Abstract
The aim of this pilot study was to compare the effects of an intensive nutritional intervention with usual care conditions on dropout rate, body weight, lifestyle changes and glycemic control in patients with type 2 diabetes mellitus (T2DM). Thirty outpatients with T2DM but without insulin treatment (mean age: 57 ± 9 yr) were randomly assigned to one of the two intervention groups: intensive care (IC) or usual care (UC). Patients in the UC group were given advice about dietary and physical activity goals in one consultation session at baseline, while patients in the IC group attended five goal-oriented consultation sessions held approximately every two weeks from baseline onwards. Changes in body weight, T2DM knowledge, dietary intake, physical activity, HbA1c, and percentage of dropouts were evaluated at 1-year follow-up post-intervention. Fifty percent of patients quitted the program and were classified as "dropouts". Program completers were older and included a lower percentage of newly diagnosed T2DM compared with dropouts. A tendency to a negative association between attendance of the IC group and the likelihood of dropping out was found (p = 0.08). No difference was detected between UC and IC groups regarding changes in body weight, HbA1c or other outcome measures, at post-intervention or 1-year follow-up. This pilot study did not confirm advantages of intensive nutritional intervention in T2DM patients in terms of glycemic control, body weight, diet and physical activity. However, the high dropout rate may have hampered its effectiveness.
Keywords: type 2 diabetes, glycemic control, diet, dropout, non-attendance, lifestyle
Introduction
Nutritional intervention, as an integral part of diabetes management, aims to attain and maintain optimal metabolic outcomes, to prevent and treat medical complications, and to improve general health [1]. Although there are individual studies showing that medical nutrition therapy provided by dietitians improves glycemic control and lipid profile in diabetic patients [2-4], most systematic reviews yielded inconclusive findings regarding the effect of diet on type 2 diabetes mellitus (T2DM) [5]. This could be partly attributed to the low compliance and adherence rates to diet [6-8]. T2DM patients encounter several educational, environmental, psychological and lifestyle difficulties in modifying their lives to accommodate disease management [9, 10], and, in general, they appear to be more likely to cooperate with pharmaceutical management than with self-care behavior such as dietary modification [11]. Dietitians believe that provision of additional and more individualized education, as well as obtainable goals, could help patients to overcome the barriers [12]. From the patients' point of view, non-attendance at the meetings with the dietitian could be improved by the provision of more new information during consultation, better coordination of the appointment with other specialists, as well as dietary advice that is better tailored to meet personal needs [13].
Incorporating suggestions from both dietitians and patients for improving nutrition management at an outpatient clinic, we implemented an intensive nutritional intervention and examined its effectiveness, in terms of body weight changes and glycemic control, as well as its effect on the dropout rate. The results of the pilot study are presented here.
Methods
Subjects
Thirty T2DM patients (16 men and 14 women, mean age: 57 ± 9 yr), attending an outpatient clinic in a general public hospital, were randomly assigned to a usual care group (UC) or an intensive care group (IC). After being informed of the purpose and procedures of the study, all subjects signed a consent form. The study protocol was approved by the Harokopio University Ethics Committee.
Intervention
The aim of the intervention was to enable patients to make informed and reasonable changes with regard to their diet and physical activity, namely to increase their fruit and vegetable consumption to 5 portions per day, to consume 4-6 meals and snacks, to reduce their dietary intake of saturated fat, sweets and sugar-containing beverages and to increase their physical activity to 30 minutes at least 5 days/week. They were also informed about smoking risks and encouraged to stop or limit smoking.
In the UC (standard dietary care for patients with diabetes in the hospital), dietary and physical activity goals were discussed in one consultation session at baseline. Patients were re-evaluated on a monthly or bi-monthly basis, following their appointments at the outpatient clinic. People with diabetes in the IC attended five consultation sessions, scheduled approximately every two weeks, independent of their outpatient clinic appointment, for a 2-month period. The sessions were goal-oriented. A visual agenda setting chart was used [14] and patients were encouraged to identify their own priority goals with regards to diet and physical activity, as well as to make their own proposals for feasible changes in their lifestyle in order to attain and maintain their goals. A new goal was allocated in each session and previous goals were re-evaluated along with suggestions on the management of high-risk situations. Positive reinforcement was provided throughout the intervention. All consultations were conducted by two experienced clinical dietitians, who had received further appropriate training.
Clinical, nutritional and biochemical assessment
Information on the health status and prescription of antidiabetic medication of the participants was retrieved from medical records. Body weight, height and waist circumference were measured. Dietary intake was assessed using a modified version of a widely-used semi-quantitative food frequency questionnaire [15], including the main food groups of the Greek diet, namely dairy products, fruits, vegetables, cereals, potatoes, legumes, red meat, poultry, fish, sweets, alcoholic and non-alcoholic beverages. Physical activity was estimated through a brief self-reported questionnaire, which collects the previous week's physical activity [16]. Patients' knowledge about T2DM and lifestyle parameters was evaluated through a relevant questionnaire. Measurement of HbA1c was used to assess glycemic control. During intervention implementation, patients who wanted to quit the intervention at any stage or who did not appear in two or more consultations were classified as "dropouts" and the remaining patients as "completers". All the assessments were conducted at baseline, at post-intervention (or 2 months after baseline examination) and at 1-year follow-up.
