Abstract
The mitochondrial total calcium content ([Ca]mt) was studied with electron probe microanalysis (EPMA) in isolated guinea-pig ventricular myocytes in order to answer the question of whether electrical stimulation increases [Ca]mt in subsarcolemmal and central mitochondria to a different extent.
In unstimulated myocytes subsarcolemmal [Ca]mt was (mean ±s.e.m.) 535 ± 229 μmol (kg dry weight (DW))−1 and central [Ca]mt was 513 ± 162 μmol (kg DW)−1. These values do not differ and correspond to approximately 180 μmol calcium per litre of mitochondria or 180 μM.
Contractions were potentiated to an optimum by stimulation with trains of 12 paired stimuli. After potentiation with 12 paired action potentials, cells were shock-frozen 120 ms after the start of the first action potential of the 13th pair. Subsarcolemmal [Ca]mt was 1·3 ± 0·4 mmol (kg DW)−1 (433 μM) and central [Ca]mt was 227 ± 104 μmol (kg DW)−1 (76 μM). The difference was significant.
After potentiation with 12 paired voltage-clamp pulses, cells were shock-frozen 120 ms after the start of the first pulse of the 13th pair. Subsarcolemmal [Ca]mt was 2·2 ± 1·0 mmol (kg DW)−1 (733 μM) and central [Ca]mt was 630 ± 180 μmol (kg DW)−1 (210 μM). After removal of extracellular K+, five paired voltage-clamp pulses increased subsarcolemmal [Ca]mt to 2·1 ± 0·8 mmol (kg DW)−1 (700 μM), which was significantly higher than the central [Ca]mt of 389 ± 88 μmol (kg DW) −1 or 130 μM.
In unstimulated cells, [Na] and [K] in subsarcolemmal and central mitochondria were not different. In potentiated myocytes, subsarcolemmal [Na]mt was 236 ± 20 mmol (kg DW)−1 or 79 mM, which is significantly higher than the central [Na]mt of 50 ± 5 mmol (kg DW)−1 or 16 mM.
The differences in [Ca]mt and [Na]mt are attributed to subsarcolemmal cytosolic microdomains of elevated [Ca2+] and [Na+] generated during contractile potentiation by transmembrane Ca2+ and Na+ fluxes.
We have shown in a previous electron probe microanalysis (EPMA) study that repetitive stimulation increases the cytosolic sodium concentration ([Na]cy) of cardiac myocytes from 10 to 60 mM (Wendt-Gallitelli et al. 1993). The elevation of [Na] was restricted to a 30 nm fringe of subsarcolemmal cytosol ([Na]SL), while cytosolic [Na] in the centre of the cell was nearly unchanged. Here, we follow up our previous results with the idea that the potentiation-induced rise in [Na]SL may cause an increase in mitochondrial [Ca]mt in subsarcolemmal but not in central mitochondria. The electron micrograph of Fig. 1 shows the arrangement of mitochondria.
Figure 1. A cross-section of a multicellular guinea-pig ventricular preparation.

The muscle strip was fixed with buffered 3 % glutaraldehyde, postfixed for 2 h in a solution containing 2 % osmium tetroxide and 0·8 % potassium ferrocyanide in 0·1 M sodium cacodylate buffer (pH 10). This postfixation produces a pronounced staining of the SR (Forbes et al. 1984). The network of free tubular sarcoplasmic reticulum envelops the packages of myofibrils and the central mitochondria (SR, arrowheads). Along the inner side of the sarcolemma SR-tubuli are interposed between myofibrils and sarcolemma. Subsarcolemmal mitochondria face directly the surface membrane, tubular SR is generally absent in the narrow space between subsarcolemmal mitochondria (m) and surface membrane. ECS, extracellular space. Bar = 1 μm.
Subsarcolemmal (synonymous with peripheral) mitochondria ‘contact’ the inner side of the sarcolemma via a ca 30 nm narrow fringe of cytosol. Approximately one-third of their outer mitochondrial membrane contributes to the diffusional barrier forming the narrow subsarcolemmal ‘fuzzy’ space in which influx of extracellular Na+ and Ca2+ ions induces accumulation of [Na]SL and [Ca]SL. We postulate that the high subsarcolemmal concentration drives Na+ and Ca2+ ions into subsarcolemmal mitochondria and raises [Na]mt and [Ca]mt. Central mitochondria are surrounded by packages of myofibrils and a network of free sarcoplasmic reticulum (SR); a 30 nm narrow ‘contact’ between central mitochondria and the sarcolemma of transversal tubules is seen on less than 2 % of their surfaces. Since a membrane-delimited fuzzy space is absent, Na+ and Ca2+ accumulation should be less in the centre than in the periphery of the cell. Hence, we expect potentiation to increase [Na] and [Ca] of subsarcolemmal but not of central mitochondria. EPMA with its high spatial resolution (approximately 16 nm) is an appropriate method to test this hypothesis.
The amount of mitochondrial calcium uptake depends on both spatial localization and kinetics. EPMA of myocytes shock-frozen at diastole as well as at various times after the start of systole indicated that [Ca]mt rises and falls during each individual contraction cycle, with a ca 20 ms delay after changes of [Ca]cy (Wendt-Gallitelli & Isenberg, 1991; Isenberg et al. 1993). Unfortunately, the experimental effort for such a kinetic analysis is enormous since shock-freezing ends the experiment and because statistics needs ca six cells per time point. It is therefore unsuitable for the present study where measurements are made from several spatial locations. Hence, we restrict the present study to a single time point of late systole, e.g. 120 ms after the start of depolarization, and we compare the elemental distribution of this functional state with that during rest.
The time point of late systole was selected for two reasons. Firstly, we would like to understand why another EPMA laboratory was unable to detect any increment in [Ca]mt in hamster trabeculae, approximately 100 ms after start of contraction (Moravec & Bond, 1991, 1992). Secondly, we would like to address apparent inconsistencies in our own work on [Ca]mt. In one study we found that 120 ms after the start of depolarization [Ca]mt no longer significantly differed from diastolic [Ca]mt (Wendt-Gallitelli & Isenberg, 1991). However, in subsequent work, we demonstrated that subsarcolemmal [Na]cy was still substantially elevated at such a time (Wendt-Gallitelli et al. 1993). Elevated [Na]SL should be linked to changes in [Na]mt and [Ca]mt via the mitochondrial Na+-Ca2+ exchanger, and hence the lack of change in [Ca]mt is rather surprising. A simple explanation would be that in the 1991 study we analysed mostly central mitochondria for the simple reason that central mitochondria are present in much larger numbers than subsarcolemmal mitochondria.
In the present study, we have compared [Ca]mt in potentiated and unstimulated (‘resting’) myocytes. The comparison was made in guinea-pig ventricular myocytes because activity-induced potentiation of contraction and cellular calcium content are well documented in this species (‘positive staircase’ of force and SR [Ca]: Wendt-Gallitelli, 1985). We have demonstrated that stimulation by paired voltage-clamp pulses potentiates the unloaded shortening and the cytosolic Ca2+ transients to physiological levels (Wendt-Gallitelli & Isenberg, 1991; Han et al. 1994). Since paired-pulse potentiation can eventually induce Ca2+ overload, we applied a train of only 12 paired pulses and discarded cells with signs of Ca2+ overload (after-contractions, transient inward currents, see e.g. Eisner & Valdeolmillos, 1986).
Functional implications
Elevated [Ca2+]mt is thought to constitute one of the mechanisms that may adapt mitochondrial respiration to the demands of cardiac work (e.g. Hansford, 1985; McCormack et al. 1990). In isolated rat ventricular myocytes, slow and sustained increments in free [Ca2+]mt have been measured after β-stimulation (indo-1-loaded rat ventricular myocytes: Miyata et al. 1991; however, see also Moravec et al. 1997). In guinea-pig ventricular myocytes, rapid beat-to-beat systolic changes in [Ca2+]mt have been extrapolated from cytosolic [Ca2+] transients (Isenberg et al. 1993) and directly measured by confocal imaging techniques (Trollinger et al. 1997). Activity-induced changes in total[Ca]mt have been measured in isolated cardiac mitochondria (McCormack & Denton, 1984) and extrapolated from 45Ca2+ fluxes that changed synchronously with the systolic force transients (Wolska & Lewartowski, 1991). EPMA should be the method of choice for direct measurements of activity-induced elevations in total [Ca]mt (see above: Wendt-Gallitelli & Isenberg, 1991; Isenberg et al. 1993). However, other EPMA laboratories suggested that [Ca]mt does not increase with contractile activity. In cardiac hamster trabeculae and Langendorff hearts, β-stimulation did not increase [Ca]mt although it increased pyruvate dehydrogenase activity (Moravec & Bond, 1992; Moravec et al. 1997). In ryanodine-treated rat cardiac trabeculae, the increase in stimulation from 0·6 to 10 Hz did not increase [Ca ]mt when [Ca2+]o was at the physiological level of 1·2 mM (Horikawa et al. 1998).
