Abstract
Bioprosthetic valves are used in thousands of heart valve replacement surgeries. Existing glutaraldehyde-crosslinked bioprosthetic valves fail due to either calcification or degeneration. Glutaraldehyde crosslinking does not stabilize valvular glycosaminoglycans (GAGs). GAGs, predominantly present in the medial spongiosa layer of native heart valve cusps, play an important role in regulating physico-mechanical behavior of the native cuspal tissue during dynamic motion. The primary objective of this study was to identify the role of cuspal GAGs in valve tissue buckling. Glutaraldehyde-crosslinked cusps showed extensive buckling compared to fresh, native cusps. Removal of GAGs by treatment with GAG-degrading enzymes led to a marked increase in buckling behavior in glutaraldehyde-crosslinked cusps. We demonstrate that the retention of valvular GAGs by carbodiimide, crosslinking together with chemical attachment of neomycin trisulfate (a hyaluronidase inhibitor), prior to glutaraldehyde crosslinking, reduces the extent of buckling in bioprosthetic heart valves. Furthermore, following exposure to GAG-digestive enzymes, neomycin-trisulfate-bound cusps experienced no alterations in buckling behavior. Such moderate buckling patterns mimicked that of fresh, untreated cusps subjected to similar bending curvatures. Thus, GAG stabilization may subsequently improve the durability of these bioprostheses.
Introduction
Currently, bioprosthetic heart valves are crosslinked with glutaraldehyde to prevent tissue degradation and to reduce tissue antigenicity. Glutaraldehyde forms stable crosslinks with collagen via a Schiff base reaction of the aldehyde with an amine group of the hydroxylysine/lysine in collagen. However, within a decade of implantation, 20–30% of these bioprostheses will become dysfunctional, and over 50% will fail due to degeneration within 12–15 years postoperatively [1, 2].
Glycosaminoglycans, a major constituent of valvular tissue, play an important role in maintaining a hydrated environment necessary for absorbing compressive loads, modulating shear stresses, and resisting tissue buckling in native heart valves. One of the disadvantages of glutaraldehyde crosslinking is its incomplete stabilization of GAGs [3, 4], which lack the amine functionalities necessary for fixation by aldehydes. Previous studies have reported a greater depth of buckling in glutaraldehyde-crosslinked aortic valves as compared to fresh uncrosslinked tissue, which was primarily attributed to collagen crosslinking [5, 6]. Buckling occurs at sites of sharp bending, producing large stresses that can eventually lead to mechanical fatigue and consequent valvular degeneration. Local structural collapse occurs at these areas of tissue buckling to minimize compressive stresses and subsequent reduction in tissue length.
We have reported the loss of GAGs in glutaraldehyde-crosslinked porcine cusps during fixation, storage, in vitro fatigue experimentation, and in vivo subdermal implantation due to enzyme-mediated GAG degradation [3, 4, 7, 8]. Additionally, GAG loss has been observed in failed porcine bioprosthetic heart valves following clinical use [9].
Therefore, to evaluate the potential role of GAGs in cusp buckling in bioprosthetic heart valves, we compared glutaraldehyde crosslinking to 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC) based crosslinking chemistries that link GAG carboxyl groups to the amine groups of proteins. Furthermore, neomycin trisulfate, a hyaluronidase inhibitor, was chemically linked to the cusps to prevent enzymatic degradation of GAGs. Previously, such fixation chemistry was found to resist in vitro and in vivo enzymatic degradation of GAGs [10]. Using these GAG-targeted fixation strategies, we demonstrate that the retention of valvular GAGs reduces the extent of buckling in bioprosthetic heart valves, which may subsequently improve the durability of these bioprostheses.
Materials & Methods
Porcine aortic heart valves were obtained from a local USDA-approved abattoir, Snow Creek Meat Processing, in Seneca, SC. The following materials were purchased from the noted vendors and used in the present studies: ammonium acetate, neomycin trisulfate salt hydrate, glutaraldehyde (50% stock), hyaluronidase (from bovine testes, type IV-s, 3,000–15,000 U/mg), chondroitinase ABC (from Proteus vulgaris, lyophilized powder, 50–250 Umg), D(+)-glucosamine-HCL, collagenase Type VII from Clostridium histolyticum, and 1–9- dimethylmethylene blue (DMMB) were all purchased from Sigma-Aldrich Corporation (St. Louis, MO); 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC) and n-hydroxysuccinimide (NHS) from Pierce Biotech (Rockford, IL); p-dimethyl aminobenzaldehyde, acetyl acetone, and 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) were purchased from Fisher Scientific (Fair Lawn, NJ); and 4-morpholinoethanesulfonic acid hydrate (MES) was obtained from Acros Organics, NJ.
Tissue harvesting and fixation
Fresh porcine aortic heart valves were thoroughly rinsed in ice-cold saline. Within 3 hours of harvesting, intact aortic valves were stuffed with cotton to maintain diastolic morphology and chemically crosslinked in three fixation groups as follows:
Group I
0.6% Glutaraldehyde in 50 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) buffered saline solution at pH 7.4 at ambient temperature for 24 hours, followed by 0.2% Glutaraldehyde in 50 mM HEPES buffered saline solution at pH 7.4 for 6 days at ambient temperature.
