Abstract
Leptospirosis is a zoonotic spirochetal disease of global importance. This disease continues to have a major impact on people living in urban and rural areas of developing countries with inestimable morbidity and mortality. Funding for research and control efforts is currently haphazard, not organized and not effective for public health efforts, primarily because there are no concerted, ongoing international efforts to assess the impact of leptospirosis on human health. Major issues in the field need to be addressed to develop strategies of control, amelioration and treatment. These include the following: mechanisms of naturally acquired and vaccine-induced protective immunity against clinical leptospirosis; mechanisms of severe leptospirosis pathogenesis; standardized, precise and simplified taxonomy of Leptospira relevant to disease manifestations, transmission and control; effective adjunct treatments in addition to antimicrobials; and environmental assessment for risk of leptospirosis transmission and relevant mammalian reservoirs. Once effective ongoing, collaborative international efforts to assess the impact of leptospirosis on human and veterinary health are underway, appropriate mobilization of clinical and public health research funding will follow.
Keywords: Epidemiology, Disease burden, Vaccine, Taxonomy, Pathogenesis
Awareness has increased internationally over the past decade that leptospirosis is a major globally important public health threat, both in developing countries and industrialized countries.[1] The economic burden imposed by this disease is unknown, yet it is widely recognized that the incidence of leptospirosis is remarkably underestimated and the disease underdiagnosed in endemic regions. Leptospirosis is estimated to affect tens of millions of humans annually with case fatality rates ranging from 5 to 25%.[2] Case finding and reporting have been limited, nonsustained and biased. Domestic veterinary loss is substantial but the burden unknown. More precise and systematic assessment of the impact of leptospirosis on humans, as well as on animals of economic importance, is critical for assuring the proper international support and priority for research in this disease. The goal of this article is to emphasize major issues in leptospirosis research that need to be addressed so that priority areas can move forward with adequate support.
Currently available data suggest that leptospirosis is the most common zoonosis worldwide. Although the disease is endemic in rural areas around the world, transmission continues in developed countries as well, for example in the US (especially tropical Hawaii[3,4] but also inner cities),[5,6] Ireland[7] and Germany.[8] Annual incidence reports of leptospirosis vary from 0.53 per 100 000 population in tropical areas to 0.04 per 100 000 population in developed countries such as Germany.[2,8]
The leptospirosis aphorism: wherever leptospirosis is looked for, it is found
Leptospirosis is underreported due to lack of clinical suspicion and barriers to diagnostic capacity. General physicians often lack familiarity with the broad clinical presentation of leptospirosis. Most commonly, human infection with pathogenic Leptospira results in asymptomatic seroconversion.[9] Less commonly, leptospiral infection of humans results in symptomatic illness. When symptomatic, leptospirosis most often manifests as an undifferentiated febrile illness. Less commonly – in perhaps fewer than 5–10% of infections – severe disease results, which is manifested by any combination of jaundice, renal failure, hemorrhage, refractory shock, and myocarditis.[1] Major syndromes such as leptospirosis pulmonary hemorrhagic disease may appear in the absence of jaundice in areas of high prevalence of the disease, such as the Andaman Islands (as discovered in the seminal and now classic descriptions of leptospirosis as the cause of Andaman Hemorrhagic Fever by the group of Sehgal),[10–12] rural Nicaragua[13] or the Peruvian Amazon.[14,15] In the case of the Nicaragua epidemic, diagnosis was delayed due to confusion with other potential causes of epidemic febrile illness such as dengue and other viral hemorrhagic fever syndromes.[16] In urban epidemics that have occurred in some places such as Salvador, Brazil,[17] Weil’s disease as manifested by jaundice and renal failure has not necessarily been associated with pulmonary hemorrhage,[17] although more recently, for unexplained reasons, pulmonary hemorrhage has emerged as an important clinical syndrome (AI Ko, personal communication). Numerous serosurveys and hospital-based case finding studies have been carried out,[3,8,11,14,18–28] reinforcing time and again that leptospirosis transmission is incredibly common yet poorly recognized.
