Abstract
We report a multilevel modified vertebral column resection (MVCR) through a single posterior approach and clinical outcomes for treatment of severe congenital rigid kyphoscoliosis in adults. Transpedicular eggshell osteotomies and vertebral column resection are two techniques for the surgical treatment of rigid severe spine deformities. The authors developed a new technique combining the two surgical methods as a MVCR, through a single posterior approach, for surgical treatment of severe congenital rigid kyphoscoliosis in adults. Thirteen adult patients with severe rigid congenital kyphoscoliosis deformity were treated by a single posterior approach using a MVCR technique. The surgery processes included a one-stage posterior transpedicular eggshell technique first, and then expanded the eggshell technique to adjacent intervertebra space through abrasive reduction of the vertebral cortices from inside out. All posterior vertebral elements were removed including the cortical vertebral bone around the neural canal. Range of resection of the vertebral column at the apex of the deformity included apical vertebra and both cephalic and/or caudal adjacent wedged vertebrae. Totally, 32 vertebrae had been removed in 13 patients, with 2.42 vertebrae being removed on average in each case. The average fusion extent was 7.69 vertebrae. Mean operation time was 266 min with average blood loss of 2,411.54 ml during operation. Patients were followed up for an average duration of 2.54 years. Deformity correction was 59% in the coronal plane (from 79.7° to 32.4°) postoperatively and 33.7° (57% correction) at 2 years follow-up. In the sagittal plane, correction was from preoperative 85.9° to 27.5° immediately after operation, and 32.0° at 2 years follow-up. Postoperative pain was reduced from preoperative 1.77 to 0.54 at 2 years follow-up in visual analog scale. SRS-24 scale was from 38.2 preoperatively to 76.9 at 2 years follow-up postoperative. Complications were encountered in four patients (30.7%) with transient neurology that spontaneously improved without further treatment within 3 months. MVCR technique through a single posterior approach is an effective procedure for the surgical treatment of severe congenital rigid kyphoscoliosis in adults.
Keywords: Kyphoscoliosis, Eggshell technique, Vertebral column resection, Modified vertebral column resection
Introduction
Severe congenital rigid congenital kyphoscoliosis in adults remains a big challenge for spine surgeons. Kyphoscoliosis is a deformity with fixed spinal vertebrae that does not allow traction, suspension, or side bending of the spine. The lack of a mobile spine frequently results in early truncal decompensation and a large compensatory curve, which may progress with time [36]. Rigid congenital kyphoscoliosis in adults usually occur with functional impairment and neurologic complications, and pain is a common symptom [9, 21, 22, 26].
The physiologic and mechanical issues inherent in the kyphoscoliosis are still challenging. Surgery is the common treatment at present. However, the surgical techniques for correcting the deformity are difficult and controversial. Usually, vertebral column resection (VCR) is a technique designed for rigid severe kyphoscoliosis deformities. VCR enables translation of spinal column and offers the advantage of a controlled manipulation of both the anterior and posterior column with active reconstruction [10, 24]. Combined anterior and posterior VCR requires a lengthy operation and has the possibility to harm the anterior vascular and visceral structures [18, 32, 35]. For severe rigid adult congenital spinal kyphoscoliosis, it is a common practice that more than one VCR has to be done to provide enough correction with substantial risks.
Transpedicular eggshell osteotomy is an alternative method to treat kyphoscoliosis [9, 15, 23, 25]. But for severe rigid adult spinal kyphoscoliosis, eggshell technique alone cannot provide adequate correction. To minimize the technical difficulties during the operation process and assure the best surgical effects, the authors developed a new method, combining transpedicular eggshell osteotomies and VCR in one procedure, and this new method is termed as “modified VCR (MVCR).” The authors here reported the clinical outcomes of 13 adult patients with severe rigid spinal congenital kyphoscoliosis, who have been treated by multilevel MVCR technique.
Material and methods
From 2003 to 2005, 13 cases of severe rigid adult congenital kyphoscoliosis (Cobb >75° in sagittal plane) were treated with multilevel MVCR technique. The clinical records were reviewed for demographic data, etiology of the lesion, operating time, average operative and postoperative blood loss, functional improvement, and complications. Clinical outcome was measured with the SRS-24, and the pain at the lumbosacral region was evaluated using a visual analog scale (VAS) preoperatively and at 2 years postoperation.
There were six males and seven females; average age at surgery was 31.03 years (range 20.5–43.2 years). Etiologies of these 13 deformities were congenital kyphoscoliosis with posterolateral hemivertebra (fully segmented hemivertebrae were found in five cases, and wedge vertebrae were in eight cases). The average inequality of leg length was less than 1 cm before surgery. All patients had truncal imbalance before surgery in coronal or sagittal plane. Before surgery, three patients (23%) presented with neurologic compromise. Among them, one patient presented with neurogenic claudication and two patients had radicular pain. In our patient group, there were six patients (46%) with intractable back pain.
Standard radiographic measurements were made from standing postero-anterior and lateral radiographs taken before surgery, 2 weeks after surgery, 2 years follow-up, and at most recent follow-up to assess deformity correction, spinal balance, complications related to the instrumentations, and any evidence of pseudarthrosis. There were three cases with hemivertebra at L2; seven cases of thoracolumbar curves, with hemivertebra at T12 or L1; three cases with hemivertebra at T11. Coronal and sagittal balance preoperatively and at postoperative stages were measured as described by Glassman et al. [13], that is, coronal balance was measured as the distance between the C7 plumb line and the center sacral line. Sagittal balance was measured as the distance between C7 plumb line and the posterior superior corner of S1. The trunk imbalance was 28.7 mm in the coronal plane and 41.7 mm in the sagittal plane. The curve was measured by the Cobb method in the coronal plane. Kyphosis was measured by Cobb method between the two most tilted vertebrae in the sagittal plane. The coronal and sagittal curves averaged 79.7° (range 70.4°–110.8°) and 85.9° (range 78.2°–105.1°), respectively (evaluated with Cobb method). On the left and right lateral spine-bending films, spontaneous deformity corrections of both primary and secondary curves were 17.73 ± 2.48%.
