Abstract
Ankle replacements appear to offer a good alternative to fusion for most arthritic conditions. Use of mobile bearings has significantly improved results of ankle replacement. Ankle replacements still have a significant minor-complication rate which does not seem to affect the long-term outcome. Medial impingement as a complication has been reported with popular designs. We reviewed the senior author’s first five years of Buechel-Pappas ankle replacements looking at AOFAS scores, VAS scores, patient satisfaction, learning curve of the surgeon and complications. Eight patients out of a total of 34 reported symptoms of medial impingement at follow-up. Four patients underwent revision surgery for this. Ankle replacements have a significant proportion of minor complications, one of which is medial impingement. Whether this is due to implant design, residual arthritis in medial recess or soft-tissue pathology is uncertain but revision surgery may be required.
Résumé
La prothèse de cheville apparaît comme une solution alternative satisfaisante à l’arthrodèse dans la plupart des arthroses de la cheville. L’utilisation de prothèses à plateaux mobiles a significativement amélioré les résultats de ce type d’arthroplastie. Elles ont toujours un taux de complication minime et ce taux ne semble pas s’aggraver avec la surveillance à long terme. Les conflits internes ont été décrits avec les implants les plus habituels. L’auteur senior de cette publication a revu toutes les prothèses de cheville de type Buechel-Pappas posées lors des cinq premières années et cotées selon le score AOFAS et le score VAS, la satisfaction des patients, la courbe d’apprentissage du chirurgien et les complications. 8 patients sur 34 ont rapporté des signes de conflits internes. 4 patients ont bénéficié d’une révision de la prothèse secondaire à ce conflit interne. Les prothèses de cheville ont une proportion significative de complications minimes, le conflit interne étant secondaire au dessin de l’implant. Les lésions arthrosiques résiduelles et la pathologie des tissus mous environnant peuvent, avec ce conflit interne, nécessiter une reprise chirurgicale.
Introduction
Arthrodesis of the ankle joint gives satisfactory short- and medium-term results; however, in the longer term, it frequently leads to sub-talar and mid-tarsal osteoarthritis which is difficult to treat [3]. The first ankle prostheses in the early 1970s had high failure rates [4]. First- and second-generation ankle replacements had a high rate of failure due to instability and loosening respectively. Third-generation designs incorporate three major improvements: mobile bearing, cementless fixation and minimal bone resection. Use of mobile bearings has significantly improved results of ankle replacement [13]. The Buechel-Pappas™ ankle prosthesis (Endotec, NJ, USA) is a cementless, porous-coated, congruent-contact, mobile-bearing total ankle replacement system. It does not replace malleolar joints. Ankle replacements have a significant complication rate including nerve injury and fractures which have been suggested to be minor complications as they do not seem to affect outcome.
Materials and methods
Thirty-four consecutive total ankle replacements performed by the senior author from October 1999 to May 2004 were reviewed in this study. Mean follow-up was 2.8 years (range: 1–5.5 years). Pre- and post-operative VAS (visual analogue scale) scores and AOFAS (American Orthopaedic Foot and Ankle Society) scores were evaluated to assess patient satisfaction and outcome. Operative notes and radiographs were reviewed to determine intra-operative and post-operative complications. Tourniquet time as recorded in operation notes indicated that there was a learning curve for the procedure.
AOFAS score [6] is the most commonly used scoring system for assessment of ankle problems [7]. VAS is a standard measurement tool in pain research and clinical practice [10]. Patient satisfaction was graded as ‘very happy’(would recommend to others), ‘happy’ ( will not recommend to others, but happy with result), ‘satisfactory’ (much better), ‘unhappy’ ( will consider alternatives next time).
Results
Male-to-female ratio was 1:1.4. Mean age was 65 years (range: 33–83). Indication for surgery was primary osteoarthritis in 13, post-traumatic arthritis in 13 and rheumatoid arthritis in eight. Average VAS score was 8.2 pre-operative and improved to 2.0 at follow-up. AOFAS score improved to 72 from 39.1 (Table 1). Operating time averaged 113 min in 1999 and 85 min in 2004. Significant complications were medial impingement, intra-operative malleolar fractures and nerve injury (Table 2). Five patients had intra-operative malleolar fractures (four medial, one lateral). Only one needed internal fixation and all healed uneventfully in due course. Three patients had injury to cutaneous nerves, which was diagnosed by painful neuromas over the scar, and none had any significant functional disability from this. Three patients had superficial infection which settled with antibiotics, but there were no cases of deep infection. In total, 58% of patients were very happy, 32.5% were happy or satisfactory, 9.5% were unhappy with the result. Two patients had had ankle fusion on the opposite side earlier, both were happier with the replaced side.
Table 1.
