Abstract
The aim of this study is to explore the occurrence and the risk factors of back-related loss of working time in patients undergoing surgery for lumbar disc herniation. One hundred and fifty-two gainfully employed patients underwent surgery for lumbar disc herniation. Two months postoperatively, those patients completed a self-report questionnaire including queries on back and leg pain (VAS), functional capacity (Oswestry disability index—ODI, version 1.0), and motivation to work. After 5 years, lost working time was evaluated by means of a postal questionnaire about sick leave and disability pensions. The cumulative number of back pain-related days-off work was calculated for each patient. All 152 patients, 86 men and 66 women, were prescribed sick leave for the first 2 months. Thereafter, 80 (53%) of them reported back pain-related sick leave or early retirement. A permanent work disability pension due to back problems was awarded to 15 (10%) patients, 5 men (6%) and 10 women (15%). Median number of all work disability days per year was 11 (interquartile range [IQR] 9–37); it was 9 days (IQR 9–22) in patients with minimal disability (ODI score 0–20) at 2 months postoperatively and 67 days (IQR 9–352) in those with moderate or severe disability (ODI > 20; P < 0.001). The respective means were 61, 29, and 140 days/year. Multivariate analysis showed ODI > 20, leg pain, and poor motivation to work to be the risk factors for extension of work disability. Results of the present study show that after the lumbar disc surgery, poor outcome in questionnaire measures the physical functioning (ODI) and leg pain at 2 months postoperatively, as well as poor motivation to work, are associated with the loss of working time. Patients with unfavourable prognosis should be directed to rehabilitation before the loss of employment.
Keywords: Lumbar disc herniation, Surgery, Oswestry disability index, Lost working time, Work disability
Introduction
Lumbar disc herniation is a common problem in the working population [24]. In most cases, patients are first given medication for pain and followed-up to see whether their sciatic symptoms disappear spontaneously, which in most cases occur within the first 3 months [3, 43, 48]. However, a considerable number (5–20%) of patients require surgery to relieve symptoms and to restore functional and work capacity [12, 24, 50].
The outcome of lumbar disc surgery is measured against two major factors: pain and functioning. Preoperative prediction of outcome is of paramount importance for selecting the right patients for surgery at the right time. After surgery, it is equally important to identify the patients whose recovery is poor to start rehabilitation before the development of adverse psychosocial consequences and loss of employment [16].
Studies about the prognosis after lumbar disc surgery show almost consistently that in addition to high level and long duration of pain and presence of motor and sensory deficits in preoperative physical examination, many psychosocial factors such as low education level, occurrence of psychological complaints, and longer duration of sick leave, are the risk factors for an unfavourable outcome in terms of pain and functional capacity [2, 4, 6, 23, 25, 26, 28, 31, 35, 39, 40, 45, 47, 50]. In some studies, the clinical outcome has also been associated with some preoperative image findings [45]. Return-to-work has been influenced by psychosocial factors, as well as work-related factors like physical loading of the work, ability to change working conditions, and work satisfaction, whereas clinical and image findings have a little impact [1, 5, 15, 44].
Most studies on productivity loss due to lost work related to lumbar disc herniation have only considered permanent exit from the labour market and reported that 60–85% of patients return to work within 1–3 years after lumbar disc surgery [15, 40, 49]. With longer follow-up times (7–10 years) 77–93% of patients have regained employment [22, 34]. However, shorter-term work disability, i.e., sick leave periods, may represent a substantial portion of the total impact of lumbar disc herniation on work performance. The cumulative number of work disability days is an accurate and a valid measure of lost productivity, i.e., indirect costs of a disease frequently outnumbering the direct costs of medical treatment [38, 41].
In the present study, we evaluate the occurrence and risk factors of lost work days over 5 years in a cohort of patients surgically treated on lumbar disc herniation.
Patients and methods
In Jyväskylä Central Hospital in 1999, 210 patients (∼1/1,000 inhabitants of the area) underwent surgery on lumbar disc herniation. Out of this, 173 patients volunteered for the present study. The remaining 37 patients were not included for the following reasons: 21 did not receive notification about the study when they were discharged from the hospital after operation, 8 were still suffering from severe back pain and had been referred to re-examination at the time of study, 4 failed to comply with the follow-up assessments, 2 had already undergone spondylodesis of the lumbar spine, 1 was pregnant, and 1 had Parkinson’s disease.
