Abstract
Soft-tissue management is a critical factor in total knee arthroplasty, especially in valgus knees. The stepwise release has been based upon surgeon’s experience. Computer-assisted surgery has gained increasing scientific interest in recent times and allows the intraoperative measurement of leg axis and gap size in extension and flexion. We therefore aimed to analyse the effect of sequential lateral soft-tissue release and the resulting change in the a.p. limb axis on the one hand and the tibiofemoral gaps on the other hand in extension as well as in flexion in eight cadaveric knees. Measurements were obtained using a CT-free navigation system. In extension the highest increase compared to the previous release step was found for the first (iliotibial band, P = 0.002), second (popliteus muscle, P = 0.0003), third (LCL, 0.007) and the sixth (entire PCL, P = 0.001) release step. In 90° flexion all differences of the lateral release steps were statistically significant (P < 0.004). Massive progression of the lateral gap in flexion was found after the second (popliteus muscle, P = 0.004) and third (LCL, 0.007) release step. Computer-assisted surgery allows measurement of the effect of each release step of the sequential lateral release sequence and helps the surgeon to better assess the result.
Résumé
La libération des tissus mous lors de la réalisation d’une prothèse totale du genou est un facteur important notamment dans les génu valgum. Les techniques de «releases» sont bien connues des chirurgiens. La chirurgie assistée par ordinateur permet de mesurer en peropératoire les axes et les espaces en flexion et en extension. Pour cela nous avons mesuré tous ces paramètres lors d’une expérimentation sur 8 genoux de cadavre, utilisant un système de navigation avec en extension, libération de la bandelette iliotibiale (P = 0.002) puis du muscle poplité (P = 0.003) et enfin, du ligament collatéral (P = 0.007), en sixième position libération du ligament croisé postérieur (P = 0.001). A 90° de flexion toutes les étapes de la libération tissulaire sont importantes. L’étape importante pour redonner de l’espace est atteinte après libération du muscle poplité puis du ligament collatéral. La chirurgie assistée par ordinateur permet de mesurer les effets de chaque étape de cette libération tissulaire et permet donc aux chirurgiens d’améliorer leurs résultats.
Introduction
Total knee replacement (TKR) has become a successful and reliable treatment of primary and secondary osteoarthritis of the knee with a highly satisfactory outcome in more than 80 percent of patients [20]. It is well accepted that postoperative imbalance of collateral ligaments and coronal malalignment may lead to early loosening of a prosthesis [6, 8, 14]. So, the cornerstone of total knee replacement is to achieve a stable, well-aligned knee over the full range of movement with symmetrical extension and flexion gaps. As preoperative bony deformities with resulting ligamentous instability or contractures are well-recognised difficulties in primary TKR, numerous ligament balancing techniques and soft-tissue release sequences have been published [2, 7, 9, 13, 15, 17, 21, 23, 24]. The release techniques for the lateral side for correcting varus deformities are still discussed controversially. Ranawat, for example, performs a three-step lateral release, where the ilitiobial band is pie-crusted, the posterolateral capsule is released and the posterior collateral ligament is sacrificed [17]. In contrast, Kanamiya et al. (2002) and Matsueda et al. (1999) propose a sequential release, where the lateral soft tissues are released according to deformity and the surgeon has the opportunity to deal with different degrees of deformity [7, 13]. But, until recently the effect of these stepwise release techniques has been based upon the surgeon’s experience, because no measuring tool was available.
Over the last 5 years, computer-assisted surgery has been introduced in TKR. These systems provide the possibility to improve the accuracy of component orientation and restoration of the mechanical limb axis [1]. Using the computer-aided technique, highly precise intraoperative angular and tibiofemoral gap measurements have become available with an accuracy of less than 1° or 1 mm [3]. So, navigation in total knee replacement has led to an even more precise implantation technique. One of the most interesting features is the soft-tissue support. As we have shown in earlier studies for the varus deformity, ligament-balancing techniques become easier and predictable [11, 12] with the use of computer-assisted surgery.
The aim of the current cadaver study was to elucidate the relationship between a standardised sequential lateral soft-tissue release and the resulting a.p. leg axis during soft-tissue management and the resulting change of the medial and lateral tibiofemoral gap in extension and flexion. We performed a standardised sequential lateral soft-tissue release modified according to the recommendations of Matsueda et al. [13] and measured the change of coronal leg axis and tibiofemoral gaps navigation controlled in full-body cadaver knees in extension and 90° flexion.
