Summary
Background
Analysis of primary healthcare datasets offers the possibility to increase understanding of the epidemiology of acute uncommon conditions such as anaphylaxis, but these datasets remain under-exploited.
Aim
To investigate recent trends in the recorded incidence, lifetime prevalence and prescribing of adrenaline for anaphylaxis in England.
Methods
QRESEARCH is one of the world's largest national aggregated health databases containing the records of over nine million patients. We extracted data on all patients with a recorded diagnosis of anaphylaxis and calculated annual age-sex standardized incidence and lifetime period prevalence rates for each year from 2001–2005. We also analysed trends in adrenaline prescribing in those with a recorded diagnosis of anaphylaxis. National population figures were used to estimate numbers of people in England that have experienced anaphylaxis at some point in their lives.
Results
The age-sex standardized incidence of anaphylaxis was 6.7 per 100,000 person-years in 2001 and increased by 19% to 7.9 in 2005. Lifetime age-sex standardized prevalence of a recorded diagnosis of anaphylaxis was 50.0 per 100,000 in 2001 and increased by 51% to 75.5 in 2005. Prescribing of adrenaline increased by 97% over this period. By the end of 2005 there were an estimated 37,800 people that had experienced anaphylaxis at some point in their lives.
Conclusions
Recorded incidence, lifetime prevalence and prescribing of adrenaline for anaphylaxis all showed substantial increases in recent years. An estimated 1 in 1,333 of the English population have at some point in their lives experienced anaphylaxis.
Introduction
The American College of Allergy, Asthma and Immunology Epidemiology Working Group on Anaphylaxis recent international literature review highlighted the substantial gaps in our understanding of the epidemiology of anaphylaxis, noting that: ‘An improved epidemiologic understanding of this disorder would aid ongoing efforts to reduce morbidity and mortality from anaphylaxis and could provide important clues for primary prevention.’1 Particularly important are gaps in relation to describing the actual numbers of people at high risk of experiencing anaphylaxis, disease trends over time and identifying those at greatest risk of severe outcomes. Challengesto answering these questions include the inherent difficulties of mounting serial cross-sectional and prospective cohort studies of acute, short-lived and uncommon conditions such as anaphylaxis.2
In the absence of such population-based studies, exploitation of large national healthcare datasets, with their key strengths of large numbers and representative data, offers an important opportunity to develop insights into the epidemiology of anaphylaxis.3 Work from England studying hospital admissions for anaphylaxis has, for example, found rapid and sustained increases in the numbers of hospital admissions for anaphylaxis over the last decade, these data suggesting an underlying increase in the incidence of anaphylaxis.4–8
There are, however, important inherent limitations associated with extrapolating population estimates from hospital admission data in the case of anaphylaxis, as it seems likely that only a minority of those experiencing anaphylaxis in England are actually admitted as in-patients. Evidence suggests that the majority of cases of anaphylaxis are sent home from accident and emergency departments.9 Understanding how the epidemiology of anaphylaxis may be changing is also potentially problematic because of the risk of changing admission thresholds affecting findings. There has, furthermore, been the additional challenge posed by the fact that, until recently, English hospital data at national level have only provided measures of admission episodes rather than numbers of individual patients admitted, thereby rendering it impossible to assess the impact of repeated admissions of the same individual.8
Studying primary care databases, which are more likely to reflect the overall population picture of anaphylaxis than hospital in-patient episode data, should help to overcome some of these limitations. Building on our previous work using hospital datasets,4–8 we sought to describe trends in recorded diagnosis of anaphylaxis and prescribing for anaphylaxis in England during the five-year period between 1 January 2001 and 31 December 2005. Future planned work will seek to identify those at greatest risk of poor outcomes.
Methods
We used Version 10 of the QRESEARCH database, which is a very large nationally representative anonymized aggregated health dataset derived from 525 general practices throughout the UK.10 It contains data on over 30 million patient years of observation, these being derived from over nine million individual patients.
