Abstract
Cervical spondylotic myelopathy is a common clinical problem. No study has examined the pattern of neurological recovery after surgical decompression. We conducted a prospective study on the pattern of neurological recovery after surgical decompression in patients with cervical spondylotic myelopathy. Patients suffering from cervical spondylotic myelopathy and requiring surgical decompression from January 1995 to December 2000 were prospectively included. Upper limbs, lower limbs and sphincter functions were assessed using the Japanese Orthopaedic Association (JOA) score. Assessment was done before the operation, at 1 week, 2 weeks, 1 month, 3 months, 6 months, 1 year and then yearly after surgery. Results were analysed with the t-test. Differences with P-values less than 0.05 were regarded as statistically significant. Fifty-five patients were included. The average follow-up period was 53 months. Thirty-nine patients (71%) had neurological improvement after the operation with a mean recovery rate of 55%. The JOA score improved after surgery, reaching statistical significance at 3 months and a plateau at 6 months. Thirty-six patients (65%) had improvement of upper limb function. Twenty-four patients (44%) had improvement of lower limb function. Eleven patients (20%) had improvement of sphincter function. The recovery rate of upper limb function was 37%, of lower limb function was 23% and of sphincter function was 17%. Surgical decompression worked well in patients with cervical spondylotic myelopathy. Seventy-one percent of patients had neurological improvement after the operation. The neurological recovery reached a plateau at 6 months after the operation. The upper limb function had the best recovery, followed by lower limb and sphincter functions.
Keywords: Cervical spondylotic myelopathy, Neurological recovery
Résumé
Les myélopathies cervicales sont un problème courant. Aucune étude n’a examiné la récupération neurologique après décompression chirurgicale. Nous avons conduit une étude prospective sur ce sujet, chez des patients ayant bénéficié d’une décompression pour myélopathie cervicale. Les patients opérés entre janvier 1995 et décembre 2000 ont été inclus dans cette étude. Les fonctions des membres supérieurs, des membres inférieurs et les fonctions sphinctériennes ont été évaluées selon le score de la JOA (Association Japonaise d’Orthopédie). L’évaluation a été réalisée avant l’opération, une semaine, deux semaines, un mois, trois mois, six mois, un an et chaque année après l’intervention chirurgicale. Les résultats ont été analysés selon le P test et en appréciant ensuite les résultats statistiquement ou non statistiquement significatifs. Cinquante-cinq patients ont été inclus. Le suivi moyen a été de 53 mois, 39 patients (71%) ont montré une amélioration neurologique après l’intervention avec un taux de récupération complète de 55%. Le score de la JOA a été amélioré à 3 mois avec un plateau de récupération à 6 mois. Trente-six patients (65%) ont vu une amélioration au niveau des fonctions du membre supérieur, 24 (44%) au niveau des membres inférieurs, 11 (5%) au niveau des fonctions sphinctériennes. Le taux de récupération au niveau des membres supérieurs a été de 37%, pour les membres inférieurs de 23% et pour les fonctions sphinctériennes de 17%. La décompression chirurgicale des myélopathies cervicales est une opération intéressante; 71% des patients ont vu une amélioration neurologique après l’intervention. Cette récupération atteint un plateau six mois après l’intervention. La récupération des membres supérieurs est la plus importante, suivie de la récupération des membres inférieurs puis de la récupération sphinctérienne. Mots clés : myélopathie cervicale, récupération neurologique.
Introduction
Cervical spondylotic myelopathy results from degenerative changes in the cervical spine and associated soft-tissue structures that lead to spinal canal stenosis, spinal cord compression and subsequent spinal cord dysfunction. Surgical decompression is recommended for patients with moderate to severe disease [1]. Studies have been done to evaluate the results of different treatment methods, namely sub-total corpectomy, laminectomy and laminoplasty [6, 13, 15, 20], and factors affecting the surgical outcomes [3, 4, 11, 18, 21]. However, these assessments tend to be of a more global perspective, looking at a composite score for upper limb, lower limb and bladder and bowel function. So far, no study has looked into the relative recovery of upper and lower limb function and bladder and bowel changes; this pattern of neurological recovery is important as it can inform both patients and surgeons about what to expect after the surgery. The aim of our study is to investigate the pattern of neurological recovery after surgical decompression for patients suffering from cervical spondylotic myelopathy.