All patients went preoperative and 2 years follow-up VAS and SRS-24 scale test to analyze the function condition. They were also evaluated with preoperative full-length spinal cord MRI for neurological abnormalities. One case had cryptorachischisis, another one had low set of spinal cord or cauda eguina, but these two cases were without neurological symptoms. Computerized tomography with 3-D reconstruction imaging was routinely carried out preoperatively in all the patients for determining the range of kyphoscoliosis and the position of apical vertebra. There were ten cases that had 3-D reconstruction imaging examination at 2 years follow-up. In addition, we routinely obtained pulmonary function testing (PFT) for all patients before surgery and postoperatively.
Surgical techniques
All surgeries were performed by the first author under motor-evoked potential monitoring. No preoperative embolization of the affected vertebra was performed. Maquet operation table was used. Patients were positioned such that biplanar imaging could be performed during operation. With the patients placed in prone position, the incision could be a straight posterior midline or curve incision depending on the type and size of the deformity.
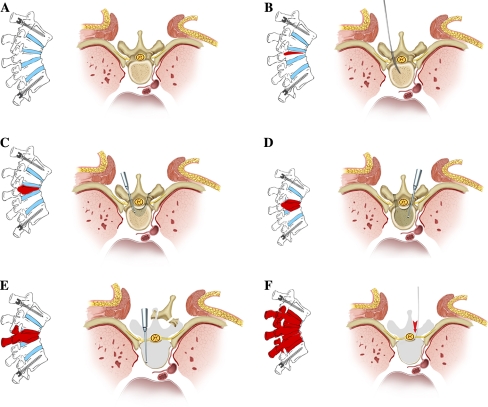
With the spine exposed, pedicle screws were first inserted according to the preoperative plan (Fig. 1a). With intraoperative radiograph controls, two or three pairs of pedicle screws were inserted into the vertebrae, which were cephalic or caudal accordingly with free-handed fashion (Fig. 1a). A stabilizing rod was preset on the concaved side. The dissection was then carried out according to the characteristics of apical vertebra and adjacent wedged vertebrae according to the preoperative 3-D CT reconstruction images. For the dissecting segments, a probe was used to determine the entry point and depth (Fig. 1b). After enlarging the entry with a curette, a 5-mm burr was used to perform regular “eggshell” technique with icy water flush, and during this process the inner wall of the pedicle was kept as intact as possible (Fig. 1c). The entry was further enlarged both cephalically and caudally to penetrate the corresponding walls, and small amount of bony wall was kept to protect the nerve roots from upper and lower segments (Fig. 1d). When the end-plates of the upper and lower intervertebral space were exposed, a Kerrison rongeur or burr was used to abrade the anterior and lateral walls of the vertebral body, which was then collapsed under pressure laterally to expose the posterior walls further (Fig. 1e). Then a similar vertebral body resection was advanced to cross the midline in an abrasive way with the burr. The upper and lower end-plates of the resected vertebra as well as intervertebral discs were removed with a curette (Fig. 1f). The same MVCR process was carried out for other wedged vertebra on the same side. Once the concaved side was completed, the rod was then pre-set on the convex side. MVCR was completed in the convex side in the same fashion. During the surgery, absorbable hemostatic gauze and gelatin sponge were packed at the wound sites for stopping bleeding.
Fig. 1.
Diagram illustration of the MVCR procedure. a Pedicle screws were inserted into the vertebrae; a stabilizing rod was preset on the concaved side. b A probe was used to determine the entry point and depth in the dissecting segment. c After enlarging the entry with a curette, a 5-mm burr was used to perform regular “eggshell” technique, and during this process, the inner wall of the pedicle was kept as intact as possible. d The entry was further enlarged both cephalically and caudally to penetrate the corresponding walls, and small amount of bony wall was kept to protect the nerve roots. e When the end-plates of the upper and lower intervertebral space were exposed, a Kerrison rongeur or burr was used to abrade the anterior and lateral walls of the vertebral body, which was then collapsed under pressure laterally to expose the posterior walls further. f Then a similar vertebral body resection was advanced to cross the midline in an abrasive way with the burr. Adjacent upper and lower end-plates as well as intervertebral discs were removed with a curette
Following vertebral removal, spinous process, vertebral lamina, facet joints, and the transverse process of those resected vertebrae were all carefully removed. Posterior structures, as described earlier, of adjacent vertebra were also partially removed. Kerrison rongeur or curette was used to abrade the inner and posterior walls of vertebral canal. Nucleus pulposus punch may be used to remove the spongy bone of posterior wall when necessary. In this way, MVCR was accomplished with one similar transpedicular expanded eggshell technique. Conjunction between the rod and screw was then inserted as we placed the rods on both convex and concaved sides with the interconnecting linkage bar enclosing the space left by MVCR. The spine was then shortened, while segmental compression was achieved. After internal fixation, autograft of bone chips was implanted into the residual intervertebral spaces. In some cases, when the multilevel posterior structures were removed, the posterior gap was not able to close just by compression with the rods; we then harvested iliac bone sticks and implanted them into the posterior space and/or placed them over the transverse processes. Closed suction drains were inserted at the resection sites, and the surgical wound was closed layer-by-layer.
Three methods were used to save or replace the blood supply: (1) Cell saver was used to save blood during operation, and usually 800–1,400 ml of blood could be saved and refused back to the patient; (2) At the same time, blood from the blood bank had also been given to the patient when necessary; (3) The first 6 hours blood drain was collected by using a postoperation cell saver (Stryker, USA) and given back to the patient (the average volume of the blood saved was about 350–700 ml).
Postoperation care
The patients were allowed to sit up in bed 24 h after the surgery. Postoperative loss through the drains was measured and recorded everyday (see Table 1). Usually, the drain was removed when the blood loss through drain was less than 50 ml per 24 h. Patients were allowed out of bed with a custom-made plastic thoracolumbosacral orthosis (TLSO) at the second postoperative week. The TLSO for those two-segment resection patients was kept for 3 months, and for those three-segment MVCR patients, the TLSO was kept for 6 months.
Table 1.