Materials and methods
We used eight formalin-fixed full-body cadavers for our testing, four female and four male cadavers. All knees were without severe deformities (coronal alignment in between ±4° varus-valgus), no specimen had had previous operations on the ipsilateral foot, knee and hip, nor osteoarthritis greater than grade II according to the classification of Outerbridge. The cadavers were kept at room temperature for 4 h before any testing. Inclusion criteria were a full range of movement of the ipsilateral hip and the operated knee.
Navigation system
The navigation system used in this study was the Ci CT-free navigation system (DePuy I-Orthopaedics, Munich, Germany, software version 1.1.2). This system is based on an optical tracking unit, which detects reflecting marker spheres attached to the bone and instruments by an infrared camera system. One of the useful software features of the system used in this study is the ligament balancing modus. This allows measuring of the a.p. limb axis in extension and determining the gaps between the medial and lateral femoral and tibial condyle over the full range of movement.
Surgical technique
The experiment followed our standard operation routine. No soft tissues were removed. After a mid-line skin incision preparation of the capsule was performed. Then a medial parapatellar approach opened the capsule and the anterior cruciate ligament and menisci were resected. Then two Schanz screws were drilled bicortically into the femur and tibia, respectively, to fix the reference array (Fig. 1). The anatomical landmarks of the tibia and femur were defined according to the navigation’s workflow. Then, a first navigation-controlled measurement of the physiological and preoperative a.p. leg alignment with the patella subluxed in extension as well as in 90° flexion was carried out and taken as reference for all of the following measurements. The cutting jig for the tibial cut was then adjusted according to the recommendations of the navigation system (the tibial slope was set to 3° posterior slope) and the cut was performed. After verifying this cut the spreader device (DePuy, Fig. 2) was put into the extension gap and spread with 150 N in extension and 90 N in flexion. The resulting leg axis, the medial and lateral gaps were calculated by the navigation system (Fig. 3). Then the release was performed stepwise and after each release step the measurement was performed as described above. All angular measurements were repeated three times and averaged.
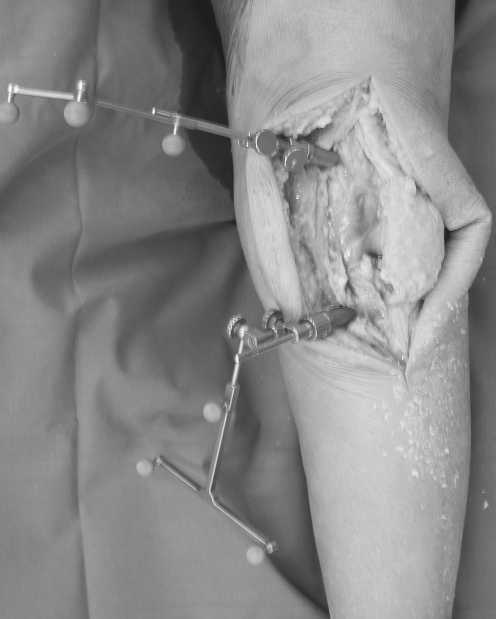
Fig. 1.
Reference arrays of the navigation system are fixed bicortically to the tibia and femur with Schanz´ srews
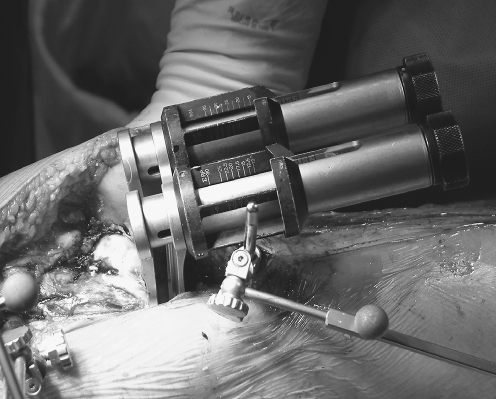
Fig. 2.
The spreader (Depuy) is put into the extension gap and spread with 150 N as recommended by the manufacturer
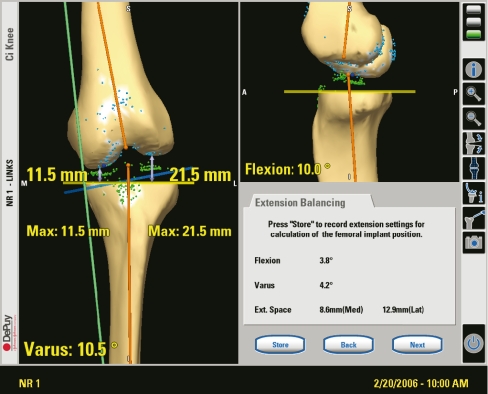
Fig. 3.