Environmental assessment to assess leptospirosis risk
A better understanding of the epidemiologic determinants of leptospirosis is needed to better determine appropriate public health approaches to ameliorate leptospirosis transmission. Animal reservoirs of leptospirosis may be domestic livestock, peridomestic rats and mice, companion animals particularly dogs and potentially wild animals such as bats,[29,30] marsupials and a large variety of rodents.[29]
The zoonotic sources of infection vary in different regions. Leptospirosis has traditionally been considered mainly a disease of farmers. In places where cattle and pigs are raised, these animals are often chronically colonized by pathogenic Leptospira with frequent transmission to humans. Over the past decade, there is increased recognition that additional risk groups include urban dwellers[5,17] and adventure travelers. The outbreak of leptospirosis associated with the EcoChallenge in Borneo was seen worldwide in athletes returning to their home countries.[31] However, of high public health importance, the urban environment is an important place where transmission of severe leptospirosis takes place. In such places, rats likely predominate as the zoonotic source of epidemic disease in urban environments such as Salvador, Brazil[17] or Baltimore[5] and Detroit[6,32] in the US. Dogs must be considered as important sources of urban transmission, which may be transmitted from vaccinated[33] or dogs wandering in the community. In some regions, canine leptospirosis is considered an emerging infectious disease of veterinary and potentially zoonotic importance. Dogs have increasingly been noted to be infected by serovars not included in the commercially available vaccines, particularly serovar Grippotyphosa; raccoons are thought to be the source of infection.[34]
In endemic areas of leptospirosis, factors such as lack of sanitary conditions, mud flooring, together with rainy seasons and flooding catastrophes contribute to periodic outbreaks.[35,36] Interestingly, in this setting, many exposed people have asymptomatic seroconversion and some also undiagnosed fever; a small but important minority may develop severe disease. In Hawaii, a tropical region of the US where leptospirosis is common and is a major public health concern [Figure 1], the zoonotic sources of leptospirosis transmission have not been precisely identified. The hazard of fresh water exposure for leptospirosis causes substantial alarm among tourists and local inhabitants, but as yet, there is no way to assess the true risk of infection for people there. In developing countries where proper sanitation is not maintained such as in favelas in Brazil or market and living areas of urban slums in the Peruvian Amazon, surface waters must be considered as representing substantial risk of leptospirosis transmission.
Figure 1.
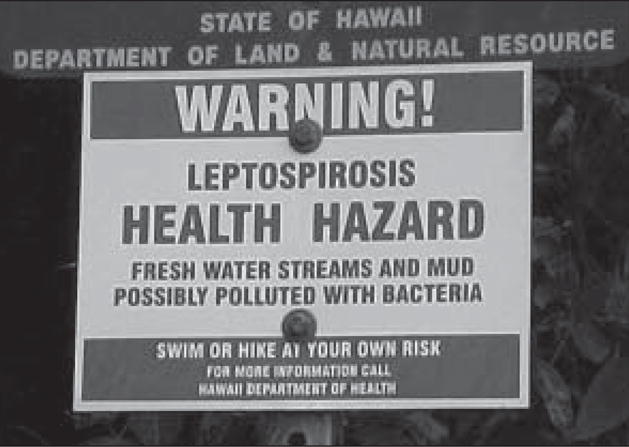
Warning sign in Hawaii, US about the risk of environmental exposure to leptospirosis
Quantifying the presence and determining types of pathogenic Leptospira in environmental surface waters would be an important tool for guiding leptospirosis control efforts in endemic regions, such as an outbreak that occurred in 2004 in a new village, Los Delfines, in the Peruvian Amazon region of Iquitos [Figure 2]. Such an approach would also have economic implications. For example, Hawaiian tourism has been negatively affected by unremediated leptospiral contamination of environmental surface waters [Figure 1]. Outbreaks of leptospirosis among elite athletes has occurred due to contamination of fresh water competition sites.[31,37] Culture methods are insufficient to address this task since saprophytic leptospires and other microbes have confounded such attempts in the past. We have been using a pathogen-specific quantitative PCR-based assay combined with molecular taxonomy to determine the types and quantities of pathogenic Leptospira in urban and rural areas in the Peruvian Amazon. Preliminary results indicate that in this region, far higher concentrations of pathogenic Leptospira, including Leptospira interrogans are present in the urban slum areas compared to rural water sources, where Leptospira inadai and Leptospira santarosai predominate but in far lower concentrations (C Ganoza, D Collins-Richards, MA Matthias, JM Vinetz, manuscript submitted). This approach promises to make a major contribution to assessing human risk for acquiring leptospirosis in relationship to activities of daily living for residents of endemic areas.
