Abstract
A descriptive clinical study in healthy adolescents was done to evaluate the clinical shoulder balance and analyze the correlation between clinical and radiological parameters which are currently used to evaluate shoulder balance. In addition to trunk shift and rib hump, shoulder balance is one of the criteria that are used to evaluate the outcomes in spinal deformity surgery. Several methods have been proposed to evaluate the shoulder balance in scoliotic patients; however, there is no uniformity to these methods in the current literature. Patients who applied to pediatric clinic without musculoskeletal pathology formed the patient population. Volunteers were asked to fill out a questionnaire assessing shoulder balance perception and had their clinical photograph taken simultaneously with a P–A chest X-ray. The clinical shoulder balance was evaluated through analysis of the clinical photograph. The X-rays were used to evaluate the radiological shoulder balance. The evaluated parameters included coracoid height difference (CHD), clavicular angle (CA), the clavicle–rib cage intersection difference (CRID), clavicular tilt angle difference (CTAD), and T1-tilt. The study group was composed of 48 male and 43 female patients with an average age of 13.6 ± 2.1 (10–18) years. In the questionnaire, all patients stated that their shoulders were level. The digital photographs revealed that only 17(18.7%) adolescents had absolutely level shoulders. The average height difference between shoulders was 7.5 ± 5.8 mm. The average CHD was 6.9 ± 5.8 mm, average CA was 2.2 ± 1.7°, average CRID was 4.8 ± 3.6 mm, average CTAD was 4 ± 3.2°, and average T1-tilt was 1.3 ± 1.4°. CHD, CA, and CRID demonstrated high correlation with clinical pictures, whereas CTAD demonstrated moderate and T1-tilt demonstrated only mild correlation. The radiological parameters used to evaluate the shoulder balance correlate with the clinical appearance. Contrary to popular belief, shoulder balance in healthy adolescents often does not exist.
Keywords: Shoulder balance, Adolescent, Normal population, Deformity, Radiological parameters
Introduction
Established traditions in orthopedic practice require continuous questioning instead of general acceptance. As in daily life, there are several myths in orthopedic practice that have received general acceptance and not been questioned for years. For instance, the asymmetric abdominal skin reflex was considered a sign of occult intraspinal pathology in scoliosis patients for decades until Yngve [6] demonstrated that it is observed in 27% of the normal population. Similarly, it was accepted that the cranium was centralized over the pelvis in the normal population. For decades, treatment plans for spinal deformity patients were planned to achieve this goal. However, Ashton-Miller et al. [1] demonstrated that in otherwise healthy adolescents the C7 spinous process was located within 20 mm of the central sacral vertical line. This led to dramatic changes in the goals of scoliosis surgery in terms of the coronal balance expectations of both surgeons and patients.
A similar myth exists for shoulder balance. The normal healthy population is considered to have level shoulders. Although any disturbance in the equality of the spatial position of both shoulders is regarded as pathological, no studies dealing with shoulder balance in healthy adolescents without deformity of the spine or extremities exist. The aim of this study was to evaluate the concordance between radiological and clinical parameters used to measure shoulder balance.
Materials and methods
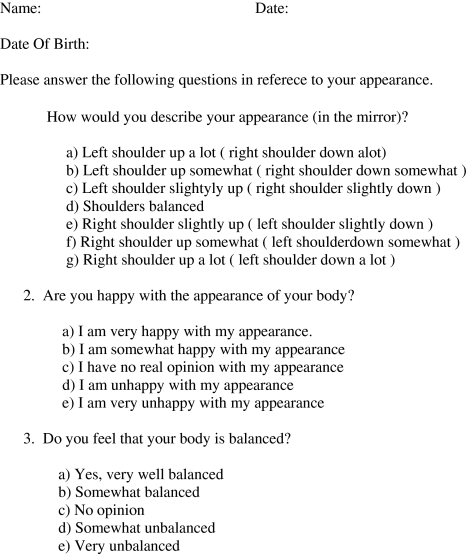
The study group comprised volunteers who attended the pediatrics clinic and required a chest X-ray examination. The study was approved by the hospital ethics committee and informed consent was obtained from the volunteers and their legal guardians. The subjects were examined to rule out any spinal deformity, pelvic obliquity, upper extreme deformity, and lower limb length inequality. They were asked to fill out a questionnaire assessing shoulder balance perception (Fig. 1). It was a part of the questionnaire prepared by Kuklo et al. [4] in order to evaluate shoulder balance perception in the scoliotic population who had surgical intervention.