Materials and methods
From January 1995 to January 2001, 55 consecutive patients suffering from cervical spondylotic myelopathy (CSM) underwent surgical treatment at a tertiary referral spine centre in Hong Kong and were prospectively included. The diagnosis of cervical myelopathy was made based on clinical signs and symptoms of cervical myelopathy with corresponding cervical stenosis on cervical magnetic resonance imaging.
Surgical treatments were performed for patients with a Japanese Orthopaedic Association score (JOA score) of less than 13 points (Table 1). Patients with one or two stenotic levels were treated with anterior decompression and anterior spinal fusion using autologous iliac crest bone graft. Patients with more than two stenotic levels and preserved cervical lordosis were treated with laminoplasty. Patients with more than two stenotic levels and loss of cervical lordosis were excluded from the study.
Table 1.
Japanese Orthopaedics Association score for cervical myelopathy
| Japanese Orthopaedics Association Score | |
|---|---|
| I | Motor function of upper extremity |
| 0: Unable to eat with either spoon or chopsticks | |
| 1: Possible to eat with spoon, but not chopsticks | |
| 2: Possible to eat with chopsticks, but inadequate | |
| 3: Possible to eat with chopsticks, but awkward | |
| 4: Normal | |
| II | Motor function of lower extremity |
| 0: Impossible to walk | |
| 1: Need cane or aid on flat ground | |
| 2: Need cane or aid only on stairs | |
| 3: Possible to walk without cane or aid, but slow | |
| 4: Normal | |
| III | Sensory deficit |
| A) Upper extremity | |
| 0: Apparent sensory loss | |
| 1: Minimal sensory loss | |
| 2: Normal | |
| B) Lower extremity | |
| 0: Apparent sensory loss | |
| 1: Minimal sensory loss | |
| 2: Normal | |
| C) Trunk | |
| 0: Apparent sensory loss | |
| 1: Minimal sensory loss | |
| 2: Normal | |
| IV | Sphincter dysfunction |
| 0: Complete urinary retention | |
| 1: Severe disturbance | |
| 2: Mild disturbance | |
| 3: Normal | |
Clinical conditions before and after surgical treatment were assessed using the Japanese Orthopaedic Association (JOA) score. The JOA score was assessed before the operation, at 1 week, 2 weeks, 1 month, 3 months, 6 months, 1 year and then yearly after the operation. A group of occupational therapists trained in JOA score assessment did all the assessments. The upper limb function score was defined as the upper limb motor JOA score plus the upper limb sensory JOA score, which gives a total of six points. The lower limb function score was defined as the lower limb motor JOA score plus the lower limb sensory JOA score, which gives a total of six points. The sphincter function was assessed by the sphincter function JOA score, which has a total of three points (Table 1). The pattern of neurological recovery in the overall JOA scores, upper limb function JOA score, lower limb function JOA score and sphincter function JOA score after surgical decompression were documented and analysed. Statistical analyses were done with one sample Student’s t-tests. P-values less than 0.05 were regarded as statistically significant.
Results
In total, 55 patients were included in the study; 35 were males (63%) and 20 were females (37%). The average patient age was 64 ± 11 years (average ± standard deviation). Twenty-seven patients (49%) were over 65 years old and 28 (51%) under 65 years old. The duration of myelopathy symptoms before surgery was 17 ± 30 months. Posterior decompressions were performed in 28 patients (51%) and anterior decompression in 27 patients (49%). The mean follow-up period was 54 ± 26 months, ranging from 15 to 103 months.
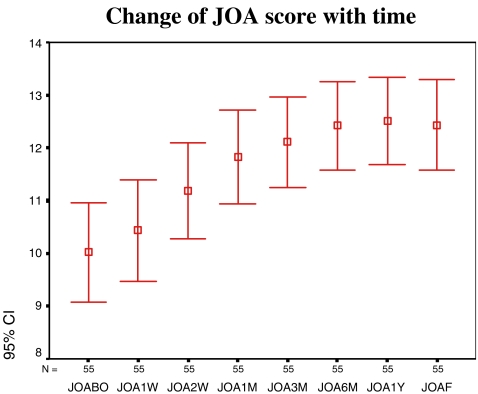
Thirty-nine patients (71%) had improvement of the JOA scores after the operation. The JOA scores improved gradually after surgical decompression. Statistically significant improvement was achieved at 3 months after operation and reached a plateau at 6 months (Fig. 1). The preoperative JOA score was 10.0 ± 3.5, and it improved to 12.4 ± 3.2 at the final follow-up. The mean recovery rate was 55%.