Figure 2.
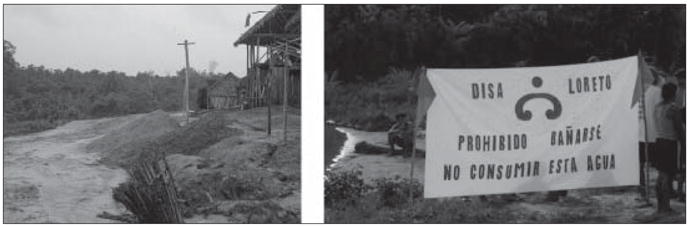
An outbreak of leptospirosis occurred in a swimming hole (left) at the edge of a newly developed village, Los Delfines, 10 km outside the city of Iquitos in the Peruvian Amazon. This outbreak resulted in the death of three children who had renal and respiratory failure, and cutaneous and gingival haemorrhage. Sixty-seven people sought medical attention for undiagnosed fever. Quantitative analysis of the creek running from the pig farm to the swimming hole showed that a new pig farm upstream of the village was the source of the outbreak. The Directorate of Public Health (DISA Loreto) placed a warning sign (right) at the swimming hole translated as ‘swimming prohibited. Do not drink this water’
What determines the severity of leptospiral infection? Host Vs infecting strain
Why do only some people develop any clinical manifestations of leptospirosis such as undifferentiated fever,[9] and of these, few (less than 5–10%) develop severe disease[13] despite being infected with highly pathogenic leptospires such as L. interrogans serovar Icterohaemorrhagiae?[3] The discrepancy between infection and symptomatic and severe disease remains a central mystery. Possible explanations (summarized in Table 1) include considerations of both the pathogen and the human host. It has long been thought that certain leptospiral serovars are particularly pathogenic. For example, serovars Copenhageni and Lai, whose whole genome sequences have been determined have been associated with severe human leptospirosis. These serovars do not cause disease in their natural mammalian reservoirs (Rattus spp. and Apodemus mice, respectively) but cause severe disease in experimental models of infection such as in hamsters or guinea pigs or in accidental hosts such as dogs. In fact most people infected with these serovars probably do not develop severe disease, possible no disease at all. Serosurveys in urban areas of Brazil where serovar Copenhageni predominates as a single clonal subpopulation[38] show that many people with anti-Copenhageni antibodies never had severe leptospirosis.[28] Conversely, a wide variety of Leptospira have been shown to cause severe disease, including the ‘intermediate’ leptospire, Leptospira fainei serovar Hurstbridge,[39] even though, again, most infections are probably inapparent.[40] Therefore, intrinsic virulence properties of pathogenic or intermediate Leptospira cannot be the sole explanation of severe human disease.
Table 1.
Possible determinants of leptospirosis severity
| Virulence properties of infecting Leptospira |
| Infectious inoculum at time of exposure |
| Preexisting immunity due to previous exposure |
| Hormonal influences (men more commonly develop severe disease) |
| Human host genetics: acquired or innate immunity |
| Nutritional factors: malnutrition, alcohol consumption |
Alternatively, human host genetics are likely to determine clinical outcomes of leptospiral infection. One report suggests the association of a major histocompatibility complex allele, HLA-DQ6, with risk of infection due to ingestion of Leptospira-contaminated water in an outbreak of leptospirosis in the US.[41] However, no investigations have been reported of human genetic susceptibility to severe leptospirosis. A major contribution to understanding the role of human immune factors in intrinsic resistance to the effects of pathogenic Leptospira would be to develop an international multi-center, prospective study of well defined cohorts to create a specimen bank consisting of isolates, serum, and patient DNA samples. The recent publication of two leptospiral whole genome sequences[42,43] and recent advances in systems biology would facilitate microarray and proteomic analysis of leptospiral[44–46] and human host determinants of disease susceptibility and clinical manifestations.
Another potential determinant of leptospirosis severity could include the dose of Leptospira inoculated during environmental exposure. Such an explanation can now be addressed with the quantitative molecular methods for assessing leptospiral contamination of environmental surface waters.