Indications for lumbar disc surgery were extensive or unbearable pain radiating down to the lower extremity and/or muscle weakness and, in majority of patients, a positive straight leg raising test gave a value of <60 [49, 51]. Patients may also have presented loss of patellar or Achilles reflex, cauda equina syndrome and/or regional sensory loss. The diagnosis of lumbar disc herniation was based on preoperative symptoms, clinical examination, and spinal nerve root compression detected during magnetic resonance imaging or computed tomography. Whenever possible, conservative treatment was applied first. Analgesics were given and 61 patients received physiotherapy; 30 of them received massage, 17 received TENS, 15 received cold treatment, and 10 received acupuncture. Local anesthetics were injected to seven patients. Patients were encouraged to do muscle stretching and strengthening.
The patients were operated on using the open mini approach described by Wood and Hanley in 1991 [50]. The presence of disc herniation was confirmed, the herniated fragment was extracted, and thereafter loose material from the intervertebral disc space was removed. Fusions were not performed.
Postoperatively, the patients were instructed to avoid sitting and driving a car for 4 weeks. Lifting, carrying, and forward bending of the back were restricted for 6 weeks. The patients were instructed to perform light stretching and mobility exercises during their 2 month sick leave period.
Collection of data
Before surgery, the patients completed a questionnaire including items about the duration of preoperative back and leg pain, intensity of pain (visual analogue scale—VAS, 0–100 mm) [13], employment status, and physical work load (physically light work or physically demanding work). Out of 173 patients, 21 were not employed at the time of operation and were excluded from the subsequent analysis. All the 152 employed patients were routinely prescribed sick leave for 2 months after the surgery.
On 2 months follow-up, intensity of the current back and leg pain (VAS 0–100 mm) was recorded. The degree of disability during the previous week was assessed by the original Oswestry low back pain disability questionnaire (scale 0–100) [18, 19]. The Short form of the Beck depression inventory (SDI) was used to evaluate the mood of the patient [30]. Motivation to the work was assessed by the modified questionnaire developed by Eva Esbjörnsson [17].
After the 2 months visit, patients were treated according to the routine principles. Sick leave was prescribed, if the patient was unable to perform his or her regular job or another similar job. If work incapacity persisted for 1 year at least, disability pension could be awarded according to the decision of medical examiners of the social insurance institutions.
After 5 years, a postal questionnaire was sent out, and the patients were asked to report any sick leave after the 2 months visit, as well as the causes of the sick leave. Further, the patients were asked to report retirements from work after the operation including the date and the reason of retirement (back problem, any other disease, or retirement due to age). For each patient, the cumulative number of all back-related days-off work were calculated and divided by the number of follow-up years during which the patient was available to the workforce, except for the back disease.
Statistical analysis
Descriptive values of variables are expressed as means with standard deviations (SDs) and with 95% confidence intervals (CIs), when the variables were not normally distributed as medians with interquartile ranges (IQRs). Accordingly, the median regression method served to analyze factors related to the cumulative number of work disability days. Statistical comparisons between groups were made by the t test for normally and by the Mann–Whitney test for not normally distributed groups. The rate of back-related permanent work disability pensions was analyzed by the Kaplan–Meier method and the factors associating with the pensions by the Cox regression method.
The Ethical Committee of Jyväskylä Central Hospital approved the study design.
Results
Demographic and clinical data on the 152 patients who underwent simple discectomy for lumbar disc herniation are shown in Table 1. Women (n = 66) had higher scores of preoperative pain, whereas men (n = 86) more often had a physically demanding job. In 145 cases, the disc herniation was in lateral (right in 60, left in 85) and in seven cases it was in medial. The level of operation was L5-S1 in 65 patients, L4-5 in 71, L3-4 in 6, L2-3 in 3, and L1-L2 in 3 patients. Four individuals were operated in two levels.
Table 1.
Demographics and clinical data of the 152 patients operated for lumbar disc herniation
| Variables | Male | Female | All |
|---|---|---|---|
| Number of patients | 86 | 66 | 152 |
| Age (years), mean (SD) | 38 (10) | 40 (10) | 39 (10) |
| Body mass index, mean (SD) | 26.1 (2.9) | 25.6 (3.7) | 25.8 (3.3) |
| Physically demanding job (%) | 35 (41) | 19 (29) | 54 (36) |
| Preoperative duration of back pain (months), median (IQR) | 9 (3, 24) | 10 (3, 24) | 10 (3, 24) |
| Preoperative duration of leg pain (months), median (IQR) | 6 (3, 12) | 9 (4, 15) | 6 (3, 15) |
| Back pain before operation, VAS, median (IQR) | 50 (32, 78) | 71 (44, 85) | 60 (36, 82) |
| Leg pain before operation, VAS, median (IQR) | 70 (47, 86) | 83 (70, 91) | 74 (57, 89) |
| Number of re-operated patients (%) | 2 (2) | 4 (6) | 6 (4) |
After 2 months of surgery, the median Oswestry disability index (ODI) was 14 (IQR 6–26) while mean was 17. No gender difference was found. Compared to the preoperative situation (Table 1), the pain scores (VAS) were markedly reduced: median back pain was 13 (IQR 3–29) and median leg pain was 10 (IQR 3–23).