Fig. 1.
Change of JOA scores with time after surgical decompression. JOABO: JOA score before operation; JOA1W: JOA score at 1 week; JOA2W: at 2 weeks; JOA1M: at 1 month; JOA3M: at 3 months; JOA6M: at 6 months; JOA1Y: at 1 year; JOAF: at final
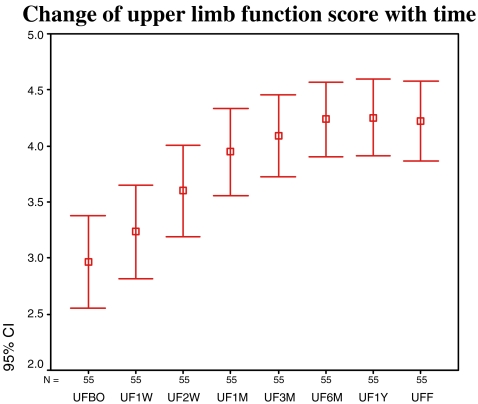
Thirty-six patients (65%) had improvement of upper limb function. The upper limb function score had a similar trend as the overall JOA score (Fig. 2). The upper limb function score improved from 3.0 ± 1.5 pre-operatively to 4.2 ± 1.3 at the final follow-up with an average recovery rate of 37%.
Fig. 2.
Change of upper limb function with time after surgical decompression. UFBO: upper limb function score before operation; UF1W: upper limb function score at 1 week; UF2W: at 2 weeks; UF1M: at 1 month; UF3M: at 3 months; UF6M: at 6 months; UF1Y: at 1 year; UFF: at final
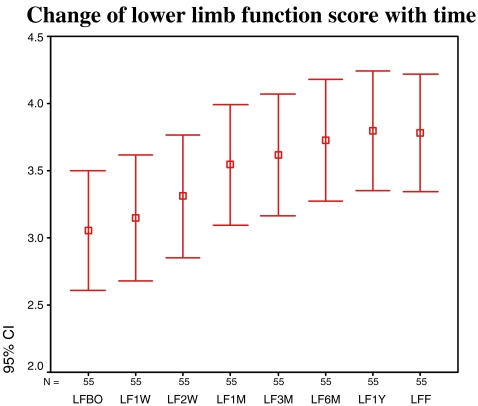
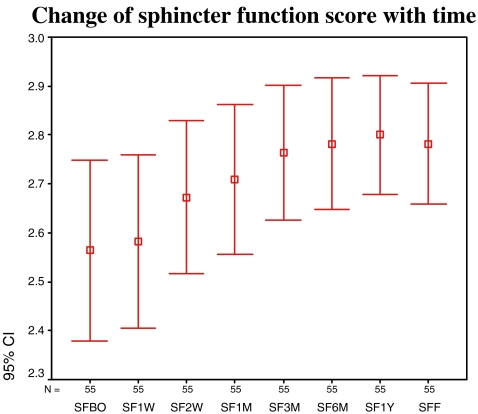
Twenty-four patients (44%) had improvement of lower limb function. The lower limb function score improved from 3.1 ± 1.7 pre-operatively to 3.8 ± 1.6 at the final follow-up with an average recovery rate of 23%. Eleven patients (20%) had an improvement of sphincter function after the operation with the pre-operative sphincter function JOA score improved from 2.6 ± 0.7 to 2.8 ± 0.5 with an average recovery rate of 17%. The recovery rate of upper limb function was higher compared with lower limb and sphincter functions, though the differences were not statistically significant (Table 2). The pattern of lower limb and sphincter function improvement also followed that of the upper limbs and overall JOA scores (Figs. 3 and 4). However, they could not reach statistical significance at the final follow-up.
Table 2.
Upper limb, lower limb and sphincter function recovery after surgical decompressions
| Pre-operative score | Final score | Recovery rate % | |
|---|---|---|---|
| Upper limb function score | 2.9 | 4.2 | 37 |
| Lower limb function score | 3.1 | 3.8 | 23 |
| Sphincter function score | 2.6 | 2.8 | 17 |
Fig. 3.