Fig. 1.
The questionnaire
Digital photographs of the subjects were taken to evaluate clinical shoulder balance. The digital photographs and the X-ray images were taken simultaneously. The digital camera was placed on the X-ray tube in order to standardize the clinical pictures. The subjects were asked to stand up straight with their arms by their sides. The X-ray technicians were instructed to focus the beam at T1 level, with the tube 150 cm away from the subject, and to include both shoulders in the Roentgenogram. Physicians at the adolescent clinic were informed about the position of the arms during the X-ray examination to prevent misinterpretation of these X-rays.
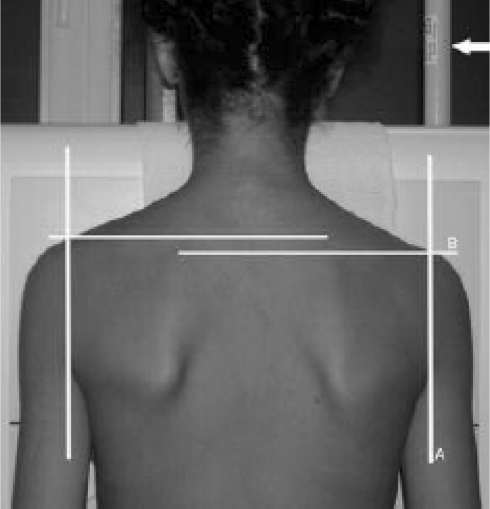
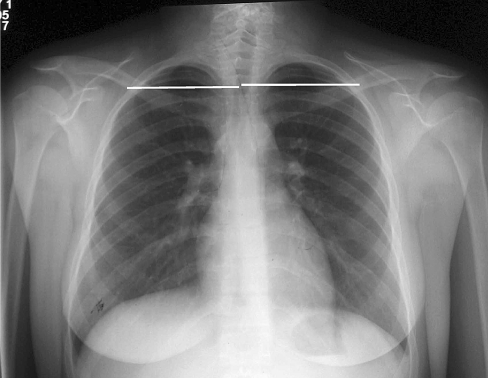
The digital clinical pictures were measured with a special drawing program (CorelDRAW®-Version 11.0-© 2002 Corel Corporation). Vertical lines were drawn through the volunteers’ posterior axillary folds. The points where these lines intersected with the shoulders were regarded as the reference points. The height difference between these points in millimeters was measured to reflect the clinical shoulder balance (Fig. 2). The values were calibrated with the size of a part of the X-ray machine. Negative values represented right shoulder elevation, with positive values for left shoulder elevation.
Fig. 2.