The present data suggest that central and subsarcolemmal mitochondria load differently with sodium and calcium when the cell is potentiated. We hope that the presented differences between central and subsarcolemmal mitochondria help to resolve the controversy on the function-dependent changes in cardiac [Ca]mt. In addition, the findings may provide insight into possible mechanisms for generating cytosolic [ATP] heterogeneities, since the different mitochondrial calcium load is thought to stimulate the respiratory oxidation of central and subsarcolemmal mitochondria to a different extent (Kargacin & Kargacin, 1997).
Parts of this work have been presented in abstract form (Wendt-Gallitelli et al. 1998).
METHODS
Isolation of myocytes
Guinea-pig ventricular myocytes were isolated as described previously (Isenberg & Klöckner, 1982). Briefly, guinea-pigs of approximately 300 g weight were killed by cervical dislocation. The heart was excised and mounted on a Langendorff apparatus for retrograde perfusion (37°C), first with a nominally Ca2+-free solution (mM: 140 NaCl, 10 KCl, 1 MgCl2, 10 glucose, 5 Hepes; with 1 mg ml−1 bovine serum albumin (BSA; Sigma); pH 7·3) for 5 min, and next with a similar salt solution containing collagenase (Worthington Type II, 338 U mg−1) and 6 μM Ca2+. After 20 min, perfusion was continued with 40 ml ‘KB-Medium’ (mM: 30 KCl, 0·5 KH2PO4, 50 glutamic acid, 20 taurine, 10 glucose, 3 MgSO4, 0·5 EGTA; with 1 mg ml−1 BSA; adjusted with KOH to pH 7·3). The ventricles were then cut off and the cells were dissociated by gentle agitation. Cells were stored in KB medium for at least 3 h before use. All procedures involving the use and treatment of animals were in accordance with the guidelines of, and were approved by, the animal welfare committee of the University of Halle.
Chamber and solutions
The experimental chamber had a volume of 120 μl and a flow rate of 2 ml min−1. The superfusate within the chamber could be changed within ca 10 s. Myocytes were continuously superfused with a physiological salt solution (PSS) containing (mM): 150 NaCl, 5·4 KCl, 1 MgCl2, 10 glucose, 5 Hepes (titrated to a pH of 7·4 with 4 mM NaOH), 3·6 CaCl2: this corresponds to a [Ca2+]0 of 1·5 mM (as measured with a Ca2+-sensitive electrode), due to the Ca2+ buffering effect of 15 % BSA added to reduce the water content of the extracellular solution to approximately 85 % (which results in fewer freezing artefacts in the frozen PSS, and hence better cryocutting conditions). The PSS was preheated and the experiments were performed at 36 ± 0·5°C.
Electrical recording and data acquisition
For whole-cell clamp, patch electrodes of 1·5-3·0 MΩ resistance were filled with a solution containing (mM): 150 KCl, 10 Hepes/KOH, 0·005 EGTA; pH 7·4. An RK-400 patch-clamp amplifier (Biologic, France) was used for voltage clamp (whole-cell method). The currents were filtered at 1 kHz and not corrected for leakage or capacitive components. A CED-1401 interface (Cambridge Electronic Design, Cambridge, UK; software custom written in-house) generated voltage-clamp commands and stimulus currents, and it digitized the data (5 kHz). Currents were recorded online with a thermowriter and were also stored in the computer for offline analysis. Figure 2 shows a recording of membrane potential while shock-freezing the myocyte during the repolarizing phase of the action potential, the cell being potentiated with a train of 12 paired 2 ms currents (1 nA) at a basic frequency of 1 Hz.
Figure 2. Freezing protocol of a myocyte stimulated with 2 ms depolarizing pulses.

The impact with the coolant is indicated by the vertical arrow. The membrane potential was stable at -80 mV, and after-depolarizations are completely absent.
Shock-freezing of the myocytes
The equipment and the protocol for time-freezing the single myocytes while recording membrane ionic currents have been described in detail in previous papers (Wendt-Gallitelli & Isenberg, 1989, 1991). Briefly, a quiescent myocyte with clear cross-striations was sucked onto the patch electrode, lifted from the bottom of the experimental chamber and transferred into the funnel of a silver micro-holder where it was placed on a thin film of Pioloform (polyvinyl butiral, Wacker Chemie, Munich, Germany). After rupture of the membrane patch, potentiation of contraction was achieved with paired voltage or current depolarizing pulses. Then a series of computer-controlled pneumatic movements was initiated. The inverted stage of the microscope with the chamber was moved backwards; this movement positioned the silver holder with the myocyte, the PSS and the electrode over a container with supercooled propane. Finally, at the appropriate time, the container with the supercooled propane (-196°C) was pneumatically pushed upwards for freezing. The mechanical movements did not damage the myocyte or induce leakage across the cell membrane, as monitored by continuously recording the membrane current till the very moment of shock-freezing (Fig. 2). Contact of the cell with the coolant induced a negative spike followed by a large positive current. The position of this artefact allowed us to measure the exact time when shock-freezing occurred.
EPMA and cryotechniques
Potentiation of contraction was monitored by the extent of cell shortening and the inward tail current to the Na+-Ca2+ exchanger (compare Egan et al. 1989). The elemental distribution in the different subcellular compartments was arrested by shock freezing the myocytes. Shock freezing was timed during rest, or during systole. The frozen silver micro-holder with the myocyte embedded in frozen PSS was cut at -150°C with a Reichert Ultracut FC4 cryoultramicrotome. The 100-200 nm thick sections (which during freeze drying were reduced by 65-80 % of their original volume) were analysed at -110°C in a Philips CM12 STEM electron microscope equipped with an energy dispersive germanium X-ray detector and digital signal processor (Link Gem with superATW, ISIS-300, Oxford Instruments, High Wycombe, UK). Since intracellular total [Ca] is low, to improve count statistics the acquisition time was as long as 800-1000 s for each data point (for details see Schultz & Wendt-Gallitelli, 1998; Schultz et al. 1999). The electron source was a Fei LaB6 filament. Under our analysis conditions the beam current was in the range of 10 nA.
Quantitative analysis
The X-ray spectrum consists of two components: peaks characteristic of elements present in the analysed microvolume, and a background proportional to the total analysed mass. The ratio between characteristic and continuum counts is linearly related to the concentration (mass fraction) of an element in the analysed volume (Hall, 1979). The ‘Bioquant’ program of the ISIS-300 analytical system for calculation of elemental concentrations is based on the continuum theory of Hall (1979), and was used (after costumer modifications and corrections) for calculating the concentrations of the elements (in mmol (kg DW)−1). To obtain the number of counts in a given peak, the program compares (with a multiple least square fit) the filtered spectrum to a library of primary reference files containing pure element spectra. Location of the peak centroid and resolution of the detector were calibrated for each spectrum with a computer fitting program which determines centroid position and resolution of two peaks (Statham, 1977). The inclusion of the first and second derivative of the important elements peaks in the deconvolution procedure minimizes errors due to small peak centroid shifts or detector resolution changes (Kitazawa et al. 1983). The program corrects the background by subtracting the extraneous components due to film, grid and holder. Recently, we have introduced in the program for processing the spectra an additional correction for Si contamination (Schultz et al. 1999). The continuum region selected was 1-5 keV. Mixtures of purified phosvitin and albumin (dry weight proportions 2:8) were used as secondary standards for quantifying the elements in the analysed volume (Shuman et al. 1976). We chose these biological standards since their organic matrix is similar to that of the analysed myocytes. [Na], [Mg] and [Ca] covalently bound in the two proteins were known, as measured by atomic absorption. Additionally, 600 mmol (kg DW)−1 KCl was added to the proteins mixture in order to simulate the [K]/[Ca] ratio in the intracellular space. Aqueous solutions (80 %, similar to the water content of cardiac myocytes) of the proteins and salts mixed as indicated above were prepared, frozen, cut, freeze-dried and analysed under the same conditions as the myocytes. The known concentrations of the elements in the biological standards allowed us to calculate the concentrations of the elements present in the cell compartments.