Statistical analysis
The Kolmogorov-Smirnov test was used to test for the normality of distributions. Two-sample t tests and two-sample Mann-Whitney U tests were used where appropriate to compare continuous variables of interest between groups. Logistic regression analysis was performed with membership in the drop-out group as the outcome of interest. Because of the small sample size, the rank transform method has been used to evaluate differences between pre-intervention, post-intervention and follow-up values i.e. observations were replaced by their respective ranks and ranked repeated measures analysis of variance was performed (Friedman's test).
Results
No differences were found between the two groups in anthropometric, dietary and physical activity parameters at baseline (Table 1). IC patients had significantly higher HbA1c values, compared to those in UC (9.5 ± 1.6 vs. 7.6 ± 1.8%, p = 0.04), whereas 93% in the IC vs. 60% of the UC were on antidiabetic medication (p = 0.08).
Table 1. Clinical characteristics of study participants.
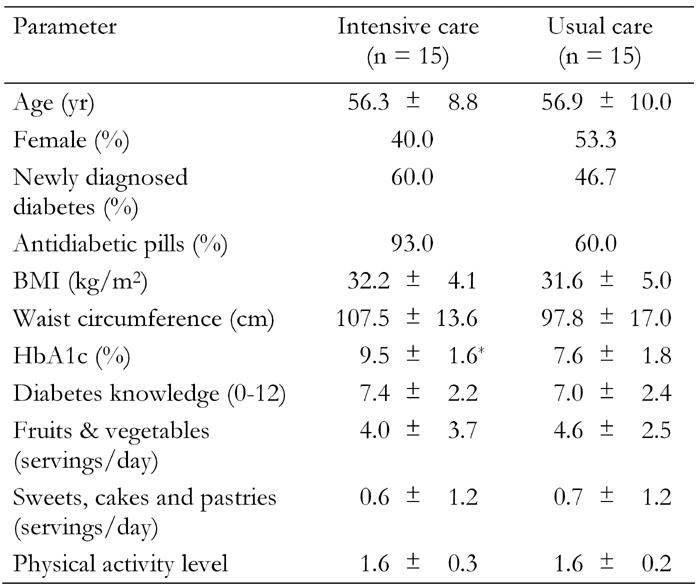
Data are mean ± SD. Diabetes knowledge and physical activity levels were determined using questionnaire with grading system. * Significant different from usual care (p = 0.04).
Fifty percent of patients were dropouts. Comparisons between completers and dropouts revealed no statistically significant differences between the two groups (with regards to history of diabetes, sex, HbA1c, BMI or waist circumference), apart from their age, with those not completing the intervention being younger compared to completers (53 ± 9 vs. 60 ± 9 yr, p = 0.05) (Table 2). A trend for an association between group and dropout was observed: 66.7% in the UC and 33.3% in the IC were dropouts (p = 0.07). To explore the effect of several factors in relation to the likelihood of being a dropout, a logistic regression was performed. Older people (p = 0.03) and those with newly diagnosed T2DM (p = 0.05) were more likely to complete the program, whereas a tendency for a negative association between attendance of the IC group and the likelihood of dropping out was found (p = 0.08).
Table 2. Baseline characteristics of study completers and dropouts.
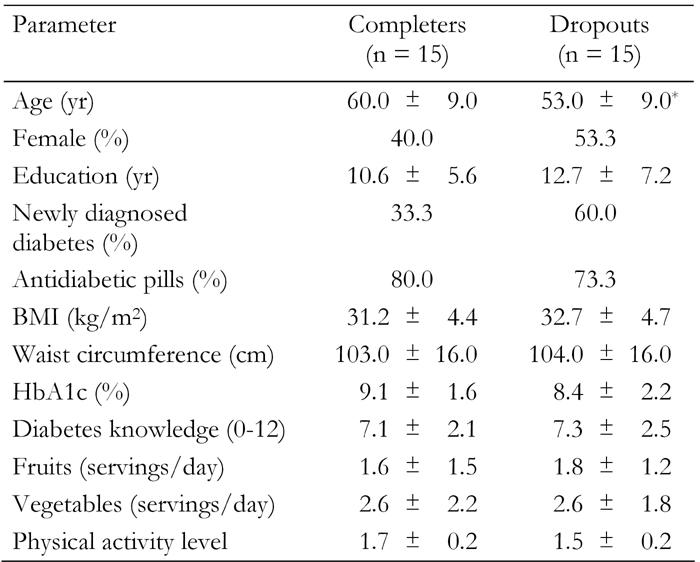
Data are mean ± SD. Diabetes knowledge and physical activity levels were determined using questionnaire with grading system. * Significant different from completers (p < 0.05).