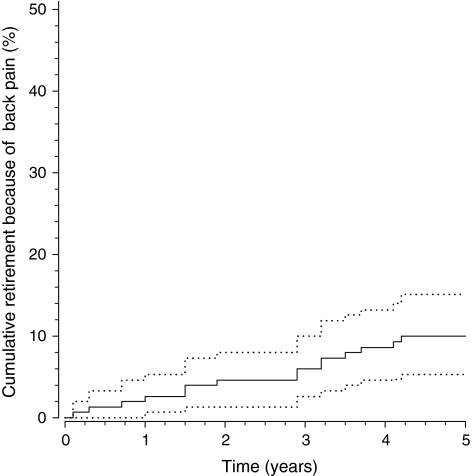
All the 152 patients were prescribed sick leave for the first 2 months, which was customary at that time in Finland. Thereafter, 80 (53%) of them reported back-related sick leave or a work disability pension. A permanent work disability pension due to back was awarded to 15 (10%) patients (Fig. 1); 5 of them were men (6% of men), and 10 were women (15% of women). When days on sick leave were included, the median number of all work disability days per year was 11 (IQR 9–37); the mean was 61 days. Women had more days-off work than men: the respective medians were 17 days (IQR 9–72) and 9 days (IQR 9–27) per year (P = 0.038), and the means were 77 and 49 days. The distribution of the individuals’ work disability days was very skewed.
Fig. 1.
The rate of permanent disability pensions related to back problems (95% confidence interval) of 152 patients operated for lumbar disc herniation
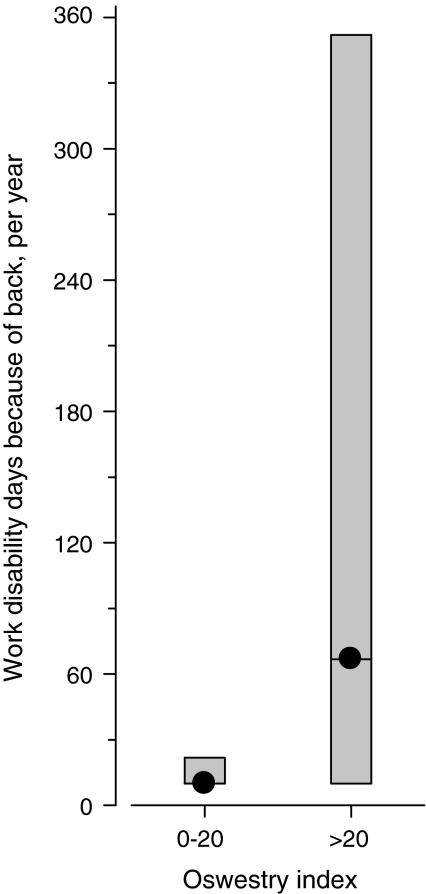
After 2 months of surgery, 108 (71%) of the patients had only minimal disability (ODI 0–20) while 44 (29%) had moderate or severe disability (ODI > 20). In the former group, the median number of work disability days per year was 9 (IQR 9–22), whereas in the latter it was 67 (IQR 9–352) (P < 0.001; Fig. 2). Multivariate analysis revealed that a higher ODI, more intensive leg pain, and poor motivation to work at 2 months postoperatively were risk factors for extension of work disability, whereas gender was not an independent predictor (Table 2).
Fig. 2.
The number of work disability days per patient-year by Oswestry disability index at 2 months postoperatively; median with interquartile range
Table 2.