The detectability limit
The detectability limit of the system for calcium concentrations is determined by the count statistics of the CaKα peak and by the errors introduced with the techniques used for processing the spectrum (so-called ‘error of the single measurement’). Poor count statistics strongly influence the resolution, which in turn plays a crucial role in the deconvolution of partially overlapping peaks, as is the case for CaKα and KKβ. As shown recently in Schultz & Wendt-Gallitelli (1998), with the new system, the improved resolution for calcium reduced the mean error of the single measurement from 1·7 mmol (kg DW)−1 to 0·5 mmol (kg DW)−1, whereas the standard deviation of the mean [Ca]mt did not change (0·9 mmol (kg DW)−1). This indicates that a large biological variability rather than the analysis system represents the limit for quantification of low calcium concentrations in ventricular myocytes. The new system improved the sensitivity for [Ca] measurements by a factor of 1·4 and for [Na] by a factor of 6·2 (compared with conventional Si(Li) detectors with Be window).
Mass loss
Mass loss during analysis is due to interactions between energy-rich electrons of the electron beam and the biological material. The most important mass loss probably occurs during the very first (milli)seconds of exposure of the cryosection to the energy-rich electron beam, before acquisition of the spectrum. This mass loss possibly escapes our detection, and we presume it has also remained undiscovered in all the other laboratories. During the 800-1000 s acquisition time we recorded continuously the count rates of X-rays. For the cardiac myocytes, after 800 s acquisition the count rate was 95-97 % of the maximal rate reached during the total acquisition time and measured from the start of acquisition. (Although we carried out analysis at -110°C in the microscope, we cannot exclude the possibility that part of an initial mass loss may have been partially compensated by some contamination during the long acquisition time). Since we measured a larger mass loss (20 % and more) in standards with dextrane as the matrix, for the present study we used only phosvitin/albumin standards which, analysed under identical conditions, revealed a modest mass loss similar to that of the myocytes. Thus we feel confident that mass loss and contamination were similar in the standard and in the myocytes.
In order to be sure that ‘centrally’ located mitochondria did not stem from superficial cryosections cut tangentially to the surface membrane, only longitudinal cryosections with a recognizable nucleus or perinuclear regions were analysed. The analysing beam had a diameter of 16 nm. For analysis of mitochondria, a rectangular area just smaller than the area of the mitochondrion was scanned. For analysis of cytosol around the mitochondria, an area of the surrounding cytosol was scanned, excluding structures of the sarcoplasmic reticulum (SR) and extracellular space (ECS). The elemental concentrations were evaluated in mmol (kg DW)−1 of the compartment (e.g. [Ca]mt) by the Link ISIS-300 program and by customer-written software (MSQuant, written in-house). The methods have been described in detail previously (Wendt-Gallitelli & Isenberg, 1989, 1991).
Statistics
Spectra were collected from centrally located mitochondria and from those located just underneath the sarcolemma of the same cell. Mitochondria were attributed to the subsarcolemmal population only if (a) the cryosection had cut the surface membrane transversally, (b) the membrane was clearly recognizable, and (c) the subsarcolemmal location of the mitochondria was unequivocal. Since these three criteria were not always fulfilled, the number of subsarcolemmal mitochondria measured was in some cases smaller than the number of central mitochondria. Mitochondria were attributed to the central population only if the nucleus or the perinuclear domain were visible in the cryosection, in order to exclude the possibility that the measurements were made in a superficial cryosection with only peripheral mitochondria.
In the present study, cells from four different experimental protocols were analysed: (1) unstimulated myocytes (label in the figures: Unstim); (2) cells frozen 120 ms after start of depolarization following potentiation with paired voltage-clamp pulses (label: PP120 ms); (3) cells frozen 120 ms after start of depolarization following excitation with action potentials (label: AP120 ms); (4) cells frozen after potentiation with five paired pulses in K+-free bath solution (label: K+ free). In 16 cells from seven animals a minimum of 40 mitochondria were analysed in each experimental group, the number (n) of both, central and peripheral analysed mitochondria being given in the columns on the figures.
Quantitative data were transferred to a PC and statistically evaluated with the SAS statistic package (SAS Inst., Cary, NC, USA). To take into account differences in concentrations due to cell-to-cell and animal-to-animal variance, nested analysis of variance for unbalanced groups was performed. If the overall F test was significant (P < 0·05), differences between the single groups were then tested by linear comparison (Tukey-Kramer test).
In experiments with a homogeneous calcium load in the mitochondria (i.e. low biological variability in the group), as in resting myocytes, 0·2 mmol (kg DW)−1[Ca] was the minimal statistically significant difference detectable for the given number of analysed spectra (n). In the experimental groups with stimulated myocytes, which always showed a larger biological variability, the minimal statistically significant difference in [Ca]mt for the number of collected spectra was in the range of 0·6-0·7 mmol (kg DW)−1[Ca].
Concentration units
EPMA measures the amount of calcium per kilogram dry weight of the analysed compartment (mmol (kg DW)−1). In order to compare these concentrations with those in the patch electrode solution, or with data in the literature, they were transferred into units of molarity (mM). For example, there are good measurements of the water content of mitochondria which is approximately 66 % (Werkheiser & Bartley, 1957; Somlyo et al. 1981). Thus, a [Ca]mt of 1 mmol (kg DW)−1 can be translated into 0·33 mM (mmol (l mitochondria)−1). Assuming that the ratio of protein to dry weight is 0·75:1 in mitochondria, 1 mmol (kg DW)−1 corresponds to 1·33 nmol (mg protein)−1. The water content of the cytosol is estimated to be approximately 75 % (Polimeni, 1974).
The spatial resolution of subcellular compartments is limited by the diameter of the electron beam obtainable in the microscope and by the thickness of the cryosections. Since in modern microscopes the minimal beam diameter is no longer limiting, it is the 25-60 nm thickness of the freeze-dried cryosections that may preclude analysis of small compartments when the section is thicker than the diameter of the analysed structure (e.g. membrane vesicles, or SR tubules with a narrow lumen). In this paper, we primarily discuss calcium measured in the mitochondria. In this compartment, the spatial resolution of analysis is not limited by the thickness of the section and the morphology of the mitochondria is easily recognizable in cryosections.
RESULTS
In our previous papers we have shown that 10-12 paired voltage-clamp pulses potentiated contraction and Ca2+ transients to a new steady level, and we presented the records of the membrane currents before and during shock-freezing (Wendt-Gallitelli & Isenberg 1991). Figure 2 shows the alternative freezing protocol, the myocyte being stimulated with 2 ms depolarizing current pulses and frozen during the action potential. The normal diastolic membrane potential and the absence of transient membrane depolarization between the beats indicate the absence of leakage or of Ca2+ overload (Eisner & Valdeolmillos, 1986).
In Fig. 3A and B a longitudinal unstained cryosection of a ventricular myocyte is shown. The figure shows the excellent preservation of the cell compartments. Importantly freezing artefacts due to ice crystal formation are not visible. The mitochondria are clearly recognizable. Sarcomeres with Z- and M-lines and t-tubules with adjacent junctional SR and sarcolemma are very well preserved. The cell is surrounded by less well frozen bath solution. Small fragments of the silver holder, cut with the cell and bath solution are also visible (arrow).
Figure 3. Longitudinal cryosection of a ventricular myocyte.