Group II
30 mM EDC / 6 mM NHS solution buffered with 50 mM 4-morpholinoethanesulfonic acid hydrate (MES) at a pH of 5.5 for 24 hours at ambient temperature. Following the carbodiimide fixation, valves were thoroughly rinsed in a 50 mM HEPES buffered (pH 7.4) saline solution and subsequently crosslinked with 0.6% glutaraldehyde for 24 hours, followed by storage in 0.2% glutaraldehyde for the remaining 5 days.
Group III
1-hour incubation in 1 mM neomycin trisulfate solution comprised of MES buffer solution at a pH of 7.4. Next, valves were rinsed with deionized water and subsequently fixed with carbodiimide fixation chemistry as outlined above, followed by storage in 0.2% glutaraldehyde.
Group IV
Fresh porcine aortic valves that were not chemically fixed were used as controls to observe buckling in native valve tissue.
Enzymatic degradation of GAGs
Following the above-mentioned respective tissue fixation and storage procedures, cusps were excised from their subtending aortic walls and thoroughly rinsed in 100 mM ammonium acetate buffer (pH 7.4). Whole cusps were incubated in 1.2 ml of 10 U/ml high purity hyaluronidase and 0.2 U/ml high purity chondroitinase ABC buffered in the aforementioned ammonium acetate buffer for 24 hours at 37°C under vigorous shaking at 650 RPM. Fresh cuspal tissue exposed to these enzymatic conditions have shown to completely deplete the valvular tissues of GAGs [3]. Following incubation in enzyme-buffered solutions, samples were thoroughly rinsed in deionized water.
GAG quantification by hexosamine analysis
Previously published methods were employed to quantify total hexosamine content in the respective tissue groups [3]. Briefly, lyophilized cusps were acid hydrolyzed using 2 M hydrochloric acid for 20 hours at 95°C in a vacuum desiccator. After thorough drying under nitrogen gas flow in a boiling water bath, tissue hydrolysates were dissolved in 2 ml of 1 M sodium chloride solution and reacted with 2 ml of 3% acetyl acetone in 1.25 M sodium carbonate. Next, these samples were incubated for 1 hour at 96°C. Following the cooling to room temperature, 4 ml of absolute ethanol and 2 ml of Ehrlich’s reagent (0.18 M p-dimethylaminobenzaldehyde in 50% ethanol containing 3 N HCl) were added to the tube. An incubation period of 45 minutes at room temperature allowed formation of a color product reflective of the hexosamine quantities present in the cuspal tissue. Using the optical absorbance readings at 540 nm of the tissue hydrolysate and D(+)-glucosamine (0 – 200 μg) standards, the hexosamine quantities were determined.
Glycosaminoglycan quantification by dimethylmethylene blue assay
Following enzymatic digestion of GAGs using above-mentioned procedures, GAGs released into the enzyme solutions were quantified by 1–9-dimethylmethylene blue (DMMB) assay using previously described methods [10–13] with minor modifications. In a 96 well-plate, 20 μl of the aforementioned enzyme solution, 30 μl of PBE buffer solution (100 mM Na2HPO4, 5 mM EDTA, pH 7.5), and 200 μl of DMMB reagent solution (40 mM NaCl, 40 mM Glycine, 46 μM DMMB, pH 3.0) were added to each well. Next, optical absorbance readings were read at 525 nm. GAG release in buffer solutions (100 mM ammonium acetate buffer at pH 7.4) were used as controls. Chondroitin sulfate (0 – 1.25 μg) standards were also treated with 20 μl of the above-mentioned enzyme solution. Likewise, chondroitin sulfate (0 – 1.25μg) standards without any exposure to GAG-degrading enzymes were employed to determine GAG release in buffer solution.
Specimen bending preparation
The cusps were excised from the aortic root, and circumferential strips were obtained from the belly region of the cuspal tissue. These 5 mm wide strips (with varied length to fit the desired curvature, see below) were bent to desired curvatures by bending them against natural curvature to mimic physiological bending in the belly region of the cusps [5, 14].
To maintain a bent configuration of the cusps, stainless steel pins were pierced through both ends of the strips; the ends were separated to a desired radius of curvature and held in place by using cork stoppers at either end of the pin for 24 hours in 0.2 % Glut solution.
The radius of curvature was varied by changing the length of the tissue to satisfy the following relationship:
| (1) |
Whereby s denotes the arc length of the curvature, r represents the desired radius of curvature, and θradius is the radian angle of the arc. In this case, a radian angle of π was used to represent a semi-circular arc produced by the bent cuspal strips.
