2001). The 1999−2002 National Health and Nutrition Examination Survey found that among persons 20 to 39 years old, lifetime history of injection was more common in NH-Whites than NH-Blacks, while the reverse was true for those 40 to 59 years old (Armstrong, et al., 2006). An analysis of the 1979−2002 National Household Survey on Drug Abuse found that NH-Blacks had higher lifetime probability of drug injection than NH-Whites in cohorts born before 1955, but lower in cohorts born after 1955 (Armstrong, 2007). These national surveys were limited, however, in their underrepresentation of populations with high rates of injection drug use, including the homeless. As a point of comparison, half of CIDUS-III participants reported recent homelessness (Garfein, et al., 2007) and other studies of young IDUs report equivalent or higher levels (Havens, et al., 2004; Lankenau, et al., 2007; Evans, et al., 2003). Whether young NH-Blacks who currently use heroin intranasally can avoid injection for the rest of their heroin use careers is unknown. The event most likely to alter this trajectory is a decline in the quality of heroin to a level that makes snorting it untenable (Strang et al, 1997; Frank, 2000).
A second key finding is that injection trends for NH-Whites moved in the opposite direction compared to NH-Blacks. Consistent with this finding, researchers in Ohio reported increases in heroin use and injecting among White young adults in middle- and upper middle-class families, often in suburban or rural areas (The Ohio Substance Abuse Monitoring Network, 2006). In South Florida, White noninjecting heroin users transitioned faster to injection than did other racial/ethnic groups (Kelley and Chitwood, 2004) and a study in San Francisco reported that IDUs younger than 30 years were significantly more likely to be White than were older IDUs (Kral, et al., 2000).
Of the 5 PMSAs examined using TEDS, Baltimore and Chicago showed the greatest increases in heroin injection in younger NH-Whites. However, injection was so pervasive in Los Angeles and Seattle that similar increases were impossible. The variation in injection prevalence probably reflects geographic differences in the type of heroin available. Mexican black tar heroin, the dominant form in most Western states, is difficult to use intranasally and is usually injected, while powdered South Asian and South American heroin that is easily snorted dominates the Midwestern and Eastern PMSAs (NDIC, 2006). The smaller proportion of young Whites among heroin-using IDUs in TEDS for West Coast PMSAs may be due in part to methamphetamine having a greater presence in these areas (SAMHSA, 2007). In CIDUS-III, over a quarter of participants at the West Coast sites mostly injected methamphetamine/amphetamine, while almost none did so at the other sites.
While these trends clearly warrant further investigation, several explanations have been advanced regarding declines in heroin injection and use among young African-Americans and increases in young Whites. Some hypothesize that African-American communities have experienced particularly severe consequences from drug injection, including high rates of HIV infection, that motivate members to avoid this practice (Johnson, et al., 1998; Boyle and Brunswick, 1980).
Agar and Reisinger hypothesize that heroin epidemics cluster in groups experiencing “open marginality,” a rapid and negative change in the ability to realize socioeconomic expectations (Agar and Reisinger, 2001). For instance, they suggest that the Civil Rights movement in the 1960s raised African-Americans' expectations beyond actual opportunities for moving into mainstream American life, causing pain and dissatisfaction some treated with heroin. The authors suggest that more recent declines in well-compensated industrial/blue-collar jobs generate gaps between the expectation and actual ability of many young Whites' to achieve a standard of living at least comparable to that of their parents. For young Whites who grew up in neighborhoods where drug injection and HIV were rare or hidden, there appears to be fewer inhibitions about initiating injection. Bourgois and colleagues similarly hypothesized that differences they observed between older African-American and White IDUs in San Francisco, including differences in self-identity and drug use practices, were tied to racial/ethnic variations in how major social structural changes in the 1960s-1970s, including upheavals in urban labor markets, were experienced (Bourgois et al, 2006). It is worth noting that these explanations avoid ascribing risk status to racial and ethnic groups, a practice that implicitly suggests behaviors, such as injection drug use, are mostly a product of a specific racial/ethnic culture (Schiller, 1992).