Patients condition
| Patients | Operation condition | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Gender | Age at operation (years + months) | Hemi site | Follow-up | MVCR | Blood loss operation (ml) | Estimated blood (%) | Blood loss postop (ml) | Estimated blood (%) | Operation time (min) | Fused segment |
| 1 | F | 27 + 5 | T11 | 2 years 11 months | 2.5 | 2,500 | 57 | 750 | 17 | 310 | 7 |
| 2 | F | 20 + 6 | L1 | 2 years 7 months | 3 | 3,000 | 79 | 1,910 | 51 | 310 | 7 |
| 3 | F | 43 + 2 | L1 | 2 years 8 months | 3 | 3,200 | 79 | 860 | 21 | 210 | 7 |
| 4 | F | 28 + 1 | T11/12 | 3 years 2 months | 2 | 2,100 | 57 | 780 | 21 | 245 | 7 |
| 5 | M | 40 + 7 | T12 | 2 years 2 months | 2 | 1,800 | 31 | 665 | 11 | 250 | 8 |
| 6 | M | 21 + 11 | T11 | 3 years 3 months | 3 | 3,000 | 54 | 585 | 10 | 245 | 8 |
| 7 | M | 30 + 6 | T11 | 2 years 4 months | 3 | 2,700 | 54 | 490 | 9 | 350 | 12 |
| 8 | F | 22 + 10 | L2 | 2 years 1 month | 2.5 | 2,800 | 70 | 590 | 15 | 260 | 8 |
| 9 | F | 41 + 5 | L1 | 2 years | 2.5 | 1,950 | 47 | 770 | 18 | 245 | 8 |
| 10 | M | 36 + 10 | L2 | 2 years 5 months | 2 | 2,600 | 44 | 830 | 14 | 220 | 7 |
| 11 | F | 29 + 2 | L2 | 2 years 3 months | 2.5 | 1,800 | 44 | 950 | 23 | 305 | 7 |
| 12 | M | 38 + 7 | L1 | 2 years 9 months | 2 | 1,900 | 40 | 990 | 18 | 208 | 7 |
| 13 | M | 22 + 6 | T12 | 2 years 4 months | 2 | 2,000 | 37 | 430 | 8 | 300 | 7 |
| Average | 31 + 0 | 2.54 years | 2.46 | 2,411.54 | 54 | 815.38 | 18 | 266 | 7.69 | ||
Results
Totally, 32 vertebrae had been removed in 13 patients, with 2.42 vertebrae being removed on average in each case (range 2–3 vertebrae). Intraoperative measurements of spine-column-shortening were 34 mm (range 28–48 mm). Average fusion extend was 7.69 vertebrae (range 7–12 vertebrae). Mean operating time was 266 min (range 208∼350 min), with average blood loss of 2,411.54 ml (range 1,800–3,200 ml) during operation, and the postoperative blood loss through drain was 815.38 ml in average (Table 1). The drain was kept for 5.7 days (4–8 days).
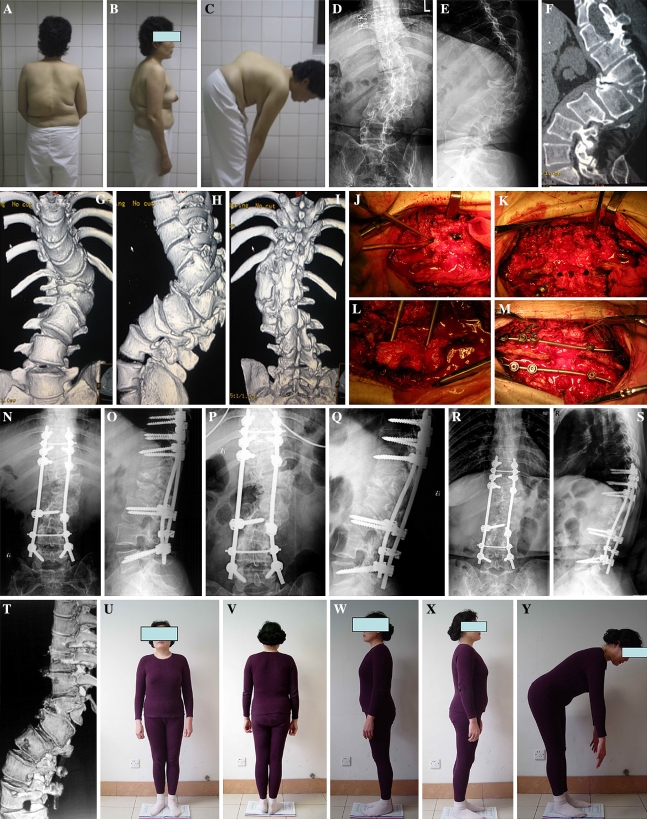
Every patient in the study finished at least 2 years of follow-up and an average of 2.54 years (range 2–3.2 years) with radiological and physical evaluations to assess spinal balance and decompensation. Deformity correction was 59% in the coronal plane postoperatively (from 79.7° to 32.4°) and 33.7° (57% correction) at 2 years follow-up. In the sagittal plane, deformity correction was from preoperative average 85.9° to 27.5° immediately after operation, and 32.0° at 2 years follow-up. Bony fusion could be seen in all of their radiographs 2 years after surgery (Fig. 2). Postoperative coronal and sagittal balances were improved to 12.1 and 20.7 mm, showing an improvement of 16.6 and 21 mm, respectively. At 2 years follow-up, all patients had satisfied spinal balance; postoperative coronal and sagittal balances were 17.4 and 28.06 mm (Table 2). Average preoperative VAS was 1.77 and reduced to 0.54 at 2 years follow-up in VAS. The improvement of patients VAS was significant. SRS-24 scale was from preoperative 38.2 to 76.9 at 2 years following up postoperative. Pain, general self-image, function from back condition, and level of activity all demonstrated statistically significant improvement as compared with preoperative status (P < 0.05) (Table 3).
Fig. 2.