Histological preparation
Routine histological preparations of the paraffin-embedded samples were performed to quantify the extent of buckling. To visualize and identify GAGs, alcian blue staining with Brazilliant!® nuclear fast red (Anatech Ltd., Battle Creek, MI) counterstain was used. Briefly, 5 μm thick paraffin sections were deparaffinized and hydrated with distilled water, mordant in 3% aqueous acetic acid for 3 minutes then stained with 1% alcian blue in 3% acetic acid at pH 2.5 for 30 minutes. After thorough rinsing, sections were counterstained with the above-mentioned nuclear fast red stain (0.1%) for 5 minutes, thoroughly rinsed, and dehydrated for subsequent mounting and coverslipping.
Tissue buckling quantification
Following histological evaluation of the samples, the extent of buckling was quantified using a Zeiss Axioskop 2 plus (Carl Zeiss MicroImaging, Inc., Thornwood, NY) in conjunction with SPOT Advanced software. Using measuring and drafting functions, such as circular and linear dimension line features of the SPOT Advanced software, the actual curvature of the bending, tissue thickness, and depth of buckling were measured. To determine the radius of curvature, a circle was fitted visually to the semi-circular arc of the tissue. The tissue thickness was measured by averaging the local thickness of the tissue away from the sites of tissue buckling. Depth of tissue buckling was quantified by measuring the distance between the deepest point of buckling and the inner boundary of the tissue thickness (Figure 1). The fractional depth of buckling was obtained by dividing buckling depth by the local tissue thickness. Due to variability in tissue thicknesses among cusps, the bending curvature and tissue thickness were expressed as a product. Also, it must be noted that expressing these two independent variables as a product increased the correlation coefficients of the obtained graphical plots.
Figure 1.

Tissue buckling quantification. Depth of tissue buckling was quantified by measuring the distance between the deepest point of buckling and the inner boundary of the tissue thickness. Arc length was determined by fitting a circular function around the bending arc of the tissue.
To normalize the variation in tissue thickness between samples, the curvature was multiplied by the local thickness of tissue. Thus, both variables, curvatures and tissue thickness, affect the degree of buckling depth. Per histological observations, it was evident that as the radius of curvature decreased, or as the curvature of bending increased, the extent of buckling increased. To demonstrate this relationship, fractional depth of buckling versus the product of tissue thickness and curvature of bending were plotted as described previously by Vesely. et al [5, 6].
Additionally, to assess the affect of chemical fixation on the number of buckles produced by valvular tissue bending, the number of buckles present in the semi-circular arc of bent cuspal strips was determined.
Qualitative assessment of buckling using Scanning Electron Microscopy
Following the above-mentioned respective tissue fixation and storage procedures, and specimen bending preparations, samples (with intact pins to maintain curvature) were lyophilized and mounted on aluminum alloy stubs. An ultra-thin coating of gold-palladium was applied using Denton Vacuum Desk II sputter coater. A low vacuum, high resolution environmental scanning electron microscope (JSM 5300 LV ESEM; Joel Ltd, Tokyo, Japan) was used at 5.0 kV to capture images at various magnifications ranging from 35 to 100 X.
Statistical analyses
Results obtained for hexosamine analysis, water content, and rehydration studies are expressed as a mean ± the standard error of the mean (SEM). Statistical analyses for these results were performed using single-factor analysis of variance (ANOVA) whereby significance was defined as p < 0.05. Graphical analysis of valvular tissue buckling behavior was conducted by fitting a linear regression to the data set. Statistical comparisons of the trendlines were performed using two-sample t-test of the predicted values obtained from the regression. Two near-boundary curvatures representing high and low bending radii were selected to evaluate cuspal buckling patterns. Significant differences were defined as p < 0.05.
Results
Resistance of crosslinked cusps to enzymatic degradation of GAGs
The efficacy of various fixation chemistries to prevent enzymatic degradation of GAGs was quantified by treating crosslinked cuspal tissue with GAG-degrading enzymes (namely, hyaluronidase and chondroitinase) and comparing their GAG content to crosslinked cusps not exposed to any GAG-digestive treatments. In addition, GAG content of fresh, untreated, and GAG-digested cusps was evaluated. Following the above-mentioned treatments, Hexosamine analysis indicated the highest loss of GAGs (p<0.05) in glutaraldehyde-crosslinked cusps during crosslinking and storage and further loss after enzymatic digestion (Table I). Cusps crosslinked with EDC/NHS alone showed no statistical difference in their GAG content values as compared to glutaraldehyde-crosslinked cusps (p>0.05). Cusps exposed to GAG-targeted fixation chemistry combined with neomycin trisulfate exhibited the highest stability of GAGs during crosslinking and storage, mimicking fresh, untreated cuspal GAG content (p>0.05). Additionally, these neomycin trisulfate treated cusps showed most resistance to enzymatic removal of GAGs (p<0.05).
Table I.