Our findings have implications for future HIV trends. Infections attributable to sharing contaminated injection equipment should decline markedly among African-Americans, though those who do inject will remain at elevated risk due to the high background prevalence of HIV in African-American communities. While needle sharing is common among young White IDUs (Kral, et al., 2000; Novelli, et al., 2005; Bailey, et al., 2007) and suburban residents (Thorpe, et al., 2001), it often takes place in low HIV prevalence settings that produce few infections (Garfein, et al., 2007). To better understand the potential for future infection, research is needed that examines how risk networks of young IDUs evolve over time to see if changes in membership, resources, means of support and other attributes cause a drift toward new network configurations marked by higher HIV prevalence.
Our findings also have implications for other injection-related viral infections. For example, the prevalence of hepatitis C virus (HCV) infection, including the difficult-to-treat genotype 1, is greater among African-Americans than Whites (Armstrong, et al., 2006; Nainan, et al., 2006; Conjeevaram, et al., 2006; Layden-Almer, et al., 2003). Absent a vaccine, new HCV infections should decline among African-Americans and may increase among Whites. In the near term, an aging cohort that initiated injection in the 1970s will increasingly seek care for conditions related to chronic HCV infection.
These findings also suggest an avenue of research regarding needle exchange programs (NEPs). Given consistent evidence of the effectiveness of NEPs in discouraging needle sharing (GAO, 1993; Lurie, et al., 1993; Wodak and Cooney, 2005; National Academy of Sciences, 2006; Gibson et al 2001), opposition to NEPs now largely centers on the contention that these programs enable and signal approval of injection. Reviews of research have found no evidence to indicate NEPs contribute to the initiation of drug injection (GAO, 1993; Lurie, et al., 1993; Wodak and Cooney, 2005; National Academy of Sciences, 2006), but the 1995 review by the National Research Council and Institute of Medicine suggested revisiting these findings to see if they held up over the next decade (Normand, et al., 1995). Since that report, NEPs became commonplace. Because it is likely that NH-Blacks were exposed more often to NEPs than were other groups, due to a greater likelihood of living in neighborhoods with relatively high levels of drug injection and HIV infection, future research should assess the relationship between NEPs and the large decline in drug injection among NH-Blacks reported in this and other studies.
Our study has several limitations. First, routine efforts to improve TEDS may account for some historical variation in the data. Second, the extent to which TEDS covers admissions data is affected by differences in State systems of licensure, certification, accreditation, and disbursement of public funds and the data set may underrepresent persons receiving treatment in private programs, the Veterans Administration hospitals, and correctional facilities. As a result, selection biases may exist that influence the racial/ethnic composition of TEDS data. However, assuming that such biases are relatively stable across time, our analyses of trends should not be affected substantially. Further, veterans and criminal justice referrals are present in TEDS, constituting 2% and 10% of all TEDS admissions in 2004, respectively. Third, TEDS does not represent the prevalence of substance use in the general population. Fourth, TEDS is an admission-based system, and therefore multiple admission records for the same individual in a single year may occur. However, the number of previous episodes reported in our TEDS sample did not differ substantially by race/ethnicity and year. In addition, within a single continuous treatment episode, TEDS is able in many cases to distinguish between an initial admission and subsequent transfers to different service types. Fifth, all 3 data sources relied on self-reports, which are subject to inaccurate recall and socially desirable reporting. However, substance abuse treatment data have been shown to be reliable and consistent (Adair, et al., 1996; Turner and Hubbard, 1995; Adair, et al., 1995), and both CIDUS-III and NIHU-HIT used short recall periods and A-CASI interviews that minimize socially desirable reporting (Ghanem, et al., 2005; Perlis, et al., 2004). Sixth, the representativeness of participants in CIDUS-III and NIHU-HIT is unknown, though both employed multiple methods to recruit a cross-section of participants. Despite these potential limitations, the consistency of the multiple data sources we examined suggests that findings presented here reflect real changes in the racial/ethnic composition of heroin-using IDUs.
