Abstract
Cementless total hip arthroplasty has achieved reliable long-term results since porous coatings were developed, but postoperative changes around the stem remain poorly documented. In this study, changes of the bone mineral density (BMD) were compared between two types of cementless stem. In group B (28 patients with 31 hips), a straight tapered stem with porous plasma spray coating on the proximal 1/4 was used, while group S (24 patients with 26 hips) was given a fluted, tri-slot stem with porous hydroxyapatite coating on the proximal 1/3. In group B, there was an early decrease of BMD, which recovered after 12 months, indicating that stress shielding was minimal. In group S, however, BMD continued to decrease without recovery. The stem shape and radiological findings suggested that the cause of stress shielding in group S was distal fixation.
Résumé
Les prothèses totales de hanche sans ciment ont de bons résultats à long terme, notamment depuis qu’ont été développées les techniques de revêtement poreux, mais les modifications post opératoires autour de la pièce fémorale, ont été jusqu’à présent peu documentées. Dans cette étude, nous avons souhaité étudier les modifications de la densité osseuse (BMD) en comparant deux types de prothèses sans ciment. Dans le groupe B (28 patients, 31 hanches) une pièce fémorale droite avec un plasma spray proximal pour le groupe S (24 patients, 26 hanches) la pièces fémorale a été recouverte d’hydroxyapatite sur le tiers proximal. Les patients du groupe B ont présenté une diminution précoce de la BMD indiquant un stress shielding minime et dans le groupe S, la BMD diminue sans récupération alors que cette BMB réaugmente dans le groupe B. Ceci nous indique que la cause du stress shielding dans le groupe S est secondaire à la fixation distale.
Introduction
Cemented total hip arthroplasty (THA) was developed by Sir John Charnley [3], and it achieves reliable results. However, problems such as the toxicity of bone cement, tissue destruction by heat during polymerisation, and various technical difficulties have been noted. The alternative is cementless THA using stems with a porous coating that allows bone ingrowth to achieve rigid fixation, and these stems have been shown to survive for over 10 years. However, the problems of osteolysis due to polyethylene wear particles and bone atrophy because of stress shielding mean that the long-term stability of uncemented THA is still in question [7, 14, 24]. The length, design, composition, and elasticity of a stem, as well as the extent of its porous coating, have all been pointed out as factors that influence stress shielding postoperatively [1, 2, 11]. Bone mineral density (BMD) can be measured with a high degree of accuracy by the use of dual-energy X-ray absorptiometry (DEXA) [13, 25]. In this study, two stems with different shapes and coatings were compared to assess the changes of radiographic findings and BMD after THA.
Materials and methods
Group B underwent THA with a Biomet prosthesis (Warsaw, Indiana, USA) that had a modular head and porous coating on the proximal 1/4 of the stem (a straight tapered Bimetric stem), while group S underwent THA with a Stryker prosthesis (Fairfield Rd, Kalamazoo, USA) that had a modular head and a fluted Tri-slot, Secure-Fit plus stem with porous hydroxyapatite (HA) coating over the proximal 1/3. The Biomet prosthesis was used from January 1996 to December 1999 and the Stryker prosthesis was employed from January 2000 to April 2003. Two distal stem sizes were available, but there was only one size for the proximal part of the implant (Fig. 1).
Fig. 1.
Prostheses used for THA
The subjects were 62 patients (65 hips) in whom surgery was performed at least two years before the present study. Group B comprised 28 patients (26 women and two men with 31 hips) who had osteoarthritis of the hip joint (27 hips) or osteonecrosis of the femoral head (four hips). Their mean age at the time of operation was 62.7 years (range: 41–80 years), and the mean postoperative follow-up period was 52 months. Group S included 24 patients (23 women and one man with 24 hips) who had osteoarthritis of the hip joint (22 hips) or osteonecrosis of the femoral head (four hips), with a mean age of 64.0 years (range: 51–83 years) at the time of operation and a mean postoperative follow-up period of 34 months.
The posterior approach was used in all patients and a cementless porous acetabular cup was inserted in both groups. Partial weight bearing was allowed one week after the operation, with full weight bearing after 3 weeks. The Harris hip score [9] was used to evaluate the clinical outcome. BMD was measured by DEXA using an XR-36 device (Norland Inc. Cranbury, USA). Patients were placed in the hip scanning position, with the hip joint in 0° of extension, 0° of internal or external rotation, and slight abduction. The region around the stem was divided into seven Gruen zones [8]. DEXA was initially performed less than one month postoperatively, as well as after six months, 12 months, 18 months, and 24 months, and then annually. Using the value obtained within one month of surgery as the baseline, the BMD ratio was calculated at each time of measurement. Loosening and periprosthetic X-ray changes were also compared.