A 43-year-old woman who presented with hemivertebra kyphoscoliosis deformity with dysplasia of several vertebrae adjacent to the apical vertebra. a–c Preoperative outlook. d, e Radiographic evaluation found that the apical hemivertebra of kyphoscoliosis was L1; the curve in coronal and sagittal plane was 75.4° and 84.1°, respectively. f–i Computerized tomography and 3-D reconstruction images revealed that the apical vertebra and its adjacent vertebrae of T12 and L2 had severe wedged deformity on anterior, posterior, and lateral views having a local kyphosis deformity of 95.2°, which was far more severe than X-ray measurement. j–m MVCR surgical procedure was carried out to resect the vertebrae of T12, L1, and L2, with posterior pedicle screw fixation, vertebrae compression, and fusion with bone chip autograft. n, o The deformity was corrected to 36.3° and 12.2° in the coronal and sagittal plane, respectively, as shown in the corresponding radiographs. p, q 6-month follow-up. r, s 2-year follow-up X-ray measurement: her deformity was 36.4° and 25.6° in the coronal and sagittal plane, respectively, and fusion can be found both in X-ray and 3-D reconstruction images. t 3-D reconstruction images. u–y 2-year follow-up outlook image
Table 2.
Coronal and sagittal balance
| Case | Coronal balance | Sagittal balance | ||||
|---|---|---|---|---|---|---|
| Preop (mm) | Postop (mm) | 2 years postop (mm) | Preop (mm) | Postop (mm) | 2 years postop (mm) | |
| 1 | 25.1 | 20.3 | 28.6 | 40.7 | 20.7 | 27.5 |
| 2 | 34.4 | 10.7 | 15.5 | 43.5 | 22.4 | 30.7 |
| 3 | 53.5 | 18.6 | 26.4 | 51.3 | 24.7 | 24.5 |
| 4 | 10.7 | 2.8 | 6.5 | 37.6 | 18.4 | 18.7 |
| 5 | 24.8 | 14.2 | 14.2 | 30.5 | 21.7 | 22.4 |
| 6 | 13.4 | 7.5 | 15.2 | 36.7 | 15.4 | 27.8 |
| 7 | 28.8 | 11.6 | 20.6 | 35.2 | 17.6 | 19.4 |
| 8 | 42.3 | 19.8 | 27.8 | 48.7 | 26.4 | 35.9 |
| 9 | 36.9 | 25.4 | 27.6 | 42.5 | 19.8 | 20.3 |
| 10 | 17.9 | 3.2 | 4.4 | 40.7 | 25.6 | 35.1 |
| 11 | 37.2 | 8.2 | 10.2 | 50.5 | 17.8 | 34.1 |
| 12 | 21.2 | 4.5 | 18.8 | 39.7 | 23.9 | 39.7 |
| 13 | 26.6 | 10.6 | 10.3 | 45.4 | 15.6 | 28.7 |
| Average | 28.67 | 12.10 | 17.39 | 41.76 | 20.76 | 28.06 |
Table 3.
Correction of deformity, PFT, and scales
| Case | Coronal plane | Sagittal plane | Pulmonary function test | SRS24 scale | Visual analog scale | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop (°) | Postop (°) | Correction (%) | 2 years postop (°) | 2 years correction (%) | Preop (°) | Postop (°) | 2 years postop (°) | FVC | FEV-1 | Preop | 2 yrs postop | Preop | 2 yrs postop | |||
| Preop | Postop | Preop | Postop | |||||||||||||
| 1 | 78.2 | 24.4 | 69 | 26.3 | 67 | 78.2 | 31.3 | 33.3 | 2.50 | 2.47 | 2.11 | 2.51 | 42 | 82 | 0 | 0 |
| 2 | 70.4 | 24.3 | 66 | 24.6 | 66 | 92.5 | 35.7 | 41.8 | 2.03 | 2.5 | 1.97 | 1.77 | 38 | 79 | 0 | 0 |
| 3 | 75.4 | 36.4 | 52 | 36.3 | 52 | 84.1 | 12.2 | 25.6 | 3.40 | 3.71 | 2.85 | 2.95 | 40 | 81 | 4 | 0 |
| 4 | 70.6 | 35.8 | 50 | 40.6 | 43 | 105.1 | 20.0 | 30.6 | 2.83 | 2.74 | 2.36 | 2.46 | 31 | 72 | 0 | 0 |
| 5 | 80.7 | 30.8 | 63 | 31.6 | 61 | 81.6 | 30.1 | 31.7 | 3.30 | 3.48 | 3.02 | 3.12 | 36 | 77 | 5 | 4 |
| 6 | 77.2 | 42.2 | 45 | 40.8 | 48 | 78.3 | 23.4 | 26.8 | 3.41 | 3.59 | 3.18 | 3.11 | 45 | 85 | 0 | 1 |
| 7 | 110.8 | 34.2 | 69 | 33.1 | 70 | 79.3 | 35.5 | 39.3 | 3.67 | 3.72 | 2.40 | 2.50 | 40 | 75 | 0 | 0 |
| 8 | 74.9 | 28.1 | 62 | 35.1 | 53 | 79.8 | 38.1 | 41.3 | 2.73 | 2.54 | 2.50 | 2.60 | 41 | 78 | 2 | 0 |
| 9 | 75.1 | 32.4 | 57 | 32.8 | 57 | 78.9 | 29.9 | 28.2 | 2.91 | 3.08 | 2.37 | 2.07 | 39 | 76 | 6 | 0 |
| 10 | 95.5 | 37.7 | 61 | 39.2 | 59 | 88.4 | 33.3 | 37.2 | 3.50 | 3.62 | 2.90 | 3.00 | 44 | 83 | 3 | 1 |