It is worth noting that our data have little to say about the risk practices of IDUs, such as injection frequency and the sharing of injection paraphernalia, that are key determinants in assessing IDUs' risk for bloodborne infections, abscesses and other injection-related morbidities. Here we sought only to examine US trends in injection overall. Future research should examine whether and to what extent demographic changes in injection patterns influence individual level risk practices.
In summary, our findings document important changes in the profiles of young heroin injectors likely to shape future trends in HIV and hepatitis C infection and their treatment. Developing a greater understanding of the reasons young NH-Blacks are refraining from injecting and the extent to which NH-Whites constitute a new and growing cohort of heroin IDUs could advance the prevention and treatment of substance abuse and its associated ills.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dita Broz, Division of Epidemiology and Biostatistics University of Illinois at Chicago, School of Public Health 1603 W. Taylor Street (M/C 923) Chicago, IL 60612 USA Tel.: +1 312 355 4753 Fax: +1 312 996 1450 E-mail: dbroz2@uic.edu.
Lawrence J. Ouellet, Division of Epidemiology and Biostatistics University of Illinois at Chicago, School of Public Health 1603 W. Taylor Street (M/C 923) Chicago, IL 60612 USA
References
- Adair EB, Craddock SG, Miller HG, Turner CF. Assessing consistency of responses to questions on cocaine use. Addiction. 1995;90:1497–502. doi: 10.1046/j.1360-0443.1995.901114978.x. [DOI] [PubMed] [Google Scholar]
- Adair EB, Craddock SG, Miller HG, Turner CF. Quality of treatment data. Reliability over time of self-reports given by clients in treatment for substance abuse. J Subst Abuse Treat. 1996;13:145–9. doi: 10.1016/0740-5472(96)00043-8. [DOI] [PubMed] [Google Scholar]
- Agar M, Reisinger HS. A heroin epidemic at the intersection of histories: the 1960s epidemic among African Americans in Baltimore. Med Anthropol. 2002;21:115–56. doi: 10.1080/01459740212904. [DOI] [PubMed] [Google Scholar]
- Agar MH, Reisinger HS. Explaining drug use trends: Suburban heroin use in Baltimore County. In: Springer A, Uhl A, editors. Illicit Drugs: Patterns of Use-Patterns of Response. STUDIENVerlag; Innsbruck: 2000. pp. 143–165. [Google Scholar]
- Agar MH, Reisinger HS. Open marginality: heroin epidemics in different groups. J Drug Issues. 2001;31:729–46. [Google Scholar]
- Armstrong GL. Injection drug users in the United States, 1979−2002: An aging population. Arch Intern Med. 2007;167:166–73. doi: 10.1001/archinte.167.2.166. [DOI] [PubMed] [Google Scholar]
- Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144:705–14. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- Bailey SL, Ouellet LJ, Mackesy-Amiti ME, Golub ET, Hagan H, Hudson S, Latka M, Thiede H, Wei W, Garfein RS. Perceived risk, peer influences, and injection partner type predict receptive syringe sharing among young injection drug users in 5 U.S. cities. Drug Alcohol Depend. 2007;91S:S18–S29. doi: 10.1016/j.drugalcdep.2007.02.014. [DOI] [PubMed] [Google Scholar]
- Ball JC, Chambers CD, Charles C, editors. Thomas; Springfield, IL: 1970. The Epidemiology of Opiate Addiction in the United States. [Google Scholar]
- Ball JC, Cottrell ES. Admissions of narcotic drug addicts to public health service hospitals, 1935−63. Public Health Rep. 1965;80:471–5. [PMC free article] [PubMed] [Google Scholar]
