Abstract
The purpose of this paper was to evaluate the results of acetabular revisions with the use of an oblong revision cup that is designed with its longitudinal diameter elongated relative to its transverse diameter. Between 1996 and 2001, 62 hips in 60 patients underwent an acetabular revision with the insertion of a LOR acetabular component. Seven hips were lost to follow-up or the patients died; the remaining 55 hips (53 patients) remained in follow-up for an average of 7.2 years (range: 5.0–10.1 years). One socket was revised for aseptic loosening, and another was operated on for a late polyethylene liner dissociation. The average Harris hip score (HHS) improved from 34 to 79. Results were rated as excellent in 16 hips, good in 28, fair in six and poor in three. Radiographic analysis demonstrated an improvement in the average vertical displacement of the hip centre: 49 hips had a well-fixed, bone-ingrown cup and four had a stable fibrous union. For large superolateral acetabular bone deficiencies, this implant facilitated a complex reconstruction without the need for bulk structural acetabular bone grafts, provided good clinical results and showed satisfactory stability at the midterm follow-up.
Résumé
Le but de cette étude est d’évaluer les résultats des révisions acétabulaires par l’utilisation d’une cupule oblongue. 62 hanches chez 60 patients ont bénéficié de cette révision acétabulaire avec cet insert (LOR). Ces révisions ont été réalisées de 1996 à 2001. 7 hanches ont été perdues de vue ou les patients décédés, 55 hanches (53 patients) ont été suivies en moyenne pendant 7,2 ans (de 5 à 10,1 ans). Une cupule a été révisée pour descellement aseptique et une autre a été reprise pour un débricolage de l’insert en polyéthylène. Le score HHS moyen a été amélioré passant de 34 à 79. Les résultats ont été cotés comme excellents dans 16 hanches, bons dans 28 hanches, moyens dans 6 hanches et mauvais dans 3 hanches. L’analyse radiographique a montré une amélioration du centrage de la hanche, 49 implants sont considérés comme bien en place et bien fixés, 4 hanches ont une fixation fibreuse mais stable. Cet implant facilite les reconstructions difficiles lorsqu’il existe une perte de substance supérieure et latérale du cotyle sans qu’il soit nécessaire de greffer les patients par une allogreffe. Il permet d’avoir de bons résultats et montre une stabilité tout à fait satisfaisante à moyen terme.
Introduction
Reconstruction of the acetabulum in patients with significant acetabular bone deficiency remains a major challenge in revision total hip arthroplasty (THA). Among the available options for acetabular reconstruction, several published studies suggest that standard hemispherical uncemented acetabular components are appropriate for the majority of acetabular revisions and clearly improve the success rate of revision surgery [2, 11, 14, 15].
In many cases of acetabular revisions, however, the socket has a prevalent superior migration with large superior segmental bone deficiencies. In these cases, a standard hemispheric cementless component cannot be placed solely on native bone at the normal hip centre. Under these circumstances, traditional treatment options for reconstruction include: structural bone grafting with acetabular reconstruction at an anatomical hip centre [13, 17], acetabular reconstruction at a superiorly positioned high hip centre [4] or, when the defect allows, conversion of the oblong defect to a larger hemispheric defect followed by placement of extra-large or “jumbo” uncemented hemispherical acetabular components [16, 21]. In these large superior segmental bone deficiencies, the acetabulum presents with a longitudinal diameter that is greater than its transverse diameter. As such, an oblong cup rather than an hemispherical cup should adapt better to the pre-existing bone defect without further sacrifice of residual bone.
The purpose of this paper was to evaluate the five to ten year results associated with the use of an oblong revision cup – designed with its longitudinal diameter elongated relative to its transverse diameter – for acetabular revisions in the presence of bone loss.
Materials and methods
Sixty-two hips in 60 patients had an acetabular revision with insertion of a LOR acetabular component (Sulzer Medica, Winterthur, Switzerland; now Zimmer, Warsaw, Ind.) from June 1996 to November 2001. All operations were performed by the senior author (MIG).