Results
Harris hip score
The clinical outcome was evaluated from the Harris hip score. In group B, the score improved from 33.2 preoperatively to 90.7 postoperatively, while the score for group S improved from 35.3 to 91.4. Improvement of pain was significant, with the pain score increasing from 13.8 to 41.2 in group B and from 13.8 to 41.2 in group S. Both groups showed an excellent clinical outcome.
Radiological changes
At the final radiological examination, there was no loosening, sinking, or osteolysis in either group. Spot welds were found in 65% of group B and 100% of group S. Six hips (19%) from group B and eight hips (31%) from group S showed first-degree stress shielding in zones 1 and 7. Cortical hypertrophy was seen in zones 2, 3, and 5 of 3%, 0%, and 10% of group B hips, respectively, versus 15%, 4%, and 15% of group S hips. Radiolucent zones were less than 1 mm wide in all cases, but were found in zones 3, 4, and 5 of 13%, 22%, and 10% of group B hips, respectively, versus 12%, 31%, and 15% of group S hips, respectively.
BMD
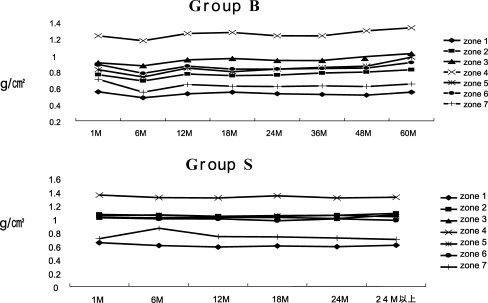
The BMD around the stem was assessed within one month postoperatively, as well as after six, 12, 18, and 24 months, and then annually. In group B, there was a decrease of BMD in all zones at six months postoperatively, but the BMD recovered to baseline by 12 months and then remained stable or increased further. BMD was highest in zone 4, lowest in zone 7, and second lowest in zone 1. In group S, there was no decrease of BMD within six months of the operation, but a gradual decline occurred subsequently in zones 1 and 7. Similar to group B, the highest BMD was in zone 4, the lowest was in zone 7, and the second lowest was in zone 1 (Fig. 2).
Fig. 2.
Changes of BMD
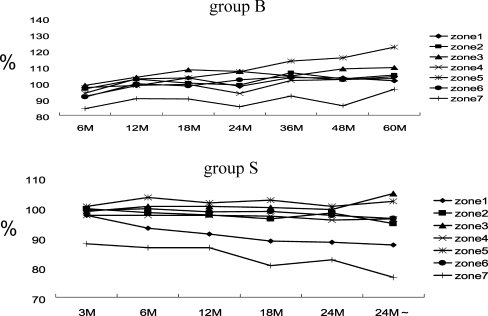
BMD ratio
When the BMD measured within one month of the operation was taken as 100% to calculate BMD ratios, all zones showed a decline of the BMD ratio below 100% at six months postoperatively in group B, after which the BMD ratio increased to exceed 100% at 36 months and remained above 100% until 60 months in all zones (except zone 7). These results suggested good proximal fixation of the stem. In group S, the BMD ratio was approximately 100% for zones 2, 3, 4, 5, and 6 at three months postoperatively. In zones 1 and 7, the BMD ratio decreased slightly after three months (97%) and then declined to 90% by 18 months. In zone 7, the BMD ratio decreased below 90% after 3 months and then declined below 80% after 24 months. From the radiological findings, it was concluded that this decline of the BMD ratio was caused by stress shielding around the proximal stem (Fig. 3).
Fig. 3.
Changes of BMD ratio
In group B, nine hips were in patients over 70 years old, and 22 hips were in younger patients. In group S, the respective numbers were nine and 17 hips. Based on comparison of the two age groups, the BMD showed a decrease as the age increased, but there was no significant trend of the BMD ratio. We also categorised the hips on the basis of the medullary cavity stem occupation ratio (above or below 90% on frontal X-ray films), but there were no significant differences of the BMD ratio between these subgroups in either group B or group S.