- Berk RA, Western B, Weiss RE. Statistical Inference for Apparent Populations. Sociol Methodol. 1995;25:421–58. [Google Scholar]
- Bourgois P, Martinez A, Kral A, Edlin BR, Schonberg J, Ciccarone D. Reinterpreting ethnic patterns among white and African American men who inject heroin: A social science of medicine approach. PloS Med. 2006;3:e452. doi: 10.1371/journal.pmed.0030452. DOI: 10.1317/journal/pmed.0030452. [DOI] [PMC free article] [PubMed]
- Boyle JM, Brunswick AF. What happened in Harlem? Analysis of a decline in heroin use among a generation unit of urban Black youth. J Drug Issues. 1980;10:109–130. [Google Scholar]
- Brecher EM. Licit and Illicit Drugs. Little, Brown and Company; Boston, MA: 1972. [Google Scholar]
- CDC . HIV/AIDS Surveill Rep. Vol. 17. US Department of Health and Human Services, Centers for Disease Control and Prevention (CDC); Atlanta: 2006. Cases of HIV infection and AIDS in the United States and Dependent Areas, 2005. [Google Scholar]
- CDC Epidemiology of HIV/AIDS--United States, 1981−2006. MMWR Morb Mortal Wkly Rep. 2006;55:589–92. [PubMed] [Google Scholar]
- Chitwood DD, Comerford M, Weatherby NL. The initiation of the use of heroin in the age of crack. In: Inciardi JA, Harrison LD, editors. Heroin in the Age of Crack Cocaine. Sage; Thousand Oaks, CA: 1998. pp. 51–76. [Google Scholar]
- Clayton RR, Voss HL. Young men and drugs in Manhattan: A causal analysis. NIDA Res Monogr. 1981;39:1–187. [PubMed] [Google Scholar]
- Community Epidemiology Work Group . NIH Pub. No. 99−4526. National Institute on Drug Abuse; Rockville, MD: 1999. Epidemiologic Trends in Drug Abuse: Vol 1, Executive Summary, December 1998. [Google Scholar]
- Conjeevaram HS, Fried MW, Jeffers LJ, Terrault NA, Wiley-Lucas TE, Afdhal N, Brown RS, Belle SH, Hoofnagle JH, Kleiner DE, Howell CD. Peginterferon and ribavirin treatment in African American and Caucasian American patients with hepatitis C genotype 1. Gastroenterology. 2006;131:470–7. doi: 10.1053/j.gastro.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Cooper H, Friedman SR, Tempalski B, Friedman R, Keem M. Racial/ethnic disparities in injection drug use in large US metropolitan areas. Ann Epidemiol. 2005;15:326–34. doi: 10.1016/j.annepidem.2004.10.008. [DOI] [PubMed] [Google Scholar]
- Courtwright DT. Dark Paradise: Opiate Addiction in America Before 1940. Harvard University Press; Cambridge, MA: 1982. [Google Scholar]
- Dai B. Opium Addiction in Chicago. Patterson Smith; Montclair, NJ: 1970. [Google Scholar]
- Des Jarlais DC, Friedman SR, Perlis T, Chapman TF, Sotheran JL, Paone D, Monterroso E, Neaigus A. Risk behavior and HIV infection among new drug injectors in the era of AIDS in New York City. J Acquir Immune Defic Syndr Hum Retrovirol. 1999;20:67–72. doi: 10.1097/00042560-199901010-00010. [DOI] [PubMed] [Google Scholar]
- DuPont RL, Greene MH. The dynamics of a heroin addiction epidemic. Science. 1973;181:716–22. doi: 10.1126/science.181.4101.716. [DOI] [PubMed] [Google Scholar]
- Evans JL, Hahn JA, Page-Shafer K, Lum PJ, Stein ES, Davidson PJ, Moss AR. Gender differences in sexual and injection risk behavior among active young injection drug users in San Francisco (the UFO Study). J Urban Health. 2003;80:137–46. doi: 10.1093/jurban/jtg137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank B. An overview of heroin trends in New York City: past, present and future. Mt Sinai J Med. 2000;67:340–6. [PubMed] [Google Scholar]