Sreenshot of the navigation system within the ligament balancing modus, which provides the leg axis and the width of the medial and lateral gap and the degree of flexion
Sequential lateral soft tissue release
The sequential lateral ligament release technique was carried out according to the recommendation of Matsueda et al. [13], which is currently used in our daily routine. The single steps were carried out using subperiosteal or subligamentous sharp dissection by scalpel or Cobb elevator:
Release of the iliotibial band at the level of the joint line
Release of the femoral attachment of the popliteus muscle
Release of the lateral collateral ligament from the femoral condyle
Release of the posterolateral capsule from the femoral side
Release of the lateral half of the posterior cruciate ligament on the tibial side
Release of the entire posterior cruciate ligament on the tibial side
Each release step was followed by measuring the coronal angulation and the tibiofemoral gaps in full extension and 90° flexion three times.
Statistical analysis
Statistical analysis was performed using the paired t-Test. A P-value of 0.05 was considered to be statistically significant. The analysis was carried out to determine the effect and possible significance of the different angles and gaps after each lateral release step. For comparing the leg axis and the medial gap in extension between each release step, box plots were used. The box height is the interquartile range which represents half of all values. Twenty-five percent of values are higher and 25% of values are lower than the box. The median is displayed as a horizontal line across each box. The minimum and maximum values are represented with the vertical lines.
Analysis of the data was performed using the SPSS statistical package (version 12.0, SPSS Inc., Chicago, IL).
Results
A.p. limb axis
The difference of the a.p. limb axis in extension measured by the navigation system for each release step was statistically significant (P < 0.009). The coronal angle increased constantly after each release step (Table 1, Fig. 4). Especially after the first (iliotibial band, P = 0.009), the third (LCL, P = 0.0004) and the fourth (posterolateral capsule, P = 0.000014) release step, the change in the leg axis was greater than for the other release steps.
Table 1.
Lateral release: change of the a.p. leg axis (in degrees) after sequential medial release compared with before release
| Lateral release step | Extension |
|---|---|
| Reference | 1.9 (1.91) |
| Iliotibial band on the level of the joint line | 4.02 (1.65) |
| Femoral attachment of the popliteus muscle | 5.63 (2.39) |
| Lateral collateral ligament from the femoral condyle | 7.56 (1.73) |
| Posterolateral capsule from the femoral side | 9.4 (1.66) |
| Lateral half of the posterior cruciate ligament | 10.44 (1.66) |
| Entire posterior cruciate ligament | 11.6 (1.53) |
Values are mean (standard deviation)
Fig. 4.
Change of the leg axis in degree during the lateral release sequence
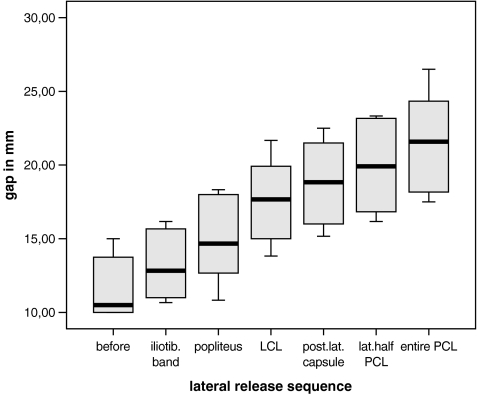
Lateral gap extension
For the lateral gap we found statistically significant progression (P < 0.002) in the gap distance for each release step (Table 2, Fig. 5). In extension the highest increase compared to the previous release step was found for the first (iliotibial band, P = 0.002), the second (popliteus muscle, P = 0.0003), the third (LCL, 0.007) and the sixth (entire PCL, P = 0.001) release step.
Table 2.