Prediction of the risk factors for work disability days after lumbar disc herniation surgery
| Coefficient | 95% confidence interval | p-value | |
|---|---|---|---|
| Patient characteristics | |||
| Age | 0.047 | –3.17 to 4.11 | 0.80 |
| Body mass index | 0.31 | –0.72 to 1.34 | 0.55 |
| Male sex | –2.71 | −9.14 to 3.72 | 0.41 |
| Physically demanding work | 3.33 | –3.24 to 9.90 | 0.32 |
| Preoperative variables | |||
| Duration of preoperative back pain | 0.011 | –0.09 to 0.11 | 0.81 |
| Duration of preoperative leg pain | −0.11 | −0.23 to 0.09 | 0.071 |
| Variables 2 months postoperatively | |||
| Back pain, VAS | −0.15 | −0.37 to 0.07 | 0.17 |
| Leg pain, VAS | 0.58 | 0.38 to 0.79 | <0.001 |
| Oswestry index > 20 | 32.01 | 23.7 to 40.4 | <0.001 |
| Short depression inventory | −0.12 | −1.27 to 1.04 | 0.84 |
| Motivation to work | −2.88 | −3.97 to −1.79 | <0.001 |
| Constant | 37.2 | – | – |
Poor functional capacity (ODI > 20) was also a risk factor for a permanent back-related disability pension (hazard ratio [HR] 15.2; 95% CI 2.1–112), in addition to older age (HR 1.25; 95% CI 1.04–1.50) (Table 3).
Table 3.
The factors associated with permanent disability pension after lumbar disc herniation surgery
| Hazard ratio | 95% confidence interval | p-value | |
|---|---|---|---|
| Patient characteristics | |||
| Age (years) | 1.25 | 1.04 to 1.50 | 0.019 |
| Body mass index | 1.06 | 0.75 to 1.49 | 0.75 |
| Male sex | 0.78 | 0.04 to 16.3 | 0.87 |
| Physically demanding work | 1.03 | 0.07 to 15.0 | 0.98 |
| Preoperative variables | |||
| Duration of back pain (months) | 1.00 | 0.97 to 1.03 | 0.95 |
| Duration of leg pain (months) | 1.00 | 0.98 to 1.03 | 0.72 |
| Variables 2 months postoperatively | |||
| Back pain, VAS 0–100 | 1.01 | 0.98 to 1.04 | 0.41 |
| Leg pain, VAS 0–100 | 1.02 | 0.96 to 1.08 | 0.46 |
| Oswestry index > 20 | 15.2 | 2.07 to 112 | 0.007 |
| Short depression inventory | 1.09 | 0.76 to1.57 | 0.63 |
| Motivation for work | 0.93 | 0.63 to 1.37 | 0.71 |
Discussion
In this study, we showed that a higher functional disability (ODI), more intensive leg pain, and poor motivation to work at 2 months after lumbar disc operation are risk factors for future loss of working time. Functional disability also was a predictor of permanent work disability. The cut-off-point of 20 in ODI score divided the patients into two groups differing considerably on their future work capacity. High scores in the ODI and in leg pain assessment by VAS can be regarded as alarm signals for a poor socioeconomic outcome, i.e., more lost working days and higher costs to the society.
The ODI has earlier appeared to be a predictor of permanent or prolonged disability after lumbar disc surgery [15, 19, 28]. The present study is the first to show that the ODI is a risk factor for loss of working time, i.e., indirect societal cost, as well.
In general, self-reported questionnaire measures of functioning like the ODI have been shown reliably to predict future functioning and disability in many specialist areas of medicine and they have frequently been used as better predictors than bio-physiological measures such as laboratory tests and radiography [29, 37]. The questionnaire measures of functioning are multifaceted instruments which reflect not only physical function but also psychosocial status. These measures, however, do not take into account the requirements of a patient’s job. These factors are included in the patient’s prediction of his or her own ability to work, which has also appeared as a significant predictor of working ability after lumbar disk surgery [15].
Leg pain but not back pain at 2 months postoperatively was also a risk factor for days-off work. The postoperative leg pain may result from prolonged preoperative compression of the nerve root leading to nerve injury and constant pain or from failed back surgery. Further, the experience of pain may be associated with psychological characteristics negatively affecting the work capacity.
In many studies, duration of pain adversely has an impact on the prognosis of work capacity [32, 39, 40]. Workers who report an episode of low-back pain mostly return to work within 1 month, while a small number, fewer than 5%, never return. By the time a worker has been out of work for 6 months, the likelihood of returning to work is just 50%, and when the worker has been out of work for 1 year, the likelihood returning to work drops to 25% [21]. In addition to the functional disability itself, the adverse psychosocial consequences of prolonged sick leave play a role in this phenomenon. Contrary to these findings, duration of preoperative pain did not achieve statistical significance as an explanatory variable in the multivariate model of loss of working time in the present study. This may be due to association between prolonged preoperative pain and high postoperative ODI. Unfortunately, we have no data on preoperative ODI or duration of preoperative sick leave.