General practices were included in the analysis if they were based in England, were using the Egton Medical Information Systems (EMIS) software and had transmitted complete data to the central QRESEARCH repository for the period from 1 January 1999 to 31 December 2005. This stipulation for practices to be submitting data for a full two years prior to our period of interest was to ensure that practices had sufficient lead time to become accustomed to using their computing systems for routine work.
Four hundred and twenty-two (80%) of the QRESEARCH practices had complete data for England for the seven-year period in question (1999–2005), these practices yielding a total of 2,958,366 patients. Contributing practices were distributed throughout England and had an age-sex structure that was found to be directly comparable to the age-sex structure of the English population (data not shown).
Patients were included in the analysis year if they were registered for the entire analysis year in question. Patients who might have incomplete data (i.e. temporary residents, newly registered patients and those who joined, left or died during the year) were therefore not eligible for inclusion.
We considered patients to have anaphylaxis if they had a computer-recorded diagnostic Read code for anaphylaxis in their electronic health record for the relevant time period.
Incidence was defined as the number of new cases of disease diagnosed in a specific year, with the denominator of number of patient years of observation (this being calculated as a product of the number of patients registered with practices and their length of registration) being used to calculate incidence rates. Lifetime prevalence was defined as the numbers of people with a diagnosis of anaphylaxis recorded in the GP records on at least one occasion at any point in their lives; the denominator used to calculate the lifetime prevalence rate was the number of patients registered with the study practices.
Because of the known age and sex variations, we standardized rates by sex and five-year age bands using the estimated mid-year population estimates for England in each year as our reference population. These results were then scaled up to estimate the actual numbers of people with anaphylaxis in England. In order to better estimate the actual numbers of people affected by anaphylaxis, we calculated 95% confidence intervals around these estimates of lifetime prevalence and absolute numbers of people affected in 2005.11
In order to describe trends in prescribing of self-administered adrenaline, we extracted linked prescribing data in those with a recorded diagnosis of anaphylaxis and estimated numbers of prescriptions prescribed (which may or may not equate with the numbers of prescriptions dispensed) nationally for each of the five years.
Results
Age-sex standardization of rates
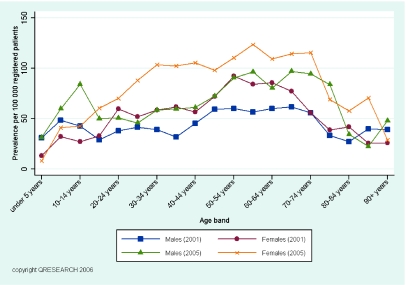
Figure 1 reveals how the lifetime prevalence of anaphylaxis varied very markedly by age and sex. In the pre-pubertal period, lifetime prevalence was highest in males, but then increased very rapidly in females, peaking during the fifth decade. These findings underscore the importance of age-sex standardization of data.
Figure 1.
Age-sex variations in lifetime prevalence of anaphylaxis per 100,000 registered patients for 2001 and 2005
Incidence rate of anaphylaxis and changes over time
Table 1 details the incidence rate of anaphylaxis for each of the five years of interest, these data showing an overall 19% increase during the period 2001–2005.
Table 1.
Incidence rate of anaphylaxis per 100,000 patient-years, 2001–2005
| Year | Age-sex standardized incidence rate/100,000 person-years | 95% CI |
|---|---|---|
| 2001 | 6.7 | 5.7–7.7 |
| 2002 | 6.6 | 5.7–7.6 |
| 2003 | 6.8 | 5.9–7.9 |
| 2004 | 8.5 | 7.5–9.6 |
| 2005 | 7.9 | 7.0–9.0 |
Lifetime prevalence rate of anaphylaxis and changes over time
Table 2 details the age-sex standardized lifetime prevalence rate of anaphylaxis for each of the five years of interest, these data revealing a 51% increase in recorded lifetime prevalence of anaphylaxis over this time period.
Table 2.
Lifetime prevalence of anaphylaxis per 100,000 registered patients, 2001–2005
| Year | Age-sex standardized prevalence rate/100,000 | 95% CI |
|---|---|---|
| 2001 | 50.0 | 47.5–52.7 |
| 2002 | 55.9 | 53.3–58.7 |
| 2003 | 61.8 | 59.0–64.7 |
| 2004 | 68.5 | 65.6–71.6 |
| 2005 | 75.5 | 72.4–78.7 |
Trends in adrenaline prescribing
Table 3 details the estimated numbers of community prescriptions in patients with anaphylaxis throughout England for each of the five years, these revealing a 97% increase in prescribing of adrenaline over the study period.