Lateral release: Change of the medial and lateral tibiofemoral gaps (in millimeters)
| Lateral release step | Lateral gap (mm) | Medial gap (mm) | ||
|---|---|---|---|---|
| Extension | 90° flexion | Extension | 90° flexion | |
| Reference | 11.69 (2.22) | 18.19 (1.65) | 9.58 (2.54) | 11.38 (2.37) |
| Iliotibial band on the level of the joint line | 13.23 (2.52) | 18.58 (1.81) | 9.6 (2.5) | 12.17 (2.57) |
| Femoral attachment of the popliteus muscle | 14.98 (2.99) | 20.42 (2.04) | 9.94 (2.68) | 12.63 (2.48) |
| Lateral collateral lig. from the femoral condyle | 17.58 (2.94) | 23.96 (3.13) | 10.19 (2.35) | 12.73 (2.77) |
| Posterolateral capsule from the femoral side | 18.79 (3.12) | 26.27 (2.83) | 10.65 (2.63) | 13.33 (2.52) |
| Lateral half of the posterior cruciate ligament | 19.92 (3.24) | 27.75 (2.94) | 10.52 (2.79) | 13.88 (2.59) |
| Entire posterior cruciate ligament | 21.52 (3.63) | 29.17 (3.08) | 11.44 (2.85) | 14.16 (1.92) |
Values are mean (standard deviation)
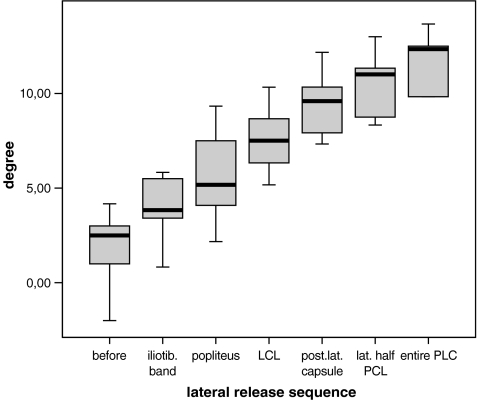
Fig. 5.
Changes of the lateral gap in mm during the lateral release sequence in extension
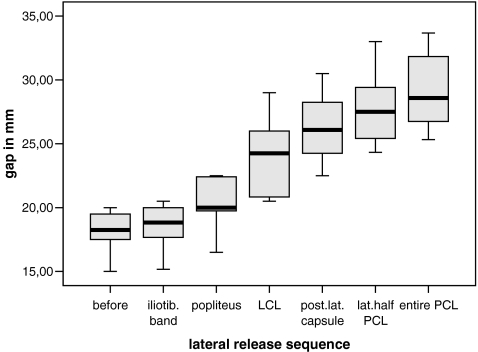
Lateral gap flexion
In 90° flexion all differences of the lateral release steps were statistically significant (P<0.004). Massive progression of the lateral gap in flexion was found after the second (popliteus muscle, P = 0.004) and the third (LCL, 0.007) release step (Table 2, Fig. 6).
Fig. 6.
Changes of the lateral gap in mm during the lateral release sequence in 90° flexion
Medial gap
Only little variation of the medial tibiofemoral gap was seen during the release sequence for extension and 90° flexion. Mean overall changes were 1.86 mm in extension and 2.78 mm in 90° flexion (Table 2).
Discussion
Longevity of a total knee prothesis is based on a perfectly aligned and a stable prosthesis over the full range of motion with sufficient tension of the soft tissues [19, 25]. It is commonly accepted that ligament balancing is an essential step in achieving this goal [4, 7, 13, 15]. It is a formidable challenge to correct these deformities especially in severe valgus knees. The current literature delivers many reports about different soft-tissue releases, their necessity and the clinical results of different techniques [7, 10, 13, 15, 21]. Up to now there have only been very few studies which focus on the effect of each lateral release step according to the leg axis [7, 9, 13, 15]. Many surgeons perform different surgical approaches and soft-tissue release sequences [2, 7, 8, 13, 15–18, 21, 23, 24]. Up to now, the effect of these release sequences has been based upon the experience of the surgeon. No measuring tool could determine the amount of the deformity and the necessity of release. To elucidate each effect of a standardised sequential lateral soft tissue release as recommended by Matsueda et al. [13] and to make the stepwise release more predictable, we performed a cadaver study and measured the resulting leg axis and the tibio-femoral gaps in extension and flexion with a navigation system.
In our study the highest increase compared to the previous release step was found for the first (iliotibial band, P = 0.002), second (popliteus muscle, P = 0.0003), third (LCL, 0.007) and the sixth (entire PCL, P = 0.001) release step in extension. These findings are similar to those of Matsueda [13] who found major effects when releasing the lateral collateral ligament and the lateral posterior capsule. Kanamiya et al. also found the lateral collateral ligament to be a strong stabilisation over the full range of movement [7].
