Abstract
Shared decision making in health care is a mutual partnership between the health care provider and the patient. Traditionally, children have had little involvement during their medical care visits or in decisions regarding their health care. Shared decision making in children with asthma may enhance their self-confidence as well as improve their self-management skills. Allowing the child to participate during the visit requires assessing the child’s competence at different ages and abilities. Specific communication techniques to use with children during medical encounters include visual aids, turn-taking, clarifying communication, and role modeling. Providers additionally can offer strategies to parents on how to provide general information about asthma and treatments based on the child’s questions and interest. The goal for school age children with asthma is to change dyadic interactions between the provider and parent into triadic interactions to improve the child’s asthma management.
Over the past two decades, delivery of healthcare has been undergoing a shift from doctor-centered care to patient-centered care (Brown, Stewart, McCracken, & McWhinney, 1986; Levenstein, McCracken, McWhinney, Stewart, & Brown, 1986) in an effort to improve quality of health care. The U.S. Institute of Medicine report in 2001 (Institute of Medicine, 2001) endorsed patient-centered care and recommended that health care providers implement the shared-decision model (SDM) in clinical settings (Berwick, 2002). Shared decision making in health care is defined as an active mutual partnership between the physician or other health care provider and the patient (Charles, Gafni, & Whelan 1997). Because pediatric asthma care involves several professional groups, our use of the term “provider” encompasses physicians, nurses, nurse practitioners, physician assistants, and respiratory therapists.
Patient centeredness honors the individual patient by respecting the patient’s choices, culture, social context, and specific needs (Berwick, 2002) with the aim to customize patient care. A recent study using clinical vignettes for parental rating of satisfaction with care indicated that shared decision-making for acute otitis media between parent and provider would lead to lower antibiotic use and higher satisfaction with care (Merenstein, Diener-West, Krist, Pinneger, & Cooper, 2005). Few studies examine shared decision-making with children.
Children as young as 2 years of age can participate in communicating their health and treatment needs (Nova, Vegni, & Moja, 2005). Most preschoolers believe that the health care provider holds absolute authority (Broome, 1999) and may only be able to share their symptoms or describe what they do not like about a prescribed regimen. At this age children are unable to “partner” with the provider in health care decisions. However, school-aged children may be able to share in some of their health care decisions, and some studies indicate that children as young as eight years are self-managing their asthma medications (Winkelstein et al, 2000).
Traditionally, the child’s contribution during medical visits has been rather limited at an estimated 10% of the visit, and the communication is dominated by the physician and parent (Wissow, Roter, & Bauman, 1998; Tates & Meeuwesen, 2001). Yet, the information received from the child may provide information that differs from the parent’s report and may actually improve the child’s care (Guyatt, Juniper, Griffith, Feeny, & Ferrie, 1997). In a study of physician-parent-child communication in a pediatric emergency room, the number of statements made to a provider by the child was far fewer than the parent. Children spoke in only 12% of the statements made to the provider, and the mean number of statements made by the parent was 156 statements versus 20 statements by the child (Wissow et al., 1998).
Common barriers to child participation in the medical visit include parent restriction of the child’s communication and limitation of communication to social talk lacking any health instruction. In general, physicians strive for active participation from the child, but parents often restrict the child’s participation and want to lead the medical visit (Tates & Meeuwesen, 2000). When physicians do communicate with the child during the visit, most of the physician-child interaction is restricted to affective behavior including social behavior, joking, and asking about school, but not directed at health instruction (van Dulmen, 1998; Pantell, Stewart, Dias, Wells, & Ross, 1982). Rarely is the child included in the discussion of the diagnosis or treatment (Wissow et al., 1998; Korsch, Gozzi, & Francis, 1968). Thus, the typical pediatric medical visit is primarily a dyadic interaction between the provider and parent (Tates, Meeuwesen, Elbers, & Bensing, 2002) rather than a triadic interaction among provider, parent, and child.