| 11 | 81.5 | 38.8 | 53 | 37.2 | 54 | 93.2 | 27.4 | 31.1 | 2.24 | 2.01 | 1.80 | 1.90 | 35 | 76 | 0 | 0 |
| 12 | 75.7 | 23.1 | 69 | 24.4 | 68 | 79.2 | 19.6 | 21.9 | 2.17 | 2.26 | 1.96 | 2.06 | 40 | 77 | 3 | 1 |
| 13 | 70.7 | 32.3 | 54 | 36.7 | 49 | 99.1 | 21.7 | 27.5 | 3.15 | 3.23 | 2.74 | 2.34 | 25 | 60 | 0 | 0 |
| Average | 79.75 | 32.35 | 59 | 33.75 | 57 | 85.98 | 27.55 | 32.02 | 2.90 | 2.99 | 2.50 | 2.49 | 38.15 | 76.92 | 1.77 | 0.54 |
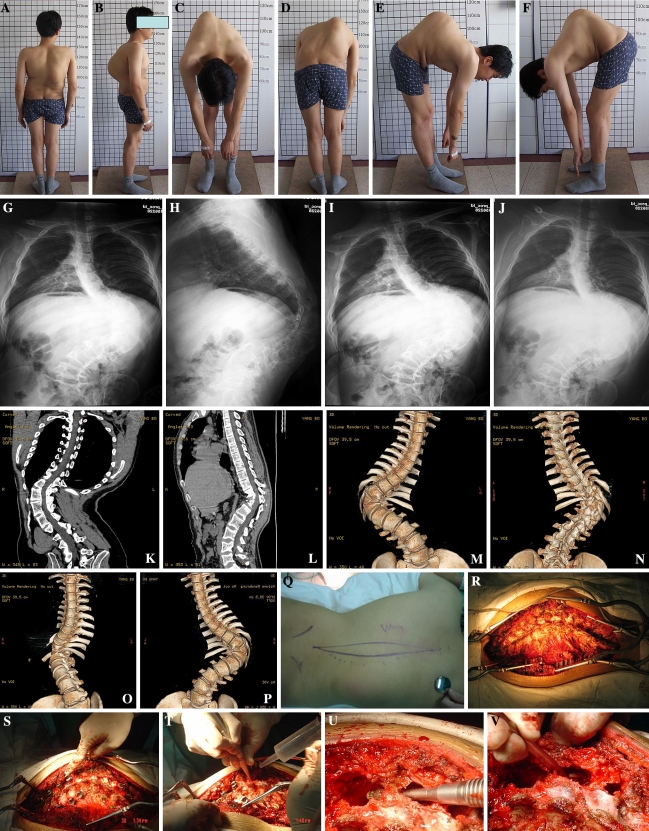
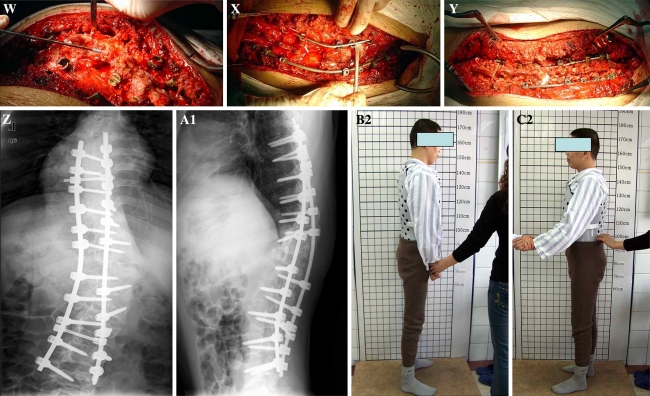
Complications were encountered in four patients (30.7%), including two with transient neurology complications, one with wound problem, and one with pleural membrane rapture. One patient was detected of transient neurologic deficit, immediately after surgery (ASIA grade is D); the symptoms were alleviated 1–2 weeks after operation without any intervention (ASIA grade is E). Two-year follow-up showed that his VAS was 0 and his movement was normal. Another patient (case no. 7, Fig. 3) was 30 years old when operated. During the MVCR process (rod rotation process to the maximal extent), a change had been found in evoked potentials monitoring meeting warning criteria, and then we closed the wound immediately and stopped the operation. He was found to have incomplete paraplegia postoperatively (ASIA grade is C). Methylprednisolone was administered for 24 h continuously. At 29 h postoperation, the patient recovered to normal sensory and muscle strength of grade IV. He recovered completely at 6 weeks postoperation (ASIA grade is E).
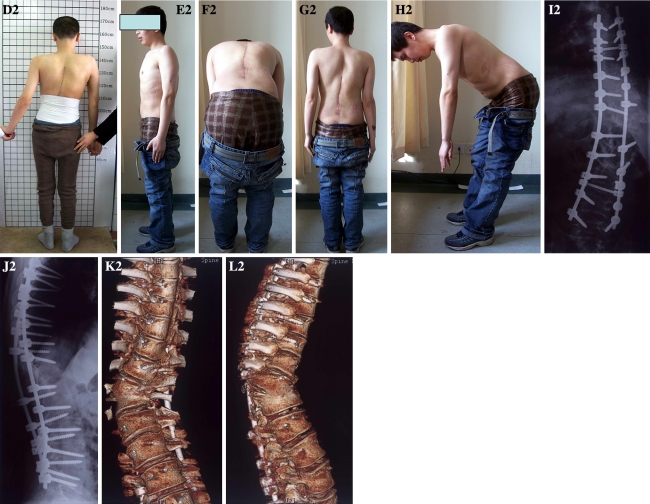
Fig. 3.
a–f A 30-year-old man who presented with hemivertebra (T11) kyphoscoliosis deformity with dysplasia of several vertebrae adjacent to the apical vertebra. g–j His preoperative coronal and sagittal deformities were 110.8° and 79.3°, respectively. k–p Computerized tomography and 3-D reconstruction images revealed that the apical vertebra and its adjacent vertebrae of T10 and T12 had severe wedged deformity on anterior, posterior, and lateral views. q–y He was treated with three-level MVCR to resect the vertebrae of T10, T11, and T12, with posterior pedicle screw fixation, vertebrae compression, and fusion with bone chip autograft, and 12 segments were fused. z–a1 Right after operation, his deformity correction in coronal and sagittal plane was 34.2° and 35.5°, respectively. b2–d2 The patient outlook image 2 weeks after operation; he needed other people’s help to stand up because of his recent recovery from temporary paraplegina postoperatively. e2–h2 The patient outlook image 2 years after operation. i2–l2 Two-year follow-up X-ray measurement: his deformity was 33.1° and 39.3° in the coronal and sagittal plane, respectively, and fusion can be found both in X-ray and 3-D reconstruction images
There was one case of wound problem: 0.5 × 0.7 cm2 skin damage was caused by electrotome at the edge of wound incision. Fat liquefaction was found postoperatively. We kept changing dressing everyday and finally, wound healed about 20 days later. For the case of pleural membrane rupture, the complication was caused during operation when we tried to expose the rid head widely from concave side. We closed the rupture area by suturing the pleural membrane carefully, and air-proof test in water was used to make sure the closing had very good effect. It has been proved by postoperative X-ray that there was a little “air” in the thoracic cavity, and the air disappeared 1 week later when we checked the thoracic cavity by X-ray again.