Change of lower limb function score with time. LFBO: lower limb function score before operation; LF1W: Lower limb function score at 1 week; LF2W: at 2 weeks; LF1M: at 1 month; LF3M: at 3 months; LF6M: at 6 months; LF1Y: at 1 year; LFF: at final
Fig. 4.
Change of sphincter function score with time. SFBO: Sphincter function before operation; SF1W: sphincter function at 1 week; SF2W: at 2 weeks; SF1M: at 1 month; SF3M: at 3 months; SF6M: at 6 months; SF1Y: at 1 year; SFF: at final
Patients aged above 65 years had significantly lower pre-operative and final JOA scores compared with patients aged below 65 years. The mean pre-operative JOA score for patients above 65 years of age was 8.3 ± 3.5 and for patients below 65 years of age was 11.7 ± 2.7. There was significant improvement in the JOA score after surgical decompression in both groups of patients. The JOA score for patients aged above 65 years improved from 8.3 ± 3.5 to 11.0 ± 3.5 with a recovery rate of 33%. The JOA score for patients aged below 65 years improved from 11.7 ± 2.7 to 13.8 ± 2.1 with a recovery rate of 40%. There was no significant difference in the recovery rate between the two groups (Table 3).
Table 3.
JOA scores and recovery rates in different age groups, genders and pre-operative duration of symptoms
| Pre-operative JOA score | Final JOA score | Recovery rate % | |
|---|---|---|---|
| Age <65 | 11.7+ | 13.8 | 40 |
| Age >65 | 8.3+ | 11.0 | 33 |
| Male | 10.5 | 12.6 | 52 |
| Female | 9.1 | 12.2 | 60 |
| Symptoms duration <6 months | 8.6 | 11.5 | 46 |
| Symptoms duration 6–12 months | 10.3 | 13.4 | 88 |
| Symptoms duration >12 months | 10.6 | 11.6 | 28 |
+Difference in pre-operative JOA scores in different age groups was statistically significant (P < 0.05)
Both male and female patients had significant improvement in JOA scores after surgical decompression. The JOA scores in male patients improved from 10.5 ± 3.5 to 12.6 ± 3.4 after surgery with a recovery rate of 52%. The JOA scores in female patients improved from 9.1 ± 3.4 to 12.2 ± 2.8 after surgery with a recovery rate of 60% (Table 3). The differences were not statistically significant.
There was also no significant difference in neurological recovery for patients with different pre-operative durations of symptoms. The JOA scores for patients with a pre-operative duration of symptoms less than 6 months improved from 8.6 ± 3.4 to 11.5 ± 3.4 with a recovery rate of 46%. The JOA scores for patients with a pre-operative duration of symptoms from 6 to 12 months improved from 10.3 ± 3.9 to 13.4 ± 1.7 with an 88% recovery rate. The JOA scores for patients with a pre-operative duration of symptoms of more than 12 months improved from 10.6 ± 3.6 to 11.6 ± 3.3 post-operatively with a recovery rate of 28% (Table 3).
Discussion
Cervical spondylotic myelopathy causes upper limb, lower limb and sphincter dysfunctions. Surgical decompression has been shown to be effective in relieving these symptoms. Prakash et al. compared patients with cervical spondylotic myelopathy treated conservatively and treated surgically. The surgically treated group had significant improvement in neurological symptoms and functional status compared to a significant worsening in neurological symptoms in the non-surgically treated group [17]. Surgical decompression using anterior or posterior approaches produce excellent and good results in approximately 70% of patients [2, 19, 22]. Fessler et al. reported 92% of patients had symptom improvement after anterior decompression and fusion for cervical spondylotic myelopathy [9]. However, multi-level anterior decompression and fusion have been shown to have complication rates up to 60% [15]. Bone graft dislodgement after multi-level corpectomies is very common [1, 8, 12]. In order to avoid such high complication rates with multiple level anterior decompression and fusion, posterior decompression has been advocated. Edwards et al. reported 83% of patients developed improvement of neurological symptoms after laminoplasty [6]. Yonenobu et al. compared subtotal corpectomy versus laminoplasty with 10-year follow-up. They showed no difference in neurological outcomes between the two groups. However, the laminoplasty group had more axial neck pain and less cervical range of movements [20]. Sagittal alignment of the cervical spine is important for laminoplasty to have an indirect decompressive effect on the spinal cord. Laminoplasty for patients with cervical kyphosis has been shown to have a poor outcome [8, 14]. Based on this information, we offered anterior decompression and fusion for patients with one or two levels of disease. For patients with more than two levels of disease with preservation of cervical lordosis, we offered laminoplasty. Patients with more than two levels of disease involving the kyphotic cervical spine were excluded from the study because of the higher complication rate.
