Summary
Objectives
To assess the ability of partners and clinicians to make proxy judgements on behalf of patients with prostate cancer relating to selection of life priorities and quality of life (QoL).
Design
47 consecutive patients with histologically proven adenocarcinoma, and their partners, were recruited. The partners were asked to assess, by proxy, the QoL of the patient by completion of a series of interview-led questionnaires assessing global QoL (SEIQoL-DW), health-related QoL (FACT-P) and overall QoL (visual analogue score [VAS]). The patients' clinicians were asked to complete the SEIQoL-DW and VAS by proxy as soon as possible after a consultation with the patient.
Setting
Patients with histologically proven adenocarcinoma, their partners and their clinicians.
Main outcome measures
Proxy scores for SEIQoL-DW, FACT-P and VAS, as provided by partners and clinicians.
Results
25 partners made a proxy assessment of the patients. The results showed that partners were able to select similar QoL cues to those of the patients (Spearman-Rank correlation 0.89). Comparison of the QoL scores obtained from patients and partners in proxy using the questionnaires showed no statistically significant difference (paired t-test). Urologists were poor predictors of areas of life (cues) that were important to their patients. The doctors overemphasized the importance of survival, postoperative complications, urinary symptoms, sexual ability, activities of daily living and finance, but underestimated the importance of wife, family, home and religion. Comparison of the QoL scores obtained from patients and urologists by proxy showed a significantly lower score when assessed by urologists using the SEIQoL-DW questionnaire.
Conclusions
Partners are able to accurately assess, by proxy, the areas of life that are of importance to patients. Clinicians, however, who are charged with making decisions on behalf of patients, are very poor judges of their patients' life priorities and QoL. This illustrates that conventional views held by most doctors regarding the priorities patients set themselves when planning treatment should be called into question and consequently suggests that the way in which doctors and patients arrive at treatment decisions must be reviewed.
Introduction
Proxy assessment (i.e. assessment of one individual by another) occurs frequently in medicine. In general it is good clinical practice to involve partners in management discussions, but when patients are seriously ill the partner can provide vital insight into the patient's quality of life (QoL) priorities and their perceived feelings and wishes.
The majority of management decisions are made following discussions between patient and doctor and consequently the clinician has to make some assumptions and judgements on behalf of the patient. This is clearly a difficult process as the doctor and patient commonly do not know each other well and therefore important clinical decisions could at times be based on an incorrect assessment of the patient's expectations. Despite this, it is generally assumed that clinicians are capable of making proxy judgements and therefore are able to make appropriate management decisions for their patients.
Opinion from the published literature seems divided on whether health care professionals or relatives can accurately make a proxy assessment.1–3 In general the literature supports the viability of employing individuals other than clinicians to assess patient QoL.4–8 In addition, there is some evidence to suggest that proxy assessment is not only dependent on whether the assessor was a relative or health care professional but is influenced by the QoL dimension under consideration.9
This study aims to assess the ability of clinicians and partners to make proxy judgements on behalf of patients with prostate cancer relating to selection of life priorities and QoL. This study was not a comparison of QoL between prostate cancer patients.
Patients and methods
Partners' proxy assessment
A cohort of 47 newly diagnosed patients with partners and with histologically proven adenocarcinoma was recruited to participate in the study. As the hypothesis being tested was whether or not partners and urologists were able to accurately assess QoL by proxy, all stages and proposed treatments were included. Those patients for whom English was not their first language were excluded. Consent was obtained from both patient and partner. The partners were asked, by proxy, to assess the QoL of the patient by completion of a series of interview-led questionnaires. Patient assessments were performed at the same visit, in confidence and independent of the partner. Assessment was made after diagnosis and discussion but before treatment.
Several different instruments were used to assess patient QoL.
Global quality of life
This was measured using the Schedule for the Evaluation of Individualised Quality of Life-Direct Weighting (SEIQoL-DW).10–14 This interview-led questionnaire is based on the individuals' personal view of life and allows patients to judge their own QoL by selecting a specified number of domains which they deem to be important to them as individuals.
Using the SEIQoL-DW, QoL was elicited in the following way:
Cue Elicitation: the patient or proxy was asked to name the five most important areas of their own or their partner's life that were central to QoL. These are called cues.