In 90° flexion all differences of the lateral release steps were statistically significant (P = 0.004). Massive progression of the lateral gap in flexion was found after the second (popliteus muscle, P = 0.004) and third (LCL, P = 0.007) release step as well as the last (entire PCL, P = 0.0005).
This supports the findings of Krackow et al. [10] who reported (although in a medial release sequnece) that the sacrifice of the PCL led to a 4-mm increase of the flexion gap, but only little average increase for the extension gap of the same knee. Freeman performed a dynamic magnetic resonance imaging study and could demonstrate the behaviour of PCL in flexion and extension. His findings strengthen the hypothesis that PCL is tightened in 90° flexion, but not in full extension. Mihalko and co-workers report a similar effect (for a medial release sequence). They found a significantly larger flexion gap than extension gap after releasing the PCL [15]. The work of Krackow [9] on valgus knees supports our findings.
Up to now the current literature provides very few papers which deal with the same matter as our work [7, 9, 13, 15]. Mihalko [15] compares two different ligament-balancing techniques for gaining a balanced flexion and extension gap for the lateral side. Although they develop similar results as ours, the usage of cadaveric knees without hip and ankle joints is to be criticised. True assessment of the leg axis is not possible. This is also one aspect one might criticise focussing on Matsuedas et al.’s work [13], which used cadaveric knees with soft tissues removed and with transsection 30 cm from the joint space. Although the setup is standardised and the optical encoder used delivers reproducible results, their setup differs greatly from the clinical situation, as does the work of Kanamiya et al. [7]. Their calculation of gap widths and angles is far away from the clinical and intraoperative situation. This is the reason why we used full-body cadavers with all soft tissues in situ to come as close to the clinical situation as possible.
However, one criticism of the current study is that we studied the lateral release sequence on cadaveric, but normal knees without deformities. So, the magnitude of the changing a.p. leg axis and tibiofemoral gaps may differ from arthritic knees with valgus deformity. Another point to discuss is the concept of spreading the extension and flexion gap with the spreader device. Up to now there are very few reports about the “correct” tension in extension and flexion [5, 22]. There is still no commonly accepted view about the amount of tension for the soft tissues in total knee arthroplasty. Moreover the tension of soft tissues in cadavers may differ from the real situation. Nevertheless, we needed a consistent and calibrated tensioning device to gain reproducible moments for the medial as well as the lateral gap in extension and 90° flexion. This cannot be guaranteed by common laminar spreaders with the surgeon producing a manual tension [21].
However, overall we could show clearly that the use of a navigation system simplifies stepwise lateral soft tissue release and helps the surgeon to make the effect of each single step possible to visualise and predict. Thus, the highly demanding lateral release in valgus knees becomes easier and clearer with a navigation system in addition to better leg alignment.
In this cadaver study we could show the significant sequential increase of a defined lateral soft tissue release sequence. To the best of our knowledge this is the first study using a common navigation system for measuring a.p. leg axis as well as tibiofemoral gaps in extension and flexion. As far as the authors are concerned, the study is limited for the reason that we used knees without deformities as did other authors [7, 9, 13, 15]. The effect of the described release sequence may therefore differ from the clinical situaton. We are therefore working on a computer-assisted clinical outcome study focussing on the effect of sequential lateral soft-tissue release in knees with valgus deformities.
Conclusion
Our study addresses the effect of the sequential lateral soft tissue release in total knee replacement on the a.p. leg axis in extension and the tibiofemoral gaps in extension as well as in 90° flexion. The results underline that each sequential lateral soft-tissue release step has its desired influence on the a.p. leg axis and the tibiofemoral gaps, but there are differences between extension and flexion. The navigation system supports the surgeon and makes the lateral release step predictable.
