Abstract
The rotational axis of the tibial component in total knee arthroplasty described by Insall is generally accepted, but rotational mismatch between the femoral and the tibial components can occur because the alignment of each component is determined separately. We developed a connecting instrument to synchronise the axis of the tibia to the axis of the femur. We compared the rotational axis of the tibial component using our method and medial one third of tibial tuberosity (Insall’s reference) in 70 consecutive TKAs. The rotational axis of the tibial component from the femoro-tibial synchronisation was rotated internally 13.8° ± 5.8° (range, 2° – 24°) more than the axis of Insall’s reference. Eighty three percent of patellae tracked centrally and the patellae tilt measured 2.2° on average. More attention should be given to the rotational congruency between the femoro-tibial components, because the recent prosthetic design has more conforming articular surfaces.
Résumé
La rotation axiale du composant tibial dans la prothèse totale du genou décrite par Insall est généralement acceptée mais elle peut poser problème lorsqu’il existe un trouble de rotation sur le composant fémoral et le composant tibial du fait d’une détermination séparée de la position de chaque composant au moment de l’implantation. Nous avons pour cela développé un instrument qui permet de synchroniser l’axe du tibia et l’axe du fémur. Nous avons comparé la rotation axiale du composant tibial en utilisant notre méthode à propos de 70 prothèses totales consécutives du genou. L’axe de rotation après synchronisation des deux composants a été noté en rotation interne. Cette rotation interne est plus importante que celle prévue par l’axe de référence d’Insall qui est représenté par le tiers interne de la tubérosité tibio-intérieure. 83% des rotules avaient une course normale et un accrochage rotulien a été noté dans 2,2% en moyenne. Une attention particulière doit être portée à la congruence en rotation des éléments fémoro-tibiaux pendant l’implantation d’une PTG d’autant que cette congruence est plus importante dans les nouveaux dessins de prothèses totales du genou récentes.
Introduction
Correct rotational alignment of femoral and tibial components is one of the difficult and controversial aspects in total knee arthroplasty (TKA), but as of yet, there is no ‘golden rule’ for this subject [1, 10, 13, 14, 16, 23, 25]. Numerous studies have been undertaken to establish the rotational axis of the femur whereby the transepicondylar axis is regarded as more reliable [4, 7]. For the rotational axis of the tibia, medial 1/3 of the tibial tuberosity advocated by Insall (Insall’s reference) is approved by most surgeons [14]. But determination of the rotation by fixed anatomical landmarks can lead to rotational mismatch between the femoral and the tibial components. Incorrect kinematics caused by femoro-tibial rotational mismatch can cause several problems such as femoro-tibial subluxation, accelerated tibial polyethylene (PE) wear and patellofemoral dysfunction [2, 4, 20].
In this study, we describe a method to determine the rotational axis of the tibial component with reference to the rotation of the femoral component to achieve rotational congruency and compare it with Insall’s reference.
Patients and methods
We conducted a prospective, observational study of 70 consecutive primary posterior cruciate ligament substituting TKAs (Scorpio, Osteonics, Stryker, New Jersey, USA) in 70 patients. There were three men and 67 women enrolled in the study. The mean age of the patients at the time of surgery was 69 ± 6.6 years (range, 54–82 years). Patients had a confirmed diagnosis of degenerative osteoarthritis in 69, and osteonecrosis of distal femur in one. Two kinds of rotational axes of the tibial component were measured intraoperatively. The first was the axis of the tibial component using a customised instrument (Linker) developed for the rotational congruency between the femoro-tibial components. The second was the line connecting the medial 1/3 of the tibial tuberosity and the centre of the posterior cruciate ligament, described by Insall [14]. We postulated that the rotational congruency between the femoral and the tibial component in full extension could be achieved by the author’s method using Linker.