Efficacy of fixation chemistries to stabilize and maintain GAGs with and without exposure to GAG degrading enzymes: (A) Hexosamine content indicating valvular GAG retention in fresh, untreated and chemically pretreated cusps and; (B) amount of GAGs in enzyme solutions as per DMMB analysis.
| HEXOSAMINE CONTENT OF CUSPAL TISSUE (HEXOSAMINE ASSAY) | ||
|---|---|---|
| Group | μg Hexosamine/10mg Dry Cusp Tissue | ± SEM |
| Fresh; Untreated | 295.64 | 36.89 |
| Fresh; GAG Digested | 98.79 | 7.26 |
| Glut | 182.51 | 7.89 |
| Glut; GAG Digested | 141.30 | 8.19 |
| EDC/NHS | 193.57 | 8.78 |
| EDC/NHS; GAG Digested | 176.73 | 4.65 |
| Neomycin Trisulfate | 242.01 | 14.17 |
| Neomycin Trisulfate; GAG Digested | 239.04 | 8.55 |
| TOTAL GAG CONTENT OF ENZYME SOLUTION (DMMB ASSAY) | ||
| Group | μg Total GAGs/10mg Dry Cusp Tissue | ± SEM |
| Glut | Not Detectable | NA |
| Glut; GAG Digested | 43.34 | 4.41 |
| EDC/NHS | Not Detectable | NA |
| EDC/NHS; GAG Digested | 7.87 | 2.19 |
| Neomycin Trisulfate | Not Detectable | NA |
| Neomycin Trisulfate; GAG Digested | Not Detectable | NA |
To further quantify the loss of GAGs from crosslinked cuspal tissues following GAG-digestive treatments, the respective enzyme solutions of each group were analyzed for released GAGs by DMMB assay (Table I). Significantly higher GAG content (p<0.05) was detected in the enzyme solutions of glutaraldehyde-crosslinked cusps followed by EDC/NHS crosslinked cusps, while an insignificant amount (p<0.05) of GAGs were released into the enzyme solutions of cuspal tissue with bound neomycin trisulfate. These results complemented hexosamine data on the cusp tissue after GAG digestion treatments.
The role of GAGs in valvular tissue buckling
To examine the potential role of GAGs in valvular tissue buckling, fresh untreated, glutaraldehyde-crosslinked, and GAG-stabilized cusps were subjected to varying radii of curvatures. Additionally, to observe buckling in GAG-depleted valvular tissue, these cusps were exposed to GAG-digestive enzymes prior to evaluation of tissue buckling pattern.
Histology results showed that the extent of buckling increased with decreasing radii of bending or with an increase in curvature. Of note, a greater depth of buckling in general was observed in cusps crosslinked with glutaraldehyde, compared to fresh, untreated cusps (Figures 2A and 2B). However, unlike glutaraldehyde-crosslinked cuspal tissue, cusps pretreated with GAG-targeted fixation chemistries exhibited only moderate tissue buckling (Figures 2C and 2D). After GAG digestion, only glutaraldehyde crosslinked cusps showed increased buckling (Figures 2 E–H).
Figure 2.
Histological evaluation of buckling behavior before and after exposure to GAG degrading enzymes in (A, E) fresh, untreated; and (B, F) glutaraldehyde crosslinked; (C, G) carbodiimide crosslinked alone; and (D, H) neomycin trisulfate coupled with carbodiimide fixation treated cusps bent to similar curvatures. Blue staining using Alcian Blue indicates the presence of GAGs.
To demonstrate the differences in buckling depth graphically, the fractional depth of buckling was plotted against the product of bending curvature and tissue thickness. The graphical analyses of buckling behavior suggests that fresh valvular cusps not exposed to any chemical pretreatment experienced relatively mild compressive buckling, with an absence of such tissue deformations at low curvatures. However, glutaraldehyde-crosslinked cusps experienced a greater depth of buckling at all curvatures, including mild bending curvatures (p<0.05) (Figures 3A and 3B). Moreover, when exposed to GAG-digestive enzymes, these glutaraldehyde-crosslinked cusps buckled almost through their entire thickness when tightly bent to high curvatures. Conversely, only slight increase in buckling pattern was observed in untreated, fresh cusps after treatment with GAG-degrading enzymes. Thus, at all bending radii, the fractional depth of buckling in fresh, untreated cusps was significantly lower than in cusps crosslinked with glutaraldehyde with or without GAG-digestion (p<0.05). At high curvatures, cusps treated with carbodiimide fixation chemistry alone buckled to a lower extent than those with glutaraldehyde-fixed cusps (p<0.05) (Figure 3C). Cusps with bound neomycin trisulfate experienced the least degree of buckling at all bending curvatures than their glutaraldehyde-crosslinked counterparts bent to similar configurations (p<0.05) (Figure 3D). Moreover, following GAG-digestion treatment, neomycin trisulfate treated tissues exhibited no significant difference in buckling pattern (p>0.05) (Figure 3D).
Figure 3.
Graphical analyses of fractional depth of buckling of (A) fresh, untreated; and (B) glutaraldehyde crosslinked; (C) carbodiimide crosslinked alone; and (D) neomycin trisulfate coupled with carbodiimide fixation treated cusps subjected to increasing bending curvatures prior to and following treatment with GAG-digestive enzymes. Fractional depth of buckling is plotted against the product of thickness and curvature.