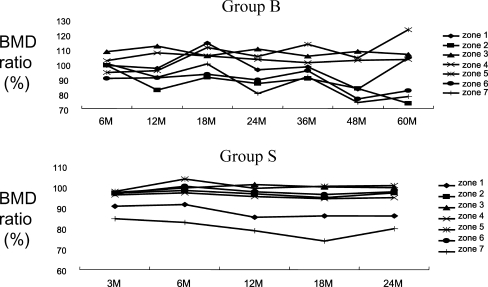
Stress shielding
First-degree stress shielding was found in zones 1 and 7 of six hips from group B and eight hips from group S. In the hips of group B, the BMD ratio was greater than 100% in zones 3, 4, and 5, and it increased distally, while the ratio was less than 100% in zones 1, 2, 6, and 7, so that it decreased proximally. In the hips of group S, the BMD ratio was 100% in zones 2, 3, 4, 5, and 6, but it was only 90% in zones 1 and 7 and continued to decline over time, presumably due to stress shielding (Fig. 4).
Fig. 4.
Changes of the BMD ratio with stress shielding cases
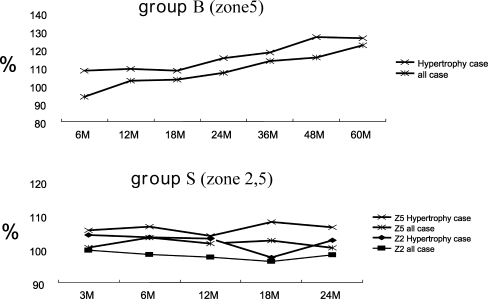
Cortical hypertrophy
In group B, two hips showed cortical hypertrophy in zone 5. The BMD ratio data suggested that this cortical hypertrophy was caused by continuous stress in zone 5. In group S, eight cases of hypertrophy were found (affecting zones 2 and 5 in four hips). Because the BMD ratio remained high in the other zones over time, the stem design was assumed to be the cause of continuous stress in these zones (Fig. 5).
Fig. 5.
Changes of the BMD ratio with cortical hypertrophy
Hips with a BMD ratio <100% in all zones
Two hips in group B and six hips in group S had a BMD ratio < 100% in all zones for more than 24 months. There was no significant correlation between the low BMD ratio and the age, the stem occupation ratio of the medullary cavity, or the condition of the opposite hip. Calculation of Noble’s canal flare index showed that four hips had a champagne flute canal in group B, as did eight hips in group S, while the rest were normal (no hip had a stovepipe canal). In group S, four of the six hips with low BMD ratios had a champagne flute canal and it was assumed that distal fixation of the stem had occurred (Table 1).
Table 1.
Patients with a BMD ratio <100% in all zones for more than 2 years
| Patient | Group | Opposite side | Stem/canal filling ratio (%) | Pedestal formation | CFI (Noble) |
|---|---|---|---|---|---|
| 66 F | B | OA | 79 | + | 3.90 |
| 67 F | B | THA | 92 | + | 4.11 |
| 63 M | S | Normal | 92 | − | 4.18 |
| 73 F | S | Normal | 90 | − | 5.00 |
| 77 F | S | Normal | 85 | − | 5.15 |
| 59 F | S | Normal | 100 | + | 5.50 |
| 69 F | S | THA | 85 | + | 3.46 |
| 70 F | S | Normal | 100 | − | 6.50 |
Discussion
Cemented THA was developed by Charnley and achieves good results, but problems with the technique (such as tissue destruction by heat during polymerisation or intraoperative hypotension) prompted the development of cementless THA. Initially, cementless THA only achieves moderate stability, but there is no consensus about the optimum stem shape and coating to improve stability, so various types have been produced. We did not use a stem with a collar because bone loss occurs around the collar over time after surgery. With regard to the extent of coating on the stem, moderate stability has been reported to be achieved with fully coated stems such as the AML, but other studies have found no significant association between stability and the extent of coating on the proximal stem [23]. However, there have been reports about the frequent occurrence of stress shielding [5, 10] as well as the difficulty of removing the fully coated stems at re-operation. Niinimaki [17] claimed that the design of the stem has an effect on bone remodelling by allowing the loading of the bone as proximally as possible, and long stiff stems should be avoided. Since sufficient stability can be achieved by a proximal porous coating, we selected two proximally porous coated stems for our patients. A decrease of the BMD ratio around the stem after surgery has been reported previously [12, 20]. In this study, we used stems with a porous coating of the proximal 1/4 and a straight tapered distal part or porous coating of the proximal 1/3 and a fluted, tri-slot distal part, and we compared the changes of radiological findings and BMD between the two groups of patients. The position of the femur is important [4, 27] when measuring BMD by DEXA, so we adopted the neutral position. Our study showed that the BMD ratio decreased in all zones until six months after surgery in group B and then improved subsequently.