Surgical technique
All procedures were performed by a single senior surgeon. A standard midline skin and capsular incision that divides the quadriceps tendon in its medial 1/3 and peels the quadriceps expansion from patella was performed. Soft tissue balancing was performed by release of medial soft tissues, both cruciate ligaments and cheilectomy. These procedures were progressively performed to correct a fixed deformity, bringing the limb alignment into an approximate mechanical axis. Coronal and sagittal alignment of the femoral component were determined using the intramedullary alignment system and rotational alignment was accessed with the transepicondylar axis (TEA) and Whiteside’s line. After anterior skim cut, the distal femoral cutting block was assembled and adjusted to match the thickness of the femoral component (for example, 8 mm for Scorpio). Once in place, the distal femoral cutting block represented coronal, saggital and rotational axes of the femoral component.
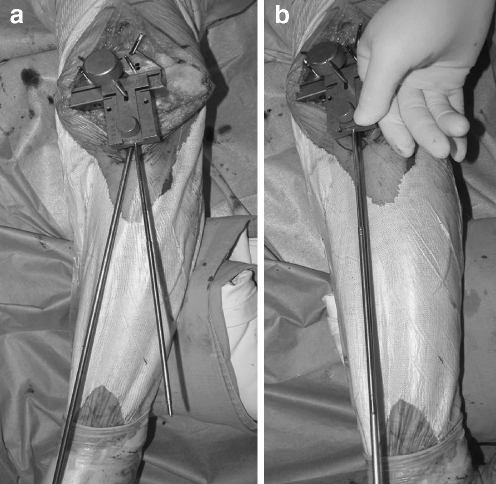
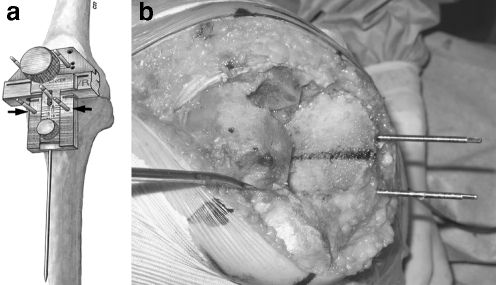
Next, we used a connecting instrument (Linker) to place the proximal tibial cutting block. After a headless pin was inserted just below the tibial plateau on the line of the mechanical axis of the tibia, the knee was fully extended. While maintaining the knee in full extension, a specially designed instrument (Linker) to synchronise the three dimensional axes between the femoral and tibial components was connected with the cutting slot of the distal femoral cutting block over the headless pin of the proximal tibia (Fig. 1a). With this procedure, the direction of the tail of Linker represented the mechanical axis of the femur. Additional mediolateral soft tissue balancing was performed until the mechanical axis of the tibia could be parallel to the tail of Linker (Fig. 1b). The goal in this procedure was to gain proper limb alignment with equal tension on the medial and lateral collateral ligaments. During tensioning of both collateral ligaments, varus or valgus stresses were applied to identify any remaining laxity; in addition, the alignment of the second toe was confirmed to point anteriorly because a degree of rotational movement might be possible after removing both cruciate ligaments. Keeping the mechanical axes between femur and tibia parallel, a pair of headless pins were inserted into the holes of Linker and the direction of these two pins indicated the rotation of the tibial component (Fig. 2a). Using this procedure, we could determine the three dimensional axes of the tibial component including the rotational axis that is synchronised with the axis of the femoral component. After resection of the proximal tibia, the rotational axis of the tibial component was marked with methylene blue on the cut surface of the tibia (Fig. 2b). The medial and lateral borders of tibial tuberosity were palpated and marked at both medial 1/3 of the tubercle and at the centre of the tibial insertion area of the posterior cruciate ligament with methylene blue. Then the axis advocated by Insall was also marked on the cut surface of the tibia. The angle between the two axes was measured with a protractor.