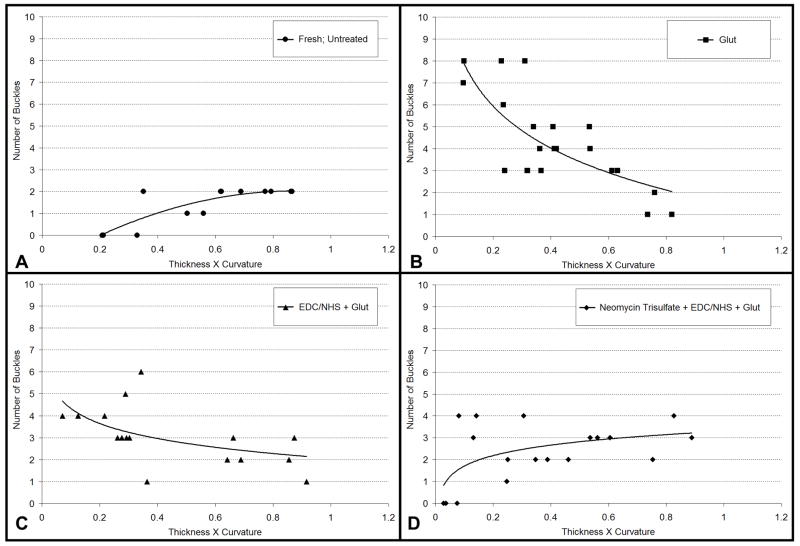
To further characterize the surface buckling pattern of the aforementioned treatment groups, the number of buckles developed during various cuspal bending radii was quantified. Fresh, untreated cusps experienced no buckling at low curvatures (Figure 4A), increasing to minimal numbers of buckles at higher bending curvatures. However, cusps crosslinked with glutaraldehyde fixation produced numerous buckles (approximately 6–7) at low curvatures (Figure 4B).
Figure 4.
Graphical evaluation of change in number of buckles produced by (A) fresh, untreated; and (B) glutaraldehyde crosslinked; (C) carbodiimide crosslinked alone; and (D) neomycin trisulfate coupled with carbodiimide fixation bent to increasing curvatures. Number of buckles is plotted against the product of thickness and curvature.
EDC-crosslinked cusps had lower numbers of buckles than glutaraldehyde-crosslinked cusps at lower curvature (Figure 4C). Neomycin-trisulfate-bound leaflets experienced minimal to no buckling at low curvatures compared to other chemically crosslinked cuspal groups at similar bending curvatures (Figure 4D). The number of buckles is only compared at low curvatures; as, at high curvatures, due to space limitations, the number of buckles is reduced and buckling depth becomes physiologically relevant.
Surface characterization of bent cusps, performed by scanning electron microscopy, was also conducted to compare the surface differences among different groups. As evident in the SEM images, bent glutaraldehyde-crosslinked cusps exhibited a significant amount of deep creases, indicating tissue buckling sites (Figures 5A and 5B), while surface crimps and kinks were minimal in bent cusps with bound neomycin trisulfate at similar bending radii (Figures 5C and 5D).
Figure 5.

Surface characterization of valvular tissue buckling: (A) glutaraldehyde crosslinked cusp and (B) neomycin-trisulfate bound cusp bent to similar curvatures. Images (C) and (D) correspond to the highlighted insets of glutaraldehyde pretreated and neomycin-trisulfate bound cusp bent to similar curvatures, respectively. Arrows indicate areas of valvular tissue buckling.
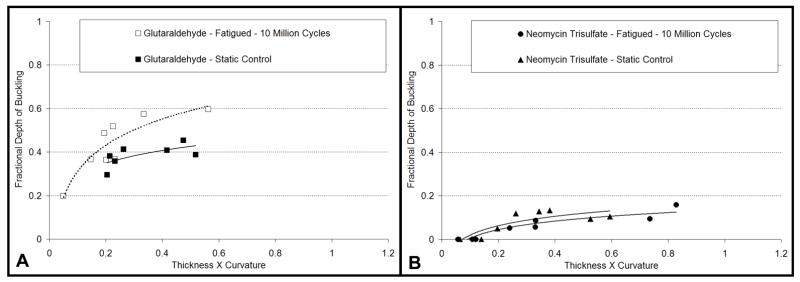
The effect of in vitro cyclic fatigue on valvular tissue buckling behavior following treatment with GAG-targeted fixation chemistry
The efficacy of neomycin trisulfate to resist tissue buckling by stabilizing valvular GAGs was evaluated following in vitro cyclic fatigue. To determine the effect of cyclic fatigue on valvular tissue buckling behavior, glutaraldehyde-crosslinked and neomycin-trisulfate-bound cusps were subjected to various radii of curvatures after undergoing 10 million accelerated fatigue cycles. Alternatively, another set glutaraldehyde-crosslinked and neomycin-trisulfate-bound valves were stored under static conditions to discern the change in tissue buckling pattern, if any, due to cyclical fatigue only.