Though there are many studies demonstrating good neurological recovery after surgical decompression for cervical spondylotic myelopathy, there are few studies showing the temporal manner of the neurological recovery and pattern of neurological recovery. Prabha et al. reported 26 patients with significant improvement in hand function in terms of the Jebsen-Taylor test and 10-s test at 1 week after surgical decompression [16]. Engsberg et al. described neurological recovery of one patient after a one-level anterior decompression and anterior spinal fusion for cervical spondylotic myelopathy. The patient had elbow flexor spasticity that returned to normal at 11 days after the operation, gradual improvement of upper limb power and walking speed up to 6 months after operation [7]. The JOA score is commonly used to assess the severity of symptoms in patients with cervical spondylotic myelopathy [6, 10, 21, 22]. It assesses the upper limb, lower limb and sphincter functions of patients. It is useful in pre-operative assessment and also to monitor the neurological recovery post-operatively. In our study, we demonstrated improvement in upper limbs, lower limbs and sphincter functions in terms of the JOA score after surgical decompression. They gradually improved, reached statistical significance at 3 months then reached a plateau at 6 months.
Chiles et al. followed up 75 patients with anterior decompression and anterior spinal fusion done for cervical spondylotic myelopathy for 1 year. He found that 46.7% of patients had improvement of lower limb function and 75.4% patients had improvement in upper limb function [5]. It appeared that the upper limbs recovered better compared with lower limbs. Our study shared similar findings. Thirty-six patients (65%) had improvement of overall upper limb function compared with 24 patients (44%) who had improvement of overall lower limb functions. The recovery rate of overall upper limb function was the best (37%), followed by lower limb function (23%) then sphincter function (17%). The differences were not statistically significant probably due to the small sample size.
Prognostic factors for surgical treatment of cervical spondylotic myelopathy are still controversial. Tomosato [21] and Fessler [9] reported no difference in neurological recovery for patients aged below and above 65 years after surgical decompression.
However, Yonenobu [10] showed post-operative recovery of spinal cord function in the older age group is inferior to that of younger patients. In our study we found that older patients had a significantly lower pre-operative JOA score. This finding was also present in Tomosato’s study. It may be due to the functional demand of elderly patients, which is less compared with younger patients, so they can tolerate more functional loss before seeking medical advice, or some patients are reluctant to undergo surgery at younger ages and their condition thus deteriorated when they got older and required treatment. Our study showed that the recovery rate for patients aged below and above 65 years were 40% and 33%, respectively, while there may be a trend to suggest that patients over age 65 recover less well. There was no significant difference between the two age groups. Tomosato [21] demonstrated patients with a longer duration of symptoms had inferior neurological recovery. However, Fessler and Chung reported the duration of symptoms did not affect surgical outcomes [4, 9]. In our study, there was no significant difference in neurological recovery in patients with different pre-operative durations of symptoms.
Conclusion
This is the first study to look at the pattern of neurological recovery after surgical decompression in patients suffering from cervical spondylotic myelopathy. Surgical decompression for cervical spondylotic myelopathy produced neurological recovery in 71% of patients. The neurological recovery in terms of JOA scores improved after surgical decompression, reached statistical significance at 3 months and reached a plateau at 6 months. The neurological recovery apparently was best in the upper limb function, followed by lower limb function, and was worst in the sphincter function. There was no significant difference in neurological recovery in patients with different genders, age groups and pre-operative duration of symptoms.