Acquired and innate immunity to leptospira in endemic regions
Humans living in leptospirosis-endemic regions are commonly exposed to Leptospira during their activities of daily living. Therefore, it is likely that some people living in leptospirosis-endemic regions develop naturally acquired protective immunity against severe disease. What are the mechanisms of such protective immunity in humans? Serovar-specific antibodies targeted against lipopolysaccharide or antibodies against cross-species conserved proteins such as LipL32 or others?[46] Does acquired cellular immunity with either T cells with ab T cell receptors or T cells with gd T cell receptors playing an important role.[47–49] Are naturally acquired protective immune mechanisms long- or short-lived since protective immunity induced by bacterins (killed whole cell vaccines) are short-lived? What in vitro tests or small animal models can be developed to assess naturally acquired protective immunity in humans? Do such responses affect disease pathogenesis? Can naturally acquired immunity be used to guide vaccine development for humans?
Some of the reasons may relate to transmission intensity and pre-existing population immunity, virulence of circulating leptospiral serovars and/or host immunogenetic factors. Data are limited regarding the exact contribution of each of these variables. It seems intuitive that pre-existing immunity due to previous exposure protects against subsequent infection. However, no published data either support or refute this concept. Of note, anti-leptospiral antibodies, as detected by the microscopic agglutination test, can be short-lived (in the order of months), or May last years. It is also possible that pre-existing immunity may influence the severity of a subsequent leptospiral infection. No evidence suggests that an immune sensitization phenomenon predisposes to severe leptospirosis as occurs in dengue virus infection, where a second infection with a different dengue virus serotype increases the risk for dengue haemorrhagic fever. Future prospective studies are needed to address the central issues of the role of acquired and innate immunity in protection from leptospirosis. Such studies would include establishing cohort studies in endemic areas in which risk for symptomatic leptospirosis during primary Vs subsequent exposure is quantified. Being able to precisely determine the infecting leptospiral strain would be essential to such studies. To determine whether human protective immunity develops in exposed population requires the development of experimental methods (in vitro or small animal) to determined correlates of acquired and innate protective immunity against leptospirosis in humans.
Identification of leptospiral isolates
A common problem in leptospirosis is how to identify infecting Leptospira isolated from clinical specimens, from animals, and from environmental sources. Leptospira are conventionally classified phenotypically by a cumbersome and outdated serologically based scheme with expensive polyclonal and monoclonal antibody reagents and reference strains available only from reference laboratories. The gold standard serological classification, the cross agglutination absorption test (CAAT) is labour-intensive, requires a large panel of live leptospires, takes months to complete and, being phenotypic, does not reflect genetic relatedness. The most comprehensive classification scheme is based on DNA relatedness among members of the family Leptospiraceae,[50] a technique not available outside of reference centers. Many molecular methods have been applied to the characterization of leptospiral isolates, including restriction enzyme analysis, pulse field gel electrophoresis, random amplified polymorphic DNA analysis and arbitrarily primed PCR fingerprinting.[51,52] 16S ribosomal RNA gene sequence analysis can distinguish leptospiral species[53,54] but whether it has sufficient discriminatory power to distinguish among strains (i.e. serovars) within a species has not been shown.
A major priority of international collaborative research efforts should be to create a comprehensive Leptospira database curated by an expert group. This database should contain reference information for all known Leptospira. A comprehensive entry for a leptospiral isolate might include:date of isolation, source (human, animal or water source), clinical outcome of patient (if applicable), region, serological typing CAAT, monoclonal antibody, DNA-DNA hybridization, PFGE, RAPD, and AP-PCR patterns (under standardized conditions), 16S ribosomal RNA gene sequence. This database should be accessible using appropriate informatics tools through an Internet browser interface. The service should be provided gratis and be timely. The goal should be to provide a resource for the rapid identification of infecting leptospires for clinical, epidemiologic and basic research purposes.
Conclusion
Recent worldwide progress in leptospirosis compels increased international attention towards addressing its role in clinical and public health. Organizations such as the International Leptospirosis Society should be the focal point for developing international co-operative efforts. Agencies such as the World Health Organization, the Food and Agricultural Organization, the Pan American Health Organization, the US National Institutes of Health and the European Union should be approached for sustained support to address some of the following central problems of international importance:
Development of an international registry of cases with an estimate of incidence and prevalence, to provide policy guidance to public health authorities.