During the period of the study, two patients (two hips) died from causes not related to the hip procedure. At their deaths, they had been followed up for an average of 4.8 years, and neither patient had required revision; both had satisfactory fixation of the acetabular component, as determined on radiographs made within 1 year prior to their deaths. Five patients (five hips) were lost to follow-up at an average of 5.3 years (range:1–5 years) after the operation. These patients had no radiographic evidence of loosening at the time of their last follow-up.
The remaining 55 hips (53 patients) were available for inclusion in the study after a minimum follow-up of 5 years. The average length of the follow-up was 7.2 years (range: 5.0–10.1 years). Twenty-four of the patients were men (24 hips) and 29 were women (31 hips). The mean age of the patients at the time of the index revision surgery was 50 years (range: 25–77 years). The average time between the previous surgery and the index revision was 6 years (range: 1–10 years). Revision with the LOR cup was the first revision in 37 of the 55 hips, the second revision in 11 hips, the third revision in five hips and the fourth revision in two hips.
The Paprosky system was used to classify all of the acetabular defects on the basis of preoperative and intraoperative assessments [16]. According to this classification, nine cases were type 1, 12 cases were type 2a, 21 cases were type 2b, four cases were type 2c and nine cases were type 3a.
The LOR cup component consists of a shell of pure titanium with a coarse blasted surface. It has an oblong shape with the supero-inferior dimension greater than the antero-posterior dimension. In the transverse axis, this cup looks like an hemisphere without the pole segment; in the longitudinal axis, the hemisphere is elongated by 6–12 mm. Consequently, each size category of LOR shell (52, 56, 60, 64, 68, 72 mm) has a 6-mm and 12-mm augmented longitudinal diameter version. Two rows of holes are arranged parallel to the outer rim of the shell to take the titanium screws. The LOR cup is equipped with an ultra-high-molecular-weight polyethylene liner which is available, in the longer socket, with the centre of rotation central or 6 mm caudally displaced. The other characteristics of the implant have been described in detail elsewhere [12].
All revisions were carried out using a direct lateral approach with the patients in the supine position [7]. The operation was combined with an extended trochanteric osteotomy in three cases when this was required for revision of the femoral component. Concomitant femoral component revision was performed in 38 hips (69.1%).
After removal of the acetabular component, the cement, when present, and the pseudomembrane at the bone-implant interface were removed. The acetabulum was reamed with sequentially standard hemispherical reamers until an adequate oblong bony bed was created for insertion of the revision component. Care was taken to avoid damage to the anterior and posterior column. A trial component was used to check implant stability.
Non-structural allografts were used in all cases. In the last 16 cases, we used allografts augmented with demineralised bone matrix. The morselised graft material was packed into the acetabular defect and shaped using an acetabular reamer in the reverse mode. The final cup was positioned in the acetabulum with a specialised T-shaped impactor which enables full control of the desired orientation of the socket.
In 34 (61.8%) cases we used the 6-mm elongated component and in 21 (38.2%) cases we used the 12-mm elongated component. Of these, in nine cases we used a polyethylene liner with the articular surface distally displaced to restore the physiological centre of rotation.
Although all components were considered to be rigidly fixed at the time of the index revision, we always used screws as supplementary fixation. The average number of screws was 3.2 (range: 2–5). In only nine cases did we limit fixation of the screws to the cranial area in the iliac bone; in all the remaining cases we always added a screw caudally in the ischial bone.
The patients were evaluated clinically using the Harris hip rating system before the index revision and at the time of the most recent follow-up. An Harris hip score of 90–100 points is considered to be an excellent result, with 80–89 points being a good result, 70–79 points a fair result and less than 70 points a poor result [8].