Clinical picture used to evaluate clinical shoulder balance. aVertical lines were drawn through the posterior axillary folds. b The height difference between the horizontal lines where vertical lines intersected with the shoulders was measured to reflect the clinical shoulder balance (arrow the tube whose size was used to calibrate the clinical shoulder balance measurements)
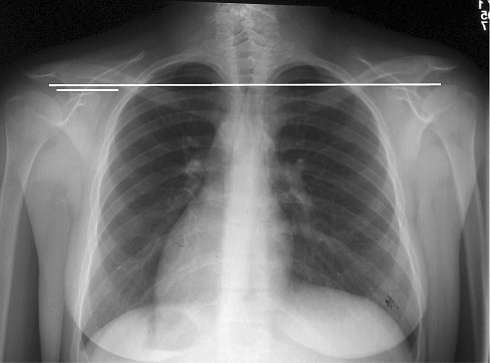
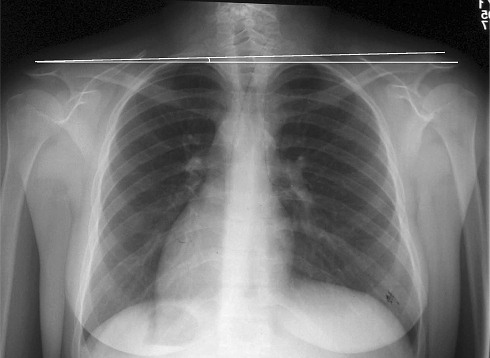
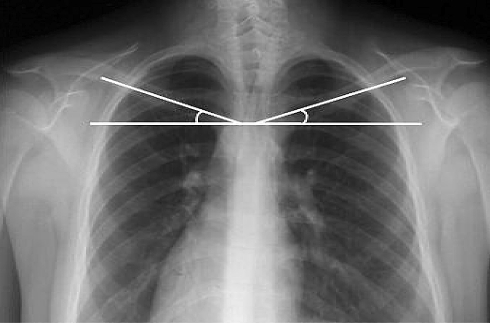
The parameters that were measured on the X-rays included coracoid height difference (CHD), clavicular angle (CA), T1-tilt, clavicle–rib cage intersection difference (CRID) (previously described by Bago et al. [2]), and a new parameter that was recently described, clavicular tilt angle difference (CTAD). CHD measures the height difference between the coracoid processes by tracing a horizontal line at the upper margin of each and measuring the difference, which is expressed in millimeters (Fig. 3). CA represents the angle between the line connecting the highest points of the clavicles and the horizontal plane (Fig. 4). CRID represents the height difference between the horizontal lines passing through the point where the superior border of the clavicle intersects with the outer edge of the second rib on each side (Fig. 5). Clavicular tilt angle is the angle between the line bisecting the proximal portion of the clavicle and the horizontal. The difference between these angles represents CTAD (Fig. 6). T1-tilt is the angle between the upper end-plate of the T1 vertebra and the horizontal line. The measurements that are expressed in millimeters (mm) were calibrated according to the scale on the digital X-rays. Negative values represented right shoulder elevation whereas positive values for left shoulder elevation.
Fig. 3.
Coracoid height difference (CHD) measures the height difference between the horizontal lines (A, B) that pass through the upper margin of each coracoid process
Fig. 4.
The clavicular angle (CA) represents the angle between the line connecting a the highest points of the clavicles and b the horizontal plane
Fig. 5.
Clavicle–rib intersection difference (CRID) represents the height difference between the horizontal lines (A, B) passing through the point where the superior border of the clavicle intersects with the outer edge of the second rib on each side
Fig. 6.
Clavicular tilt angle (CTAD) is the angle between the line bisecting the proximal portion of a the clavicle and b the horizontal. The difference between these angles represents clavicular tilt angle difference
Statistical analysis
Data were summarised as mean ± standard deviation (SD). In order to calculate the means and standard deviations of imbalance, absolute values were used. Correlations of the radiological parameters with clinical pictures were calculated using Spearman’s correlation coefficient and the actual values were used, with positive and negative signs indicating different directions clinical shoulder height difference that was measured from clinical digital picture, was used as a gold standard test to determine shoulder balance. Ten millimeter clinical shoulder height difference was used as a cut-off point [4] and patients who has 10 mm difference between their shoulder heights are grouped as “imbalanced” and patients who has <10 mm difference between shoulder heights were grouped as “balanced”. Receiver operating characteristic (ROC) curves were used to describe the performance of the diagnostic value of radiological findings according to this 10 mm cut-off value. Area under curve defines the similarity of both measurement methods. Youden’s index was used to indicate the ideally sensitive and specific cut-off points for each radiological method. Summation of sensitivity and specificity, then subtraction of one from this equation yields Youden’s index. Intraclass correlation coefficient (ICC) was used to evaluate interobserver and intraobserver reliability of the radiographic measurement techniques. All analyses were performed with a special software (SPSS 11.5, Chicago, IL, USA). For all analyses, p < 0.05 was considered statistically significant.