Motivation is a crucial factor for functioning of any kind and not surprisingly, it was inversely related to the number of work disability days. The concept of motivation, however, is somewhat controversial and no widely accepted measure for motivation exists [33]. Further, motivation may include factors like work satisfaction, occurrence of psychological complaints, etc., which have been associated with work disability in other studies which have not assessed motivation. Despite earlier results, depression did not appear as an independent risk factor for future work incapacity in our multivariate model [15, 45]. This may be due to the fact that depressed patients generally report more pain and disability [42].
Physically heavy work was not a risk factor in this study, but the self-reported work load—dichotomized as physically light or physically demanding—may not be an accurate and a valid measure of the actual work load. The physical and psychological requirements of a patient’s job should be clarified more thoroughly. For assessment of physical work load, some validated patient questionnaires have been developed [7, 46]. Combination of this information with data on the patient’s functional capacity, e.g., the individual items of the ODI, could further facilitate the identification of patients at risk of losing work capacity and assist in planning appropriate rehabilitation [16, 21]. None of the work load questionnaires, however, have gained popularity so far.
Older age was a risk factor for back-related retirement. Performance capacity decreases with age, and long life entails debilitating disorders and diseases [9]. Older patients are less often suited to vocational rehabilitation because they are, on average, less well educated and less motivated for a change of employment than younger individuals. In addition, employers may be reluctant to employ them. Consequently, older people are more likely to end up on a disability pension. In the present study, 10% of the patients had a permanent work disability pension due to back after 5 years of surgery. Similar but also much differing rates of work disability have been reported earlier [15, 22, 34, 40, 49].
We have no data on the rehabilitation received by our patients, but several randomized studies have shown that specific exercise therapy of back muscles significantly reduces pain and disability after disc surgery [10, 11, 14, 20, 51]. Carragee et al. [8] have shown that early return to vigorous activities is possible in the majority of patients (98%) and early return-to-work with the mean sick leave of 1.7 weeks did not increase the rate of complications. The 2 months sick leave which was routinely prescribed during this study may be inappropriately long in many cases. Longer sick leave has adverse psychosocial impact increasing the odds of permanent loss of employment [6, 25] but the rate of work disability here was less than the reported in many studies [15, 22, 34, 40, 49]. A 2 months sick leave, however, may cause needless loss of work productivity. Nowadays, the duration of sick leave prescribed in our hospital after lumbar disc surgery varies from 4 to 6 weeks according to the patient’s work demand.
Among the societal costs of many musculoskeletal conditions, the indirect costs, i.e., costs due to the loss of work productivity, play a dominant role [27]. The mean monetary value of one lost working day was evaluated as €82 in Finland in 2002 [41]. In the present study, this translates into a mean annual loss of productivity of €2,400 in the group with an ODI score of ≤20 and of €11,500 in the group with an ODI score of >20. Consequently, interventions to prevent loss of working time may have marked economic value. In this study, the number of days-off work was based on self-report, which carries a risk of recall bias. This, however, is not likely to be different between the two groups formed according to the ODI.
At the time of commencement of the present study, preoperative questionnaire data like the ODI, SDI, and motivation were not routinely collected in the Department of Orthopedics of Jyväskylä Central Hospital. This may be regarded as a limitation of our study. However, our purpose was to investigate the normal care of lumbar disc herniation and in that setting, the ODI at 2 months postoperatively, proved to be a valid, feasible, and marked predictor of future work capacity and societal costs.
Our patients represent nearly all the patients with lumbar disc herniation in the Central Finland region, where the private sector in operative health care is almost non-existent. The population of Finland is very homogenous and thus the results can be generalized to the whole country. The Finnish social insurance system and labour market may have some impact on the results. In general, rates of work disability have been higher in European countries than in the USA, where welfare facilities are more limited but the labour market is more flexible than in Europe.
In summary, self-reported measures of functional capacity, pain, and motivation to work may help in the early postoperative phase after lumbar disc surgery to identify those patients who are at risk of an unfavourable outcome and may need special therapeutic and rehabilitative interventions. Vocational counselling on the basis of data on patient’s functional capacity and requirements of his or her job is highly important [16]. Early rather than later commencement of rehabilitation has shown to yield better results [36]. Activities targeted to improve work capacity and prevent days-off work may lead to substantial savings to the society.
Acknowledgments
This study was supported by the Medical Research Foundation of Jyväskylä Central Hospital.