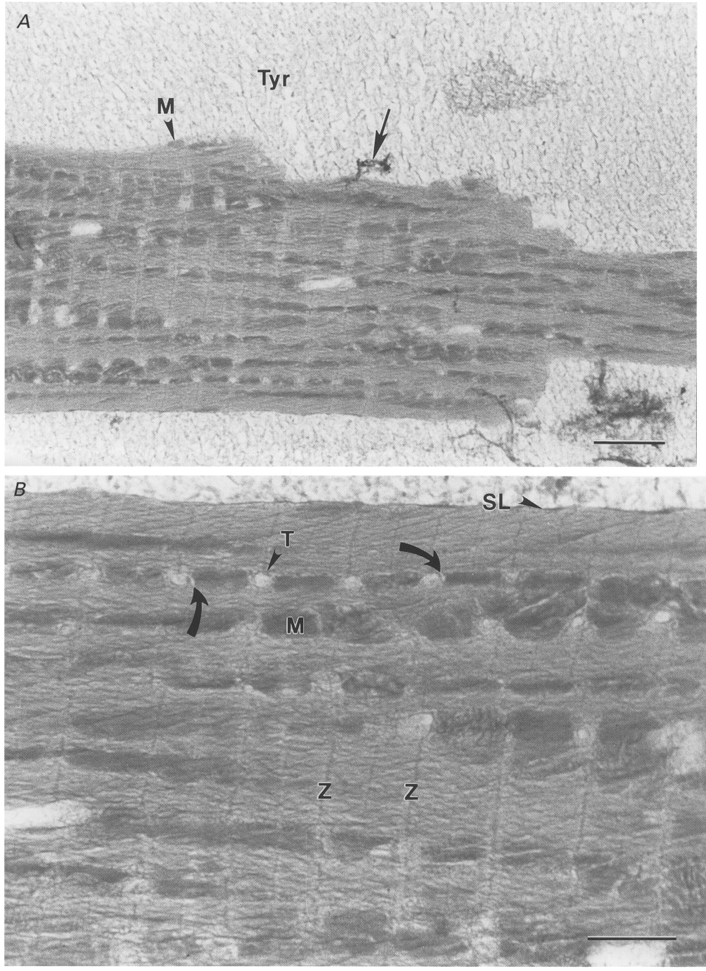
A, the figure shows the excellent preservation of the cell compartments. The sarcomeres have a constant length over the whole preparation, and the mitochondria are not swollen. The cell is surrounded by less well frozen bath solution. Small fragments of the silver holder (arrow) cut with cell and bath solution are also visible. Bar = 3·6 μm. B, the same myocyte at higher magnification: t-tubules are normal in diameter and elements of junctional SR around them are recognizable (curved arrows). Note that freezing artefacts due to ice crystal formation are not visible. Sarcomeres with Z- and M-lines and t-tubules with adjacent junctional SR and sarcolemma (SL) are well preserved in the unstained cryosection. M, mitochondrion. Z, z-line. T, t-tubule. Tyr, freeze-dried Tyrode solution. Bar = 1·8 μm.
Influence of potentiation on [Ca]mt
[Ca]mt in unstimulated myocytes
The myocytes were frozen after stimulation was interrupted for several minutes. Such a prolonged period of rest induces in guinea-pig ventricular myocytes a decay in the amplitude of contraction (‘rest decay’: Allen et al. 1976; Wendt-Gallitelli, 1985), which reaches a minimum within 5 min. In a previous study (Wendt-Gallitelli, 1985), we had shown that, after prolonged rest, the internal calcium stores of the myocytes (junctional and corbular SR) were depleted of calcium, whereas the calcium content of these compartments increased at the end of diastole after potentiation of contraction. In unstimulated myocytes, [Ca]mt of peripheral mitochondria was 535 ± 229 μmol (kg DW)−1 and that of central mitochondria was 513 ± 162 μmol (kg DW)−1. Both concentrations are low and not statistically different (compare left-hand columns labelled ‘Unstim’ in Fig. 4A).
Figure 4. Mitochondrial [Ca] and [Na] in unstimulated and potentiated myocytes.

A, [Ca]mt in peripheral (▪) and central (□) mitochondria of unstimulated and potentiated myocytes. Bars represent s.e.m; n, number of analysed mitochondria. Asterisks indicate level of significance between peripheral and central [Ca]mt within one experimental group: *P < 0·01; **P < 0·001. Unstim, mitochondria frozen after prolonged rest, at least 5 min. PP120 ms, mitochondria frozen 120 ms after the start of the 13th depolarizing pulse to 0 mV; cells potentiated with 12 paired pulses. Due to the high variance of [Ca]mt in peripheral mitochondria of this group, P < 0·1. AP120 ms, mitochondria frozen 120 ms after the start of the 13th action potential; cells potentiated with 12 paired action potentials. K+ free, mitochondria frozen 120 ms after the start of a depolarizing pulse to 0 mV; cells potentiated with 5 paired voltage-clamp pulses in K+-free bath solution. B, stimulation increases [Na]mt more in peripheral than in central mitochondria of guinea-pig ventricular myocytes. Bars represent s.e.m.*P < 0·001.
[Ca]mt in potentiated myocytes
After the myocytes had been potentiated to an optimum with a train of 12 paired voltage-clamp pulses they were shock-frozen 120 ms after start of the 13th clamp pulse to 0 mV. X-ray analysis indicated that [Ca]mt was higher in the potentiated than in the quiescent cells, when the peripheral mitochondria were concerned. More importantly, the analysis suggests the existence of two mitochondrial populations in the same cell. While the peripheral mitochondria underneath the sarcolemma contained calcium at high concentrations, the calcium concentration of central mitochondria was low (compare the two columns labelled ‘PP120 ms’ in Fig. 4A). [Ca]cy in the cytosol surrounding the peripheral mitochondria was 6 ± 2 mmol (kg DW)−1 (or 1·5 mM), while that in the centre of the cell was 4·5 ± 2·2 mmol (kg DW)−1 (or 1·1 mM).
It has been argued (Moravec et al. 1997) that potentiation with depolarizing voltage-clamp pulses was “un-normal” and would induce cellular calcium overload, hence, we repeated the experiments and potentiated the cell contractions with trains of 12 paired action potentials instead of 12 clamp pulses. The cells were shock-frozen 120 ms after start of the first action potential of the 13th pair (Fig. 4A, columns labelled ‘AP120 ms’). In contrast to unstimulated cells, potentiation by 12 paired action potentials changed the elemental composition of the cell significantly (P < 0·001), the changes being in the same direction as, but to a lesser extent than, those observed after potentiation by 12 paired clamp pulses. After potentiation with action potentials, [Ca]mt was 1·3 ± 0·4 mmol (kg DW)−1 (or 433 μM) in peripheral mitochondria and 227 ± 104 μmol (kg DW)−1 (or 76 μM) in central mitochondria. [Ca]cy in the cytosol surrounding the peripheral mitochondria of this group was 4·4 ± 1·2 mmol (kg DW)−1 (or 1·1 mM), while that in the centre of the cell was 2·3 ± 0·9 mmol (kg DW)−1 (or 575 μM).
We substituted the normal bath solution (5·4 mM [K+]o) with a K+-free bath solution. With this experiment we tested whether the increase in subsarcolemmal [Na]cy could be accelerated by K+-free solutions which inhibit the sarcolemmal Na+,K+-ATPase, and whether this increased subsarcolemmal [Ca]cy and [Ca]mt in turn. The myocytes were frozen in systole, 120 ms after start of depolarization. Before freezing, the cells were stimulated with five paired depolarizing voltage-clamp pulses (when 12 pulses were applied at [K+]o= 0, transient diastolic inward currents and after-contractions indicated Ca2+ overload). The columns of Fig. 4A labelled ‘K+ free'show that the five depolarizing pulses increased [Ca]mt exclusively in peripheral mitochondria, while [Ca]mt in the central mitochondria remained low. The increase was highly significant (P < 0·001). In this group, subsarcolemmal [Ca]cy was 2·5 ± 0·2 mmol (kg DW)−1 (or 425 μM) and central [Ca]cy was 1·7 ± 0·5 mmol (kg DW)−1 (or 242 μM). A stimulation-dependent [Ca] gradient from the cytosol to the adjacent mitochondria was present in the centre as well as in the subsarcolemmal region of the cell.
Influence of potentiation on [Na]mt
[Na]mt in peripheral and central mitochondria of unstimulated myocytes
Figure 4B (columns labelled ‘Unstim’) shows that the mitochondrial sodium concentration in unstimulated myocytes ([Na]mt) is between 26 and 41 mmol (kg DW)−1 (or 8·7-13·8 mM). [Na]mt in peripheral mitochondria was slightly higher than in central mitochondria, but the difference was not statistically significant. In unstimulated cells, [Na]mt was not significantly different from [Na]cy of the surrounding myoplasma (18-27 mM).
[Na]mt in peripheral and central mitochondria of potentiated myocytes
When the myocytes were potentiated with a train of 12 paired voltage-clamp pulses and frozen 120 ms after the start of the 13th pulse (Fig. 4B, PP120 ms), [Na]mt in the periphery was 112 ± 14 mM, which is significantly higher than 25 ± 7 mM in the central mitochondria (P < 0·001). In central mitochondria [Na]mt was not significantly different from [Na]mt in unstimulated myocytes (P > 0·05). After potentiation with paired action potentials (Fig. 4B, AP120 ms), the [Na]mt was also significantly higher in peripheral mitochondria (70 ± 9 mM) than in central mitochondria (11 ± 2 mM). Similar results were obtained when the myocytes were frozen after inhibition of the sarcolemmal Na+,K+-ATPase. In K+-free solution (Fig. 4B, K+ free), [Na]mt was significantly higher in peripheral mitochondria than in central mitochondria.