Upon histological observations, it was apparent that these cuspal tissues exhibited similar buckling patterns as seen previously (Figures 6). Glutaraldehyde-crosslinked cusps, subjected to cyclic fatigue testing, buckled to a greater extent than those stored under static conditions when subjected to similar bending configurations (Figure 6A). However, no substantial difference in buckling behavior was observed between neomycin-trisulfate-bound valvular tissues when subjected to fatigue cycling or when maintained in a static environment (Figure 6B).
Figure 6.
Histological evaluation of buckling behavior in (A) glutaraldehyde crosslinked; and (B) neomycin trisulfate bound cusps bent to similar curvatures following 10 million fatigue cycles. Blue staining using Alcian Blue indicates the presence of GAGs. Bars represent 500 μm.
To quantitatively corroborate the abovementioned observations, graphical analyses of the cuspal groups was performed. In concurrence with the qualitative results, analogous tissue buckling behavior was obtained (Figure 7A and 7B), whereby fatigued neomycin-trisulfate-bound cusps experienced significantly lower fractional buckling depths than glutaraldehyde-crosslinked cusps with or without cyclical fatigue (p<0.05). Also, cusps with bound neomycin trisulfate exhibited no change in buckling behavior between statically stored and cyclical fatigued valves (p>0.05).
Figure 7.
Graphical analyses of fractional depth of buckling (A) glutaraldehyde crosslinked; and (B) neomycin trisulfate bound cusps subjected to increasing bending curvatures prior to and following 10 million fatigue cycles.
Discussion
Valvular tissue buckling has been implicated in the evolution of fatigue failure in the bioprostheses. Characterized by structural deformations, buckling occurs at areas of large stresses during valvular motion. During diastole, xenograft valves are subjected to uniaxial compression due to sharp bending in the belly and commissural regions of the cusps [5, 6, 14]. Such valvular behavior produces surface kinks and crimps, resulting in local structural collapse to reduce the bending stresses. Upon initiation of buckling, such tissue-bending deformations continue to occur in the same area during each successive valvular cycle. Consequentially, the bending site fatigues, which may lead to subsequent tearing of the cusp. By modulating shear stresses, the medial spongiosa layer, rich in GAGs, buffers the appositional movement of the outer layers in native valves, which are subjected to tensile and compressive loads. These hydrophilic GAGs form a gel-like layer capable of absorbing such stresses during valvular bending.
Conventional glutaraldehyde crosslinking of porcine aortic valves does not provide complete stabilization of valvular extracellular matrix [15–18]. Previous work by Vesely et al. has elucidated the role of collagen crosslinking in tissue buckling, but the role of GAGs in such valvular tissue buckling has not been examined. The pronounced depth and amount of buckling observed in glutaraldehyde-crosslinked valvular cusps in the present study is attributed to the combined effects of the stiffness imparted by collagen crosslinking and the loss of GAGs. Due to the relative loss of flexibility, the glutaraldehyde-crosslinked cusps buckle unlike untreated cusps that do not exhibit such abnormal bending behavior. Following GAG-digestive treatment, glutaraldehyde-crosslinked cuspal tissue, depleted of valvular GAGs, experienced a greater degree of valvular tissue buckling, clearly showing the role of GAGs in tissue buckling. We have previously shown that GAG-degrading enzymes, native to the valves, are still active after glutaraldehyde fixation [4]. Thus, these native valve enzymes or enzymes infiltrated from the serum, could access cleavage sites of GAGs and deplete GAGs from the BHVs, making them more vulnerable to buckling.
Stabilization of glycosaminoglycans to reduce valvular tissue buckling
Chemical stabilization of valvular GAGs alone does not prevent enzymatic degradation of these extracellular matrix components [7]. In the present study, carbodiimide fixation alone was shown to only partially inhibit GAG digestion. The carboxylic acid functionalities of GAGs are active sites for enzymatic degradation [19, 20]. Thus, carbodiimide crosslinking might have prevented enzyme binding to some carboxyl groups in GAGs. As all carboxylic acids are not involved in crosslinking, enzymes still could cleave GAGs. This might have lead to the partial loss of GAGs, and thus, these cusps experienced less deeper buckling than those cusps crosslinked with glutaraldehyde. We recently reported the use of neomycin trisulfate, a hyaluronidase inhibitor [21], coupled with carbodiimide-based crosslinking chemistry to effectively stabilize valvular GAGs [10]. Such GAG-targeted fixation chemistry utilizes the presence of amine functionalities present in neomycin trisulfate to chemically bind to carboxylic groups of GAG uronic acids by carbodiimide crosslinking [10]. Valvular cusps with bound neomycin trisulfate completely inhibited enzyme-mediated GAG degradation. Neomycin trisulfate not only blocks active sites on GAGs but also confers GAG-digestive enzymes inactive by binding to GAG-degrading enzymes. Steric hindrance of the active site and conformational change of the enzyme precludes loss and digestion of GAGs. Therefore, the neomycin-trisulfate-bound cusps exhibited the least amount and extent of buckling, mimicking fresh, untreated tissue-buckling behavior. Furthermore, neomycin-trisulfate-bound cuspal tissue experienced no change in buckling behavior after exposure to GAG-digestive enzymes. This was in contrast to glutaraldehyde-treated cusps, which demonstrated the greatest depth of buckling at all curvatures and a significant number of buckles at low curvatures following incubation with GAG-degrading enzymes.