Discussion
Adult severe rigid congenital kyphoscoliosis has been a persistent and perplexing problem [19, 20, 27, 37]. The operative or nonoperative treatments often fail, resulting in a three-dimensional deformity at coronal, sagittal, and frontal planes [2, 16, 29, 30]. In contrast to the adolescent scoliosis, which is usually asymptomatic, the adult scoliosis patients usually present with back pain [34, 38]. In addition, adult patients are more likely to experience symptoms of spinal stenosis and radiculopathy from osteoarthritis and rotatory subluxation, which may lead to nerve root impingement and stretching. Decreased vital capacity and other parameters of pulmonary function may occur in patients with severe thoracic curves, especially in the presence of thoracic lordosis, which effectively decreases the anterior/posterior chest diameter. Finally, the psychological impact of chronic pain and deformity must be considered. In a world where appearance and health become increasingly important for social acceptance and well-being, the inability to function at the level of one’s peers due to pain or deformity can create a huge psychological burden. As the recognition, evaluation, and treatment of spinal deformity continues to progress, there are many emerging new methods for the treatment of kyphoscoliosis, including common VCR, SPO (Smith-Petersen osteotomy), PSO (pedicle subtraction osteotomy), PVCR, and eggshell methods [5, 8, 28, 33]. In general, for minor degree of imbalance and curve less than 70° and 50° in coronal and sagittal planes, posterior soft tissue release with compression on the convex side should be sufficient to produce moderate correction and balance [11]. For rigid kyphoscoliosis (>75° in sagittal plane), VCR (including PVCR) and eggshell methods are the most popular techniques at present.
Vertebrectomy was first illustrated in 1922 by Mac-Lennan, who demonstrated an apical resection from a posterior-only approach with postoperative casting for the treatment of severe scoliosis [29]. However, most of the patients had complications of nerve injuries and infection, which showed poor results. Several authors have subsequently reported their experiences with vertebrectomy, mostly for congenital scoliosis. In 1987, Bradford presented a modification of vertebrectomy, in which the apical vertebra was subperiosteally dissected and a rongeur was used to remove the vertebral body from posterior longitudinal ligament. Posterior fixation with instrumentation at first or second stage was completed to correct the spine deformity with resection of posterior elements. In another report, Bradford et al. [4] investigated 24 patients with rigid coronal decompensation who underwent anterior–posterior VCR, spinal shortening, and posterior instrumentation. Coronal and sagittal decompensations were corrected to 82 and 87%, respectively. Preoperative scoliosis averaging 103° was corrected to 49° with an improvement of 52%. In 2002, Suk et al. reported the procedure of PVCR, which combined the technique of spine tumor resection [31]. The posterior elements were resected to remove the rib head articulation. Anterior vertebral body was subperiosteally exposed, dissected, and compressed for shortening correction by instrumentation. In their series, mean operation time was 4 h 31 min with average blood loss of 2,333 ml. The deformity correction was 61.9% in the coronal plane and 45.2% in the sagittal plane. Complications were encountered in 24 patients (out of 143 cases): two complete cord injuries in severe adult scoliosis and thoracic kyphosis patient who had significant preoperative cord compromise, six hematomas, four root injuries (all incomplete), five fixation failures, two infections, and five hemopneumothoraxes [31]. Since then, the PVCR method became more popular and widely accepted for correction of kyphosis deformity of spine.
However, for severe rigid kyphoscoliosis in adults (Cobb >75° in sagittal plane), single-level PVCR often could not fulfill the task of satisfactory deformity correction. But multilevel PVCR was extensive and aggressive with longer operating time, greater amount of blood loss, and with higher risks of complications [4, 5]. In the 1970s, Heinig developed the “eggshell” procedure, a technique to allow anterior decompression and posterior fusion through a posterior transpedicular approach [12]. The “eggshell” procedure is a salvage technique reserved for complex reconstructive problems in the treatment of acute trauma, deformity, tumor, or infection. The goal of the Heinig’s procedure [15] was to achieve similar deformity correction, neural decompression, and stabilization with fewer complications. The eggshell technique encompasses procedures ranging from simple transpedicular decompression and posterior fusion to more complex procedures, including transpedicular vertebrectomy and strut-grafting or pedicle subtraction (closing wedge) osteotomy with posterolateral fusion [1, 6, 7]. The key point of operation includes beginning with smaller curettes and gradual decancellation through the pedicle. Progressively larger curettes were then used, with care to preserve the medial pedicle wall and posterior wall of the vertebral body. The transverse process could be removed and exposed to the lateral pedicle wall. Curettage is carried out across the midline and cephalad through the adjacent disc space. After completing decancellation, the medial pedicle wall is removed followed by the posterior wall using down-going bone tamps. Several authors have reported high success rates with the eggshell procedure for the treatment of spine deformity and trauma [1, 3, 12, 14, 17, 25].