Fig. 1.
a The tail of the connecting instrument (Linker) represents the mechanical axis of the femur. b Mechanical axis of the femur and the tibia could be parallel after meticulous balancing of the soft tissues
Fig. 2.
a The rotational axis of the tibial component is synchronised with the rotation of the femoral component by using Linker. Two headless pins (arrow) were inserted into the holes of Linker. b A line parallel to the headless pins indicates the rotational axis of the tibial component
Postoperatively, the tilt of the patella was measured by the methods described by Gomes et al. [12]. Statistical analysis was performed with the use of SPSS statistical software system version 11.5 (SPSS Inc., Chicago, Illinois). The t-test for paired samples was used to compare the rotation of the tibial component between the authors’ method and Insall’s reference. The relationship between lateral patellar tilting and the angular deviation between the authors’ method and Insall’s reference was analysed with Spearman correlation analysis. P values of <0.05 were regarded as significant.
Results
With the knee in full extension, the axis tibial component with the femoro-tibial synchronisation was rotated internally 13.8° ± 5.8° (range, 2° – 24°) more than the axis of Insall (p < 0.001). Eighty three percent of the knees tracked centrally, and 17% tilted laterally. The amount of tilt of patella was a mean of 2.2° ± 3.5° (range, 0° – 15°). There was no statistical relationship between the incidence and severity of lateral patella tilting, and the angular deviation between the author’s method and Insall’s reference (Spearman’s correlation coefficient r = 0.093, p = 0.46).
Discussion
Three different methods in determining rotational reference axes of the femoral component are generally accepted [4, 7]. These include the posterior condylar axis, the midtrochlear line (so called ‘Whiteside’s line’) and the transepicondylar axis (TEA). The posterior condylar axis is generally believed not to present a neutral mediolateral axis, especially in valgus or severely varus knee. In almost all knees, TEA and Whiteside’s line are approximately perpendicular to each other and they are reported as being more predictable than the posterior condyle [7].
In contrast to the femur, less attention has been given to the rotational axis of the tibial component, and it is more equivocal compared to the femoral side [1, 8, 9, 17]. Insall advocated that the tibial component should be aligned to the line connecting the medial 1/3 of the tibial tuberosity and the centre of posterior cruciate ligament [14]. Akagi et al. [1] demonstrated that medial border of patella tendon attachment at the tibia can serve as a reliable anterior landmark to determine the anteroposterior axis of the tibia. Furthermore, the mid-sulcus line of the tibial spine [8], the transcondylar line of tibia [9] and the posterior tibial condylar line [17] have also been suggested as a guide for the reference axis of tibial rotation. Although anatomical landmarks described by Insall or Akagi appear to be acceptable, they also might have the problem in that rotational alignment between femoral and tibial components could not be completely matched because the alignment of each component was determined separately. Rotational mismatch caused by reliance on a fixed anatomical landmarks can lead to several problems such as patellofemoral dysfunction, accelerated tibial PE wear, premature component loosening, toe-in gait, and even total knee dislocation [2, 4, 20, 23]. Another useful method that avoids an anatomical landmark is the ROM technique [3, 10], in which the tibial component rotation is determined by flexion and extension with a trial component in place allowing the tibial trial to seek its own rotation. However, it also has the disadvantage due to the difficulty in marking the proper rotational position on the anterior tibial cortex [3, 10].
In this investigation of 70 primary TKAs with synchronisation of the femoro-tibial component, the rotational axis of the tibial component showed the tendency to rotate internally on average 13.8° more than the axis of Insall’s reference. There are several reports that aligning the tibial component with the medial 1/3 of the tibial tuberosity will result in excessive external rotation in some cases [8, 10, 23]. Eckhoff et al. [10] documented the amount of malrotation between the femoral and tibial components with a contemporary alignment technique. They reported the average external rotation of the tibial component relative to the femoral component associated with the reference of tibial tuberosity was 19° and those rotational mismatches might account for posteromedial polyethylene wear. Uehara et al. [23] demonstrated a tendency to align the tibial component in external rotation relative to the femoral component using computed tomography. He reported rotational mismatch in nearly 50% of the subjects between the axis of medial 1/3 of the tibial tuberosity and the transepicondylar axis for femur.