A-P and lateral radiographs were made pre-operatively and at each follow-up examination. The features measured and analysed from these radiographs were: radiolucent lines, position and migration of the component and incorporation of the allografts. Radiographs taken in the immediate postoperative period and at the most recent follow-up were assessed for the presence of radiolucent or radiodense (condensation) lines around the acetabular component according to the three zones defined by DeLee and Charnley [6]. Radiolucencies greater than 1 mm in width in any portion of a zone were considered to be significant. A radiolucency was defined as complete if it was greater than 1 mm in width in all three zones. An acetabular component was considered to be probably loose when a continuous radiolucent or radiodense line of more than 1 mm in width was present around the entire porous coated region of the component.
The measurement of migration of the acetabular component and the preoperative and postoperative centres of hip rotation were estimated by measuring the position of the implant with respect to fixed pelvic landmarks. Two reference lines were drawn: one horizontal reference line between the inferior margins of the teardrops was used to evaluate vertical position and migration, and a perpendicular line tangential to the medial aspect of tear drop was drawn to measure medial position and migration [15]. The cup abduction angle was measured between the lateral opening of the cup and the horizontal interteardrop reference line. A linear change greater than 3 mm or a rotational change greater than 5° was considered to indicate component migration.
Bone graft material was considered to be incorporated if the radiographs showed evidence of trabecular bridging between the graft and host bone.
Results
The most common complication was dislocation, which occurred in three patients. All of these patients were treated successfully with closed reduction and cast immobilisation. One patient developed a transient femoral neuropraxia, which had resolved by the 1-year follow-up. Three of the 55 acetabular components were re-revised. One socket was revised for aseptic loosening after 5 years, and the other one was revised for infection, which developed 15 months after the index procedure.
One cup was operated on for a polyethylene liner dissociation, which occurred 5 months after surgery and was included in the final follow-up clinical and radiological evaluation.
Two additional hips were revised for aseptic loosening of the femoral stems; in both cases the acetabular component was well fixed.
Clinical results were available for the 53 hips that did not have revisions of the acetabular components with a minimum of 5 years of follow-up. At the latest follow-up examination the average Harris hip score improved from 34 pre-operatively to 79. Results were rated as excellent in 16 hips, good in 28, fair in six and poor in three.
Before revision, the hip centre was a mean of 38 mm (range: 17–67 mm) proximal to the interteardrop line. After revision, it was a mean of 22 mm (range: 10–48 mm) proximal to the interteardrop line. Before revision, the centre of hip rotation was a mean of 22 mm lateral to the medial aspect of the teardrop. After revision, it was a mean of 43 mm lateral to the same landmark. One socket (1.9%) showed radiological signs of migration in the first year, subsequently the implant stabilised and did not show any progressive migration; this was a case in which no caudal screws were applied.
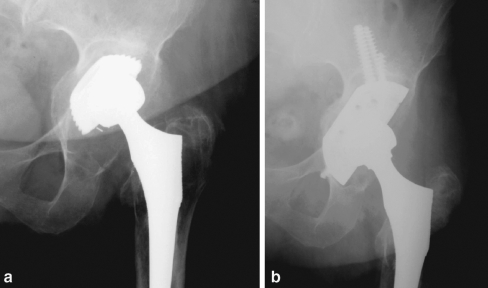
Of the 53 hips with complete radiographic follow-up, 49 (92.5%) had a well-fixed, bone-ingrown cup at the time of the last follow-up (Fig. 1). Four hips had a stable fibrous union, without migration of the cup or associated symptoms.
Fig. 1.
a Preoperative AP radiograph of a 68-years-old female with a large and oblong acetabular defect 5 years after a cementless primary total hip arthroplasty. b AP radiograph made 7 years after surgery
Radiolucent lines were present in seven sockets in one or more than one zone, but these were non-progressive and less than 2 mm in width.
We had a complete incorporation of the morselised bone grafts in 48 cases (90.6%) and a partial resorption was recorded in five cases (9.4%).