If the peripheral mitochondria of quiescent myocytes were compared by analysis of variance with those potentiated with paired pulses or with those in which the sarcolemmal Na+,K+-ATPase was inhibited with the K+-free solution, the peripheral [Na]mt of quiescent myocytes was significantly lower (P < 0·001) than in the other two groups.
In potentiated myocytes (all three experimental groups plotted together), [Na]cy was 61 ± 8 mM in the peripheral cytosol and 20 ± 2 mM in the central cytosol. A stimulation-dependent [Na] gradient from the cytosol to the mitochondria was detectable only in central regions of the cells. In the subsarcolemmal region [Na]cy (61 mM) was lower than [Na]mt (79 mM).
Heterogeneity within the mitochondrial populations
Figure 5A and B compares the frequency distribution of [Ca]mt in central (A) and peripheral (B) mitochondria of all experimental groups of potentiated myocytes (AP120 ms, PP120 ms, K+ free). Whereas central mitochondria of the three potentiated groups represented a homogeneous population with low [Ca]mt (0·36 mmol (kg DW)−1) and low biological variability (standard deviation, s.d.= 0·8), peripheral mitochondria represented a less homogeneous population with statistically significant higher mean [Ca]mt (1·76 mmol (kg DW)−1, P < 0·001) and higher biological variability (s.d.= 3·4).
Figure 5. Frequency distribution of [Ca]mt, [Na]mt and [P]mt, in central (A) and peripheral (B) mitochondria of potentiated myocytes.

The plots A and B include [Ca]mt from all 3 experimental groups of potentiated myocytes. The curve is a Gaussian curve with parameters determined by the statistics of the data plotted as histograms. Note that in all frequency distributions in Fig. 5 means ±s.d. (standard deviation) are shown, not ±s.e.m. The mean [Ca]mt of the two groups of mitochondria (central and peripheral) are statistically significantly different (P < 0·001). C-F, frequency distribution of [Na]mt (C and D) and [P]mt (E and F) in central and peripheral mitochondria of potentiated myocytes. The average [Na]mt and the standard deviation in peripheral mitochondria (D) are significantly higher than in central mitochondria (C) (P < 0·001). Frequency distribution and standard deviation of phosphorus ([P]mt) are similar in central (E) and peripheral (F) mitochondria, indicating that the higher [Na]mt is not due to systemic errors (smearing of extracellular components of the bath solution with intrcellular elemental concentrations).
Figure 5C shows that in central mitochondria of potentiated myocytes (as in Fig. 5A and B all experimental groups plotted together) [Na]mt was homogeneously low, whereas peripheral mitochondria (Fig. 5D) represented a highly inhomogeneous population, concerning [Na]mt. The mean of [Na]mt in this group (236 mmol (kg DW)−1 or 79 mM) was statistically significantly higher (P < 0·001) than the mean [Na]mt in central mitochondria (50 mmol (kg DW)−1 or 17 mM).
The frequency distribution of phosphorus in the same mitochondria ([P]; Fig. 5E and F) showed no significant differences between the two groups, and [P] was 0 mM in the bath solution. Therefore the differences in [Na]mt between central and peripheral mitochondria were not due to ‘smearing’ of extracellular components of the bath solution (high [Na] and no [P]) with the low [Na] and high [P] in the intracellular space.
Influence of potentiation of contraction on [K]mt
Figure 6 shows that in unstimulated myocytes, as well as in myocytes potentiated with APs, there was no significant difference between [K]mt in peripheral and central mitochondria. [K]mt was significantly lower in peripheral than in central mitochondria, when the myocytes were potentiated with paired pulses or when the sarcolemmal Na+,K+ATPase was inhibited.
Figure 6. Mitochondrial [K] in unstimulated and potentiated myocytes.

[K]mt in central (□) and peripheral (▪) mitochondria of ventricular myocytes frozen unstimulated (Unstim), or after potentiation with 12 APs (AP120 ms), 12 voltage-clamp pulses (PP120 ms), or 5 voltage-clamp pulses in K+-free bath solution (K+ free). n, number of analysed mitochondria. Bars represent s.e.m.*P < 0·05.
Influence of potentiation of contraction on [Cl]mt
[Cl]mt in peripheral and central mitochondria of unstimulated myocytes
The total chlorine concentration of peripheral and central mitochondria is low in unstimulated myocytes, being 90 ± 11 mmol (kg DW)−1 (or 30 mM) in peripheral and 101 ± 11 mmol (kg DW)−1 (or 34 mM) in central mitochondria (Fig. 7, Unstim). In quiescent myocytes the [Cl]mt (100 mmol (kg DW)−1 or 33 mM) is significantly lower than the 252 mmol (kg DW)−1 (or 63 mM) of the central cytosol in the same cells.
Figure 7. Mitochondrial [Cl] in unstimulated and potentiated myocytes.

Potentiation with voltage-clamp paired pulses or with paired action potentials increases [Cl]mt in peripheral (▪) more than in central (□) mitochondria of guinea-pig ventricular myocytes. n, number of analysed mitochondria. Bars represent s.e.m.*P < 0·001.
[Cl]mt in peripheral and central mitochondria of potentiated myocytes
Potentiation with trains of paired APs did not change [Cl]mt in central mitochondria (23 ± 2 mM), but increased [Cl]mt to 72 ± 9 mM in subsarcolemmal mitochondria (Fig. 7, AP120 ms). [Cl]cy was 67·5 ± 5·6 mM in central cytosol and 73 ± 8 mM in peripheral cytosol.
Potentiation with trains of paired voltage-clamp pulses increased [Cl]mt significantly in both central and peripheral mitochondria (101 ± 5 mM and 162 ± 7 mM, respectively). [Cl]cy was increased to 153 ± 11 mM in central cytosol and to 180 ± 27 mM in peripheral cytosol.
Influence of potentiation of contraction on [P]mt
Figure 8 shows that no significant difference was detected between [P]mt in peripheral and central mitochondria of unstimulated myocytes. When myocytes were potentiated with paired action potentials, [P]mt in peripheral and central mitochondria was identical. In myocytes potentiated with paired voltage-clamp pulses peripheral [P]mt was higher than central [P]mt. In the myocytes with inhibited Na+,K+-ATPase the [P]mt was significantly lower in peripheral than in central mitochondria (Fig. 8). It has been suggested that Ca2+ efflux from the mitochondria could conceivably occur by outward cotransport with Pi (Gunter & Pfeiffer, 1990). If peripheral mitochondria extrude more Ca2+ when trans-sarcolemmal Ca2+ influx becomes larger as a result of inhibition of the Na+,K+-ATPase, a coupled outward transport of Ca2+ and Pi might be not surprising. This process would explain why [P]mt was significantly higher in central than in peripheral mitochondria. Figure 8 shows also that EPMA measurements in subsarcolemmal mitochondria do not include extracellular components: phosphorous is completely absent in the bath solution surrounding the cell membrane. If measurements in subsarcolemmal mitochondria were contaminated with extracellular bath solution, the [P]mt would be lower in peripheral than central mitochondria. Hence the differences in [Ca]mt between peripheral and central mitochondria are not an artefact resulting from ‘smearing’ of extracellular components to subcellular intracellular structures.
Figure 8. Mitochondrial [Ca] and [P] in unstimulated and potentiated myocytes.

In central and peripheral mitochondria phosphorus concentrations are identical in quiescent myocytes (Unstim)and in mitochonria potentiated to optimal contractions with action potentials (AP120 ms). After paired depolarizing pulses (voltage-clamp experiment, PP120 ms) [P]mt was higher in peripheral than in central mitochondria. When the Na+,K+-ATPase (K+ free) was inhibited, [P]mt was significantly lower in peripheral than in central mitochondria. Since [Ca]mt increases significantly after potentiation with APs, whereas in the same experiment [P]mt does not change in peripheral and central mitochondria, the measurements in subsarcolemmal space are not contaminated with extracellular components (frozen bath solution). If artefactual inclusion (‘smearing’) of extracellular material had occurred, in fact, the [P] would be reduced, due to the total absence of P in the bathing solution. An increase in [Ca] in peripheral mitochondria, provoked by blocking Na+,K+-ATPase, paralleled a decrease in [P] in peripheral versus central mitochondria. Bars represent s.e.m.*P < 0·05, **P < 0·001.
Influence of potentiation on [Mg]mt
In unstimulated myocytes no significant differences were detected between the [Mg]mt of peripheral and central mitochondria (central, 32 ± 1 mmol (kg DW)−1; peripheral, 29 ± 1 mmol (kg DW)−1). Figure 9 shows the frequency distribution and standard deviation of the mean [Mg]mt in peripheral and central mitochondria of potentiated myocytes. Mean [Mg]mt were statistically not significantly different. The standard deviation of the two groups was equal.