The eggshell technique is not always adequate for satisfactory deformity correction, and the degree of deformity correction was less than that of PVCR method. To obtain better correction results, the first author combined PVCR and eggshell techniques together, and designed a modified technique for multilevel VCR (MVCR) for the treatment of severe rigid adult spinal kyphoscoliosis deformity. The surgical process combined one-stage posterior transpedicular eggshell technique with VCR procedure. The key steps of MVCR technique are illustrated in Fig. 1 and are summarized as follows. (1) At the start, the posterior structure such as spinous processes and lamina were left intact to minimize the blood loss. (2) Once the transpedicular process was completed, a 5-mm burr was used to decancellate through the pedicle. In our experience, the use of burr could control bleeding effectively and was proved to be safer than curettes. (3) When performing “eggshell” technique, the inner wall of the pedicle should be kept intact to protect the nerve roots from upper and lower segments. (4) Once entering into the vertebra, leave a thin wall of cortical bone at the anterior, lateral, and posterior parts of the vertebra. This was different from PVCR technique, in which the anterior and lateral walls were removed, only leaving the soft tissue anterior to the vertebral body intact. The entry was further enlarged both cephalically and caudally to penetrate the end-plates of the vertebra to expose the upper and lower intervertebral spaces. (5) Adjacent upper and lower end-plates as well as intervertebral discs should then be removed with a curette. (6) It should be noted that removal of posterior structures should begin with lateral elements, and posterior structures such as spinous processes and lamina should all be removed.
In our experience, MVCR technique can remove single vertebra as well as multiple adjacent vertebrae. The use of burr allows easy manipulation and reduces the risk of neurological damage. Since removal of the posterior structures (the inner and posterior walls of vertebral canal) was the final step of this procedure, it reduces blood loss. In our study, the mean operating time was 266 min (range 208–350 min), with average blood loss of 2,411.54 ml (range 1,800–3,200 ml), which was much less than VCR in time and blood loss. Using the MVCR technique, we have successfully corrected the deformities in 13 cases of severe rigid adult spinal congenital kyphoscoliosis. Among the 13 cases, only two cases had temporary nerve injuries and eventually recovered completely in a short duration. Our MVCR technique also exhibits superiority in managing the cases of previous fixation failure for severe rigid adult spinal kyphoscoliosis.
Several authors reported that after VCR and spine shortening, the spine should be fused anteriorly with titanium meshwork implant and bone chips autografts to maintain long-term fusion [27, 37]. We grafted autologous bone chips into latero-anterior intervertebral spaces and iliac bone sticks into posterior interspaces, which led to satisfactory fusion and long-term stability as demonstrated by the follow-up, and no pseudarthroses and neurological damage were found in any of the 13 patients. We believe that during removal of the inner and posterior walls of the vertebral canal, it is very difficult to control hemorrhage from epidural venous plexus with either the bipolar electrocoagulation or absorbable hemostatic gauze. The key point to avoid excessive bleeding is to abrade the vertebral bony structures with burr before removal of the inner and posterior walls of vertebral canal, which minimizes the interference to epidural venous plexus and operating time.
In conclusion, the reported MVCR technique employing the combined PVCR and eggshell techniques is an alternative to the conventional anterior–posterior VCR or PVCR methods. MVCR can provide larger extent deformity correction than eggshell, and this procedure can effectively correct combined deformities involving coronal and sagittal planes of the spine. Other advantages include the high fusion rates, acceptable operation time and bleeding, and low risk of surgery-associated complications. However, MVCR is a technically demanding and exhausting procedure with some potential risks of complications.
References
- 1.Baba H, Maezawa Y, Kamitani K, et al. Osteoporotic vertebral collapse with late neurological complications. Paraplegia. 1995;33:281–289. doi: 10.1038/sc.1995.64. [DOI] [PubMed] [Google Scholar]
- 2.Boachie-Adjei O, Ferguson JA, Pigeon RG, Peskin MR. Transpedicular lumbar wedge resection osteotomy for fixed sagittal imbalance: surgical technique and early results. Spine. 2006;31(4):485–492. doi: 10.1097/01.brs.0000199893.71141.59. [DOI] [PubMed] [Google Scholar]
- 3.Bradford DS, Boachie-Adjei O. One-stage anterior and posterior hemivertebral resection and arthrodesis for congenital scoliosis. J Bone Joint Surg Am. 1990;72:536–540. [PubMed] [Google Scholar]
- 4.Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine. 1997;22(14):1590–1599. doi: 10.1097/00007632-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, Baldus C, Blanke K. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine. 2003;28(18):2093–2101. doi: 10.1097/01.BRS.0000090891.60232.70. [DOI] [PubMed] [Google Scholar]
- 6.Bridwell KH. Causes of sagittal spinal imbalance and assessment of the extent of needed correction. Instr Course Lect. 2006;55:567–575. [PubMed] [Google Scholar]
- 7.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine. 2006;31(19 suppl):S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 8.Cho KJ, Bridwell KH, Lenke LG, Berra A, Baldus C. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine. 2005;30(18):2030–2037. doi: 10.1097/01.brs.0000179085.92998.ee. [DOI] [PubMed] [Google Scholar]
- 9.Danisa OA, Turner D, Richardson WJ. Surgical correction of lumbar kyphotic deformity: posterior reduction “eggshell” osteotomy. J Neurosurg. 2000;92(suppl 1):50–56. doi: 10.3171/spi.2000.92.1.0050. [DOI] [PubMed] [Google Scholar]