Similar results have already been reported and this initial temporary decline of BMD is thought to be caused by the impact of surgery and a decrease of activity during convalescence [6]. However, group S showed no such early decline of the BMD ratio. In both groups, the BMD ratio was highest in zone 4, lowest in zone 1, and second lowest in zone 7. The impact of surgery and the decrease of activity during convalescence were similar in both groups, but the HA-coated, tri-slot stem with distal fluting showed better initial fixation. In group B, the BMD ratio recovered after six months in all zones and exceeded 100% after 36 months (except in zone 7). There was less pain and increased activity after surgery, with improvement of the medullary BMD ratio. In group S, the BMD ratio of zones 3 and 5 returned to 100% by 12 months after surgery and then continued to increase, but it decreased in the other zones. In particular, zone 1 showed a decline of more than 10% at two years postoperatively and the decrease exceeded 20% in zone 7. These findings were similar to the BMD changes noted in zones 1 and 7 at 12 months postoperatively by Nishii [18], which were a decrease of 23% for zone 1 and 18% for zone 7, while Wixson [28] found a decrease of 5% in zone 1 and 12% in zone 7 after 24 months. A difference in the pattern of BMD changes between various stem types has already been reported [11, 23], as well as the difference of BMD changes among the different types of implants which are due to variations in stress transmission [19]. In group B, the stem continuously transmitted weight from the site of proximal fixation. In group S, early bone formation around the HA-coated proximal 1/3 of the stem apparently achieved good initial fixation. However, the stem also gradually became fixed distally, causing proximal stress shielding that led to the decline of BMD around the proximal stem. Schmidt [21, 22] described the periprosthetic bone remodelling of non-cemented taper-design stem and their study showed that loss of femoral BMD in THA is not necessarily progressive, and a full or at least partial restoration of baseline values around the implant may occur within the first three years after operation with tapered stems. Also, both the wide taper angle of the stem as well as the reduced length led to a favourable load transfer in the proximal femoral area, resulting in less pronounced bone resorption. In our study, a decrease of the proximal BMD was smaller in the taper design.
In the hips with stress shielding, the BMD ratio exceeded 100% in zones 3, 4, and 5, but it decreased below 100% in the proximal zones 1, 2, 6, and 7. In group S, thickening of cortical bone was seen in zones 2 and 5 of four hips, suggesting the possibility of the cylindrical stem becoming fixed distally. The site of distal fixation is associated with thicker bone, and the more the rigidity of the stem exceeds that of the femur, the greater stress shielding becomes [15, 16, 26]. Therefore, our data suggest that the tri-slot stem is extremely rigid. Thickening of cortical bone was also found in zone 5 of two hips from group B, suggesting that the tapered stem could sometimes also be associated with distal fixation.
Conclusion
In this study, BMD changes (measured by DEXA) were compared between two types of cementless stem. There was no loosening in either group. Both stems showed good proximal fixation, but there were differences in the pattern of BMD changes. We conclude that the HA-coated, tri-slot stem with distal fluting shows good initial stability, but it gradually becomes fixed distally, causing proximal stress shielding.
References
- 1.Bobyn JD, Glassman AH, Goto H, Krygier JJ, Miller JE, Brooks CE (1990) The effect of stem stiffness on femoral bone resorption after canine porous-coated total hip arthroplasty. Clin Orthop 261:196–213 [PubMed]
- 2.Bobyn JD, Mortimer ES, Glassman AH, Engh CA, Miller JE, Brooks CE (1992) Producing and avoiding stress shielding. Laboratory and clinical observations of noncemented total hip arthroplasty. Clin Orthop 274:79–96 [PubMed]
- 3.Charnley J, Cupic Z (1973) The nine- and ten-year results of the low-friction arthroplasty of the hip. Clin Orthop 95:9–25 [PubMed]
- 4.Cohen B, Rushton N (1995) Accuracy of DEXA measurement of bone mineral density after total hip arthroplasty. J Bone Joint Surg 77B:479–483 [PubMed]