Level of functioning of the cues: the patients were asked to rate the current status of each cue against a visual analogue score (VAS) ranging from best possible to worst possible level of functioning for this cue.
Eliciting cue weights: the cue weights in the SEIQoL-DW were derived directly from a coloured pie chart specially designed for the purpose, where the circle is subdivided into 100 percentage points. Each of the categories could be weighted from 1–100, as long as the total for all five categories was 100. This disk was presented to the recipient with each colour sector labelled with their elicited QoL cues. When presented, each cue was of similar size. The recipient then moved the sectors in the disk until the patient or proxy was content they represented his/the patient’s relative weighting of the categories.
Calculation: the final QoL score was derived by mathematical calculation using the formula: QoL = Σ(cue levels × cue weights). The results would be within the range of 0 to 100.
Health-related quality of life
Health-related QoL was assessed using the Functional Assessment of Cancer Therapy-Prostate (FACT-P) questionnaire. FACT-P is a prostate cancer-specific modification of FACT-G, developed by Cella et al.,15 and is a well-established and validated self-administered questionnaire.16 FACT-P retains the same sections as the FACT-G, but has an extra section containing additional questions relating to specific urological symptoms and side-effects from treatment regimens. In total there are 46 questions. The questionnaire was decoded according to the FACT-P administration manual.17
Overall quality of life
Overall quality of life was evaluated using a simple VAS.18
Urologists' proxy assessment
An assessment was made of the ability of urologists to make a proxy QoL evaluation on behalf of their patients.
As soon as possible after a consultation with the patient where treatment regimens had been described, the clinicians were asked to select patient cues by proxy and complete the SEIQoL-DW and VAS.
Results
Partners' proxy assessment
Twenty-five partners made a proxy assessment of the patients. Of the remainder, three patients did not want their partner to participate and eight partners refused to take part. The remaining 11 partners were willing to participate but were unable to be present on the day.
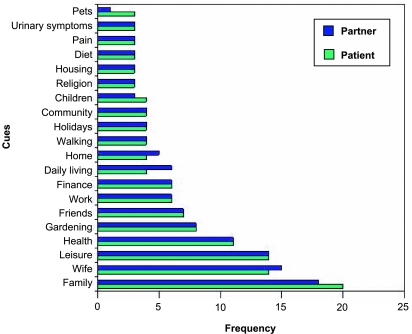
Nominated quality of life cues
The distribution of cues selected is shown in Figure 1, which compares cues selected by patients to those selected by their partners by proxy. Only cues nominated more than once are illustrated. The cues selected by both patients and partners were very similar. Family, wife, leisure, health and gardening were the most frequently cited cues. Furthermore, it was noted that partners and patients selected leisure, health, gardening, friends, work and finance with the same frequency. Using Spearman-Rank correlation to analyse the relationship between the cues nominated by the patient and the partner by proxy, a correlation factor of 0.89 was derived, indicating a high similarity in the cues selected.
Figure 1.
Comparison of cues selected by patients and by partners by proxy
Comparison of quality of life scores
The mean global QoL score for the patients using the SEIQoL-DW was 86.6 ± standard deviation of 10.8. The SEIQoL-DW questionnaire derives a score from 0 to 100, where 0 is the worst possible QoL and 100 the best. The partner's proxy assessment had a mean SEIQoL-DW score of 88.4 ± 12.1. Using the paired t-test, a comparison was made between the obtained SEIQoL-DW scores. These results showed that there was no significant difference between the mean scores obtained from patients and partners. These results indicate that partners were able to accurately predict, by proxy, those areas (cues) that were important to the patient's lives. Furthermore, these cues were accurately rated and weighted to give a similar overall QoL score.
FACT-P scores
The version of FACT-P used had a maximal score of 230. The mean health-related QoL score for patients using FACT-P was 150 ± 10.5. Partners gave a mean FACT-P score of 140 ± 6.1. The results were compared using the paired t-test and the difference was not statistically significant. These results indicate that partners were able to predict and rate, by proxy, those areas of health related to QoL.
Visual analogue scores
The mean overall QoL score for patients using the VAS was 68 ± 24.8 out of a possible 100. The partners estimation of the patients' QoL gave a mean VAS score of 65 ± 22.3. The results were compared using the paired t-test. As with the SEIQoL-DW and FACT-P scores, no significant differences were found between patients and their partners. These results indicate that partners were able to predict and rate, by proxy, overall QoL using a simple VAS.