Creation of regional and national networks of leptospirosis diagnostic laboratories with appropriate quality assurance controls.
The establishment of central repositories of leptospiral strains, hybridomas, reference polyclonal antisera and monoclonal antibodies, available at nominal cost to qualified laboratories.
Creation of an international, internet-queriable comprehensive Leptospiral database.
Development of an international, multi-center, prospective cohort study of the human, leptospiral virulence factors, and environmental determinants of leptospirosis clinical manifestations and clinical outcome. This would involve creation of a specimen bank from well-characterized leptospirosis patients and environmental and zoonotic sources to include: leptospiral isolates; clinical samples of blood and urine for molecular identification of leptospires and evaluation of new diagnostic tests; patient DNA samples for determining genetic associations with different outcomes of leptospiral infection; and environmental water samples from endemic and epidemic regions accompanied by GPS and geographic data to determine risk of transmission and infection.
Acknowledgments
This work was supported by US Public Health Service grants KO2AI50049, RO1TW05860, R01 AI053422, and D43TW007120.
References
- 1.Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, et al. Leptospirosis:A zoonotic disease of global importance. Lancet Infect Dis. 2003;3:757–71. doi: 10.1016/s1473-3099(03)00830-2. [DOI] [PubMed] [Google Scholar]
- 2.Smythe LD. Leptospirosis worldwide, 1999. Wkly Epidemiol Rec. 2001;76:109–16. [Google Scholar]
- 3.Sasaki DM, Pang L, Minette HP, Wakida CK. Active surveillance and risk factors for leptospirosis in Hawaii. Am J Trop Med Hyg. 1993;48:35–43. doi: 10.4269/ajtmh.1993.48.35. [DOI] [PubMed] [Google Scholar]
- 4.Katz AR, Effler PV. “Probable” versus “Confirmed” leptospirosis” An epidemiologic and clinical comparison utilizing a surveillance case classification. Ann Epidemiol. 2003;13:196–203. doi: 10.1016/s1047-2797(02)00275-2. [DOI] [PubMed] [Google Scholar]
- 5.Vinetz JM, Glass GE, Flexner CE, Mueller P, Kaslow DC. Sporadic urban leptospirosis. Ann Intern Med. 1996;125:794–8. doi: 10.7326/0003-4819-125-10-199611150-00002. [DOI] [PubMed] [Google Scholar]
- 6.Thiermann AB, Frank RR. Human leptospirosis in Detroit and the role of rats as chronic carriers. Int J Zoonoses. 1980;7:62–72. [PubMed] [Google Scholar]
- 7.Pate GE, Hogan MC, FitzSimon N, Mellotte GJ. A review of the epidemiology of leptospirosis in the Republic of Ireland. Ir Med J. 2000;93:114–7. [PubMed] [Google Scholar]
- 8.Jansen A, Schneberg I, Frank C, Alpers K, Schneider T, Stark K. Leptospirosis in Germany, 1962–2003. Emerging Infect Dis. 2005;11:1048–54. doi: 10.3201/eid1107.041172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashford DA, Kaiser RM, Spiegel RA, Perkins BA, Weyant RS, Bragg SL, et al. Asymptomatic infection and risk factors for leptospirosis in Nicaragua. Am J Trop Med Hyg. 2000;63:249–54. [PubMed] [Google Scholar]
- 10.Sehgal SC, Murhekar MV, Sugunan AP. Outbreak of leptospirosis with pulmonary involvement in north Andaman. Indian J Med Res. 1995;102:9–12. [PubMed] [Google Scholar]
- 11.Sehgal SC, Vijayachari P, Murhekar MV, Sugunan AP, Sharma S, Singh SS. Leptospiral infection among primitive tribes of Andaman and Nicobar Islands. Epidemiol Infect. 1999;122:423–8. doi: 10.1017/s0950268899002435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sehgal SC, Vijayachari P, Smythe LD, Norris M, Symonds M, Dohnt M, et al. Lai-like leptospira from the Andaman Islands. Indian J Med Res. 2000;112:135–9. [PubMed] [Google Scholar]