Figure 9. Frequency distribution of [Mg]mt in central and peripheral mitochondria of potentiated myocytes.

AP120 ms, PP120 ms and K+ free plotted together. The means were not significantly different, and the standard deviations were similar.
DISCUSSION
The present results confirm that the total mitochondrial calcium concentration of unstimulated ventricular myocytes is low (this study: 180 μM; see also Wendt-Gallitelli & Isenberg, 1991; for low [Ca]mt at diastole see Moravec & Bond, 1991; Horikawa et al. 1998). The present study confirms that [Ca]mt increased when the contractions of the cells were potentiated (Wendt-Gallitelli & Isenberg, 1991; Isenberg et al. 1993) by trains of either ‘non-physiological’ paired voltage-clamp pulses or by trains of paired action potentials. Most importantly and for the first time, EPMA indicates that potentiation affected subsarcolemmal and central mitochondria differently. At late systole (120 ms after the start of depolarization) [Ca]mt of subsarcolemmal mitochondria was still significantly elevated while [Ca]mt of central mitochondria did not differ from resting [Ca]mt (confirming Wendt-Gallitelli & Isenberg, 1991). The new finding may partially explain the report of Moravec & Bond (1991) where the 4-fold increase from diastolic [Ca]mt (100 ± 200 μmol (kg DW)−1) to late systolic [Ca]mt (400 ± 100 μmol (kg DW)−1) did not become significant because of high variance of the data. The present results suggest that part of this variance may have arisen from different [Ca]mt in subsarcolemmal and central mitochondria.
Mitochondrial populations with different [Ca] existed only in potentiated, not in resting myocytes, suggesting that the increase in subsarcolemmal [Ca]mt may be related to an activity-dependent accumulation of Ca2+ or Na+ ions in the narrow fringe of subsarcolemmal cytosol. Ca2+ and Na+ ions will accumulate in the membrane-delimited subsarcolemmal space with restricted diffusion when the rate of influx (Ca2+ channels, Na+ channels, Na+-Ca2+ exchange) exceeds the rates of sequestration (e.g. Ca2+ uptake by SERCA (SR Ca2+-ATPase)) and extrusion (Na+,K+-ATPase, Na+-Ca2+ exchange). In the present study, [Ca]cy in the subsarcolemmal space of potentiated myocytes was 1·1 mM, twice as high as the [Ca]cy of 575 μM in the centre of the cell. We suggest that high [Ca]cy increases the mitochondrial Ca2+ load by stimulating mitochondrial Ca2+ uptake through the uniporter and by inhibiting mitochondrial Ca2+ egress via the mitochondrial Na+-Ca2+ exchanger (Gunter & Pfeifer, 1990).
On this basis, the existence of mitochondrial populations with different [Ca]mt is attributed to the heterogeneities in the [Ca2+]cy of the adjacent cytosol (see Introduction). We wonder whether the differences in [Ca]mt may have been also caused by [Na]cy gradients from subsarcolemmal and central parts of the cell (Wendt-Gallitelli et al. 1993). The present data indicate that [Na]cy and [Na]mt did not differ when the cells were unstimulated and that potentiation increased both [Na]cy and [Na]mt. In the central regions of the cell, [Na]cy of 20 mM was higher than [Na]mt, which was 17 mM, a result in line with the fluometric study of Donoso et al. (1992) who reported lower [Na+]mt than [Na+]cy for rat ventricular myocytes. The Na+ gradient has a direction that can support egress of mitochondrial Ca2+ coupled to the influx of cytosolic Na+. In the subsarcolemmal space, however, [Na]cy was 61 mM, lower than [Na]mt in the mitochondria which was 79 mM. This Na+ gradient is not sufficient for Ca2+ efflux coupled to Na+ influx into mitochondria, or else it reduces the rate of mitochondrial Ca2+ egress. However, we cannot yet answer the question of the extent to which the different Na+ gradients are the cause or the result of the differences in [Ca]mt between subsarcolemmal and central mitochondria.
The increase in subsarcolemmal [Na]cy could be accelerated by K+-free solutions inhibiting the sarcolemmal Na+,K+-ATPase, and this would be expected to increase subsarcolemmal [Ca]cy and [Ca]mt in turn. In K+-free solution, as few as five paired pulses were sufficient to increase peripheral [Ca]mt significantly above central [Ca]mt. Although these data support the idea of subsarcolemmal [Na]cy being a key regulator of [Ca2+]mt, they cannot determine whether subsarcolemmal Na+ increases [Ca]mt via elevated [Ca2+]cy or via reduced mitochondrial Na+-Ca2+ exchange. Forthcoming experiments under conditions of identical [Ca2+]cy but different cytoplasmic [Na+] may clarify this point.
The different elemental concentrations in central versus subsarcolemmal mitochondria suggest that peripheral mitochondria could operate at a higher rate of oxidative phosphorylation than the central mitochondria.
This and our previous work used guinea-pig ventricular myocytes as a model. In these cells (as in human myocytes, Böhm et al. 1992), an increase in the rate of stimulation potentiates the influx of extracellular Ca2+ ions, resulting in improved SR Ca2+ filling, which in turn increases the activator Ca2+ and contraction (for frequency effects on inotropy and SR calcium load, see Wendt-Gallitelli, 1985; for the effects of paired stimuli, see Wendt-Gallitelli & Isenberg, 1991). In contrast, ventricular myocytes from rats and mice have a negative frequency inotropy (e.g. Shattock & Bers, 1989; Bers, 1991). Unstimulated rat ventricular myocytes show spontaneous SR Ca2+ release and Ca2+ waves due to SR Ca2+ overload (e.g. Kort & Lakatta, 1988; for references see Bers, 1991). In rat, an increase in the frequency of stimulation is expected to reduce the cytosolic activator [Ca2+]cy, and elevation of [Ca]mt seems to be unlikely. Hence, it is not surprising that ryanodine-treated rat trabeculae (functional removal of the SR Ca2+ store) did not respond to the increase in stimulation frequency (from 0·6 to 10 Hz) with an increase in [Ca]mt (Horikawa et al. 1998).
Extrapolation of experimental data to the in vivo situation requires a comparable functional state, e.g. one should compare data from potentiated and not from resting myocytes. We potentiated the guinea-pig ventricular myocytes by trains of 12 paired action potentials or paired voltage-clamp pulses. We consider that this potentiation is ‘physiological’ because the 12th contraction had a rate and amplitude similar to the contractions induced by 3 Hz steady stimulation (extent of unloaded shortening ca 10 %; see Wendt-Gallitelli & Isenberg, 1991). Potentiation by trains of paired action potentials or paired voltage-clamp pulses increased [Ca]mt to a very similar extent, i.e. the increase in [Ca]mt is not peculiar for the paired voltage-clamp pulses.
Subsarcolemmal [Ca]mt increased to 2·2 ± 1·0 mmol (kg DW)−1 in the voltage-clamp experiments and to 1·3 ± 0·4 mmol (kg DW)−1 in the action potential experiments (significance at P < 0·1). The difference may be partially attributed firstly to facilitation of Ca2+ influx via Na+-Ca2+ exchange as a result of second pulse of the pair reaching +50 mV (Wendt-Gallitelli et al. 1993). In addition, the diastolic membrane potential was ca -80 mV between the action potentials but -50 mV between the clamp pulses. Since the rate of sarcolemmal Ca2+ extrusion via Na+-Ca2+ exchange is lower at -50 than at -80 mV (for references see Bers, 1991), a longer lasting [Ca2+]cy transient may contribute to the mitochondrial Ca2+ loading.
It has been argued that increments in [Ca]mt are typical of Ca2+-overloaded but not of ‘normal’ myocytes and, in particular, that cell isolation tears the gap junctions out of the membrane, resulting in Ca2+ influx and Ca2+ overload (Moravec & Bond, 1992; Moravec et al. 1997; Horikawa et al. 1998). There is evidence for Ca2+ influx during cell dissociation (see Isenberg & Klöckner, 1982), but the effects of this influx are subsequently fully compensated. EPMA indicates that [Ca] in cytosol, SR and mitochondria is low in resting cells (present study; see also Wendt-Gallitelli & Isenberg, 1989). Ca2+ overload did occasionally occur, e.g. as the result of bad cell isolation, myocytes contracted spontaneously and were discarded. Ca2+ overload could also be induced by over-excessive potentiation, and then the occurrence of after-contractions and transient depolarizations (current clamp) or transient inward currents (voltage-clamp conditions) made us discard the cells. Potentiation with 12 paired voltage-clamp pulses regularly induced Ca2+ overload in cells with inhibited Na+,K+-ATPase (K+-free superfusates), and in these experiments the number of pulse pairs was reduced to five. In summary, all the available evidence suggests that the present data is typical for ventricular myocytes potentiated to a physiological extent.