- Friedman SR, Chapman TF, Perlis TE, Rockwell R, Paone D, Sotheran JL, Des Jarlais DC. Similarities and differences by race/ethnicity in changes of HIV seroprevalence and related behaviors among drug injectors in New York City, 1991−1996. J Acquir Immune Defic Syndr. 1999;22:83–91. doi: 10.1097/00042560-199909010-00011. [DOI] [PubMed] [Google Scholar]
- Fuller CM, Vlahov D, Ompad DC, Shah N, Arria A, Strathdee SA. High-risk behaviors associated with transition from illicit non-injection to injection drug use among adolescent and young adult drug users: a case-control study. Drug Alcohol Depend. 2002;66:189–98. doi: 10.1016/s0376-8716(01)00200-9. [DOI] [PubMed] [Google Scholar]
- Fuller CM, Vlahov D, Arria AM, Ompad DC, Garfein R, Strathdee SA. Factors associated with adolescent initiation of injection drug use. Public Health Rep. 2001;116:136–45. doi: 10.1093/phr/116.S1.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfein RS, Doherty MC, Monterroso ER, Thomas DL, Nelson K, Vlahov D. Prevalence and incidence of hepatitis C infection among young adult injection drug users. J Acquir Immune Defic Syndr. 1998;18(Suppl 1):S11–S19. doi: 10.1097/00042560-199802001-00004. [DOI] [PubMed] [Google Scholar]
- Garfein RS, Golub ET, Greenberg A, Hagan H, Hanson DL, Hudson S, Kapadia F, Kerndt P, Latka M, Ouellet L, Purcell DW, Strathdee SA, Thiede H, Williams IT. A peer-education intervention to reduce injection risk behaviors for HIV and hepatitis C virus infection in young injection drug users. AIDS. 2007;21:1923–32. doi: 10.1097/QAD.0b013e32823f9066. for the DUIT Study Team. [DOI] [PubMed] [Google Scholar]
- Garfein RS, Swartzendruber A, Ouellet LJ, Kapadia F, Hudson SM, Thiede H, Strathdee SA, Williams IT, Bailey SL, Hagan H, Golub ET, Kerndt P, Hanson DL, Latka MH. Methods to recruit and retain a cohort of young-adult injection drug users for the Third Collaborative Injection Drug Users Study/Drug Users Intervention Trial (CIDUS III/DUIT). Drug Alcohol Depend. 2007;91S:S4–S17. doi: 10.1016/j.drugalcdep.2007.05.007. [DOI] [PubMed] [Google Scholar]
- General Accounting Office (GAO) Needle Exchange Programs: Research Suggests a Promising AIDS Strategy. US Government Printing Office; Washington DC: 1993. [Google Scholar]
- Gfroerer J, Brodsky M. The incidence of illicit drug use in the United States, 1962−1989. Br J Addict. 1992;87:1345–51. doi: 10.1111/j.1360-0443.1992.tb02743.x. [DOI] [PubMed] [Google Scholar]
- Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ. Audio computer assisted self interview and face to face interview modes in assessing response bias among STD clinic patients. Sex Transm Infect. 2005;81:421–5. doi: 10.1136/sti.2004.013193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson DR, Flynn NM, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 2001;15:1329–41. doi: 10.1097/00002030-200107270-00002. [DOI] [PubMed] [Google Scholar]
- Golub AL, Johnson BD. Cohort changes in illegal drug use among arrestees in Manhattan: from the Heroin Injection Generation to the Blunts Generation. Subst Use Misuse. 1999;34:1733–63. doi: 10.3109/10826089909039425. [DOI] [PubMed] [Google Scholar]
- Havens JR, Sherman SG, Sapun M, Strathdee SA. Prevalence and correlates of suicidal ideation among young injection vs. noninjection drug users. Subst Use Misuse. 2006;41:245–54. doi: 10.1080/10826080500391811. [DOI] [PubMed] [Google Scholar]