References
- 1.Atlas SJ, Chang Y, Kammann E, Keller RB, Deyo RA, Singer DE. Long-term disability and return to work among patients who have a herniated lumbar disc: the effect of disability compensation. J Bone Joint Surg Am. 2000;82:4–15. doi: 10.2106/00004623-200001000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Atlas SJ, Keller RB, Chang Y, Deyo RA, Singer DE. Surgical and nonsurgical management of sciatica secondary to a lumbar disk herniation: five-year outcomes from the Maine lumbar spine study. Spine. 2001;26:1179–1187. doi: 10.1097/00007632-200105150-00017. [DOI] [PubMed] [Google Scholar]
- 3.Balague F, Nordin M, Sheikhzadeh A, Echegoyen AC, Brisby H, Hoogewoud HM, Fredman P, Skovron ML. Recovery of severe sciatica. Spine. 1999;24:2516–2524. doi: 10.1097/00007632-199912010-00014. [DOI] [PubMed] [Google Scholar]
- 4.Barrios C, Ahmed M, Arrotequi JI, Bjornsson A. Clinical factors predicting outcome after surgery for herniated lumbar disc: an epidemiological multivariate analysis. J Spinal Disord. 1990;3:205–209. doi: 10.1097/00002517-199009000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Boer J, Oostendorp R, Beems T, Munneke M, Evers A. Reduced work capacity after lumbar disc surgery: the role of cognitive-behavioral and work-related risk factors. Pain. 2006;126:72–78. doi: 10.1016/j.pain.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 6.Boer J, Oostendorp R, Beems T, Munneke M, Oerlemans M, Evers A. A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J. 2006;15:527–536. doi: 10.1007/s00586-005-0910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bot SD, Terwee CB, Wiundt DA, Feleus A, Bierma-Zeinstra SM, Knol DL, et al. Internal consistency and validity of a new physical workload questionnaire. Occup Environ Med. 2004;61:980–986. doi: 10.1136/oem.2003.011213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carragee EJ, Han MY, Yang B, Kim DH, Kraemer H, Billys J. Activity restrictions after lumbar discectomy. A prospective study of outcomes in 152 cases with no postoperative restrictions. Spine. 1999;24:2346–2351. doi: 10.1097/00007632-199911150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Chan G, Tan V, Koh D. Ageing and fitness to work. Occup Med (Lond) 2000;50:483–491. doi: 10.1093/occmed/50.7.483. [DOI] [PubMed] [Google Scholar]
- 10.Choi G, Raiturker PP, Kim MJ, Jin CD, Chae YS. The effect of early isolated lumbar extension exercise program for patients with herniated disc undergoing lumbar discectomy. Neurosurgery. 2005;57:764–772. doi: 10.1227/01.NEU.0000175858.80925.38. [DOI] [PubMed] [Google Scholar]
- 11.Danielsen JM, Johnsen R, Kibsgaard SK, Hellevik E. Early aggressive exercise for postoperative rehabilitation after discectomy. Spine. 2000;25:1015–1020. doi: 10.1097/00007632-200004150-00017. [DOI] [PubMed] [Google Scholar]
- 12.Deyo RA, Loeser JD, Bigos SJ. Herniated lumbar intervertebral disk. Ann Intern Med. 1990;112:598–603. doi: 10.7326/0003-4819-112-8-598. [DOI] [PubMed] [Google Scholar]
- 13.Dixon S, Bird H. Reproducibility along a 10 cm visual analogue scale. Ann Rheum Dis. 1981;40:87–89. doi: 10.1136/ard.40.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dolan P, Greenfield K, Nelson RJ, Nelson IW. Can exercise therapy improve the outcome of microdiscectomy? Spine. 2000;25:1523–1532. doi: 10.1097/00007632-200006150-00011. [DOI] [PubMed] [Google Scholar]
- 15.Donceel P, Du Bois M. Predictors for work incapacity continuing after disc surgery. Scand J Work Environ Health. 1999;25:264–271. doi: 10.5271/sjweh.433. [DOI] [PubMed] [Google Scholar]
- 16.Donceel P, Du Bois M, Lahaye D. Return to work after surgery for lumbar disc herniation. A rehabilitation-oriented approach in insurance medicine. Spine. 1999;24:872–876. doi: 10.1097/00007632-199905010-00007. [DOI] [PubMed] [Google Scholar]