In children with asthma, patient-centered care involves an ongoing relationship between the family and provider with regular decision making about environmental control, medication regimens, accurate assessment of symptoms by child and parent (Halterman, Aligne, Auinger, McBride, & Szilagyi, 2000), and when to seek emergency medical care. National asthma guidelines recommend an “active partnership” or shared decision making between the provider and patient to maximize adherence to a prescribed treatment regimen (U.S. Department of Health & Human Services, 1997; U.S. Department of Health & Human Services, 2002).
Evidence Linking Effective Doctor-Patient Communication with Health Outcomes
Positive health outcomes have been associated with provider-patient interactions that are participatory, interactive, and allow patients to effectively communicate their health story (Roter, 2000). High quality provider-patient communication has been linked to symptom resolution, improved emotional health, and pain control (Stewart, 1995); satisfaction with medical care (DiMatteo, 1998); adherence to self-care in patients with diabetes (Golin, DiMatteo, & Gelberg, 1996); and reduction in physical limitations in chronically ill patients (Kaplan, Greenfield, & Ware, 1989; Greenfield, Kaplan, & Ware, 1988).
In a study of pediatric asthma emergency department (ED) visits, parents who reported that their child’s physician used more parent-centered communication during the ED visits, rated the encounter higher for partnering with the child’s physician and receiving information (Wissow et al., 1998). Clark et al. (1998) provided further support for patient-centered care and active partnership between parent and physician. Using a seminar style meeting with physicians to teach effective clinical teaching, updated asthma guidelines, and effective communication behavior, these investigators noted that communication techniques such as offering verbal and nonverbal encouragement and attention, ascertaining patients’ worries or concerns, and tailoring the treatment plan to the family’s daily routine were associated with improved parent satisfaction with their child’s care (Clark et al., 1998). After receiving the communication intervention, physicians were more likely to engage their patients/parents in discourse and education, the interactions were of shorter duration (22.8 minutes versus 27.1), and physicians who received the training wrote more anti-inflammatory prescriptions as compared to physicians who did not receive the training (Clark et al., 1998). Parents receiving care from physicians in the intervention group felt more confident in managing the child’s asthma at home (Clark et al., 1998). Thus, the quality of the communication during the medical encounter may have been more important than the duration of the visit (Clark et al., 1998).
Poor provider-parent communication during medical care visits may be due to either provider and/or parent factors. Treatment and diagnosis information may be misconstrued by the parent due to inadequate translation of instructions into laymen’s terms or lack of sufficient time to explain and demonstrate proper use of a particular medicine or regimen. Misinterpretation of diagnosis or inaccurate assignment of severity of the child’s asthma disease by the provider may occur. Providers often define a patient’s asthma in terms of severity based on symptoms (i.e., mild, mild-intermittent, severe), but the patient may define their asthma as “good” or ‘bad” (Ehrlich, 2005) based on restriction of activity or sleepless nights. Parents may define controlled asthma as the ability to attend school and play, even if symptoms persist, while providers define “asthma control” as being symptom free (Eiser & Morse, 2001; Goldman, Whitney-Saltiel, Granger, & Rodin, 1991). Striking, in a study of urban, low-income, minority children with asthma, 65% of the parents of children diagnosed with severe asthma reported their child in “good control” demonstrating the incongruence between provider and parental perception of symptom severity (Yoos, Kitzman, McMullen, Sidora-Arcoleo, & Anson, 2005). Parents may feel embarrassed to discuss minor symptoms or may feel they are wasting the provider’s time, which results in a lack of communication relating to critical details about their child’s asthma during a medical visit (Partridge & Hill, 2000). Ultimately, this inability to communicate details of care may lead to a misdiagnosis or under-treatment of the child’s asthma.