AOFAS and VAS scores
| Diagnosis | AOFAS score | VAS score | ||
|---|---|---|---|---|
| Pre-op | Post-op | Pre-op | Post-op | |
| Osteoarthritis | 53.5 | 77.9 | 8.2 | 2.3 |
| Post-traumatic arthritis | 40.2 | 68.1 | 8.1 | 2.5 |
| Rheumatoid arthritis | 34.0 | 70.4 | 8.7 | 2.0 |
| All patients | 39.1 | 72.0 | 8.2 | 2.0 |
Table 2.
Complications
| Diagnosis | Complications | ||
|---|---|---|---|
| Fractures | Nerve injury | Medial impingement | |
| Osteoarthritis (n = 13) | 1 | 1 | 4 |
| Post-traumatic arthritis (n = 13) | 2 | 2 | 3 |
| Rheumatoid arthritis (n = 8) | 2 | 0 | 1 |
| Total (n = 34) | 5 | 3 | 8 |
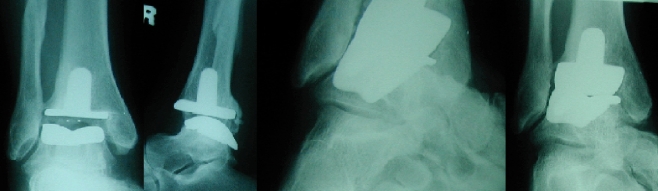
Eight patients reported persistent medial side pain at follow-up. All eight patients had evidence of arthritis in both medial and lateral recesses on follow-up radiographs, but were symptomatic only on the medial side. None of these had an intra-operative fracture or nerve injury. Four of these patients underwent surgery because of the severity of symptoms. One patient underwent arthroscopic debridement of scar tissue and impinging bone which gave good symptomatic relief. Another patient (Fig. 1) had open debridement of impinging bone in the medial malleolar joint. The other two had tibialis posterior tendonitis and underwent surgical decompression. Both were found to have degenerative tears of the tendon. The rest of the patients were treated conservatively. All four patients who had repeat surgery were symptom free at the time of review (minimum of six months follow-up), and the patients who were treated conservatively reported no further progression of symptoms.
Fig. 1.
A 48-year-old female with post-traumatic arthritis, 18 months after ankle replacement (AP, lateral and oblique X-rays) showing significant medial joint arthritis
Discussion
Ankle replacements have a high minor-complication rate. Malleolar fractures have been reported to be a common intra-operative complication of ankle replacements [8]. Literature reports the rate to be up to 20%, and some authors have recommended prophylactic pinning of malleoli as well to prevent this. Most authors feel that undisplaced fractures do not need fixation [15]. Similarly Myerson and Mroczek [9] observed a high rate of intra-operative fractures and tendon/nerve injuries. They found that incidence of complications decreased with surgeon’s experience with the procedure. We had five malleolar fractures of which only one needed fixation as others did not have any effect on the stability of the prosthesis. All fractures were found to be healed at follow-up. None of these patients had any residual medial side pain.
Spirt et al. [14] reported a high reoperation rate (28%) with Agility (DePuy, Warsaw, IN, USA) total ankle replacements and found that 45% patients had heterotopic bone formation which needed debridement. Younger age was found to have a negative effect on the rates of reoperation and failure. This shows that use of implant designs like Agility that replace medial and lateral recesses may not prevent impingement symptoms. Interestingly Buechel and Pappas [2] did not note medial impingement symptoms to be a significant problem in their series.
Rippstein [13] reported that even with significant arthritis in malleolar joints, Buechel-Pappas (BP) prosthesis was an acceptable choice provided impinging osteophytes were removed. He found insertion of the prosthesis much easier technically compared to STAR (Scandinavian Total Ankle Replacement) (Waldemar Link, Hamburg, Germany), especially for talar side resection, which does not require further bony resection. Implant designs like Agility can treat arthritis in medial and lateral gutters by extending the replacement to these joints, but can still cause soft-tissue impingement. Whether prophylactic soft-tissue decompression may offer a solution is also doubtful, but may be useful in patients who have significant medial symptoms before surgery.
Pain relief after ankle replacement may not be absolute. Pyevich et al. [12] reported that only 55% of patients reported no pain from ankle joint at an average follow-up of 4.8 years. In our series, 18% reported no pain (VAS of 0) and another 56% reported only mild pain (VAS of 1 or 2). Nishikawa et al. [11] found that even with poor clinical results, especially in terms of radiological appearance, patients often reported good levels of satisfaction. Their series used an ankle prosthesis which had a medial facet, and with that, no patients had residual medial joint pain.