- 5.Engh CA, Bobyn JD (1988) The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop 231:7–28 [PubMed]
- 6.Frost HM (1973) The origin and nature of transients in human bone remodeling dynamics. In: Frame B, Parfitt, AM, Duncan H (eds) Clinical aspects of metabolic bone disease. Excerpta Medica, Amsterdam, pp 124–137
- 7.Graeter JH, Nevins R (1998) Early osteolysis with Hylamer acetabular liners. J Arthroplasty 13:464–466 [DOI] [PubMed]
- 8.Gruen TA, McNeice GM, Amstutz HC (1979) Modes of failure of cemented stem-type femoral components. Clin Orthop 141:17–27 [PubMed]
- 9.Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone Joint Surg 51A:737–755 [PubMed]
- 10.Huiskes R (1990) The various stress patterns of press-fit, ingrown, and cemented femoral stems. Clin Orthop 261:27–36 [PubMed]
- 11.Kilgus DJ, Shimaoka EE, Tipton JS, Eberle RW (1996) Dual-energy X-ray absorptiometry measurement of bone mineral density around porous-coated cementless femoral implants. J Bone Joint Surg 75B:279–287 [DOI] [PubMed]
- 12.Kiratli BJ, Checovich MM, Mcbeath AA, Wilson MA (1996) Measurement of bone mineral density by dual-energy X-ray absorptiometry in patients with the Wisconsin hip, an uncemented femoral stem. J Arthroplasty 11:184–193 [DOI] [PubMed]
- 13.Kroger H, Miettinen H, Arnala I, Koski E, Rushton N, Suomalainen O (1996) Evaluation of periprosthetic bone using dual-energy X-ray absorptiometry: precision of the method and effect of operation on bone mineral density. J Bone Miner Res 11:1526–1530 [DOI] [PubMed]
- 14.Manley MT, D’Antonio JA, Capello WN, Edidin AA (2002) Osteolysis: a disease of access to fixation interfaces. Clin Orthop 405:129–137 [DOI] [PubMed]
- 15.McCarthy CK, Steinberg GG, Agren M, Leahey D, Wyman E, Baran DT (1991) Quantifying bone loss from the proximal femur after total hip arthroplasty. J Bone Joint Surg 73B:774–778 [DOI] [PubMed]
- 16.Nakamura Y, Katano H, Kudo Y, Okada H, Hirakawa H, Matutani K, Matumoto K (1994) A clinical study of AML cementless femoral stem. J Joint Surg Jpn 13:1075–1081
- 17.Niinimaki T, Junila J, Jalovaara P (2001) A proximal fixed anatomic femoral stem reduces stress shielding. Int Orthop 25:85–88 [DOI] [PMC free article] [PubMed]
- 18.Nishii T, Sugano N, Masuhara K (1997) Longitudinal evaluation of time related bone remodeling after cementless total hip arthroplasty. Clin Orthop 339:123–131 [DOI] [PubMed]
- 19.Richmond BJ, Bauer TW, Stulberg BN (1990) Bone mineral density in patients undergoing uncemented total hip arthroplasty. Calcif Tissue Int 46:145
- 20.Rosenthall L, Bobyn JD, Brooks CE (1999) Temporal changes of periprosthetic bone density in patients with a modular noncemented femoral prosthesis. J Arthroplasty 14:71–76 [DOI] [PubMed]
- 21.Schmidt R, Muller L, Nowak TE, Pitto RP (2003) Clinical outcome and periprosthetic bone remodeling of an uncemented femoral component with taper design. Int Orthop 27:204–207 [DOI] [PMC free article] [PubMed]
- 22.Schmidt R, Nowak TE, Muller L, Pitto RP (2004) Osteodensitometry after total hip replacement with uncemented taper-design stem. Int Orthop 28:74–77 [DOI] [PMC free article] [PubMed]
- 23.Skinner HB, Kim AS, Keyak JH, Keyak JH, Mote CD (1994) Femoral prosthesis induces changes in bone stress that depend on the extent of porous coating. J Orthop Res 12:553–563 [DOI] [PubMed]
- 24.Sochart D (1999) Relationship of acetabular wear to osteolysis and loosening in total hip arthroplasty. Clin Orthop 363:135–150 [PubMed]
- 25.Spittlehouse AJ, Smith TW, Eastell R (1998) Bone loss around two different types of hip prostheses. J Arthroplasty 13:422–427 [DOI] [PubMed]
- 26.Tunner TM, Sumner DR, Urban RM, Igroria R, Galante JO (1997) Maintenance of proximal cortical bone with use of a less stiff femoral component in hemiarthroplasty of the hip without cement. J Bone Joint Surg 79A:1381–1390 [DOI] [PubMed]
- 27.Wilson CR, Fogelman I, Blake GM, Rodin A (1991) The effect of positioning on dual-energy X-ray bone densitometry of the proximal femur. Bone Miner 13:69–76 [DOI] [PubMed]
- 28.Wixson RL, Stulberg D, Van Flandern GJ, Puri L (1997) Maintenance of proximal bone mass with an uncemented femoral stem: analysis with dual-energy X-ray absorptiometry. J Arthroplasty 12:365–372 [DOI] [PubMed]