There are a number of arguments for performing the experiments with single cells and not with multicellular trabeculae or Langendorff hearts. (1) Good cryosections ca 6 μm in thickness are obtainable with liquid coolants, which means that isolated myocytes can be frozen rapidly and homogeneously with excellent preservation of the structures to be analysed (Fig. 3). In contrast, multicellular ventricular myocytes isolated from the epicardium or endocardium often show freezing artefacts such as large ‘holes’ around the mitochondria (for example Fig. 4 in Horikawa et al. 1998). (2) In single cells of the guinea-pig, Ca2+ release and contraction are macroscopically homogeneous, i.e. the different sarcomeres are in the same functional state. This synchronization can be achieved in small cardiac trabeculae only with great effort. In Langendorff hearts, conduction of the action potential takes time, thereby preventing adequate synchronization, and EPMA characterizing the elemental distribution of a few subendocardial cells cannot really be correlated with the force transient recorded from the whole Langendorff heart. (3) Using the isolated cell, EPMA Ca concentrations is applied to the very same cell that has been functionally characterized by the electrical recordings, an important advantage that has been discussed at length when the single cell model was introduced (e.g. Isenberg & Klöckner, 1980, 1982; Powell et al. 1980). (4) Comparison of EPMA Ca concentrations with single whole-cell currents permits us to compare the amount of Ca2+ influx (Ca2+ channel current) and Ca2+ efflux (tail current due to electrogenic Na+-Ca2+ exchange) with the resulting changes in total concentrations of [Ca]cy and [Ca]mt.
Our chlorine measurements indicated that potentiation increased [Cl]mt approximately 2-fold more in subsarcolemmal than in central mitochondria. We speculatively attribute this difference to the higher [Ca]mt on the assumption that mitochondrial Ca2+ influx depolarizes the mitochondrial membrane, and that less negative mitochondrial membrane potentials would augment mitochondrial Cl− uptake (see also Zygmunt, 1994; Trafford et al. 1998). At present, this data is preliminary, and the existence and the functional importance of elevated subsarcolemmal [Cl]cy and [Cl]mt remain to be clarified by EPMA in the future.
In this study the total magnesium concentration did not change significantly between resting and stimulated cells. This finding is in apparent contrast with results of Romani et al. (1993) who detected a decrease or increase in total magnesium content of up to 10 % in perfused rat hearts stimulated with noradrenaline or carbachol for at least 5 min (Fig. 8, p. 1145 of the paper by Romani et al. 1993). We think that the discrepancy between our findings and those of Romani et al. may be explained by the facts that, firstly, our guinea-pig ventricular myocytes were not stimulated with noradrenaline, and secondly, mitochondrial magnesium seems to require a longer time course to show change than those used in this study.
In summary, subsarcolemmal mitochondria accumulated calcium to a much higher extent than the central mitochondria, and we attribute the difference in mitochondrial calcium load to differences in the potentiation-induced cytosolic Ca2+ accumulation. Since [Ca]mt is thought to be involved in regulating the rate of oxidative phosphorylation (Balaban, 1991; Gunther & Gunther, 1994), the data allow us speculate that potentiated cells have a higher mitochondrial respiration in their subsarcolemmal than in their central mitochondria. The higher rate of ATP synthesis should contribute to the local heterogeneity of [ATP]cy that has been postulated repeatedly (Kargacin & Kargacin, 1997). The above concept of a working ventricular myocyte having functionally distinct populations of mitochondria is in line with the recent finding that ischaemia decreases selectively oxidative phosphorylation in subsarcolemmal but not in central mitochondria (Lesnefsky et al. 1997).
Acknowledgments
The authors are very grateful to Nicole Walter for excellent technical assistance. This work was supported by the Deutsche Forschungsgemeinschaft Grant We 879/5-1 and by BMBF 992520/5 to M.F.G.
References
- Allen DG, Jewell BR, Wood EH. Studies of the contractility of mammalian myocardium at low rates of stimulation. The Journal of Physiology. 1976;254:1–17. doi: 10.1113/jphysiol.1976.sp011217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balaban RS. Regulation of oxidative phosphorylation in the mammalian cell. American Journal of Physiology. 1991;258:C377–389. doi: 10.1152/ajpcell.1990.258.3.C377. [DOI] [PubMed] [Google Scholar]
- Bers D. Developments in Cardiovascular Medicine. Vol. 122. The Netherlands: Kluwer Academic Publisher; 1991. Excitation-contraction coupling and cardiac contractile force; pp. 1–258. [Google Scholar]
- Böhm M, La Rosée K, Schmidt U, Schulz C, Schwinger RHG, Erdmann E. Force frequency relationship and inotropic stimulation in the non-failing and failing human myocardium: implications for the medical treatment of heart failure. Clinical Investigation. 1992;70:421–425. doi: 10.1007/BF00235525. [DOI] [PubMed] [Google Scholar]
- Donoso P, Mill JG, O'Neill SC, Eisner DA. Fluorescence measurements of cytoplasmic and mitochondrial sodium concentration in rat ventricular myocytes. The Journal of Physiology. 1992;448:493–509. doi: 10.1113/jphysiol.1992.sp019053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan TM, Noble D, Noble SJ, Powell T, Spindler AJ, Twist VW. Sodium-calcium exchange during the action potential in guinea-pig ventricular cells. The Journal of Physiology. 1989;411:639–61. doi: 10.1113/jphysiol.1989.sp017596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisner DA, Valdeolmillos M. A study of intracellular calcium oscillations in sheep cardiac Purkinje fibres measured at the single cell level. The Journal of Physiology. 1986;372:539–556. doi: 10.1113/jphysiol.1986.sp016024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes MS, Hawkey LA, Sperelakis N. The transverse-axial tubular system (TATS) of mouse myocardium: its morphology in the developing and adult animal. American Journal of Anatomy. 1984;170:143–162. doi: 10.1002/aja.1001700203. [DOI] [PubMed] [Google Scholar]
- Gunter KK, Gunter TE. Transport of Calcium by mitochondria. Journal of Bioenergetics and Biomembranes. 1994;26:471–485. doi: 10.1007/BF00762732. [DOI] [PubMed] [Google Scholar]
- Gunter TE, Pfeiffer DR. Mechanisms by which mitochondria transport calcium. American Journal of Physiology. 1990;258:C755–786. doi: 10.1152/ajpcell.1990.258.5.C755. [DOI] [PubMed] [Google Scholar]
- Hall TA. Biological X-ray microanalysis. Journal of Microscopy. 1979;11:145–163. doi: 10.1111/j.1365-2818.1979.tb00236.x. [DOI] [PubMed] [Google Scholar]
- Han S, Schiefer A, Isenberg G. Ca2+ load of guinea- pig ventricular myocytes determines efficacy of brief Ca2+ currents as trigger for Ca2+ release. The Journal of Physiology. 1994;480:411–421. doi: 10.1113/jphysiol.1994.sp020371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansford RG. Relation between mitochondrial calcium transport and control of energy metabolism. Reviews in Physiology Biochemistry Pharmacology. 1985;102:1–72. doi: 10.1007/BFb0034084. [DOI] [PubMed] [Google Scholar]
- Horikawa Y, Goel A, Somlyo AP, Somlyo AV. Mitochondrial calcium in relaxed and tetanized myocardium. Biophysical Journal. 1998;74:1579–1590. doi: 10.1016/S0006-3495(98)77869-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg G, Han S, Schiefer A, Wendt-Gallitelli MF. Changes in mitochondrial calcium concentration during the cardiac contraction cycle. Cardiovascular Research. 1993;27:1800–1809. doi: 10.1093/cvr/27.10.1800. [DOI] [PubMed] [Google Scholar]