Rippstein [13] reported medial ankle pain as a complication of both STAR and BP prostheses. This may be caused by the cylindrical shape of the talar component (the physiological talus has a cone shape with a smaller radius on the medial side). This has not been proven yet, but has been addressed in newer designs such as the Salto prosthesis (Tornier SA, France) [1] and Hintegra (Newdeal SA, France) [5]. Both Salto and Hintegra have been designed to improve the anatomical design of bearing surfaces, especially the talus, which is broader anteriorly and has a larger radius of curvature laterally than medially. This improved talar design is aimed at mimicking the physiological motion of the talus. Preliminary results from these prostheses appear encouraging [1, 5].
We believe that all these factors play a role in medial impingement. Some patients do have soft-tissue impingement and this was true in the two who had symptomatic improvement after tibialis posterior decompression. Two patients who had arthroscopic/open decompression had evidence of bony impingement. Pre-existing medial joint arthritis or an intra-operative fracture of the medial malleolus does not appear to predispose to medial impingement. Whether the improved anatomical design of newer prostheses like Salto and Hintegra will prevent medial impingement remains to be seen.
Conclusions
Ankle replacements appear to offer a good alternative to fusion in selected patients. There is a significant risk of minor complications. Medial impingement may require further surgical procedures at a later date depending on the severity of symptoms. The exact cause for this remains unknown; implant design may be incriminated if the newer anatomical designs overcome this problem.
Acknowledgements
We would like to thank Mr. Taylor’s secretary, Anita Summerfield, for her kind assistance during this study.
Conflict of interest statement No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributor Information
Harish V. Kurup, Phone: +44-1443-443443, FAX: +44-1443-443385, Email: harishvk@yahoo.com
Graeme R. Taylor, Email: Graeme.taylor@suht.swest.nhs.uk
References
- 1.Bonnin M, Judet T, Colombier JA, Buscayret F, Graveleau N, Piriou P (2004) Midterm results of the Salto total ankle prosthesis. Clin Orthop Relat Res 424:6–18 [DOI] [PubMed]
- 2.Buechel FF Sr, Buechel FF Jr, Pappas MJ (2004) Twenty-year evaluation of cementless mobile-bearing total ankle replacements. Clin Orthop Relat Res 424:19–26 [DOI] [PubMed]
- 3.Fuchs S, Sandmann C, Skwara A, Chylarecki C (2003) Quality of life 20 years after arthrodesis of the ankle. A study of adjacent joints. J Bone Joint Surg Br 85(7):994–998 [DOI] [PubMed]
- 4.Giannini S, Leardini A, O’Connor JJ (2000) Total ankle replacement: review of the designs and of the current status. Foot Ankle Surg 6(2):77–88 [DOI]
- 5.Hintermann B, Valderrabano V, Dereymaeker G, Dick W (2004) The HINTEGRA ankle: rationale and short-term results of 122 consecutive ankles. Clin Orthop Relat Res 424:57–68 [DOI] [PubMed]
- 6.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15(7):349–353 [DOI] [PubMed]
- 7.Lau JT, Mahomed NM, Schon LC (2005) Results of an internet survey determining the most frequently used ankle scores by AOFAS members. Foot Ankle Int 26(6):479–482 [DOI] [PubMed]
- 8.McGarvey WC, Clanton TO, Lunz D (2004) Malleolar fracture after total ankle arthroplasty: a comparison of two designs. Clin Orthop Relat Res 424:104–110 [DOI] [PubMed]
- 9.Myerson MS, Mroczek K (2003) Perioperative complications of total ankle arthroplasty. Foot Ankle Int 24(1):17–21 [DOI] [PubMed]
- 10.Myles PS, Urquhart N (2005) The linearity of the visual analogue scale in patients with severe acute pain. Anaesth Intensive Care 33(1):54–58 [DOI] [PubMed]
- 11.Nishikawa M, Tomita T, Fujii M, Watanabe T, Hashimoto J, Sugamoto K, Ochi T, Yoshikawa H (2004) Total ankle replacement in rheumatoid arthritis. Int Orthop 28(2):123–126 [DOI] [PMC free article] [PubMed]
- 12.Pyevich MT, Saltzman CL, Callaghan JJ, Alvine FG (1998) Total ankle arthroplasty: a unique design. Two- to twelve-year follow-up. J Bone Joint Surg Am 80(10):1410–1420 [PubMed]
- 13.Rippstein PF (2002) Clinical experiences with three different designs of ankle prostheses. Foot Ankle Clin 7(4):817–831 [DOI] [PubMed]
- 14.Spirt AA, Assal M, Hansen ST Jr (2004) Complications and failure after total ankle arthroplasty. J Bone Joint Surg Am 86-A(6):1172–1178 [DOI] [PubMed]
- 15.Wood PL, Deakin S (2003) Total ankle replacement. The results in 200 ankles. J Bone Joint Surg Br 85(3):334–341 [DOI] [PubMed]