- 13.Trevejo RT, Rigau-Perez JG, Ashford DA, McClure EM, Jarquin-Gonzalez C, Amador JJ, et al. Epidemic leptospirosis associated with pulmonary hemorrhage-Nicaragua, 1995. J Infect Dis. 1998;178:1457–63. doi: 10.1086/314424. [DOI] [PubMed] [Google Scholar]
- 14.Johnson MA, Smith H, Joseph P, Gilman RH, Bautista CT, Campos KJ, et al. Environmental exposure and leptospirosis, Peru. Emerg Infect Dis. 2004;10:1016–22. doi: 10.3201/eid1006.030660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Segura E, Ganoza C, Campos K, Ricaldi JN, Torres S, Silva H, et al. Clinical Spectrum of Pulmonary Involvement in Leptospirosis in an Endemic Region, with Quantification of Leptospiral Burden. Clin Infect Dis. 2005;40:343–51. doi: 10.1086/427110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zaki SR, Shieh WJ. Leptospirosis associated with outbreak of acute febrile illnesses and pulmonary haemorrhage, Nicaragua, 1995. Lancet. 1996;347:535–6. doi: 10.1016/s0140-6736(96)91167-8. [DOI] [PubMed] [Google Scholar]
- 17.Ko AI, Galvao RM, Ribeiro DC, Johnson WD, Jr, Riley LW. Urban epidemic of severe leptospirosis in Brazil. Salvador Leptospirosis Study Group. Lancet. 1999;354:820–5. doi: 10.1016/s0140-6736(99)80012-9. [DOI] [PubMed] [Google Scholar]
- 18.Everard CO, Hayes RJ, Fraser-Chanpong GM. A serosurvey for leptospirosis in Trinidad among urban and rural dwellers and persons occupationally at risk. Trans R Soc Trop Med Hyg. 1985;79:96–105. doi: 10.1016/0035-9203(85)90246-9. [DOI] [PubMed] [Google Scholar]
- 19.Childs JE, Schwartz BS, Ksiazek TG, Graham RR, LeDuc JW, Glass GE. Risk factors associated with antibodies to leptospires in inner-city residents of Baltimore:a protective role for cats. Am J Public Health. 1992;82:597–9. doi: 10.2105/ajph.82.4.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vijayachari V, Sugunan AP, Murhekar MV, Sharma S, Sehgal SC. Leptospirosis among schoolchildren of the Andaman & Nicobar Islands, India: Low levels of morbidity and mortality among pre-exposed children during an epidemic. Epidemiol Infect. 2004;132:1115–20. doi: 10.1017/s0950268804002948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yersin C, Bovet P, Merien F, Wong T, Panowsky J, Perolat P. Human leptospirosis in the Seychelles (Indian Ocean):a population-based study. Am J Trop Med Hyg. 1998;59:933–40. doi: 10.4269/ajtmh.1998.59.933. [DOI] [PubMed] [Google Scholar]
- 22.Kuriakose M, Eapen CK, Paul R. Leptospirosis in Kolenchery, Kerala, India:epidemiology, prevalent local serogroups and serovars and a new serovar. Eur J Epidemiol. 1997;13:691–7. doi: 10.1023/a:1007300729615. [DOI] [PubMed] [Google Scholar]
- 23.Sethi S, Sood A, Pooja Sharma S, Sengupta C, Sharma M. Leptospirosis in northern India:a clinical and serological study. Southeast Asian J Trop Med Public Health. 2003;34:822–5. [PubMed] [Google Scholar]
- 24.Cacciapuoti B, Ciceroni L, Pinto A, Apollini M. Survey on the prevalence of Leptospira infections in the Italian population. Eur J Epidemiol. 1994;10:173–80. doi: 10.1007/BF01730367. [DOI] [PubMed] [Google Scholar]
- 25.Everard CO, Edwards CN, Everard JD, Carrington DG. A twelve-year study of leptospirosis on Barbados. Eur J Epidemiol. 1995;11:311–20. doi: 10.1007/BF01719436. [DOI] [PubMed] [Google Scholar]
- 26.Lecour H, Miranda M, Magro C, Rocha A, Goncalves V. Human leptospirosis - a Review of 50 cases. Infection. 1989:17. doi: 10.1007/BF01643489. [DOI] [PubMed] [Google Scholar]