- 17.Esbjörnsson E. Personlinghet och smärta. Psykologiska factorers betydelse för arbetsåtergång hos patienter med kroniska långryggsbesvär. Academic dissertation. Göteborg: Göteborg Universitet; 1984. [Google Scholar]
- 18.Fairbank JCT, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 19.Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 20.Filiz M, Cakmak A, Ozcan E. The effectiveness of exercise programmes after lumbar disc surgery: a randomized controlled study. Clin Rehabil. 2005;19:4–11. doi: 10.1191/0269215505cr836oa. [DOI] [PubMed] [Google Scholar]
- 21.Frank JW, Brooker AS, DeMaio SE, Kerr MS, Maetzel A, Shannon HS, Sullivan TJ, Norman RW, Wells RP. Disability resulting from occupational low back pain. Part II: what do we know about secondary prevention? A review of the scientific evidence on prevention after disability begins. Spine. 1996;21:2918–2929. doi: 10.1097/00007632-199612150-00025. [DOI] [PubMed] [Google Scholar]
- 22.Graver V, Haaland AK, Magnaes B, Loeb M. Seven-year clinical follow-up after lumbar disc surgery: results and predictors of outcome. Br J Neurosurg. 1999;13:178–184. doi: 10.1080/02688699943952. [DOI] [PubMed] [Google Scholar]
- 23.Hasenbring M, Marienfeld G, Kuhlendahl D, Soyka D. Risk factors of chronicity in lumbar disc patients. A prospective investigation of biologic, psychologic, and social predictors of therapy outcome. Spine. 1994;19:2759–2765. doi: 10.1097/00007632-199412150-00004. [DOI] [PubMed] [Google Scholar]
- 24.Heliövaara M, Sievers K, Impivaara O, Maatela J, Knekt P, Mäkelä M, Aromaa A. Descriptive epidemiology and public health aspects of low back pain. Ann Med. 1989;21:327–333. doi: 10.3109/07853898909149216. [DOI] [PubMed] [Google Scholar]
- 25.Hurme M, Alaranta H. Factors predicting the results of surgery for lumbar intervertebral disc herniation. Spine. 1987;12:933–938. doi: 10.1097/00007632-198711000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Häkkinen A, Ylinen J, Kautiainen H, Airaksinen O, Herno A, Kiviranta I. Does the outcome 2 months after lumbar disc surgery predict the outcome 12 months later? Disabil Rehabil. 2003;25:968–972. doi: 10.1080/0963828031000122258. [DOI] [PubMed] [Google Scholar]
- 27.Jonsson D, Husberg M. Socioeconomic costs of rheumatic diseases. Int J Technol Assess Health Care. 2000;16:1193–1200. doi: 10.1017/S0266462300103228. [DOI] [PubMed] [Google Scholar]
- 28.Junge A, Frohlich M, Ahrens S, Hasenbring M, Sandler A, Grob D, Dvorak J. Predictors of bad and good outcome of lumbar spine surgery. A prospective clinical study with 2 years follow up. Spine. 1996;21:1056–1064. doi: 10.1097/00007632-199605010-00013. [DOI] [PubMed] [Google Scholar]
- 29.Katz JN, Punnett L, Simmons BP, Fossel AH, Mooney N, Keller RB. Workers’ compensation recipients with carpal tunnel syndrome: the validity of self-reported health measures. Am J Public Health. 1996;86:52–56. doi: 10.2105/ajph.86.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keltikangas-Järvinen L, Rimon R. Rimon’s brief depression scale, a rapid method for screening depression. Psychol Rep. 1987;60:111–119. doi: 10.2466/pr0.1987.60.1.111. [DOI] [PubMed] [Google Scholar]
- 31.Kohlboeck G, Greimel KV, Piotrowski WP, Leibetseder M, Krombholz-Reindl M, Neuhofer R, et al. Prognosis of multifactorial outcome in lumbar discectomy: a prospective longitudinal study investigating patients with disc prolapse. Clin J Pain. 2004;20:455–461. doi: 10.1097/00002508-200411000-00011. [DOI] [PubMed] [Google Scholar]
- 32.Kotilainen E, Valtonen S, Carlson CA. Microsurgical treatment of lumbar disk herniation: follow-up of 237 patients. Acta Neurochir (Wien) 1993;120:143–149. doi: 10.1007/BF02112033. [DOI] [PubMed] [Google Scholar]
- 33.Latham GP, Pinder CC. Work motivation theory and research at the dawn of the twenty-first century. Annu Rev Psychol. 2005;56:485–516. doi: 10.1146/annurev.psych.55.090902.142105. [DOI] [PubMed] [Google Scholar]