- Havens JR, Strathdee SA, Fuller CM, Ikeda R, Friedman SR, Des Jarlais DC, Morse PS, Bailey S, Kerndt P, Garfein RS. Correlates of attempted suicide among young injection drug users in a multi-site cohort. Drug Alcohol Depend. 2004;75:261–9. doi: 10.1016/j.drugalcdep.2004.03.011. [DOI] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems. 1997;44:174–199. [Google Scholar]
- Hughes PH, Barker NW, Crawford GA, Jaffe JH. The natural history of a heroin epidemic. Am J Public Health. 1972;62:995–1001. doi: 10.2105/ajph.62.7.995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes PH, Rieche O. Heroin epidemics revisited. Epidemiol Rev. 1995;17:66–73. doi: 10.1093/oxfordjournals.epirev.a036186. [DOI] [PubMed] [Google Scholar]
- Hunt LB, Chambers CD. A study of Heroin Use in the United States, 1965−1975. Spectrum Publications, Inc; New York, NY: 1976. The Heroin Epidemics. [Google Scholar]
- Johnson BD, Golub A. Generational trends in heroin use and injection in New York City. In: Musto DF, editor. One Hundred Years of Heroin. Auburn House of Greenwood Publishing Group, Inc.; Westport, CT: 2002. pp. 92–128. [Google Scholar]
- Johnson BD, Thomas G, Golub A. Trends in heroin use among Manhattan arrestees from the heroin and crack eras. In: Inciardi JA, Harrison LD, editors. Heroin in the Age of Crack Cocaine. Sage; Thousand Oaks, CA: 1998. pp. 109–130. [Google Scholar]
- Johnson BD, Williams T, Kojo AD, Sanabria H. Drug abuse in the inner city: impact on hard-drug users and the community. In: Tonry M, Wilson JQ, editors. Drug and Crime (Crime and Justice: A Review of Research, 13) University of Chicago Press; Chicago: 1990. pp. 9–67. [Google Scholar]
- Kelley MS, Chitwood DD. Effects of drug treatment for heroin sniffers: a protective factor against moving to injection? Soc Sci Med. 2004;58:2083–92. doi: 10.1016/j.socscimed.2003.08.006. [DOI] [PubMed] [Google Scholar]
- Kieffer KM, Thompson B. Interpreting statistical significance test results: a proposed new “what if” method; Paper presented at: Annual Meeting of the Mid-South Educational Research Association; Point Clear, AL. Nov 19, 1999. [Google Scholar]
- Kinlock TW, Hanlon TE, Nurco DN. Heroin use in the United States: History and present developments. In: Inciardi JA, Harrison LD, editors. Heroin in the Age of Crack Cocaine. Sage; Thousand Oaks, CA: 1998. pp. 1–30. [Google Scholar]
- Kral AH, Lorvick J, Edlin BR. Sex- and drug-related risk among populations of younger and older injection drug users in adjacent neighborhoods in San Francisco. J Acquir Immune Defic Syndr. 2000;24:162–7. doi: 10.1097/00126334-200006010-00011. [DOI] [PubMed] [Google Scholar]
- Lankenau SE, Sanders B, Bloom JJ, Hathazi D, Alarcon E, Tortu S, Clatts MC. First injection of ketamine among young injection drug users (IDUs) in three U.S. cities. Drug Alcohol Depend. 2007;87:183–93. doi: 10.1016/j.drugalcdep.2006.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansky A, Abdul-Quader AS, Cribbin M, Hall T, Finlayson TJ, Garfein RS, Lin LS, Sullivan PS. Developing an HIV behavioral surveillance system for injecting drug users: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122(Suppl 1):48–55. doi: 10.1177/00333549071220S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layden-Almer JE, Ribeiro RM, Wiley T, Perelson AS, Layden TJ. Viral dynamics and response differences in HCV-infected African American and white patients treated with IFN and ribavirin. Hepatology. 2003;37:1343–50. doi: 10.1053/jhep.2003.50217. [DOI] [PubMed] [Google Scholar]