Barriers to Effective Provider-Child Communication
Barriers that prevent effective provider-child communication during a medical visit include provider time limitations and the inability to communicate on an appropriate developmental level with each child. The perception of both the parent and provider that having the child interact during the visit will prolong the length of the visit may explain parental interfering with their child’s active participation during the medical visit. Observations of children during medical care visits indicate that parents interfere with 52% of the “turns” or interactions that the provider directs to the child (Aronsson & Rundstrom, 1988). Although the pediatric medical visits does provide a privileged place of apprenticeship where the child can learn how to be a patient (Nova et al., 2005), the child may not be socialized by the parent regarding how to participate during a medical care visit (Tates & Meeuwesen, 2000), resulting in the child remaining silent during the medical visit.
Overview of Shared Decision Model
The shared-decision making model promotes an active partnership between the patient and provider. In shared decision making at least two participants are involved, both parties actively share in any treatment decision-making, information is shared between the parties, and both parties agree to the treatment decision (Charles, Gafni, & Whelan, 1997). There is no single protocol on how to accomplish shared-decision making. The process involves mutuality or equality in shared decision-making, so that if one partner is unwilling or unable to participate than the decision-making is not shared. If the provider is unwilling to share decision-making with the patient, the patient has no choice except to find another provider or submit to the provider’s recommendations. Both the provider and patient bring information and values to the relationship (Charles et al., 1997), so if the patient shares information about a treatment decision that he or she obtained by other means or sources, then the provider can endorse or refute this information to help the patient evaluate all treatment options. However, the provider’s role is to present the patient with expert treatment options (Charles et al., 1997) while allowing the patient to evaluate the options and make a choice. Shared-decision making is finalized when both parties agree on the treatment option even if the provider believes that the patient may be better off with another treatment but through negotiation the provider agrees to endorse the patient’s decision.
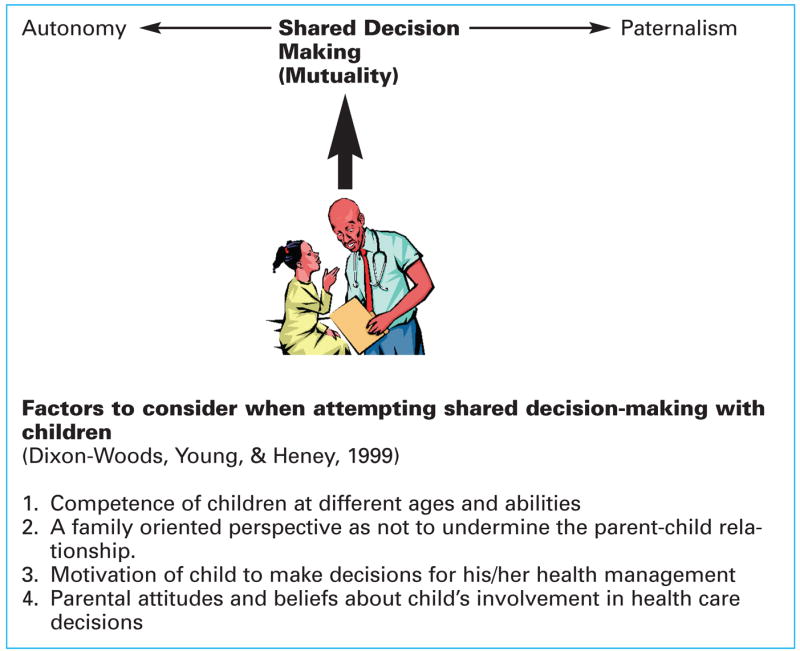
As seen in Figure 1, mutuality or shared decision-making is on a continuum of two extremes of autonomy or paternalism. In the triadic relationship, shared decision- making will ideally include the child, parent, and provider. At the paternalistic end of the continuum, the child has little involvement in the decision making for his or her health. Alternatively, at the autonomy end of the continuum the parent may allow the child to be involved with health care decisions but the child will have less of a relationship with the provider. Shared decision making promotes the triadic relationship by promoting parents and providers partner with the child and include the child’s perspective in their health care decisions (Dixon-Woods, Young, & Heney, 1999).