Urologists' proxy sssessment
It was possible to obtain a proxy assessment from the urologists for 18 patient consultations carried out within a short time period after seeing the patient.
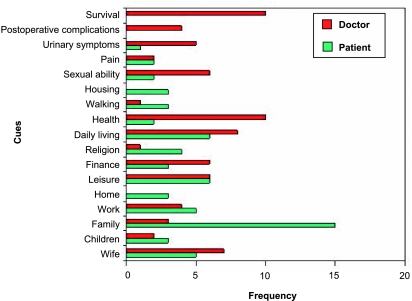
Nominated quality of life cues
The distribution of cues selected is shown graphically in Figure 2, which compares cues selected by patients with those chosen by their clinician by proxy. Only cues selected more than once by either group are shown. Figure 2 illustrates that urologists were poor predictors of areas of life (cues) that were important to their patients. The most striking finding from comparison of the cues was that the clinicians thought survival was important to nine patients (50%), whereas none of the patients mentioned this as being important to them. The doctors overemphasized the importance of postoperative complications, urinary symptoms, sexual ability, activities of daily living and finance. By contrast they underestimated the importance of wife, family, home and religion. Furthermore, urologists did not cite home (as in home life) or housing (as in buildings) as a cue.
Figure 2.
Comparison of cues selected by patients and by doctors by proxy
Comparison of quality of life scores
The clinicians underestimated patient QoL using both the SEIQoL-DW and the VAS. The mean QoL score for the patients using the SEIQoL-DW was 87.3 ± 11.1. The urologists' proxy assessment of their patients, however, had a mean SEIQoL-DW score of 67.6 ± 20.8. Using the paired t-test, a comparison was made between the SEIQoL-DW results obtained from both patient and urologist. A significant difference existed between the two groups (P=0.004).
Comparisons between those VAS obtained from patients and doctors by proxy were made. The mean QoL score for the patients using the VAS was 83.1 ± 14. The clinicians predicted a mean VAS score of 72.4 ± 14. The results were again compared using the paired t-test. Although there was a difference between these groups it failed to reach statistical significance (P=0.14).
Discussion
This study has shown that partners are able to accurately assess the areas of life that are of importance to patients. Clinicians, however, are very poor judges of their patients' life priorities.
The strength of this study was that it attempted to examine an important area of QoL assessment that is seldom covered in other research projects. In keeping with other QoL studies there are, however, some weaknesses in the methodology. The clinicians used for comparison with the patients' partners were hospital urologists. It was expected that this group would have less understanding of their patients' lives than the partners, many of whom had known the patients for many years. However, the authors felt it was important to use this group of clinicians as it is these same doctors who are making, in consultation and discussion with the patients, important treatment and life decisions. Just how poor clinicians are at judging their patients lives, however, could not have been envisaged. It would have been interesting to have asked the patients' general practitioners the same questions to see whether the ability to assess QoL by proxy is correlated to the length of time a clinician has known the patient. Unfortunately it was felt to be too logistically complicated to do this with this study.
The findings of this study are comparable to other, albeit limited, work in this area. In general terms the published literature indicates doctors are poor at predicting QoL whereas partners are much better.1–5 The only other published study to examine prostate cancer was a Dutch study in which the authors concluded that spouses of men with metastatic prostate cancer evaluate patient's physical and psychosocial functioning, symptoms and overall QoL with a fair degree of accuracy.6
The most frequently cited patient and partner cues were family, wife, leisure, health and gardening. In contrast, urologists frequently picked areas of their patient's lives (cues) that were not important to patients and failed to recognize areas that were (family, homelife, gardening, etc). However, it was surprising that although all the patients had been diagnosed with prostate cancer, survival and postoperative complications such as urinary incontinence were not cited by either patient or partner but were very commonly perceived by urologists to be of importance. This illustrates that conventional views held by most doctors regarding the priorities patients set themselves when planning treatment should be called into question and consequently suggests that the way in which doctors and patients arrive at treatment decisions need review.
In addition to poor cue selection, urologists were also unable to accurately rate and weight patient cues whereas partners did so with extreme accuracy. The results also indicate that partners were able to accurately assess both global and health-related QoL by proxy using SEIQoL-DW, FACT-P and VAS.