- Isenberg G, Klöckner U. Glycocalix is not required for slow inward calcium current in isolated rat heart myocytes. Nature. 1980;284:358–360. doi: 10.1038/284358a0. [DOI] [PubMed] [Google Scholar]
- Isenberg G, Klöckner U. Calcium tolerant ventricular myocytes prepared by preincubation in a ‘KB-Medium’. Pflügers Archiv. 1982;395:6–18. doi: 10.1007/BF00584963. [DOI] [PubMed] [Google Scholar]
- Kargacin ME, Kargacin GJ. Predicted changes in concentrations of free and bound ATP and ADP during intracellular signalling. American Journal of Physiology. 1997;273:C1416–1426. doi: 10.1152/ajpcell.1997.273.4.C1416. [DOI] [PubMed] [Google Scholar]
- Kitazawa T, Shuman H, Somlyo AP. Quantitative electron probe microanalysis: problems and solutions. Ultramicroscopy. 1983;11:251–262. [Google Scholar]
- Kort AA, Lakatta EG. Spontaneous sarcoplasmic reticulum release in rat and rabbit cardiac muscle: relation to transient and rested-state twitch tension. Circulation Research. 1988;63:969–979. doi: 10.1161/01.res.63.5.969. [DOI] [PubMed] [Google Scholar]
- Lesnefsky EJ, Tandler B, Ye J, Slabe TJ, Turkaly J, Hoppel CL. Myocardial ischemia decreases oxidative phosphorylation through cytochrome oxidase in subsarcolemmal mitochondria. American Journal of Physiology. 1997;273:H1544–1554. doi: 10.1152/ajpheart.1997.273.3.H1544. [DOI] [PubMed] [Google Scholar]
- McCormack JG, Denton RM. Role of Ca2+ ions in the regulation of intramitochondrial metabolism in rat heart. Evidence from studies with isolated mitochondria that adrenaline activates the pyruvate dehydrogenase and 2-oxoglutarate dehydrogenase complexes by increasing the intramitochondrial concentration of Ca2+ Biochemical Journal. 1984;218:235–247. doi: 10.1042/bj2180235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack JG, Halestrap AP, Denton RM. Role of calcium ions in regulation of mammalian intramitochondrial metabolism. Physiological Reviews. 1990;70:391–426. doi: 10.1152/physrev.1990.70.2.391. [DOI] [PubMed] [Google Scholar]
- Miyata HH, Silverman HS, Sollot SJ, Lakatta EG, Stern MD, Hansford RG. Measurements of mitochondrial free Ca2+ concentration in living single rat cardiac myocytes. American Journal of Physiology. 1991;261:H1123–1134. doi: 10.1152/ajpheart.1991.261.4.H1123. [DOI] [PubMed] [Google Scholar]
- Moravec CS, Bond M. Calcium is released from the junctional sarcoplasmic reticulum during cardiac muscle contraction. American Journal of Physiology. 1991;260:H989–997. doi: 10.1152/ajpheart.1991.260.3.H989. [DOI] [PubMed] [Google Scholar]
- Moravec CS, Bond M. Effect of inotropic stimulation on mitochondrial calcium in cardiac muscle. Journal of Biological Chemistry. 1992;267:5310–5316. [PubMed] [Google Scholar]
- Moravec CS, Desnoyer RW, Milovanovic M, Schluchter MD, Bond M. Mitochondrial calcium content in isolated perfused heart: effects of inotropic stimulation. American Journal of Physiology. 1997;273:H1432–1439. doi: 10.1152/ajpheart.1997.273.3.H1432. [DOI] [PubMed] [Google Scholar]
- Polimeni PI. Extracellular space and ionic distribution in rat ventricle. American Journal of Physiology. 1974;258:H452–459. doi: 10.1152/ajplegacy.1974.227.3.676. [DOI] [PubMed] [Google Scholar]
- Powell T, Terrar DA, Twist VW. Electrical properties of individual cells isolated from adult rat ventricular myocardium. The Journal of Physiology. 1980;302:131–153. doi: 10.1113/jphysiol.1980.sp013234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romani A, Marfella C, Scarpa A. Regulation of magnesium uptake and release in the heart and in isolated ventricular myocytes. Circulation Research. 1993;72:1139–1148. doi: 10.1161/01.res.72.6.1139. [DOI] [PubMed] [Google Scholar]
- Schultz M, Rudolf F, Gallitelli MF. Improvement in quantitative X-ray microanalysis of biological cryosections. Microscopy and microanalysis. 1999;5 doi: 10.1017/S1431927699000136. in the Press. [DOI] [PubMed] [Google Scholar]
- Schultz M, Wendt-Gallitelli MF. Improved quantitative X-ray microanalysis of biological cryosections using an EDS germanium detector and a super-athmosphere thin window (SuperATW) Journal of Microscopy (Oxford) 1998;190:293–297. doi: 10.1046/j.1365-2818.1998.00371.x. [DOI] [PubMed] [Google Scholar]
- Shattock MJ, Bers DM. Rat vs. Rabbit ventricle: Ca flux and intracellular Na assessed by ion-selective microelectrodes. American Journal of Physiology. 1989;256:C813–822. doi: 10.1152/ajpcell.1989.256.4.C813. [DOI] [PubMed] [Google Scholar]
- Shuman H, Somlyo AV, Somlyo AP. Quantitative electron probe microanalysis of biological thin sections: methods and validity. Ultramicroscpy. 1976;1:317–339. doi: 10.1016/0304-3991(76)90049-8. [DOI] [PubMed] [Google Scholar]
- Somlyo AV, Gonzales-Serratos H, Shuman H, McClennan G, Somlyo AP. Calcium release and ionic changes in the sarcoplasmic reticulum of tetanized muscle: an electronprobe study. Journal of Cell Biology. 1981;90:577–594. doi: 10.1083/jcb.90.3.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statham PJ. Deconvolution and background subtraction by least square fitting with prefiltering of spectra. Analytical Chemistry. 1977;49:2149–2153. [Google Scholar]
- Trafford AW, Diaz ME, Eisner DA. Ca-activated chloride current and Na+/Ca2+-exchange have different time courses during sarcoplasmic reticulum Ca release in ferret ventricular myocytes. Pflügers Archiv. 1998;435:743–745. doi: 10.1007/s004240050577. [DOI] [PubMed] [Google Scholar]
- Trollinger DR, Cascio WE, Lemaster JJ. Selective loading of Rhod 2 into mitochondria shows mitochondrial Ca2+ transients during the contractile cycle in adult rabbit cardiac myocytes. Biochemical and Biophysical Research Communications. 1997;236:738–742. doi: 10.1006/bbrc.1997.7042. [DOI] [PubMed] [Google Scholar]
- Wendt-Gallitelli MF. Presystolic calcium-loading of the sarcoplasmic reticulum influences time to peak force of contraction. X-ray microanalysis on rapidly frozen guinea-pig ventricular muscle preparations. Basic Research in Cardiology. 1985;80:617–625. doi: 10.1007/BF01907860. [DOI] [PubMed] [Google Scholar]
- Wendt-Gallitelli MF, Isenberg G. X-ray microanalysis of single cardiac myocytes frozen under voltage-clamp conditions. American Journal of Physiology. 1989;256:H574–583. doi: 10.1152/ajpheart.1989.256.2.H574. [DOI] [PubMed] [Google Scholar]
- Wendt-Gallitelli MF, Isenberg G. Total and free myoplasmic calcium during a contraction cycle: X-ray microanalysis in guinea-pig ventricular myocytes. The Journal of Physiology. 1991;435:349–372. doi: 10.1113/jphysiol.1991.sp018514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendt-Gallitelli MF, Schultz M, Isenberg G, Rudolf F. Stimulation increases calcium more in peripheral than in central cardiac mitochondria. Pflügers Archiv. 1998;435 No. 6, R73. [Google Scholar]
- Wendt-Gallitelli MF, Voigt T, Isenberg G. Microheterogenity of subsarcolemmal sodium gradients. Electron probe microanalysis in guinea-pig ventricular myocytes. The Journal of Physiology. 1993;472:33–44. doi: 10.1113/jphysiol.1993.sp019934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werkheiser WC, Bartley W. The study of steady-state concentrations of internal solutes of mitochondria by rapid centrifugal transfer to a fixation medium. Biochemical Journal. 1957;66:79–91. doi: 10.1042/bj0660079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolska BM, Lerwatowski B. Calcium in the in situ mitochondria of rested and stimulated myocardium. Journal of Molecular and Cellular Cardiology. 1991;23:217–22. doi: 10.1016/0022-2828(91)90108-x. [DOI] [PubMed] [Google Scholar]
- Zygmunt AC. Intracellular calcium activates a chloride current in canine ventricular myocytes. American Journal of Physiology. 1994;267:H1984–1995. doi: 10.1152/ajpheart.1994.267.5.H1984. [DOI] [PubMed] [Google Scholar]