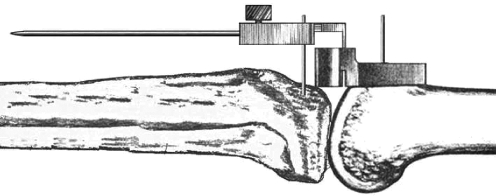
We believe the differences in our study may come from “screw-home” motion. External rotation of the tibia with respect to the femur that accompanies knee extension, the so-called “screw-home” motion, is known to occur in the normal knee [6]. This motion is thought to be a complex function of surface geometry, tension of ligamentous structures and the action of muscles [6, 15]. Several investigations were performed to determine whether screw-home motion occurs in TKA [6, 15, 19, 22, 24]. The asymmetry of the tibial articular surface and properly tensioned posterior cruciate ligament were suggested to be important factors in allowing the screw-home motion to occur in TKA [24]. Ishii asserted that the activity of the muscle may have greater effects on the screw-home motion than the presence of ligamentous structures demonstrating the screw-home motion occurs in a PCL substituting prosthesis under the load of body weight [15]. If screw-home motion is to occur after total knee arthroplasty, the rotational congruency should be checked in full extension. We determined the rotational axis of the tibial component with intact bony geometry in full extension so that screw-home motion could be in effect; thus the rotational congruency would be achieved with the knee in full extension (Fig. 3). Although rotational incongruity during range of motion may be unavoidable, we believe that rotational congruency is most important in full extension.
Fig. 3.
The rotational axis of the tibial component was determined with intact bony geometry in full extension so that screw-home motion could be in action; thus the rotational congruency could be achieved with the knee in full extension
Another possible cause of the difference is medial torsion of the tibia. Nagamine et al. [18] demonstrated that the foot could be severely rotated internally if the medial 1/3 of the tibial tuberosity was used as a guide to rotational alignment in patients with severe medial torsion of the tibia. In patients from East Asian countries, medial torsion of the tibia should be taken into account, because it can aggravate rotational mismatch.
This investigation has several limitations. First, the method of intraoperative measurement that we used (although the authors gave significant attention to the accuracy) may be less accurate than that undertaken with more sophisticated equipment like computed tomography. Second, we did not analyse the accuracy of rotation of the femoral component postoperatively. If the femoral component was rotated internally, it would magnify the result of this study because the rotation of the tibial component was determined in accordance with the femoral rotation. Third, we postulated that proper rotational congruency between femoro-tibial components could be achieved with our connecting technique, but we didn’t verify the congruency postoperatively as was done by Eckhoff [10, 11].
Our result may confuse the common belief that external rotation of the tibial component is favourable to avoid patello-femoral complications. Although our technique leads to more internal rotation of the tibial component than Insall’s reference, patellofemoral tracking was within an acceptable range [5, 21]. If the femoral component is too internally rotated with our connecting technique, the rotation of the tibial component would also be rotated internally in accordance with the femoral component. This might conflict between the congruency of the femoro-tibial joint and patellofemoral dynamics. Therefore, we are careful to make a proper alignment of the femoral component, especially with respect to internal rotation.
In conclusion, more attention should be given to the rotational congruency between femoro-tibial components, because recent prosthetic designs have more conforming articular surfaces. The rotational axis with the reference of medial 1/3 of the tibial tuberosity can lead to excessive external rotation of the tibial component. We believe that our technique of femoro-tibial synchronisation may be a solution to avoid rotational mismatch.