- Lurie P, Reingold AL, Bowser B, Chen D, Foley J, Guydish J, Kahn JG, Lane S, Sorensen J. The public health impact of needle exchange programs in the United States and abroad. University of California, Berkeley, School of Public Health; The Institute for Health Studies; San Francisco: 1993. [Google Scholar]
- Nainan OV, Alter MJ, Kruszon-Moran D, Gao FX, Xia G, McQuillan G, Margolis HS. Hepatitis C virus genotypes and viral concentrations in participants of a general population survey in the United States. Gastroenterology. 2006;131:478–84. doi: 10.1053/j.gastro.2006.06.007. [DOI] [PubMed] [Google Scholar]
- National Academy of Sciences . Preventing HIV Infection among Injecting Drug Users in High Risk Countries: An Assessment of the Evidence. National Academies Press; Washington, DC: 2006. [DOI] [PubMed] [Google Scholar]
- NDIC . Pub No. 2006-Q0317−003. US Department of Justice, National Drug Intelligence Center (NDIC); Johnstown, PA: 2006. National Drug Threat Assessment 2007. [Google Scholar]
- Neaigus A, Gyarmathy VA, Miller M, Frajzyngier VM, Friedman SR, Des Jarlais DC. Transitions to injecting drug use among noninjecting heroin users: social network influence and individual susceptibility. J Acquir Immune Defic Syndr. 2006;41:493–503. doi: 10.1097/01.qai.0000186391.49205.3b. [DOI] [PubMed] [Google Scholar]
- Neaigus A, Miller M, Friedman SR, Hagen DL, Sifaneck SJ, Ildefonso G, Des Jarlais DC. Potential risk factors for the transition to injecting among noninjecting heroin users: a comparison of former injectors and never injectors. Addiction. 2001;96:847–60. doi: 10.1046/j.1360-0443.2001.9668476.x. [DOI] [PubMed] [Google Scholar]
- Normand J, Vlahov D, Moses LE, editors. Preventing HIV Transmission: The Role of Sterile Needles and Bleach. National Academy Press; Washington, D.C: 1995. [PubMed] [Google Scholar]
- Novelli LA, Sherman SG, Havens JR, Strathdee SA, Sapun M. Circumstances surrounding the first injection experience and their association with future syringe sharing behaviors in young urban injection drug users. Drug Alcohol Depend. 2005;77:303–9. doi: 10.1016/j.drugalcdep.2004.08.021. [DOI] [PubMed] [Google Scholar]
- O'Donnell JA, Jones JP. Diffusion of the intravenous technique among narcotic addicts in the United States. J Health Soc Behav. 1968;9:120–30. [PubMed] [Google Scholar]
- O'Donnell JA, Voss HL, Clayton RR, Slatin GT, Room RG. Young men and drugs-a nationwide survey. NIDA Res Monogr. 1976;i-xiv:1–144. doi: 10.1037/e497472006-001. [DOI] [PubMed] [Google Scholar]
- Ouellet LJ, Jimenez AD, Johnson WA, Wiebel WW. Heroin again: new users of heroin in Chicago; Paper presented at: Annual meeting of the Society for the Study of Social Problems; Miami Beach, FL. Aug 11−13, 1993. [Google Scholar]
- Patton MQ. Qualitative Evaluation and Research Methods. 2nd ed. Sage; Newbury Park, CA: 1990. [Google Scholar]
- Perlis TE, Des Jarlais DC, Friedman SR, Arasteh K, Turner CF. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004;99:885–96. doi: 10.1111/j.1360-0443.2004.00740.x. [DOI] [PubMed] [Google Scholar]
- Pescor MJ. A statistical analysis of the clinical records of hospitalized drug addicts. Public Health Rep. 1938;(SuppNo143):1–30. [Google Scholar]
- Rittenhouse JD. The epidemiology of heroin and other narcotics. NIDA Res Monogr. 1977;16:i–xii, 1−247. [PubMed] [Google Scholar]