Results
The study involved 105 volunteers. Six subjects with unsuitable photographs and eight subjects who had clinically missed scoliosis diagnosed with chest X-rays were excluded. Ninety-one adolescents (48 male, 43 female), with an average age of 13.6 ± 2.1(10–18) years fulfilled the inclusion criteria.
In the questionnaire, all subjects stated that their shoulders were level in response to question-one. Sixty-six (72%) were happy with their appearance, 13 (15%) were somewhat happy with their appearance, 11 (12%) expressed no idea about their appearance, and 1 (1%) was unhappy with her appearance who, upon further questioning, expressed her unhappiness about being overweight. Seventy-nine (87%) stated that their bodies were balanced and 6 (7%) a little balanced, while 5 (5%) expressed no idea about their balance and 1 (1%) stated that his body was unbalanced (he was also unhappy with the appearance of his body).
Digital photographs revealed that only 17 (18.7%) adolescents had level shoulders. The average height difference between shoulders was 7.5 ± 5.8 mm (0–27) (Table 1). Kuklo et al. [4] defined normal shoulder balance for the scoliotic population as <10 mm side-to-side shoulder height difference. When we used this value, 70 (72%) subjects were within the normal limits.
Table 1.
Results of clinical and radiological evaluation of shoulder balance
| Methods | Mean ± SD | Range |
|---|---|---|
| Clinical picture (mm) | 7.5 ± 5.8 | 0–27 |
| CHD (mm) | 6.9 ± 5.8 | 0–28 |
| CRID (mm) | 4.8 ± 3.6 | 0–16 |
| CA (°) | 2.2 ± 1.7 | 0–11 |
| CTAD (°) | 4.0 ± 3.2 | 0–20 |
| T1-tilt (°) | 1.3 ± 1.4 | 0–6 |
CHD coracoid height difference, CRID clavicle–rib intersection difference, CA clavicular angle, CTAD clavicular tilt angle difference, SD standard deviation, and mm millimeters
The radiological examination revealed the shoulders to be level in 10 (11%) subjects with respect to CHD, 14 (15.4%) subjects with respect to CA, 14 (15.4%) subjects with respect to CRID, and 9 (9.9%) subjects with respect to CTAD while T1-tilt was zero in 29 (31.9%) subjects. To calculate the mean and standard deviation of the measurements, we used the absolute values, because our aim was to investigate any deviation from normal regardless of its direction. The average CHD was 6.9 ± 5.8 mm (0–28), average CA was 2.2 ± 1.7° (0–11), average CRID was 4.8 ± 3.6 mm (0–16), average CTAD was 4.0 ± 3.2° (0–20), and average T1-tilt was 1.3 ± 1.4° (0–6) (Table 1).
Correlation analysis was performed with Spearman’s test. Results demonstrated that all radiological parameters correlated with clinical pictures (p < 0.01). CHD, CA, and CRID demonstrated strong correlation (r = 0.76, p < 0.01; r = 0.74, p < 0.01; and r = 0.73, p < 0.01; respectively), whereas CTAD demonstrated a moderate correlation (r = 0.60, p < 0.01). T1-tilt demonstrated only a mild correlation (r = 0.28, p < 0.01) (Table 2).
Table 2.