Figure 1.
Shared Decision Making in Clinical Care of Children
Although this is a very simplistic model of the complex interaction between provider and patient, it does convey the dynamic, constantly changing provider-patient relationship. Paternalism or provider dominance in decision- making is at one extreme and focuses on the provider’s unwillingness to share decision-making with the patient. In a paternalistic approach, parents are less satisfied with their child’s care than when parents are exposed to a shared decision-making process (Merenstein et al., 2005). At the other extreme is autonomy where the patient is the sole decision-maker and the provider participates only by transferring information to the patient (Charles et al., 1997). Mutuality, the mid-point between these two extremes, promotes an interaction between provider and patient that is a dynamic exchange with both parties seeking a common goal or shared purpose (Henson, 1997).
Shared decision-making is reported to be more acceptable to younger, educated patients (Frosch & Kaplan, 1999); however, few studies have used this model with children. One such study noted that practitioners treating children with cerebral palsy focused on the usefulness and intensity of interventions while the parents and children focused on implementation of the recommended medical interventions. However, analysis of the interactions revealed more unilateral than shared decision making between the parent and child (Young, Moffett, Jackson, & McNulty 2006). Moreover, parents of children with genetic conditions described the parent-child-provider shared-decision making as an unfolding practice that continues throughout childhood. Parents valued the practitioner-child sharing of information regarding diagnosis during clinic visits and reported they lacked confidence in sharing this information to their child without the practitioner available (Gallo, Angst, Knafl, Hadley, & Smith 2005). Both studies indicate the need for practitioners to partner with parents to share accurate information with the child based on the child’s developmental level and the parent’s attitudes and beliefs.
Effective Communication Strategies to Use with Children with Asthma
Creating a shared decision model for children is best learned by direct and indirect interactions with their provider and parents during the medical visit (Tates et al., 2002). Allowing the child to participate requires some specific guidelines for providers to respect during the interaction. Assessing the child’s competence at different ages and abilities (including learning disabilities) can be achieved by asking the child to count up to 100 or spell simple words (Dixon-Woods, Young, & Heney, 1999).
Children can be involved in decision making related to their treatment. Once the child’s competency level is assessed, the child can be provided with the opportunity to ask questions about his or her treatment regimen, i.e., why he or she needs to avoid an asthma trigger, why some medications need to be taken during school. Use of prompts such as an asthma coloring book (Naumann et al., 2004) or cue card devices that include picture identification for asthma triggers, asthma symptoms, and medications can be used to start an asthma dialogue with a child or to reinforce medication instructions or symptom identification and home protocol for treatment of symptoms. For children with frequent and/or traumatic asthma episodes, a more in-depth approach may be needed such as having children draw pictures to illustrate how they feel or use metaphors or puppets to demonstrate body functioning and symptoms (Hart & Chesson, 1998).
More specific communication techniques to use with children include use of visual aids, turn-taking, clarifying communication, and role modeling (Dyer & Luce, 1996).
Visual aids
A visual aid can be an effective communication tool for use with children. A coloring book, comic book, or photo novella for asthma symptoms can be provided during clinic visits to prompt children to talk about their asthma. Asking children to list what they don’t like about their asthma can be a prompt to discuss issues of nonadherence to medications or environmental control recommendations. Use of a dollhouse or pictures of rooms in a home are another effective prompt for children to identify asthma triggers in the home and how to avoid exposure to the environmental triggers. Some children may need prompting by the provider to talk about asthma with phrases such as, “Tell me when you know to take your asthma medicine?” or “What do you think about taking this medicine everyday?” or “What do you think about staying away from your friend’s house because he has a cat?” When explaining medical procedures such as spirometry or peak flow devices, providers can use short explanations and show children graphic results of the test. This provides children with a concrete image of their lung function and asthma control.