References
- 1.Bäthis H, Perlick L, Tingart M, Lüring C, Zurakowski D, Grifka J (2004) Alignment in total knee arthroplasty: a comparison of computer-assisted implantation with the conventional technique. J Bone Joint Surg Br 86(5):682–687, Jul [DOI] [PubMed]
- 2.Clarke HD, Fuchs R, Scuderi GR, Scott WN, Insall JN (2005) Clinical results in valgus total knee arthroplasty with the pie-crust technique of lateral soft tissue releases. J Arthroplasty 20(8):1010–1014 [DOI] [PubMed]
- 3.Evaluation of image guided surgery systems (2002) Official report of the “medicines and healthcare products regulatory agency”, Deptartment of Health, UK MDA 01025
- 4.Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–978 [DOI] [PubMed]
- 5.Hiroshi A, Hoshino A, Wilton TJ (2004) Soft-tissue tension total knee arthroplasty. J Arthroplasty 19(5):558–561 [DOI] [PubMed]
- 6.Insall JN, Binazzi R, Soudry M, Mestriner LA (1985) Total knee arthroplasty. Clin Orthop 192:13–17 [PubMed]
- 7.Kanamiya T, Whiteside LA, Nakamura T, Mihalko WM, Steiger J, Naito M (2002) Effect of selctive lateral ligament release on stability in knee arthroplasty. Clin Orthop 404:24–31 [DOI] [PubMed]
- 8.Karachalios T, Sarangi PP, Newman JH (1994) Severe varus deformities treated by total knee arthroplasty. J Bone Joint Surg Br 76:938–943 [PubMed]
- 9.Krackow KA, Mihalko WM (1999) Flexion-extension joint gap changes after lateral structure release for valgus deformity correction in total knee arthroplasty: a cadaveric study. J Arthroplasty 14(8):994–1004 [DOI] [PubMed]
- 10.Krackow KA, Mihalko WM (1999) The effect of medial release on flexion and extension gaps in cadaveric knees: implications for soft tissue balancing in total knee arthroplasty. Am J Knee Surg 12:222–228 [PubMed]
- 11.Lüring C, Bäthis H, Hüfner T, Grauvogel C, Perlick L, Grifka J (2006) Gap configuration and a.p. leg axis after sequential medial ligament release in rotating platform total knee arthroplasty. Acta Orthop Scand 77(1):149–155 [DOI] [PubMed]
- 12.Lüring C, Hüfner T, Kendoff D, Perlick L, Bäthis H, Grifka J, Krettek C (2006) The Effect of medial soft tissue release in total knee arthroplasty: a navigation controlled cadaver study. J Arthroplasty 21(3):428–434, Apr [DOI] [PubMed]
- 13.Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB (1999) Soft tissue release in total knee arthroplasty. Cadaver study using knees without deformities. Clin Ortho 366:264–273 [DOI] [PubMed]
- 14.Matsueda S, Gengerke TR, Murphy M, Lew WD, Gustilo RB (1999) Changes in knee alignment after total knee arthroplasty. Clin Orthop 367:39–42 [DOI] [PubMed]
- 15.Mihalko WM, Whiteside LA, Krackow KA (2003) Comparison of ligament-balancing techiniques during total knee arthroplasty. J Bone Joint Surg (Am) 85:132–139 [DOI] [PubMed]
- 16.Miyasaka KC, Ranawat CS, Mullaji A (1997) 10- to 20-year folloup of total knee arthroplasty for valgus deformities. Clin Orthop 345:29–34 [PubMed]
- 17.Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS (2004) Total knee arthroplasty for severe valgus deformity. JBJS Am 86(12):2671–2676 [DOI] [PubMed]
- 18.Ranawat CS, Rose HA, Rich DS (1984) Total condylar knee arthroplasty for valgus and combined valgus-flexion deformity of the knee. Instr Course Lect 33:412–415 [PubMed]
- 19.Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop 299:153–159 [PubMed]
- 20.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L (2000) Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 71(3):262–267 [DOI] [PubMed]
- 21.Stern SH, Moeckel BH, Insall JN (1991) Total knee arthroplasty in valgus knees. Clin Orthop 273:5–9 [PubMed]
- 22.Takahashi T, Wada Y, Yamamoto H (1997) Soft-tissue balancing with pressure distribution during total knee arthroplasty. J Bone Joint Surg (Br) 79:235–238 [DOI] [PubMed]
- 23.Whiteside LA, Saeki K, Mihalko WM (2000) Functional ligament balancing in total knee arthroplasty. Clin Orthop 380:45–49 [DOI] [PubMed]
- 24.Whiteside LA (1993) Correction of ligament and bone defects in total knee arthroplasty of the severely valgus knee. Clin Orthop 288:234–238 [PubMed]
- 25.Winemaker MJ (2002) Perfect balance in total knee arthroplasty: the elusive compromise. J Arthroplasty 17:2–9 [DOI] [PubMed]