Correlation of the radiological parameters with the clinical pictures
| Radiological methods | Ra | P |
|---|---|---|
| CHD (mm) | 0.76 | <0.01 |
| CRID (mm) | 0.73 | <0.01 |
| CA (°) | 0.74 | <0.01 |
| CTAD (°) | 0.60 | <0.01 |
| T1-tilt (°) | 0.28 | <0.01 |
CHD coracoid height difference, CRID clavicle–rib intersection difference, CA clavicular angle, CTAD clavicular tilt angle difference, SD standard deviation, mm millimeters
aspearman’s correlation coefficient
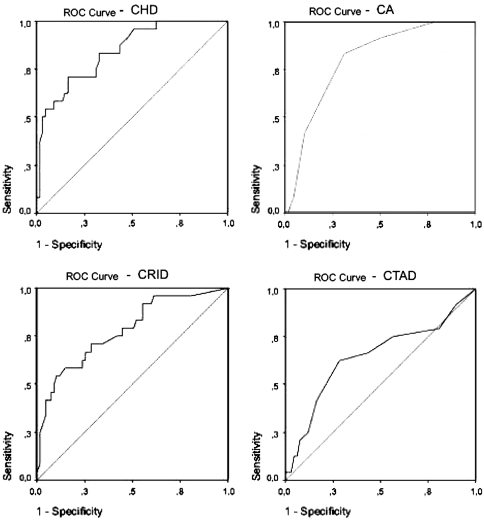
ROC analysis performed for the radiological parameters with a 10 mm cut-off value revealed that all radiological parameters but T1-tilt could predict the above or below 10 mm values for clinical shoulder balance. The area under the ROC curve for CHD, CRID, CA, and CTAD were 0.84, 0.78, 0.80, and 0.65, respectively (Fig. 7; Table 3). All were considered to be statistically significant (p < 0.001 for CHD, CRID, and CA; p = 0.034 for CTAD). We have been able to define cut-off values for different levels of sensitivity and specificity using ROC curve and Youden’s index. For example, CHD values that are >9 mm indicate a clinical shoulder imbalance of >10 mm with a sensitivity of 70.8% and a specificity of 83.6% or CA values of >2.5° indicate that there is a clinical shoulder balance of >10 mm. CRID values >7.1 mm and CTAD values >4.5° indicate clinical shoulder imbalance of >10 mm (Table 3).
Fig. 7.
Receiver operating characteristic (ROC) curves for each radiological parameter
Table 3.
The results of the ROC analysis for radiological methods and the clinical shoulder balance
| Radiological methods | AUC | p | Cut-off | Youden’s index | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|
| CHD (mm) | 0.84 | 0.0001 | 9.0 | 0.544 | 70.8 | 83.6 |
| CRID (mm) | 0.78 | 0.0001 | 7.1 | 0.437 | 54.2 | 89.6 |
| CA (°) | 0.80 | 0.0001 | 2.5 | 0.520 | 83.3 | 68.7 |
| CTAD (°) | 0.65 | 0.034 | 4.5 | 0.341 | 62.5 | 71.6 |
| T1-tilt | 0.48 | >0.05 | 4.5 | 0.068 | 8.3 | 98.5 |
CHD coracoid height difference, CRID clavicle–rib intersection difference, CA clavicular angle, CTAD clavicular tilt angle difference, AUC area under curve
In order to evaluate intraobserver reliability of the radiographic measurement techniques, one of the authors (I.A.) repeated the measurements with 4 week interval by using the same goniometer and marking pen. Since the distribution of the data was normal, intraclass correlation coefficient (ICC) method was used to evaluate the reliability of the methods. The ICC for CHD was 0.83 (0.76–0.89), CA was 0.67 (0.54–0.77), CRID was 0.80 (0.71–0.87), CTAD was 0.50 (0.32–0.64), and T1-tilt was 0.25 (0.05–0.43) (Table 4).
Table 4.