- 27.Perolat P, Reeve PA. First evidence of leptospirosis in Vanuatu. Trans Roy Soc Trop Med Hyg. 1992;86:557–9. doi: 10.1016/0035-9203(92)90111-o. [DOI] [PubMed] [Google Scholar]
- 28.Romero EC, Bernardo CC, Yasuda PH. Human leptospirosis: A twenty-nine-year serological study in Sao Paulo, Brazil. Rev Inst Med Trop S Paulo. 2003;45:245–8. doi: 10.1590/s0036-46652003000500002. [DOI] [PubMed] [Google Scholar]
- 29.Bunnell JE, Hice CL, Watts DM, Montrueil V, Tesh RB, Vinetz JM. Detection of pathogenic Leptospira spp. infections among mammals captured in the Peruvian Amazon basin region. Am J Trop Med Hyg. 2000;63:255–8. [PubMed] [Google Scholar]
- 30.Matthias MA, Diaz MM, Campos KJ, Calderon M, Willig MR, Pacheco V, et al. Diversity of bat-associated Leptospira in the Peruvian Amazon inferred by Bayesian phylogenetic analysis of 16S ribosomal DNA sequences. Am J Trop Med Hyg. 2005 [PMC free article] [PubMed] [Google Scholar]
- 31.Sejvar J, Bancroft E, Winthrop K, Bettinger J, Bajani M, Bragg S, et al. Leptospirosis in Eco-Challenge Athletes, Malaysian Borneo, 2000. Emerg Infect Dis. 2003;9:702–7. doi: 10.3201/eid0906.020751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thiermann AB. Incidence of leptospirosis in the Detroit rat population. Am J Trop Med Hyg. 1977;26:970–4. doi: 10.4269/ajtmh.1977.26.970. [DOI] [PubMed] [Google Scholar]
- 33.Thiermann AB. Canine leptospirosis in Detroit. Am J Vet Res. 1980;41:1659–61. [PubMed] [Google Scholar]
- 34.Ward MP, Guptill LF, Prahl A, Wu CC. Serovar-specific prevalence and risk factors for leptospirosis among dogs:90 cases (1997–2002) J Am Vet Med Assoc. 2004;224:1958–63. doi: 10.2460/javma.2004.224.1958. [DOI] [PubMed] [Google Scholar]
- 35.Kupek E, de Sousa Santos Faversani MC, de Souza Philippi JM. The relationship between rainfall and human leptospirosis in Florianopolis, Brazil, 1991–1996. Br J Infect Dis. 2000;4:131–4. [PubMed] [Google Scholar]
- 36.Bharadwaj R, Bal AM, Joshi SA, Kagal A, Pol SS, Garad G, et al. An urban outbreak of leptospirosis in Mumbai, India. Jpn J Infect Dis. 2002;55:194–6. [PubMed] [Google Scholar]
- 37.Morgan J, Bornstein SL, Karpati AM, Bruce M, Bolin CA, Austin CC, et al. Outbreak of leptospirosis among triathlon participants and community residents in Springfield, Illinois, 1998. Clin Infect Dis. 2002;34:1593–9. doi: 10.1086/340615. [DOI] [PubMed] [Google Scholar]
- 38.Pereira MM, Matsuo MG, Bauab AR, Vasconcelos SA, Moraes ZM, Baranton G, et al. A clonal subpopulation of Leptospira interrogans sensu stricto is the major cause of leptospirosis outbreaks in Brazil. J Clin Microbiol. 2000;38:450–2. doi: 10.1128/jcm.38.1.450-452.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petersen AM, Boye K, Blom J, Schlichting P, Krogfelt KA. First isolation of Leptospira fainei serovar Hurstbridge from two human patients with Weil’s syndrome. J Med Microbiol. 2001;50:96–100. doi: 10.1099/0022-1317-50-1-96. [DOI] [PubMed] [Google Scholar]
- 40.Chappel RJ, Khalik DA, Adler B, Bulach DM, Faine S, Perolat P, et al. Serological titres to Leptospira fainei serovar hurstbridge in human sera in Australia. Epidemiol Infect. 1998;121:473–5. doi: 10.1017/s095026889800137x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lingappa J, Kuffner T, Tappero J, Whitworth W, Mize A, Kaiser R, et al. HLA-DQ6 and ingestion of contaminated water:possible gene-environment interaction in an outbreak of leptospirosis. Genes Immun. 2004;5:197–202. doi: 10.1038/sj.gene.6364058. [DOI] [PubMed] [Google Scholar]