Turn-taking
In turn-taking, the provider teaches and encourages the child to take turns talking with the provider during the medical encounter. This includes teaching the parent that the child will be allowed to take turns during the visit and will be encouraged to talk. If the parent repeatedly prevents the child from having a turn to talk during the visit, then the provider can intervene by directly asking the child to describe his or her symptoms, routine for taking medicine, or the taste of the medicine. Parents can be taught that turn-taking can be practiced at home during family conversations by teaching the child to ask for a turn to speak during a conversation among family members.
Eliciting attention/requesting help
This technique can be taught by modeling correct behavior with the child during the clinic visit. Children can be taught to say, “Excuse me Dr. Jones, I would like to tell you something about my medicines.” Another option for children is to ask for help with their asthma medications. For example, children can be taught to say “Dr. Jones I need some help with taking my medications. May I tell you about my medicines?”
Clarifying communication with children
At the end of the medical encounter, school age children should be asked to rephrase their understanding of the treatment instructions in their own vocabulary. Misinformation should be corrected immediately so that children learn correct health information. For example, if the child states that he or she would not tell anybody at school about wheezing after recess, the child should be corrected to inform the teacher, the school nurse, or principal whenever he or she start to wheeze or become short of breath at school. By asking the child to rephrase the information, the provider learns what the child assimilated during the encounter (O’Neill, 2002) and if there is any misinformation.
Role modeling
Role-playing is a positive force in shaping the performance of school age children and has been used in several behavioral programs for bedwetting and reducing fears of medical treatment programs (Dixon & Stein, 2000). Role modeling by the provider during a clinic visit can be very effective in teaching children how to communicate during a medical encounter. Use of scenarios with children prevents personalizing the experience for the child.
One example of a scenario is listed in Table 1. The scenario demonstrates that it is helpful for the child to disclose medication nonadherence to the provider to enable the two of them to problem solve the issue together and to agree that the child will continue to take the medication. The child learns that the provider is willing to partner with him or her to problem solve the nonadherence to medication use.
Table 1.
Example of Role Play Scenario with Children
| Tanya is a nine-year-old girl with asthma who does not like the taste in her mouth after she uses her asthma medication inhaler (list controller medication name, i.e., flovent, beclovent). She is afraid to tell her mother or doctor because she believes she will be punished for not taking her medicines. You (the child) pretend that you are Tanya and I will be the doctor. |
| Tanya: Sometimes I don’t take my medicine because it tastes bad for me after I use my inhaler. |
| Doctor: I’m glad you told me this about your medicine because I can help you with getting rid of the bad taste. Let’s have you try to rinse out your mouth with some mouthwash after you use your Flovent inhaler. That should help get rid of the bad taste. |
| Tanya: I don’t use mouthwash, but maybe my mother will help me get some. |
| Doctor: Mrs. Henson, could you get Tanya some mouthwash and help her rinse out her mouth after she uses her Flovent to get rid of the bad taste? This means that we can all work together to get rid of the bad taste in her mouth due to her medicine. |
Teaching Parents How to Deliver Medical Information to Children
In a study of children with genetic conditions, most parents reported receiving no information about how to share medical information with their child (Gallo, Angst, Knafl, Hadley, & Smith, 2005). To confidently and accurately disclose the information to the child, parents may need a demonstration or modeling of how to integrate the information into the child’s self-concept and adaptation to the condition (Gallo et al., 2005). Using role modeling during medical encounters with the family may provide concrete examples of medical explanations for parents to use at home. Providers can offer parents strategies on how to give general information about the condition, procedures, and treatments based on the child’s questions and interest (Gallo et al., 2005).