References
- 1.Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C (2005) Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 436:172–176 [DOI] [PubMed]
- 2.Bargren JH (1980) Total knee dislocation due to rotatory malalignment of tibial component: a case report. Clin Orthop Relat Res 147:271–274 [PubMed]
- 3.Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55 [DOI] [PubMed]
- 4.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47 [PubMed]
- 5.Bindelglass DF, Cohen JL, Dorr LD (1993) Patellar tilt and subluxation in total knee arthroplasty. Relationship to pain, fixation, and design. Clin Orthop 286:103–109 [PubMed]
- 6.Blankevoort L, Huiskes R, de Lange A (1988) The envelope of passive knee joint motion. J Biomech 21:705–720 [DOI] [PubMed]
- 7.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–118 [DOI] [PubMed]
- 8.Dalury DF, Jiranek W, Pierson J, Pearson SE (2003) The long-term outcome of total knee patients with moderate loss of motion. J Knee Surg 16:215–220 [PubMed]
- 9.Eckhoff DG, Johnston RJ, Stamm ER, Kilcoyne RF, Wiedel JD (1994) Version of the osteoarthritic knee. J Arthroplasty 9:73–79 [DOI] [PubMed]
- 10.Eckhoff DG, Metzger RG, Vandewalle MV (1995) Malrotation associated with implant alignment technique in total knee arthroplasty. Clin Orthop Relat Res 321:28–31 [PubMed]
- 11.Eckhoff DG, Piatt BE, Gnadinger CA, Blaschke RC (1995) Assessing rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 318:176–181 [PubMed]
- 12.Gomes LS, Bechtold JE, Gustilo RB (1988) Patellar prosthesis positioning in total knee arthroplasty. A roentgenographic study. Clin Orthop Relat Res 236:72–81 [PubMed]
- 13.Huddleston JI, Scott RD, Wimberley DW (2005) Determination of neutral tibial rotational alignment in rotating platform TKA. Clin Orthop Relat Res 440:101–106 [DOI] [PubMed]
- 14.Insall JN (2001) Surgery of the knee. Churchill-Livingstone, New York
- 15.Ishii Y, Terajima K, Koga Y, Bechtold JE (1999) Screw home motion after total knee replacement. Clin Orthop Relat Res 358:181–187 [DOI] [PubMed]
- 16.Minns RJ (1991) A simple guide for rotational alignment of the tibial component in knee arthroplasty. Acta Orthop Scand 62:266–267 [DOI] [PubMed]
- 17.Moreland JR (1988) Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res 226:49–64 [PubMed]
- 18.Nagamine R, Miyanishi K, Miura H, Urabe K, Matsuda S, Iwamoto Y (2003) Medial torsion of the tibia in Japanese patients with osteoarthritis of the knee. Clin Orthop Relat Res 408:218–224 [DOI] [PubMed]
- 19.Piazza SJ, Cavanagh PR (2000) Measurement of the screw-home motion of the knee is sensitive to errors in axis alignment. J Biomech 33:1029–1034 [DOI] [PubMed]
- 20.Puloski SK, McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB (2001) Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. J Bone Joint Surg 83-A:390–397 [DOI] [PubMed]
- 21.Rand JA (1994) The patellofemoral joint in total knee arthroplasty. J Bone Joint Surg 76-A:612–620 [DOI] [PubMed]
- 22.Stein A, Fleming B, Pope MH, Howe JG (1988) Total knee arthroplasty kinematics. An in vivo evaluation of four different designs. J Arthroplasty 3(suppl):31–36 [DOI] [PubMed]
- 23.Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y (2002) Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 402:196–201 [DOI] [PubMed]
- 24.Whiteside LA, Kasselt MR, Haynes DW (1987) Varus-valgus and rotational stability in rotationally unconstrained total knee arthroplasty. Clin Orthop Relat Res 219:147–157 [PubMed]
- 25.Yamada K, Imaizumi T, Takada N (2003) Linkage guide for rotational alignment during total knee arthroplasty. J Orthop Sci 8:643–647 [DOI] [PubMed]