There are a number of possible reasons to explain the poor performance of clinicians in this study. In general, doctors commonly focus on those areas for which they are responsible and can exert some influence. Cues such as survival, postoperative complications, urinary symptoms and sexual function are all areas over which clinicians feel they have some control. These are also areas in which clinicians have traditionally been held accountable in terms of commonly measured outcomes and published research. In addition, even after a number of clinic visits, the clinician has had direct contact with the patient for only short periods of time and therefore cannot be expected to know the patient well enough to form complex judgements about their psychosocial make up and expectations. By contrast, in this relatively elderly population relationships were generally longstanding and over the years partners had therefore developed a deeper knowledge and understanding of each other, leaving them better placed to assist in decision making.
The implications of these findings are very important to clinical practice. The following are proposed:
Clinicians should be aware that patients may not have the same values and expectations of treatment as themselves and that sometimes even survival and the avoidance of postoperative complications may not constitute a high priority. Although time in the consultation is short, doctors should be encouraged to ask specific questions which might establish what goals patients have relating to their disease and its treatments. Formal training may facilitate this process.
Asking patients to complete a simple questionnaire before the consultation would identify important issues. We would suggest such a questionnaire should include direct questions concerning physical symptoms, psychological functioning and QoL priorities. An example of a suitable questionnaire is the Prostate Cancer Partner Questionnaire, which was developed and validated for patient and partner use simultaneously.19,20 Results from such a questionnaire could then form the basis for further and more detailed discussion of patient's expectations, wishes and priorities.
Partners have been shown to have an excellent understanding of the patients' symptoms and QoL; however, they are rarely involved in the consultation process. Partners should therefore be actively encouraged to attend the outpatient clinic with the patient and where possible be involved in discussion and decision-making.
Patients and partners should be given appropriate written information about their disease and the treatment options and given time to assimilate this information before important management decisions are taken. In addition, clinic letters should be copied to patients, as recommended by the recent Department of Health Guidance document.20
Nurses have been shown previously to be better proxy assessors of patients than doctors21 and in recent years there has been increasing use of specialist nurse practitioners in most speciality areas. These nurses are able to spend longer with patients and partners and by developing a better understanding of their individual expectations and wishes, may enable more appropriate treatment choices to be made.
Conclusion
This study demonstrates that, in contrast to partners, urologists are poor assessors of the subjective QoL issues that are important to patients and upon which treatment choices for prostate carcinoma are based. Within the present system of relatively short consultations it is important that doctors are aware that the patient's goals may differ from their own and that specific questions may need to be asked to determine the patient's true feelings and therefore to target treatment more effectively. Utilizing clinical nurse practitioners and involving partners will facilitate this process. Use of this combined approach should ensure that decisions concerning the patient's disease and its treatments are made jointly between doctor and patient and therefore more appropriately reflect the patient's subjective QoL priorities and expectations.
Footnotes
DECLARATIONS —
Competing interests None declared
Funding None
Ethical approval This study was fully approved by the Local Research Ethics Committee
Guarantor RP
Contributorship All authors contributed equally
Acknowledgements
Grateful thanks to the Center on Outcomes, Research & Education, Evanston for allowing the free use of the FACT-P questionnaire.