Intraobserver reliability of the radiographic measurement methods
| Radiological methods | ICC | 95% confidence interval | p | |
|---|---|---|---|---|
| Lower | Upper | |||
| CHD (mm) | 0.83 | 0.76 | 0.89 | <0.001 |
| CRID (mm) | 0.80 | 0.71 | 0.86 | <0.001 |
| CA (°) | 0.67 | 0.54 | 0.77 | <0.001 |
| CTAD (°) | 0.50 | 0.32 | 0.64 | <0.001 |
| T1-tilt (°) | 0.25 | 0.05 | 0.43 | <0.01 |
CHD coracoid height difference, CRID clavicle–rib intersection difference, CA clavicular angle, and CTAD clavicular tilt angle difference
Another author (O. K.) performed the radiological measurements by using the same goniometer and marking pen to evaluate the interobserver reliability. Since the distribution of the data was normal, intraclass correlation coefficient (ICC) method was used to evaluate the reliability of the methods. The ICC for CHD was 0.88 (0.72–0.95), CA was 0.89 (0.75–0.96), CRID was 0.89 (0.74–0.95), CTAD was 0.57 (0.18–0.80), and T1-tilt was 0.45 (0.02–0.75) (Table 5).
Table 5.
Interobserver reliability of the radiographic measurement methods
| Radiological methods | ICC | 95% confidence interval | p | |
|---|---|---|---|---|
| Lower | Upper | |||
| CHD (mm) | 0.88 | 0.72 | 0.95 | <0.001 |
| CRID (mm) | 0.89 | 0.74 | 0.95 | <0.001 |
| CA (°) | 0.89 | 0.75 | 0.96 | <0.001 |
| CTAD (°) | 0.57 | 0.18 | 0.80 | <0.01 |
| T1Tilt (°) | 0.45 | 0.02 | 0.75 | =0.02 |
CHD coracoid height difference, CRID clavicle–rib intersection difference, CA clavicular angle, and CTAD clavicular tilt angle difference
Discussion
In anatomical human drawings, the centers of both head and pelvis are situated on the same line, and both sides of the body are symmetric with regard to center line. This is a result of the general assumption that the central sacral line bisects the trunk into two halves that match not only in shape and function but also when the spatial position is taken into account. Asymmetry leading to imbalance may be the consequence of pathology. In addition to diseases of the shoulder girdle (atrophy, tumors) or rib cage (rib anomalies) causing shoulder imbalance, deformities of the spinal column also may cause shoulder imbalance in the absence of these disorders. Spinal deformities not only distort vertebral alignment, but also may result in shoulder, rib cage, and waist line asymmetry. During treatment planning and evaluation of the treatment outcome of a spinal deformity, these parameters should also be taken into account. Inability to address the shoulder balance during surgery or the patient being left with asymmetric shoulders is a measure of failure.
In healthy individuals shoulders are considered to be level, however, there is no study in the literature questioning this general assumption. Kuklo et al. [4] defined shoulder balance as a <1 cm side-to-side difference between the shoulders on clinical examination in adolescent idiopathic scoliosis patients.
In our study, posteroanterior clinical pictures taken as arms on sides simulate a routine clinical examination performed in the daily practice for assessment of the shoulder balance, whereas one may think that patients were asked to evaluate their shoulder balance according to their own mirror image which is an anteroposterior view and this may look like a paradox but the aim was to mimic the clinical examination that is mainly performed from the rear of the patient. Our results showed that in otherwise healthy adolescents the shoulders are not absolutely level. Only 19% had symmetric shoulders; in other words, the heights of their shoulders were equal and 72% had a side-to-side difference of <1 cm. In order to access the shoulder balance perception of the teenagers, we first used three questions of the questionnaire prepared by Kuklo et al. [4] dealing with the shoulder balance perception. Interestingly, none of the subjects were aware of the imbalance as indicated by the questionnaire. This shows that subjects may not have level shoulders even without a spinal deformity or limb length discrepancy. Furthermore, they may be happy with their appearance. In daily practice, any deviation of shoulder balance from exact equality should not be considered abnormal because this may lead to unnecessary treatment attempts. This study demonstrated that healthy adolescents may have up to 27 mm difference between their shoulders without a change in their body image perception.