- Schiller NG. What's wrong with this picture? The hegemonic construction of culture in AIDS research in the United States. Med Anthropol Q. 1992;6:237–254. [Google Scholar]
- Schoener EP, Hopper JA, Pierre JD. Injection drug use in North America. Infect Dis Clin North Am. 2002;16:535–51. doi: 10.1016/s0891-5520(02)00010-7. [DOI] [PubMed] [Google Scholar]
- Sherman SG, Fuller CM, Shah N, Ompad DV, Vlahov D, Strathdee SA. Correlates of initiation of injection drug use among young drug users in Baltimore, Maryland: The need for early intervention. J Psychoactive Drugs. 2005;37:437–43. doi: 10.1080/02791072.2005.10399817. [DOI] [PubMed] [Google Scholar]
- Spunt B. The current New York City heroin scene. Subst Use Misuse. 2003;38:1539–49. doi: 10.1081/ja-120023397. [DOI] [PubMed] [Google Scholar]
- Strang J, Griffiths P, Gossop M. Heroin in the United Kingdom: different forms, different origins, and the relationship to different routes of administration. Drug Alcohol Rev. 1997;16:329–37. doi: 10.1080/09595239700186711. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Service Administration (SAMHSA) DASIS Series S-7. DHHS Pub No. (SMA)99−3324. SAMHSA, Office of Applied Studies; Rockville, MD: 1999. Treatment Episode Data Set (TEDS): 1992−1997. [Google Scholar]
- Substance Abuse and Mental Health Service Administration (SAMHSA) The DASIS report: New heroin users admitted to treatment: 1992−2000. SAMHSA, Office of Applied Studies; Rockville, MD: 2003. [Google Scholar]
- Substance Abuse and Mental Health Service Administration (SAMHSA) Treatment Episode Data Set (TEDS) SAMHSA, Office of Applied Studies; Rockville, MD.: 2006. [May 2, 2006]. Available at: http://www.oas.samhsa.gov/dasis.htm#teds2. [Google Scholar]
- Substance Abuse and Mental Health Service Administration (SAMHSA) The NSDUH Report: Demographic and geographic variations in injection drug use. SAMHSA, Office of Applied Studies.; Rockville, MD: 2007. [Google Scholar]
- Terry CE, Pellens M. The extent of chronic opiate use in the United States prior to 1921. In: Ball JC, Chambers CD, editors. The Epidemiology of Opiate Addiction in the United States. Charles C. Thomas; Springfield, IL: 1970. pp. 36–67. [Google Scholar]
- The Ohio Substance Abuse Monitoring Network . Young heroin users & treatment experiences in Ohio: A targeted response initiative. Ohio Department of Alcohol and Drug Addiction Services; Columbus, Ohio: 2006. [Google Scholar]
- Thorpe LE, Bailey SL, Huo D, Monterroso ER, Ouellet LJ. Injection-related risk behaviors in young urban and suburban injection drug users in Chicago (1997−1999). J Acquir Immune Defic Syndr. 2001;27:71–8. doi: 10.1097/00126334-200105010-00012. [DOI] [PubMed] [Google Scholar]
- Turner CF, Hubbard RL. Quality of alcohol use histories collected at intake to substance user treatment. Int J Addict. 1995;30:963–89. doi: 10.3109/10826089509055822. [DOI] [PubMed] [Google Scholar]
- US Census Bureau [December 8, 2006];American Community Survey. 2005 Available at: http://factfinder.census.gov.
- US Census Bureau [October 22, 2007];US Census 2000. 2000 Available at: http://www.census.gov/main/www/cen2000.
- Vlahov D, Anthony JC, Muñoz A, Margolick J, Nelson KE, Celentano DD, Solomon L, Polk BF. The ALIVE study: a longitudinal study of HIV-1 infection in intravenous drug users: description of methods. J Drug Issues. 1991;21:759–776. [PubMed] [Google Scholar]
- Wodak A, Cooney A. Effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users. World Health Organization; Geneva: 2005. [Google Scholar]