A Basic Right
Children’s involvement in their health care is considered a basic right (De Winter, Baerveldt, & Kooistra, 1999). Currently, the provider and parent dominate the communication in many pediatric medical encounters (Tates & Meeuwesen, 2001). Allowing children to actively participate in decisions about their own health care may enhance children’s self-confidence as well as improve their self-management skills (Vessey & Miola, 1997; Holtzheimer, Mohay, & Masters, 1998; De Winter et al., 1999). The goal of all pediatric asthma visits for school-aged children is to change dyadic interactions between the provider and parent into triadic interactions that include the provider, parent, and child.
Acknowledgments
This research was supported by the National Institute of Nursing Research No. NR008544 and NR05050.
Footnotes
Note: The authors reported no actual or potential conflict of interest in relation to this continuing nursing education article.
Contributor Information
Arlene M. Butz, Arlene M. Butz, ScD, MSN, CPNP, is an Associate Professor, Johns Hopkins University Schools of Medicine and Nursing, Baltimore, MD
Jennifer M. Walker, Jennifer M. Walker, BS, MHS, is Senior Research Analyst, Johns Hopkins University School of Medicine, Department of Pediatrics, Baltimore, MD
Margaret Pulsifer, Margaret Pulsifer, PhD, is Psychologist, Massachusetts General Hospital, Harvard Medical School, Psychology Assessment Center, Boston, MA.
Marilyn Winkelstein, Marilyn Winkelstein, PhD, RN, is Independent Contractor, Johns Hopkins University School of Medicine, Department of Pediatrics, Baltimore, MD.
References
- Aronsson K, Rundstrom B. Child discourse and parental control in pediatric consultations. Text. 1988;8:159–184. [Google Scholar]
- Berwick D. A user’s manual for the IOM’s “Quality Chasm” report. Health Affairs (Millwood) 2002;21:80–90. doi: 10.1377/hlthaff.21.3.80. [DOI] [PubMed] [Google Scholar]
- Broome ME. Consent (assent) for research with pediatric patients. Seminars in Oncology Nursing. 1999;15:96–103. doi: 10.1016/s0749-2081(99)80067-9. [DOI] [PubMed] [Google Scholar]
- Brown J, Stewart M, McCracken E, McWhinney IR. The patient-centered clinical method. 2. Definitions and application. Family Practice. 1986;3:75–79. doi: 10.1093/fampra/3.2.75. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, Whelan T. Shared Decision-Making in the medical encounter: What does it mean? (Or it takes at least two to tango) Social Science and Medicine. 1997;44:681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- Clark NM, Gong M, Schork A, Evans D, Roloff D, Hurwitz M, Maiman L, Mellins RB. Impact of education for physicians on patient outcomes. Pediatrics. 1998;101:831–836. doi: 10.1542/peds.101.5.831. [DOI] [PubMed] [Google Scholar]
- De Winter M, Baerveldt C, Kooistra J. Enabling children: Participation as a new perspective on child-health promotion. Child: Care, Health and Development. 1999;25:15–25. doi: 10.1046/j.1365-2214.1999.00073.x. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. The Role of the physician in the emerging health care environment. Western Journal of Medicine. 1998;168:328–333. [PMC free article] [PubMed] [Google Scholar]
- Dixon-Woods M, Young B, Heney D. Partnerships with children. British Medical Journal. 1999;319:778–780. doi: 10.1136/bmj.319.7212.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon SD, Stein MT. Pediatric behavior and development. 3. St. Louis, MO: Mosby; 2000. Encounters with Children. [Google Scholar]
- Dyer K, Luce SC. Teaching practical communication skills. Washington, DC: American Association on Mental Retardation; 1996. Innovations. [Google Scholar]