Table 3.
Estimated numbers of prescriptions for adrenaline in patients with a history of anaphylaxis in England, 2001–2005
| Year | Estimated number of prescriptions in England | 95% CI |
|---|---|---|
| 2001 | 10,700 | 9,900–11,600 |
| 2002 | 12,600 | 11,700–13,600 |
| 2003 | 13,300 | 12,400–14,300 |
| 2004 | 16,200 | 15,200–17,300 |
| 2005 | 21,100 | 19,900–22,300 |
Numbers of people with a history of anaphylaxis
The estimated numbers of people who have had anaphylaxis at some point in their lives increased from 24,700 (95%CI 23,500–26,000) in 2001 to 37,800 (95% CI 36,300–39,400), this 2005 estimate indicating that 1 in 1,333 of the English population had a lifetime prevalence of anaphylaxis.
Discussion
There has been a marked recent increase in recorded incidence and lifetime prevalence of anaphylaxis and prescribing of adrenaline in these patients.
Considering findings in relation to the published literature
The age-sex variations described in Figure 1 are in keeping with described patterns showing an interaction between age and gender.1,12 The American College of Allergy, Asthma and Immunology Epidemiology Working Group on Anaphylaxis found that the reported lifetime frequency of anaphylaxis varies internationally between 0.02–0.5% and our estimate of 75.5 per 100,000 or 0.08% in 2005 is comparable to these data.1 These esti mates are furthermore very comparable to the limited available data from other primary care datasets.13,14
Main strengths and limitations of this work
The main strengths of this study include our interrogation of an extremely large nationally representative dataset, the fact that all contributing practices used the same computing systems for electronically recording clinical data and the approach used to ensure that all contributing practices were accustomed to electronically recording routine data. The study design means that it was not subject to selection bias due to non-responders or recall bias. As recommended by the American College of Allergy, Asthma and Immunology Epidemiology Working Group on Anaphylaxis,1 our attempt to obtain various estimates of disease frequency is allowing a comprehensive picture of the epidemiology of anaphylaxis in England to emerge.4–8
There are a number of limitations that need to be considered when using databases of routinely collected data and these all potentially apply to this work. Most importantly, we were dependant on physician-recorded diagnosis of anaphylaxis and there may have been improvements in anaphylaxis recording over this time period. The relatively short time window over which trends were studied is another limitation, but this does also have the advantage of confining analysis to a period during which there were no changes in disease definition or classification.
Conclusions and implications for future research
This large national study reveals that the recorded incidence and lifetime prevalence of anaphylaxis increased in England during the first half of this decade. Further work is now needed to explore why these increases occurred and determine which of the increasing numbers of individuals with a history of anaphylaxis are at greatest risk of recurrent anaphylaxis and severe outcomes should a further episode occur.15 The changes in disease patterns described highlight the need for ongoing surveillance of the epidemiology of anaphylaxis.
Footnotes
DECLARATIONS —
Competing interests JHC is Director of QRESEARCH. JF was a statistician employed at QRESEARCH at the time the work was undertaken. AS gave evidence to the House of Commons Health Committee review on The provision of allergy services and the House of Lords inquiry, was part of the Department of Health Allergy Review Stakeholder Group and serves on the Scottish Executive's Review of Allergy Services in Scotland Working Group. He is PI on a Scottish Executive study investigating the epidemiology of allergic disorders in Scotland (Ref: CZG/2/252). JN was funded to provide epidemiological advice to the Department of Health during itsreview of services for allergy.