Thus, stabilization of GAGs by neomycin trisulfate, coupled with carbodiimide-fixation chemistry, precludes valvular tissue buckling. The presence of valvular GAGs appropriates the cusp its structural and functional integrity necessary to resist compressive buckling during bending.
Resistance of neomycin trisulfate-enhanced, GAG-targeted crosslinking to valvular tissue buckling following in vitro cyclical fatigue
Stabilization of cuspal GAGs during cyclical motion of the valve will permit improved durability of the valves. During the cardiac cycle, valvular cusps are continuously subjected to tensile, compressive, and shear stresses. The interlayer shearing between the fibrosa and ventricularis is mediated by the medial spongiosa layer. Particularly, GAGs, hydrophilic in nature, form a gel-like layer in the spongiosa capable of distributing and dissipating these valvular stresses. To mimic this, valves were subjected to in vitro cyclic fatigue for 10 million cycles comparable to four months of physiologic use. We have previously shown that substantial amounts of GAGs are depleted by this time [4].
Glutaraldehyde-crosslinked valves exhibited a greater depth of buckling after in vitro cyclic fatigue than compared to those cusps stored under static conditions. Interestingly, current studies demonstrate no difference in buckling behavior in neomycin-trisulfate-bound cuspal tissue after accelerated fatigue testing as compared to buckling patterns of statically stored valves. Additionally, these GAG-stabilized cusps exhibited minimal fractional depth of buckling compared to glutaraldehyde-crosslinked valves which are prone to GAG loss during similar fatigue testing. Moreover, fatigued cusps with bound neomycin trisulfate maintained minimal numbers of surface buckles mimicking fresh, untreated cuspal buckling behavior. Therefore, stabilization of valvular GAGs using neomycin trisulfate coupled with carbodiimide-fixation chemistry improved the buckling behavior of these cusps following short-term cyclical fatigue. Long-term cyclical fatigue and storage studies are underway to study the effectiveness of GAG stabilization on valve durability.
Conclusions
Despite numerous advances in the design of BHVs, the durability of these bioprostheses is limited due to dysfunction and subsequent degeneration. Partly owing to the structural demands imposed by the cardiac system, stabilization of the morphological properties of valvular cusps may ultimately enhance the long-term performance and efficiency of these implants. Glutaraldehyde fails to stabilize GAGs, essential for absorbing compressive loads, modulating shear stresses, and resisting tissue buckling. Present studies demonstrate the efficacy of neomycin trisulfate, a GAG-digestive enzyme inhibitor, coupled with carbodiimide fixation to stabilize valvular GAGs and subsequently resist tissue buckling.
Thus, stabilization and retention of valvular GAGs using GAG-targeted fixation chemistries, coupled with neomycin trisulfate, may in fact reduce the extent of buckling in BHVs and subsequently improve the durability of these bioprostheses.
Acknowledgments
The authors wish to thank Snow Creek Meat Processing, Seneca, SC for supply of porcine aortic valves. We thank Drs. Lawrence Grimes and Jason Isenburg for assistance with statistical analyses of results. We express our thanks to Mrs. Linda Jenkins for histology facility support. This research was supported by NIH grant HL70969.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Everaerts F, Torrianni M, van Luyn M, van Wachem P, Feijen J, Hendriks M. Reduced calcification of bioprostheses, cross-linked via an improved carbodiimide based method. Biomaterials. 2004;25(24):5523–30. doi: 10.1016/j.biomaterials.2003.12.054. [DOI] [PubMed] [Google Scholar]
- 2.Schoen FJ, Levy RJ. Founder’s Award, 25th Annual Meeting of the Society for Biomaterials, perspectives. Providence, RI, April 28-May 2, 1999. Tissue heart valves: current challenges and future research perspectives. J Biomed Mater Res. 1999;47(4):439–65. doi: 10.1002/(sici)1097-4636(19991215)47:4<439::aid-jbm1>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 3.Lovekamp JJ, Simionescu DT, Mercuri JJ, Zubiate B, Sacks MS, Vyavahare NR. Stability and function of glycosaminoglycans in porcine bioprosthetic heart valves. Biomaterials. 2006;27(8):1507–18. doi: 10.1016/j.biomaterials.2005.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vyavahare N, Ogle M, Schoen FJ, Zand R, Gloeckner DC, Sacks M, et al. Mechanisms of bioprosthetic heart valve failure: fatigue causes collagen denaturation and glycosaminoglycan loss. J Biomed Mater Res. 1999;46(1):44–50. doi: 10.1002/(sici)1097-4636(199907)46:1<44::aid-jbm5>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 5.Vesely I, Boughner D, Song T. Tissue buckling as a mechanism of bioprosthetic valve failure. Ann Thorac Surg. 1988;46(3):302–8. doi: 10.1016/s0003-4975(10)65930-9. [DOI] [PubMed] [Google Scholar]