Discussion
Numerous studies have documented the results of cementless acetabular reconstruction in the setting of revision THA, demonstrating that excellent results can be obtained even in the severely compromised acetabulum [2, 11, 15]. However, when a superior migration of the failed implants creates an oblong rather then hemispherical defect, an uncemented socket can be used, although modifications in the standard technique are usually required. The main acetabular reconstruction techniques consist of: (1) placement of an acetabular component on the host bone in a superior position (a high hip centre) [17]; (2) placement of an acetabular component in combination with structural bone grafts [10, 20]; (3) placement of an extra-large, “Jumbo” acetabular component [4, 21].
Oversized “jumbo” components are very popular; however, in the situations described they may require additional bone sacrifice to fit a hemispherical component, and large, oblong bone deficiencies cannot be filled in an inferior-to-superior direction without marked reaming of the anterior or posterior column, with subsequent potential compromise of bone stock. According to the Paprosky classification, a prevalent superior migration is present in type 2a, 2b and 3a defects, and in most of the THA series reported these three defects account for the majority of acetabular revisions [18]. For this reason, oblong acetabular components were introduced for management of large superior acetabular defects. Their theoretical advantages include avoidance of the high hip centre and the use of bulk allograft for support. They are designed to maintain contact with the host bone and to restore a more anatomical hip centre. While oblong acetabular components are commonly believed to replace “bone with metal”, in many instances they limit the sacrifice of bone stock compared to oversized hemispherical components.
Several reports on the use of uncemented oblong implants for acetabular bone deficiencies have been published. Conflicting results have been reported with the use of bilobed components; however, we believe that the underlying strategy of the bilobed components differs completely from that of the LOR cups and that the results of experiments on the former are not comparable with our results [1, 3, 5]. When the same oblong cementless acetabular component was used, the results were generally satisfactory.
In the first peer-review study, Köster et al. reported on 102 hips (98 revisions) treated with the LOR uncemented oblong socket. Of these 102 hips, only two required re-operation for aseptic loosening. Eight other hips had migration, but in all of these hips the migration was 5 mm or less, and none had failed clinically [12]. More recently, using the same implant, Surace et al. reported on 40 acetabular revisions that were followed up for 40–99 months (mean: 63.5 months) after surgery. These researchers reported excellent clinical results, with no cases of implant migration and no revision operations [19]. Herrera et al. reviewed 35 acetabular revisions with the LOR cup that were followed up for 4–8 years (mean: 6.3 years). At the latest follow-up, the results were satisfactory even though five migrations had occurred with incomplete cup contact with the acetabular rim [9].
Our series shows that an oblong uncemented acetabular component has several advantages when used in the reconstruction of a large superior segmental acetabular bone deficiency. In this series of 55 LOR acetabular components that were followed for an average of 7.2 years, this cementless acetabular component was associated with a low rate of revision for aseptic loosening (1.9%) and predictable results with respect to clinical pain and function.
In our experience, the ideal indication for the use of this cup is acetabular revisions with bone defects of type 2a, 2b, and 3a according to the Paprosky classification where the longitudinal diameter of the defect is longer then its transverse diameter. We were able to achieve a good primary stability in most of the cases, but supplementary fixation of the screws is mandatory for the stability of the implant and to allow for allograft incorporation. However, in our experience screws should not be limited to iliac bone, instead, a caudal screw in ischium should be always added.
In conclusion, our five to ten year results are encouraging in that only one cup was revised for aseptic loosening and we had only one other migration of the component. The acetabular bone deficiencies were reconstructed in all patients without the need for bulk structural acetabular bone grafts, and in all patients, due to the geometry of the cup and the option of two PE liners, the hip centre was brought to a more normal position.