- 34.Lewis PJ, Weir BK, Broad RW, Grace MG. Long-term prospective study of lumbosacral discectomy. J Neurosurg. 1987;67:49–53. doi: 10.3171/jns.1987.67.1.0049. [DOI] [PubMed] [Google Scholar]
- 35.Loupasis GA, Stamos K, Katonis PG, Sapkas G, Korres DS, Hartofilakidis G. Seven to twenty years outcome of lumbar discectomy. Spine. 1999;24:2313–2317. doi: 10.1097/00007632-199911150-00005. [DOI] [PubMed] [Google Scholar]
- 36.Marnetoft SU, Selander J. Long-term effects of early versus delayed vocational rehabilitation: a four-year follow-up. Disabil Rehabil. 2002;24:741–745. doi: 10.1080/09638280210124338. [DOI] [PubMed] [Google Scholar]
- 37.Mayou R, Bryant B. Quality of life after coronary artery surgery. Q J Med. 1987;62:239–248. [PubMed] [Google Scholar]
- 38.Merkesdal S, Mau W. Prediction of cost-of-illness in patients with low back pain undergoing orthopedic outpatient rehabilitation. Int J Rehabil Res. 2005;28:119–126. doi: 10.1097/00004356-200506000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Nygaard OP, Romner B, Trumpy JH. Duration of symptoms as a predictor of outcome after lumbar disc surgery. Acta Neurochir (Wien) 1994;128:53–56. doi: 10.1007/BF01400653. [DOI] [PubMed] [Google Scholar]
- 40.Nygaard OP, Kloster R, Solberg T. Duration of leg pain as a predictor of outcome after surgery for lumbar disc herniation: a prospective cohort study with 1 year follow-up. J Neurosurg. 2000;92(Suppl 2):131–134. doi: 10.3171/spi.2000.92.2.0131. [DOI] [PubMed] [Google Scholar]
- 41.Puolakka K, Kautiainen H, Pekurinen M, Möttönen T, Hannonen P, Korpela M, et al. Monetary value of lost productivity over a 5 year follow up in early rheumatoid arthritis estimated on the basis of official register data on patients’ sickness absence and gross income: experience from the FIN-RACo Trial. Ann Rheum Dis. 2006;65:699–703. doi: 10.1136/ard.2005.040055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rush AJ, Polatin P, Gatchel RJ. Depression and chronic low back pain: establishing priorities in treatment. Spine. 2000;25:2566–2571. doi: 10.1097/00007632-200010150-00004. [DOI] [PubMed] [Google Scholar]
- 43.Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine. 1990;15:683–686. doi: 10.1097/00007632-199007000-00013. [DOI] [PubMed] [Google Scholar]
- 44.Schade V, Semmer N, Main CJ, Hora J, Boos N. The impact of clinical, morphological, psychosocial and work-related factors on the outcome of lumbar discectomy. Pain. 1999;80:239–249. doi: 10.1016/S0304-3959(98)00210-3. [DOI] [PubMed] [Google Scholar]
- 45.Trief PM, Grant W, Fredrickson B. A prospective study of psychological predictors of lumbar surgery outcome. Spine. 2000;25:2616–2621. doi: 10.1097/00007632-200010150-00012. [DOI] [PubMed] [Google Scholar]
- 46.Viikari-Juntura E, Rauas S, Kuosma E, Riihimäki H, Takala E-S, Saarenmaa K. Validity of self-reported physical work load in epidemiologic studies on musculoskeletal disorders. Scand J Work Environ Health. 1996;22:251–259. doi: 10.5271/sjweh.139. [DOI] [PubMed] [Google Scholar]
- 47.Vucetic N, Astrand P, Güntner P, Svensson O. Diagnosis and prognosis in lumbar disc herniation. Clin Ortop Rel Res. 1999;361:116–122. doi: 10.1097/00003086-199904000-00016. [DOI] [PubMed] [Google Scholar]
- 48.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983;8:131–140. doi: 10.1097/00007632-198303000-00003. [DOI] [PubMed] [Google Scholar]
- 49.Woertgen C, Rothoerl RD, Holzschuh M, Breme K, Brawanski A. Are prognostic factors still what they are expected to be after long-term follow-up? J Spinal Disord. 1998;11:395–399. doi: 10.1097/00002517-199810000-00005. [DOI] [PubMed] [Google Scholar]
- 50.Wood EG, Hanley EN. Lumbar disc herniation and open limited discectomy: indications, techniques, and results. Oper Tech Ortop. 1991;1:23–28. doi: 10.1016/S1048-6666(05)80003-5. [DOI] [Google Scholar]
- 51.Yilmaz Efficacy of dynamic lumbar stabilization exercise in lumbar microdiscectomy. J Rehabil Med. 2003;35:163–167. doi: 10.1080/16501970306125. [DOI] [PubMed] [Google Scholar]