During the clinical evaluation of patients, we examine the body contours and mainly the soft tissue itself. However, during surgical interventions we are concerned with the radiological skeletal landmarks mostly and use them as a guide during surgical decision making. Therefore, in order to obtain a satisfactory outcome the surgeon needs to know whether these guides are accurate. In this study we combined and evaluated the clinical and radiological scenes in a particular instant. We demonstrated that all radiological parameters significantly correlated with the clinical appearance. Although the majority of the parameters can be used as an indirect measure of clinical shoulder balance, CHD had the highest correlation with the clinical picture, the highest intraobserver reliability and a high interobserver reliability; it is the method of choice. We also demonstrated the cut-off values to differentiate clinically above and below 10 mm difference among shoulders for each radiological parameter.
In daily practice, the shoulders may not be included in the X-ray either due to technical errors or the trend to minimize patients’ radiation exposure, resulting in X-rays that only include the spine. This practice causes problems in measuring shoulder balance with methods using reference points located in this field, such as CHD, CA or CRID. Therefore, we need alternative methods. It was suggested that T1-tilt correlated well with shoulder balance [3], but this was later rejected [2, 5]. Similarly, our results suggest that T1-tilt mildly correlated with shoulder balance, making T1-tilt a weak candidate for this purpose. On the other hand, CTAD was moderately correlated with clinical appearance. This angle is formed by the difference between the angles formed by the bisecting line of the proximal portion of the clavicle and the horizontal. Our results show that it is the method of choice when the shoulders are not included in the X-ray.
There are some limitations to this study. One may criticize not using an objective measure that would evaluate whether they exerted equal amount of pressure on both foot during the study. Although, this is an important technical point, it most likely would not significantly affect our findings. First, it is impossible to evaluate the pressure distribution among both feet without using sophisticated pressure sensors, and second, our approach simulates clinical practice when a spine surgeon evaluates a patient in the clinic where shoulder balance is evaluated without any assistive devices. Although none of the adolescents reported abnormal shoulder perception, this finding may be secondary to the questionnaire that we used in order to evaluate shoulder balance. This questionnaire was in fact designed for scoliotic patients and it may not reveal imbalanced shoulders. However, this questionnaire is the only one in the literature to evaluate shoulder balance.
In summary, the radiological and clinical evaluation of healthy adolescents revealed that the shoulders are not level in the normal population. However, this imbalance does not lead to an asymmetrical body perception among this population. The radiological shoulder balance parameters reliably reflect the clinical appearance, and the method of choice is coracoid height difference when the shoulders are included in the X-ray, and clavicular tilt angle difference when they are not.
References
- 1.Ashton-Miller JA, McGlashen KM, Schultz AB. Trunk positioning accuracy in children 7–18 years-old. J Orthop Res. 1992;10(2):217–225. doi: 10.1002/jor.1100100209. [DOI] [PubMed] [Google Scholar]
- 2.Bago J, Carrera L, March B, et al. Four radiological measures to estimate shoulder balance in scoliosis. J Pediatr Orthop B. 1996;5(1):31–34. doi: 10.1097/01202412-199605010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Ginsburg H, Goldstein L, DeVanny J et al (1997) An evaluation of the upper thoracic curve in idiopathic scoliosis: guidelines in the selection of the fusion area. Presented at the annual meeting of the Scoliosis Research Society, Hong Kong
- 4.Kuklo TR, Lenke LG, Graham EJ, et al. Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine 15. 2002;27(18):2013–2020. doi: 10.1097/00007632-200209150-00009. [DOI] [PubMed] [Google Scholar]
- 5.Lee CK, Denis F, Winter RB, Lonstein JE. Analysis of the upper thoracic curve in surgically treated idiopathic scoliosis. Spine 15. 1993;18(12):1599–1608. doi: 10.1097/00007632-199309000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Yngve Abdominal reflexes. J Pediatr Orthop. 1997;17(1):105–108. doi: 10.1097/00004694-199701000-00022. [DOI] [PubMed] [Google Scholar]