References
- 1.Berry DJ, Sutherland CJ, Trousdale RT, Colwell CW Jr, Chandler HP, Hayres D, Yashar AA (2000) Bilobed oblong porous coated acetabular components in revision total hip arthroplasty. Clin Orthop 371:154–160 [DOI] [PubMed]
- 2.Chareancholvanich K, Tanchuling A, Seki T, Gustilo RB (1999) Cementless acetabular revision for aseptic failure of cemented hip arthroplasty. Clin Orthop 361:140–149 [DOI] [PubMed]
- 3.Chen WM, Engh CA Jr, Hopper RH, McAuley JP, Engh CA (2000) Acetabular revision with use of a bilobed component inserted without cement in patients who have acetabular bone-stock deficiency. J Bone Joint Surg Am 82-A:197–206 [DOI] [PubMed]
- 4.Dearborn JT, Harris WH (2000) Acetabular revision arthroplasty using so-called jumbo cementless components: an average 7-year follow-up study. J Arthroplasty 15:8–15 [DOI] [PubMed]
- 5.DeBoer DK, Christie MJ (1998) Reconstruction of the deficient acetabulum with an oblong prosthesis: three-to seven-year results. J Arthroplasty 13:674–680 [DOI] [PubMed]
- 6.De Lee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 121:20–32 [PubMed]
- 7.Hardinge K (1982) The direct lateral approach to the hip. J Bone Joint Surg 64-B(1):17–19 [DOI] [PubMed]
- 8.Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone Joint Surg 51A:737–755 [PubMed]
- 9.Herrera A, Martinez AA, Cuenca J, Canales V (2006) Management of types III and IV acetabular deficiencies with the longitudinal oblong revision cup. J Arthroplasty 21:857–864 [DOI] [PubMed]
- 10.Jasty M, Harris WH (1990) Salvage total hip reconstruction in patients with major acetabular bone deficiency using structural femoral head allografts. J Bone Joint Surg 72B:63–67 [DOI] [PubMed]
- 11.Jones CP, Lachiewicz PF (2004) Factors influencing the longer-term survival of uncemented acetabular components used in total hip revisions. J Bone Joint Surg Am 86-A:342–347 [DOI] [PubMed]
- 12.Köster G, Willert H-G, Köhler H-P, Döpkens K (1998) An oblong revision cup for large acetabular defects: design rationale and two- to seven-year follow-up. J Arthroplasty 13:559–569 [DOI] [PubMed]
- 13.Lee BP, Cabanela ME, Wallrichs SL, Ilstrup DM (1997) Bone-graft augmentation for acetabular deficiencies in total hip arthroplasty. J Arthroplasty 12:503–510 [DOI] [PubMed]
- 14.Leopold SS, Rosenberg AG, Bhatt RD, Sheinkop MB, Quigley LR, Galante JO (1999) Cementless acetabular revision: evaluation at an average of 10.5 years. Clin Orthop 369:179–186 [DOI] [PubMed]
- 15.Padgett DE, Kull L, Rosenberg A, Sumner DR, Galante JO (1993) Revision of the acetabular component without cement after total hip arthroplasty. J Bone Joint Surg 75A:663–673 [DOI] [PubMed]
- 16.Paprosky WG, Perona PG, Lawrence JM (1994) Acetabular defect classification and surgical reconstruction in revision arthroplasty: a 6 year follow-up evaluation. J Arthroplasty 9:33–44 [DOI] [PubMed]
- 17.Schutzer SF, Harris WH (1994) High placement of porous-coated acetabular components in complex total hip arthroplasty. J Arthroplasty 9:359–367 [DOI] [PubMed]
- 18.Sporer SM, Paprosky WG (2006) Acetabular revision using a trabecular metal acetabular component for severe acetabular bone loss associated with a pelvic discontinuity. J Arthroplasty 21:87–90 [DOI] [PubMed]
- 19.Surace MF, Zatti G, De Pietri M, Cherubino P (2006) Acetabular revision surgery with the LOR cup. Three to 8 years’ follow-up. J Arthroplasty 21:114–121 [DOI] [PubMed]
- 20.Traina F, Giardina F, De Clerico M, Toni A (2005) Structural allograft and primary press-fit cup for severe acetabular deficiency. A minimum 6-year follow-up study. Int Orthop 29:135–139 [DOI] [PMC free article] [PubMed]
- 21.Whaley AL, Berry DJ, Harmsen WS (2001) Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg 83A:1352–1357 [DOI] [PubMed]