- Ehrlich P. BCBL Panel of the Asthma and Allergy Foundation of America. Improving asthma control: Talk is not cheap. Annals of Allergy, Asthma and Immunology. 2005;94:415–418. doi: 10.1016/s1081-1206(10)61111-8. [DOI] [PubMed] [Google Scholar]
- Eiser C, Morse R. The measurement of quality of life in children: Past and future perspectives. Journal of Development and Behavioral Pediatrics. 2001;22:248–256. doi: 10.1097/00004703-200108000-00007. [DOI] [PubMed] [Google Scholar]
- Frosch DL, Kaplan RM. Shared decision making in clinical medicine: Past research and future directions. Development and evaluation of a decision instrument. American Journal of Preventive Medicine. 1999;17:285–294. doi: 10.1016/s0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- Gallo AM, Angst D, Knafl KA, Hadley E, Smith C. Parents sharing information with their children about genetic conditions. Journal of Pediatric Health Care. 2005;19:267–275. doi: 10.1016/j.pedhc.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Goldman SL, Whitney-Saltiel D, Granger J, Rodin J. Children’s representations of “everyday” aspects of health and illness. Journal of Pediatric Psychology. 1991;16:747–766. doi: 10.1093/jpepsy/16.6.747. [DOI] [PubMed] [Google Scholar]
- Golin CE, DiMatteo MR, Gelberg L. The Role of the patient participation in the doctor visit. Implications for adherence to diabetes care. Diabetes Care. 1996;10:1153–1164. doi: 10.2337/diacare.19.10.1153. [DOI] [PubMed] [Google Scholar]
- Greenfield S, Kaplan SH, Ware WE., Jr Expanding patient involvement in care: Effects on blood sugar control and quality of life in diabetes. Journal of General Internal Medicine. 1988;3:448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Juniper EF, Griffith LE, Feeny DH, Ferrie PJ. Children and adult perceptions of childhood asthma. Pediatrics. 1997;99:165–168. doi: 10.1542/peds.99.2.165. [DOI] [PubMed] [Google Scholar]
- Hart C, Chesson R. Children as Consumers. British Medical Journal. 1998;316:1600–1603. doi: 10.1136/bmj.316.7144.1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halterman JS, Aligne CA, Auinger P, McBride JT, Szilagyi PG. Inadequate therapy for asthma among children in the United States. Pediatrics. 2000;105:272–276. [PubMed] [Google Scholar]
- Henson RH. Analysis of the concept of mutuality. Image. 1997;29:77–81. doi: 10.1111/j.1547-5069.1997.tb01144.x. [DOI] [PubMed] [Google Scholar]
- Holtzheimer L, Mohay H, Masters IB. Educating young children about asthma: Comparing the effectiveness of developmentally appropriate asthma education videotape and picture book. Child: Care, Health and Development. 1998;24:85–99. doi: 10.1046/j.1365-2214.1998.00055.x. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) Crossing the quality chasm: A new health system of the 21st century. Washington, DC: National Academy Press; 2001. Committee on Quality of Health Care in America. [Google Scholar]
- Kaplan SH, Greenfield S, Ware WE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Medical Care. 1989;27:S110–127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication. 1. Doctor-patient interaction and patient satisfaction. Pediatrics. 1968;42:855–857. [PubMed] [Google Scholar]
- Levenstein JH, McCracken EC, McWhinney IR, Stewart MA, Brown JB. The patient- centered clinical method. A model for the doctor-patient interaction in family medicine. Family Practice. 1986;3:24–30. doi: 10.1093/fampra/3.1.24. [DOI] [PubMed] [Google Scholar]
- Merenstein D, Diener-West M, Krist A, Pinneger M, Cooper LA. An assessment of the shared- decision model in parents of children with acute otitis media. Pediatrics. 2005;116:1267–1275. doi: 10.1542/peds.2005-0486. [DOI] [PubMed] [Google Scholar]