- 42.Nascimento AL, Ko AI, Martins EA, Monteiro-Vitorello CB, Ho PL, Haake DA, et al. Comparative genomics of two Leptospira interrogans serovars reveals novel insights into physiology and pathogenesis. J Bacteriol. 2004;186:2164–72. doi: 10.1128/JB.186.7.2164-2172.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ren SX, Fu G, Jiang XG, Zeng R, Miao YG, Xu H, et al. Unique physiological and pathogenic features of Leptospira interrogans revealed by whole-genome sequencing. Nature. 2003;422:888–93. doi: 10.1038/nature01597. [DOI] [PubMed] [Google Scholar]
- 44.Cullen PA, Cordwell SJ, Bulach DM, Haake DA, Adler B. Global analysis of outer membrane proteins from Leptospira interrogans serovar Lai. Infect Immun. 2002;70:2311–8. doi: 10.1128/IAI.70.5.2311-2318.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nally JE, Whitelegge JP, Aguilera R, Pereira MM, Blanco DR, Lovett MA. Purification and proteomic analysis of outer membrane vesicles from a clinical isolate of Leptospira interrogans serovar Copenhageni. Proteomics. 2005;5:144–52. doi: 10.1002/pmic.200400880. [DOI] [PubMed] [Google Scholar]
- 46.Cullen PA, Xu X, Matsunaga J, Sanchez Y, Ko AI, Haake DA, et al. Surfaceome of Leptospira spp. Infect Immun. 2005;73:4853–63. doi: 10.1128/IAI.73.8.4853-4863.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Naiman BM, Alt D, Bolin CA, Zuerner R, Baldwin CL. Protective killed Leptospira borgpetersenii vaccine induces potent Th1 immunity comprising responses by CD4 and gamma/delta T lymphocytes. Infect Immun. 2001;69:7550–8. doi: 10.1128/IAI.69.12.7550-7558.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naiman BM, Blumerman S, Alt D, Bolin CA, Brown R, Zuerner R, et al. Evaluation of type 1 immune response in naive and vaccinated animals following challenge with Leptospira borgpetersenii serovar Hardjo:involvement of WC1(+) gammadelta and CD4 T cells. Infect Immun. 2002;70:6147–57. doi: 10.1128/IAI.70.11.6147-6157.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Klimpel GR, Matthias MA, Vinetz JM. Leptospira interrogans activation of human peripheral blood mononuclear cells:Preferential expansion of TCRgd+ T cells versus TCRab+ T cells. J Immunol. 2003;171:1447–55. doi: 10.4049/jimmunol.171.3.1447. [DOI] [PubMed] [Google Scholar]
- 50.Brenner DJ, Kaufmann AF, Sulzer KR, Steigerwalt AG, Rogers FC, Weyant RS. Further determination of DNA relatedness between serogroups and serovars in the family Leptospiraceae with a proposal for Leptospira alexanderi sp. nov. and four new Leptospira genomospecies. Int J Syst Bacteriol. 1999;49:839–58. doi: 10.1099/00207713-49-2-839. [DOI] [PubMed] [Google Scholar]
- 51.Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14:296–326. doi: 10.1128/CMR.14.2.296-326.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roy S, Biswas D, Vijayachari P, Sugunan AP, Sehgal SC. A 22-mer primer enhances discriminatory power of AP-PCR fingerprinting technique in characterization of leptospires. Trop Med Int Health. 2004;9:1203–9. doi: 10.1111/j.1365-3156.2004.01322.x. [DOI] [PubMed] [Google Scholar]
- 53.Hookey JV, Bryden J, Gatehouse L. The use of 16S rDNA sequence analysis to investigate the phylogeny of Leptospiraceae and related spirochaetes. J Gen Microbiol. 1993;139:2585–90. doi: 10.1099/00221287-139-11-2585. [DOI] [PubMed] [Google Scholar]
- 54.Levett PN, Morey RE, Galloway R, Steigerwalt AG, Ellis WA. Reclassification of Leptospira parva Hovind-Hougen et al. 1982 as Turneriella parva gen. nov., comb. nov. Int J Syst Evol Microbiol. 2005;55:1497–9. doi: 10.1099/ijs.0.63088-0. [DOI] [PubMed] [Google Scholar]