- 10.Domanic U, Talu U, Dikici F, et al. Surgical correction of kyphosis: posterior total wedge resection osteotomy in 32 patients. Acta Orthop Scand. 2004;75:449–455. doi: 10.1080/00016470410001231-1. [DOI] [PubMed] [Google Scholar]
- 11.Gabos Peter G. Treatment strategies in congenital scoliosis. Contemp Spine Surg. 2005;6(7):47–51. [Google Scholar]
- 12.Gertzbein SD, Harris MB. Wedge osteotomy for the correction of posttraumatic kyphosis. Spine. 1992;17:374–379. doi: 10.1097/00007632-199203000-00025. [DOI] [PubMed] [Google Scholar]
- 13.Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 14.Hardaker WT, Jr, Cook WA, Jr, Friedman AH, et al. Bilateral transpedicular decompression and Harrington rod stabilization in the management of severe thoracolumbar burst fractures. Spine. 1992;17:162–171. doi: 10.1097/00007632-199202000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Heinig CA. Eggshell procedure. In: Luque ER, editor. Segmental spinal instrumentation. Thorofare: Slack; 1984. pp. 221–230. [Google Scholar]
- 16.Kalra KP, Dhar SB, Shetty G, Dhariwal Q. Pedicle subtraction osteotomy for rigid post-tuberculous kyphosis. J Bone Joint Surg Br. 2006;88(7):925–927. doi: 10.1302/0301-620X.88B7.17366. [DOI] [PubMed] [Google Scholar]
- 17.Kawahara N, Tomita K, Baba H, et al. Cadaveric vascular anatomy for total en bloc spondylectomy in malignant vertebral tumors. Spine. 1996;21:1401–1407. doi: 10.1097/00007632-199606150-00001. [DOI] [PubMed] [Google Scholar]
- 18.Kieffer J, Dubousset J. Combined anterior and posterior convex epiphysiodesis for progressive congenital scoliosis in children aged ≤5 years. Eur Spine J. 1994;3:120–125. doi: 10.1007/BF02221453. [DOI] [PubMed] [Google Scholar]
- 19.Kwon BK, Elgafy H, Keynan O, Fisher CG, Boyd MC, Paquette SJ, Dvorak MF. Progressive junctional kyphosis at the caudal end of lumbar instrumented fusion: etiology, predictors, and treatment. Spine. 2006;31(17):1943–1951. doi: 10.1097/01.brs.0000229258.83071.db. [DOI] [PubMed] [Google Scholar]
- 20.Macagno AE, O’Brien MF. Thoracic and thoracolumbar kyphosis in adults. Spine. 2006;31(19 suppl):S161–S170. doi: 10.1097/01.brs.0000236909.26123.f8. [DOI] [PubMed] [Google Scholar]
- 21.McMaster MJ, Ohtsuka K. The natural history of congenital scoliosis: a study of two hundred and fifty-one patients. J Bone Joint Surg Am. 1982;64:1128–1147. [PubMed] [Google Scholar]
- 22.McMaster MJ, Singh H. Natural history of congenital kyphosis and kyphoscoliosis: a study of one hundred and twelve patients. J Bone Joint Surg Am. 1999;81:1367–1383. doi: 10.2106/00004623-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 23.McMaster MJ, Singh H. The surgical management of congenital kyphosis and kyphoscoliosis. Spine. 2001;26(19):2146–2154. doi: 10.1097/00007632-200110010-00021. [DOI] [PubMed] [Google Scholar]
- 24.Molinari, Robert W. Sagittal plane decompensation. Curr Opin Orthop. 2005;16(3):148–151. doi: 10.1097/01.bco.0000159767.67807.a9. [DOI] [Google Scholar]
- 25.Murrey DB, Brigham CD, Kiebzak GM, Finger F, Chewning SJ. Transpedicular decompression and pedicle subtraction osteotomy (eggshell procedure): a retrospective review of 59 patients. Spine. 2002;27(21):2338–2345. doi: 10.1097/00007632-200211010-00006. [DOI] [PubMed] [Google Scholar]
- 26.Nasca RJ, Stilling FH, 3rd, Stell HH. Progression of congenital scoliosis due to hemivertebrae and hemivertebrae with bars. J Bone Joint Surg Am. 1975;57:456–466. [PubMed] [Google Scholar]
- 27.Qi X, Matsumoto M, Ishii K, Nakamura M, Chiba K, Toyama Y. Posterior osteotomy and instrumentation for thoracolumbar kyphosis in patients with achondroplasia. Spine. 2006;31(17):E606–E610. doi: 10.1097/01.brs.0000229262.87720.9b. [DOI] [PubMed] [Google Scholar]
- 28.Suk KS, Kim KT, Lee SH, Kim JM. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine. 2003;28(17):2001–2005. doi: 10.1097/01.BRS.0000083239.06023.78. [DOI] [PubMed] [Google Scholar]
- 29.Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005;30(14):1682–1687. doi: 10.1097/01.brs.0000170590.21071.c1. [DOI] [PubMed] [Google Scholar]
- 30.Suk SI, Chung ER, Lee SM, Lee JH, Kim SS, Kim JH. Posterior vertebral column resection in fixed lumbosacral deformity. Spine. 2005;30(23):E703–E710. doi: 10.1097/01.brs.0000188190.90034.be. [DOI] [PubMed] [Google Scholar]
- 31.Suk SI, Kim JH, Kim WJ, et al. Posterior vertebral column resection for severe spinal deformities. Spine. 2002;27:2374–2382. doi: 10.1097/00007632-200211010-00012. [DOI] [PubMed] [Google Scholar]
- 32.Thompson AG, Marks DS, Sayampanathan SR. Long-term results of combined anterior and posterior convex epiphysiodesis for congenital scoliosis due to hemivertebrae. Spine. 1995;20:1380–1385. doi: 10.1097/00007632-199506000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Loon PJ, Stralen G, Loon CJ, Susante JL. A pedicle subtraction osteotomy as an adjunctive tool in the surgical treatment of a rigid thoracolumbar hyperkyphosis; a preliminary report. Spine J. 2006;6(2):195–200. doi: 10.1016/j.spinee.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 34.Royen BJ, Kastelijns RC, Noske DP, Oner FC, Smit TH. Transpedicular wedge resection osteotomy for the treatment of a kyphotic Andersson lesion-complicating ankylosing spondylitis. Eur Spine J. 2006;15(2):246–252. doi: 10.1007/s00586-005-1008-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walhout RJ, Rhijn LW, Pruijs JE. Hemi-epiphysiodesis for unclassified congenital scoliosis: immediate results and mid-term follow-up. Eur Spine J. 2002;11:543–549. doi: 10.1007/s00586-002-0395-9. [DOI] [PubMed] [Google Scholar]
- 36.Winter RB, Moe JH, Eilers VE. Congenital scoliosis: a study of 234 patients treated and untreated. J Bone Joint Surg Am. 1968;50:1–47. [Google Scholar]
- 37.Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5(1):9–17. doi: 10.3171/spi.2006.5.1.9. [DOI] [PubMed] [Google Scholar]
- 38.Yang BP, Ondra SL. A method for calculating the exact angle required during pedicle subtraction osteotomy for fixed sagittal deformity: comparison with the trigonometric method. Neurosurgery. 2006;59(4 suppl 2):458–463. doi: 10.1227/01.NEU.0000232628.46247.15. [DOI] [PubMed] [Google Scholar]