- Naumann PL, Huss K, Calabrese B, Smith T, Quartey R, Van de Castle B, Lewis C, Hill K, Walker J, Winkelstein M. A+ Asthma rural partnership coloring for health: An innovative rural asthma teaching strategy. Pediatric Nursing. 2004;30:490–494. [PubMed] [Google Scholar]
- Nova C, Vegni E, Moja EA. The physician-patient-parent communication: A qualitative perspective on the child’s contribution. Patient Education and Counseling. 2005;58:327–333. doi: 10.1016/j.pec.2005.02.007. [DOI] [PubMed] [Google Scholar]
- O’Neill KA. Kids speak: Effective communication with the school-aged/adolescent patient. Pediatric Emergency Care. 2002;18:137–140. doi: 10.1097/00006565-200204000-00018. [DOI] [PubMed] [Google Scholar]
- Pantell RH, Stewart TJ, Dias JK, Wells P, Ross AW. Physician communication with children and parents. Pediatrics. 1982;70:396–402. [PubMed] [Google Scholar]
- Partridge MR, Hill SR. Enhancing delivery of care for people with asthma: The role of communication, education, training and self-management. European Respiratory Journal. 2000;16:333–348. doi: 10.1183/09031936.00.16233400. [DOI] [PubMed] [Google Scholar]
- Roter DL. The enduring and evolving nature of the patient-physician relationship. Patient Education and Counseling. 2000;39:5–15. doi: 10.1016/s0738-3991(99)00086-5. [DOI] [PubMed] [Google Scholar]
- Stewart MA. Effective physician-patient communication and health outcomes: A review. Canadian Medical Association Journal. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- Tates K, Meeuwesen L. Doctor-parent-child communication: A (re) view of the literature. Social Science and Medicine. 2001;52:839–851. doi: 10.1016/s0277-9536(00)00193-3. [DOI] [PubMed] [Google Scholar]
- Tates K, Meeuwesen L. “Let mum have her say”: Turn taking in doctor-parent-child communication. Patient Education and Counseling. 2000;40:151–162. doi: 10.1016/s0738-3991(99)00075-0. [DOI] [PubMed] [Google Scholar]
- Tates K, Meeuwesen L, Elbers E, Bensing J. “I’ve come for his throat”: Roles and identities in doctor-parent-child communication. Child: Care, Health & Development. 2002;28:109–116. doi: 10.1046/j.1365-2214.2002.00248.x. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. USDHHS PHS.NIH. Expert Panel Report 2: Guidelines for the diagnosis and management of asthma. (Publication No. 97-4051) Washington, DC: National Institutes of Health; 1997. National Asthma Education and Prevention Program. [Google Scholar]
- United States Department of Health and Human Services. USDHHS PHS.NIH. Guidelines for the diagnosis and management of asthma-Update on selected topics 2002 (Publication No.02-5075) Washington, DC: National Institutes of Health; 2002. National Asthma Education and Prevention Program. [Google Scholar]
- van Dulmen A. Children’s contributions to pediatric outpatient encounters. Pediatrics. 1998;102:563–568. doi: 10.1542/peds.102.3.563. [DOI] [PubMed] [Google Scholar]
- Vessey JA, Miola ES. Teaching adolescents self-advocacy skills. Pediatric Nursing. 1997;23:53–56. [PubMed] [Google Scholar]
- Winkelstein M, Huss K, Butz A, Eggleston P, Vargas P, Rand C. Factors associated with medication self-administration in children with asthma. Clinical Pediatrics. 2000;39:337–345. doi: 10.1177/000992280003900603. [DOI] [PubMed] [Google Scholar]
- Wissow LS, Roter D, Bauman LJ. Patient-provider communication during the emergency department care of children with asthma. The National Inner-city Asthma Study. Medical Care. 1998;36:1439–1450. doi: 10.1097/00005650-199810000-00002. [DOI] [PubMed] [Google Scholar]
- Yoos HL, Kitzman H, McMullen A, Sidora-Arcoleo K, Anson E. The language of breathlessness: Do families and health care providers speak the same language when describing asthma symptoms? Journal of Pediatric Health Care. 2005;19:197–205. doi: 10.1016/j.pedhc.2005.01.010. [DOI] [PubMed] [Google Scholar]