References
- 1.Slevin M, Plant H, Lynch D, Drinkwater J, Gregory WM. Who should measure quality of life, the doctor or the patient? Br J Cancer. 1988;57:109–12. doi: 10.1038/bjc.1988.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sprangers M, Aaronson N. The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease: a review. J Clin Epidemiol. 1992;45:743–60. doi: 10.1016/0895-4356(92)90052-o. [DOI] [PubMed] [Google Scholar]
- 3.Higginson I, McCarthy M. Validity of the support team assessment schedule: do staffs’ ratings reflect those made by patients or their families? Pall Med. 1993;7:219–28. doi: 10.1177/026921639300700309. [DOI] [PubMed] [Google Scholar]
- 4.Sneeuw K, Aaronson N, Osoba D, et al. The use of significant others as proxy raters of the quality of life of patients with brain cancer. Med. Care. 1997;35:490–506. doi: 10.1097/00005650-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Sneeuw K, Aaronson N, Sprangers M, Detmar S, Wever LD, Schornagel JH. Comparison of patient and proxy EORTC QLQ-C30 ratings in assessing the quality of life of cancer patients. J Clin Epidemiol. 1998;51:617–31. doi: 10.1016/s0895-4356(98)00040-7. [DOI] [PubMed] [Google Scholar]
- 6.Sneeuw K, Albertsen P, Aaronson N. Comparison of patient and spouse assessments of health related quality of life in men with metastatic prostate cancer. J Urol. 2001;165:478–82. doi: 10.1097/00005392-200102000-00029. [DOI] [PubMed] [Google Scholar]
- 7.Sigurdardottir V, Brandberg Y, Sullivan M. Criterion-based validation of the EORTC QLQ-C36 in advanced melanoma: the CIPS questionnaire and proxy raters. Qual Life Res. 1996;5:375–86. doi: 10.1007/BF00433922. [DOI] [PubMed] [Google Scholar]
- 8.Brunelli C, Costantini M, Di Giulio P, et al. Quality of life evaluation: when do terminal cancer patients and health-care providers agree? J Pain Symptom Manage. 1998;15:149–50. doi: 10.1016/s0885-3924(97)00351-5. [DOI] [PubMed] [Google Scholar]
- 9.Sneeuw K, Aaronson N, Sprangers M, Detmar S, Wever LD, Schornagel JH. Evaluating the quality of life of cancer patients: assessments by patients, significant others, physicians and nurses. Br J Cancer. 1999;81:87–94. doi: 10.1038/sj.bjc.6690655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hickey A, Bury G, O‘Boyle C, Bradley F, O’Kelly FD, Shannon W. A new short form individual quality of life measure (SEIQoL-DW): application in a cohort of individuals with HIV/AIDS. BMJ. 1996;313:29–33. doi: 10.1136/bmj.313.7048.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joyce C, Stewart T. Applied research in judgement: what should happen. Acta Psychologica. 1994;87:217–27. [Google Scholar]
- 12.O'Boyle C. Assessment of quality of life in surgery. Br J Surg. 1992;79:395–8. doi: 10.1002/bjs.1800790506. [DOI] [PubMed] [Google Scholar]
- 13.O'Boyle C, McGee H, Hickey A. The Schedule for the Evaluation of Individual Quality of Life (SEIQoL). Administration Manual. Dublin: Royal College of Surgeons in Ireland; 1993. [Google Scholar]
- 14.Waldron D, O'Boyle C, Kearney M, Moriarty M, Carney D. Quality of life measurement in advanced cancer: assessing the individual. J Clin Oncol. 1999;17:3603–11. doi: 10.1200/JCO.1999.17.11.3603. [DOI] [PubMed] [Google Scholar]
- 15.Cella D, Tulsky D, Gray G, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–9. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 16.Esper P, Mo F, Chodak G, Sinner M, Cella D, Pienta KJ. Measuring quality of life in men with prostate cancer using the functional assessment of cancer therapy – prostate instrument. Urology. 1997;50:920–8. doi: 10.1016/S0090-4295(97)00459-7. [DOI] [PubMed] [Google Scholar]
- 17.FACT-P. FACT-P Administration manual. Evanston: Center on Outcomes, Research & Education; 2001. [Google Scholar]
- 18.Waldron D, O‘Boyle C. Individual quality of life in palliative care. In: Joyce C, O’Boyle C, McGee H, editors. Individual quality of life: Approaches to conceptualisation and assessment in health. Reading, MA: Harwood Academic; 1998. pp. 197–211. [Google Scholar]
- 19.Cliff A, MacDonagh R. Psychosocial morbidity in prostate cancer 1. Design of a new questionnaire. BJU Int. 2000;86:829–33. doi: 10.1046/j.1464-410x.2000.00913.x. [DOI] [PubMed] [Google Scholar]
- 20.Department of Health. Copying letters to patients: good practice guidelines. London: DoH; 2003. [Google Scholar]
- 21.Cliff A, MacDonagh R. Psychosocial morbidity in prostate cancer 2. A comparison of patients and partners. BJU Int. 2000;86:834–9. doi: 10.1046/j.1464-410x.2000.00914.x. [DOI] [PubMed] [Google Scholar]