References
- 1.Bernard TN Jr, Whitecloud TS (1987) Cervical spondylotic myelopathy and myeloradiculopathy. Anterior decompression and stabilization with autologenous fibula strut graft. Clin orthop 221:149–160 [PubMed]
- 2.Carol MP, Ducker TB (1998) Cervical spondylitic myelopathies: Surgical treatment. J spinal disorders 1:59–65 [PubMed]
- 3.Chen CJ, Lyu RK, Lee ST, Wong YC, Wang LJ (2001) Intramedullary high signal intensity on T2-weighted MR images in cervical spondylotic myelopathy: Prediction of prognosis with type of intensity. Neuroradiology 221:789–794 [DOI] [PubMed]
- 4.Chung SS, Lee SC, Chung KH (2002) Factors affecting the surgical results of expansive laminoplasty for cervical spondylotic myelopathy. Int Orthop 26:334–338 [DOI] [PMC free article] [PubMed]
- 5.Chiles BW, Leonard MA, Choudhri HF, Cooper PR (1999) Cervical spondylotic myelopathy: patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery 44:762–770 [DOI] [PubMed]
- 6.Edwards CC, Heller JG, Silcox DH (2000) T-saw laminoplasty for the management of cervical spondylotic myelopathy-Clinical and radiological outcome. Spine 25:1788–1794 [DOI] [PubMed]
- 7.Engsberg JR, Laurysseen C, Ross SA, Hollman JH, Walker D, Wippold FJ (2003) Spasticity, trength, and gait changes after surgery for cervical spondylotic myelopathy-A case report. Spine 28:E136–E139 [DOI] [PubMed]
- 8.Fernyhough JC, White JI, LaRocca H (1991) Fusion rates in multi-level cervical spondylosis comparing allograft fibula with autograft fibula in 126 patients. Spine 16:S561–S564 [DOI] [PubMed]
- 9.Fessler RG, Steck JC, Giovanini MA (1998) Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery 43:257–267 [DOI] [PubMed]
- 10.Fujiwara K, Yonenobu K, Ebara S, Yamashita K, Ono K (1989) The prognosis of surgery for cervical decompression myelopathy. J Bone Joint Surg (Br) 81:393–398 [DOI] [PubMed]
- 11.Hasegawa K, Homma T, Chiba Y, Hirano T, Watanabe K, Yamazaki A (2002) Effects of surgical treatment for cervical spondylotic myelopathy in patients >70 years of age: A retrospective comparative study. J Spinal Disorder Tech 15:458–460 [DOI] [PubMed]
- 12.Herkowitz HN (1989) The surgical management of cervical spondylotic radiculopathy and myelopathy. Clin Orthop 239:94–108 [PubMed]
- 13.Houten JK, Cooper PR (2003) Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression and neurological outcome. Neurosurgery 52:1081–1088 [DOI] [PubMed]
- 14.Kawakami M, Tamaki T, Ando M, Yamada H, Yoshida M (2002) Relationships between sagittal alignment of the cervical spine and morphology of the spinal cord and clinical outcomes in patients with cervical spondylotic myelopathy treated with expansive laminoplasty. J Spinal Disorder Tech 15:391–397 [DOI] [PubMed]
- 15.Pavlov P (2003) Anterior decompression for cervical spondylotic myelopathy. Eur Spine J 12(Suppl 2):S188–S194 [DOI] [PMC free article] [PubMed]
- 16.Prabhu K, Babu KS, Bot SS, Chacko AG (2005) Rapid opening and closing of the hand as a measure of early neurologic recovery in the upper extremity after surgery for cervical spondylotic myelopathy. Arch Phys Med Rehabil 86:105–108 [DOI] [PubMed]
- 17.Sampath P, Bendebba M, Davis J, Ducker TB (2000) Outcomes of patients treated for cervical myelopathy-A prospective, multicentre study with independent clinical review. Spine 25:670–676 [DOI] [PubMed]
- 18.Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M (2003) Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine 28:1258–1262 [DOI] [PubMed]
- 19.Teramoto T, Ohmori K, Takatsu T, Inoue H, Ishida Y, Suzuki K (1994) A long-term results of anterior cervical spondylodesis. Neurosurgery 35:64–68 [DOI] [PubMed]
- 20.Wada E, Suzuki S, Kanazawa A, Matsuoka T, Miyamoto S, Yonenobu K (2001) Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy-A long-term follow-up study over 10 years. Spine 13:1443–1444 [DOI] [PubMed]
- 21.Yamazaki T, Yanaka K, Sato H, Uemura K, Tsukada A, Nose T (2003) Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differencec. Neurosurgery 52:122–126 [DOI] [PubMed]
- 22.Yonenobu K, Hosono N, Iwasaki M, Asano M, Ono K (1992) Laminoplasty versus subtotal corpectomy: A comparative study of results in multisegment cervical spondylotic myelopathy. Spine 17:1281–1284 [DOI] [PubMed]