- 6.Vesely I, Mako WJ. Comparison of the compressive buckling of porcine aortic valve cusps and bovine pericardium. J Heart Valve Dis. 1998;7(1):34–9. [PubMed] [Google Scholar]
- 7.Mercuri JJ, Lovekamp JJ, Simionescu DT, Vyavahare NR. Glycosaminoglycan-targeted fixation for improved bioprosthetic heart valve stabilization. Biomaterials. 2007;28(3):496–503. doi: 10.1016/j.biomaterials.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Simionescu DT, Lovekamp JJ, Vyavahare NR. Glycosaminoglycan-degrading enzymes in porcine aortic heart valves: implications for bioprosthetic heart valve degeneration. J Heart Valve Dis. 2003;12(2):217–25. [PubMed] [Google Scholar]
- 9.Grande-Allen KJ, Mako WJ, Calabro A, Shi Y, Ratliff NB, Vesely I. Loss of chondroitin 6-sulfate and hyaluronan from failed porcine bioprosthetic valves. J Biomed Mater Res A. 2003;65(2):251–9. doi: 10.1002/jbm.a.10475. [DOI] [PubMed] [Google Scholar]
- 10.Raghavan D, Simionescu DT, Vyavahare NR. Neomycin prevents enzyme-mediated glycosaminoglycan degradation in bioprosthetic heart valves. Biomaterials. 2007;28(18):2861–8. doi: 10.1016/j.biomaterials.2007.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farndale RW, Buttle DJ, Barrett AJ. Improved quantitation and discrimination of sulphated glycosaminoglycans by use of dimethylmethylene blue. Biochim Biophys Acta. 1986;883(2):173–7. doi: 10.1016/0304-4165(86)90306-5. [DOI] [PubMed] [Google Scholar]
- 12.Farndale RW, Sayers CA, Barrett AJ. A direct spectrophotometric microassay for sulfated glycosaminoglycans in cartilage cultures. Connect Tissue Res. 1982;9(4):247–8. doi: 10.3109/03008208209160269. [DOI] [PubMed] [Google Scholar]
- 13.Hoemann CD, Sun J, Chrzanowski V, Buschmann MD. A multivalent assay to detect glycosaminoglycan, protein, collagen, RNA, and DNA content in milligram samples of cartilage or hydrogel-based repair cartilage. Anal Biochem. 2002;300(1):1–10. doi: 10.1006/abio.2001.5436. [DOI] [PubMed] [Google Scholar]
- 14.Thubrikar MJ, Skinner JR, Eppink RT, Nolan SP. Stress analysis of porcine bioprosthetic heart valves in vivo. J Biomed Mater Res. 1982;16(6):811–26. doi: 10.1002/jbm.820160607. [DOI] [PubMed] [Google Scholar]
- 15.Talman EA, Boughner DR. Internal shear properties of fresh porcine aortic valve cusps: implications for normal valve function. J Heart Valve Dis. 1996;5(2):152–9. [PubMed] [Google Scholar]
- 16.Talman EA, Boughner DR. Glutaraldehyde fixation alters the internal shear properties of porcine aortic heart valve tissue. Ann Thorac Surg. 1995;60(2 Suppl):S369–73. doi: 10.1016/0003-4975(95)00250-o. [DOI] [PubMed] [Google Scholar]
- 17.Sun W, Sacks MS, Sellaro TL, Slaughter WS, Scott MJ. Biaxial mechanical response of bioprosthetic heart valve biomaterials to high in-plane shear. J Biomech Eng. 2003;125(3):372–80. doi: 10.1115/1.1572518. [DOI] [PubMed] [Google Scholar]
- 18.Mirnajafi A, Raymer JM, McClure LR, Sacks MS. The flexural rigidity of the aortic valve leaflet in the commissural region. J Biomech. 2006;39(16):2966–73. doi: 10.1016/j.jbiomech.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 19.Menzel EJ, Farr C. Hyaluronidase and its substrate hyaluronan: biochemistry, biological activities and therapeutic uses. Cancer Lett. 1998;131(1):3–11. doi: 10.1016/s0304-3835(98)00195-5. [DOI] [PubMed] [Google Scholar]
- 20.Zhong SP, Campoccia D, Doherty PJ, Williams RL, Benedetti L, Williams DF. Biodegradation of hyaluronic acid derivatives by hyaluronidase. Biomaterials. 1994;15(5):359–65. doi: 10.1016/0142-9612(94)90248-8. [DOI] [PubMed] [Google Scholar]
- 21.Salmen S, Hoechstetter J, Kasbauer C, Paper DH, Bernhardt G, Buschauer A. Sulphated oligosaccharides as inhibitors of hyaluronidases from bovine testis, bee venom and Streptococcus agalactiae. Planta Med. 2005;71(8):727–32. doi: 10.1055/s-2005-871255. [DOI] [PubMed] [Google Scholar]