Funding NHS Health and Social Care Information Centre
Guarantor JHC
Contributorship AS, JHC and JN were involved in designing the study, with analysis conducted by JF and overseen by JHC. AS led the writing of the manuscript with all authors commenting on drafts
Acknowledgements
We would like to thank the contributing EMIS practices and patients and for EMIS for providing technical expertise in creating and maintaining QRESEARCH. We thank QRESEARCH staff (Govind Jumbu, Alex Porter, Mike Heaps and Richard Holland) for their contribution to data extraction and presentation. These findings have been reported in Primary care epidemiology of allergic disorders: analysis using QRESEARCH database 2001–2006
References
- 1.Lieberman P, Camargo CA, Bohlke K, et al. Epidemiology of anaphylaxis: findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy, Asthma Immunol. 2006;97:596–602. doi: 10.1016/S1081-1206(10)61086-1. [DOI] [PubMed] [Google Scholar]
- 2.Walker S, Sheikh A. Managing anaphylaxis: effective emergency and long-term care are necessary. Clin Exp Allergy. 2003;33:1015–8. doi: 10.1046/j.1365-2222.2003.01754.x. [DOI] [PubMed] [Google Scholar]
- 3.Anandan C, Simpson CR, Fischbacher C, Sheikh A. Exploiting the potential of routine data to better understand the disease burden posed by allergic disorders. Clin Exp Allergy. 2006;36:866–71. doi: 10.1111/j.1365-2222.2006.02520.x. [DOI] [PubMed] [Google Scholar]
- 4.Sheikh A, Alves B. Hospital admission for acute anaphylaxis: time trend study. BMJ. 2000;320:1441–4. doi: 10.1136/bmj.320.7247.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta R, Sheikh A, Strachan D, Anderson HR. Increasing hospital admission for systematic allergic disorders in England: analysis of national admission data. BMJ. 2003;327:1142–3. doi: 10.1136/bmj.327.7424.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta R, Sheikh A, Strachan D, Anderson HR. Burden of allergic disease in the UK: secondary analyses of national databases. Clin Exp Allergy. 2004;34:520–6. doi: 10.1111/j.1365-2222.2004.1935.x. [DOI] [PubMed] [Google Scholar]
- 7.Gupta R, Sheikh A, Strachan D, Anderson HR. Time trends in allergic disorders in the UK. Thorax. 2007;62:91–6. doi: 10.1136/thx.2004.038844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newton J. An epidemiological report for the Department of Health's review of services for allergy, 2006. Available from: http://www.dh.gov.uk/assetRoot/04/13/73/78/04137378.pdf (last checked 21 Jan 2007) [Google Scholar]
- 9.Stewart AG, Ewan PW. The incidence, aetiology and management of anaphylaxis presenting to an accident and emergency department. QJM. 1996;89:859–64. doi: 10.1093/qjmed/89.11.859. [DOI] [PubMed] [Google Scholar]
- 10.QRESARCH. Available from http://qresearch.org/ (last checked 23 June 2007) [Google Scholar]
- 11.http://www.statistics.gov.uk/statbase/Product.asp?vlnk=601&More=N (last checked 23 June 2007) [Google Scholar]
- 12.Sheikh A, Alves B. Age, sex, geographical and socioeconomic variations in admissions for anaphylaxis: analysis of four years of English hospital data. Clin Exp Allergy. 2001;31:1571–6. doi: 10.1046/j.1365-2222.2001.01203.x. [DOI] [PubMed] [Google Scholar]
- 13.Peng MM, Jick H. A population-based study of the incidence, cause and severity of anaphylaxis in the United Kingdom. Arch Intern Med. 2004;164:317–9. doi: 10.1001/archinte.164.3.317. [DOI] [PubMed] [Google Scholar]
- 14.Bohlke K, Davis RL, DeStefano F, Marcy SM, Braun MM, Thompson RS. Epidemiology of anaphylaxis among children and adolescents enrolled in a health maintenance organization. J Allergy Clin Immunol. 2004;1123:536–42. doi: 10.1016/j.jaci.2003.11.033. [DOI] [PubMed] [Google Scholar]
- 15.Mullins RJ. Anaphylaxis: risk factors for recurrence. Clin Exp Allergy. 2003;33:1033–40. doi: 10.1046/j.1365-2222.2003.01671.x. [DOI] [PubMed] [Google Scholar]