Ranked repeated measures analysis of variance revealed no difference between UC and IC with regards to BMI, waist circumference, T2DM knowledge, HbA1c and intervention goals at different time points, either for the study completers (n = 15) (Table 3) or for patients available for measurement at 1-year follow-up (n = 19).
Table 3. Study outcomes for the completers at baseline, post-intervention and 1-year follow-up.
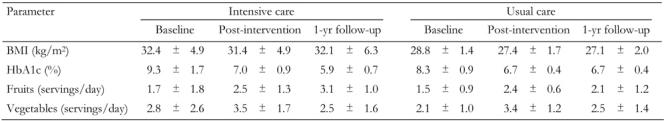
Data are mean ± SD.
Discussion
We hypothesized that an individualized, goal-oriented, intensive nutritional intervention, in terms of frequency of consultations, would improve patient-health professional relationships, challenge patients' perceptions and thus induce significant changes in the investigated outcomes. Our results did not support this hypothesis, as the implementation of this type of intervention did not bring about changes in glycemic control, body weight, and dietary or physical activity parameters. On the contrary, patients' nonattendance emerged as the major problem and as the limiting factor for the power of the study. A tendency towards a lower dropout rate was observed in the intensive program, where more time was devoted to patients and nutritional advice was more closely tailored to individual needs. However, other parameters, such as patients' age and being newly diagnosed for T2DM were found to be more important in explaining dropout.
The high non-attendance of T2DM patients to dietetic consultations has been of particular interest [13]. The 50% rate observed in the present study, although high, was within the range reported for diabetes outcome studies in the review by Norris et al. [17]. Attrition rate constituted an important problem for the validity of the effectiveness of self-management training in T2DM [17]. General health locus of glycemic and dietary control and feelings of obligation to keep the appointment with the dietician have been found to be the most important predictors of non-attendance, with a substantial proportion of patients perceiving their visit to the dietician to be of little usefulness [13]. Patients' motivation, defined as the probability that a person will enter into, continue and adhere to a specific change strategy [18], may, therefore, be important in reducing dropouts. Patients' readiness for change has also been recognized as one of the factors that set hurdles in the clinical setting [19]. Nutritional intervention should aim at both providing knowledge and motivating patients to increase their likelihood of following the recommended course of action. We speculate that a potential benefit from the application of the nutritional intervention and a lower dropout rate would have occurred, if a motivation component had been included in the intensive program.
Indeed, substantial improvements in HbA1c were found at 1-year follow-up after an educational intervention in patients with elevated HbA1c baseline levels, who were likely to be highly motivated and prepared to make a change in their diabetes management [20]. Furthermore, as it has been previously shown that the beneficial effect on glycemic control disappeared one year after the last session of a short-term individual education program that did not include a structured follow-up [21], regular reinforcements may be proven to be an essential component of the intervention in order to achieve sustained motivation. Nonetheless, although some previous studies have shown favorable effects of intensive intervention programs on cardiovascular risk factors in diabetic patients [22-24], a review of the use of behavioral therapies in the management of T2DM concluded that behavioral diet/exercise interventions are effective in inducing changes in metabolic outcome measures, but no patterns could be discerned in the available trials to suggest specific patient, provider, or intervention characteristics that would influence the effectiveness of behavioral therapies [25].
In conclusion, the present pilot study did not reveal any advantage from an intensive nutritional intervention in T2DM patients in terms of changes in glycemic control, body weight, dietary and physical activity habits. However, the high dropout rate observed may have hampered its effectiveness. Further explorative studies are needed to evaluate dropout characteristics, namely readiness to change, and to investigate the effect of including motivation techniques in a nutritional intervention for inducing significant improvements in nutritional and biological outcomes.
Acknowledgments
The authors would like to acknowledge Mr. Nikos Voutzourakis for his contribution during data collection.
References
- 1.Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer-Davis E, Mooradian AD et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25(1):148–198. doi: 10.2337/diacare.25.1.148. [DOI] [PubMed] [Google Scholar]
- 2.Wolf AM, Conaway MR, Crowther JQ, Hazen KY, J LN, Oneida B, Bovbjerg VE. Translating lifestyle intervention to practice in obese patients with type 2 diabetes: Improving Control with Activity and Nutrition (ICAN) study. Diabetes Care. 2004;27(7):1570–1576. doi: 10.2337/diacare.27.7.1570. [DOI] [PubMed] [Google Scholar]
- 3.Laitinen JH, Ahola IE, Sarkkinen ES, Winberg RL, Harmaakorpi-Iivonen PA, Uusitupa MI. Impact of intensified dietary therapy on energy and nutrient intakes and fatty acid composition of serum lipids in patients with recently diagnosed non-insulin-dependent diabetes mellitus. J Am Diet Assoc. 1993;93(3):276–283. doi: 10.1016/0002-8223(93)91552-2. [DOI] [PubMed] [Google Scholar]
- 4.Johnson EQ, Valera S. Medical nutrition therapy in non-insulin-dependent diabetes mellitus improves clinical outcome. J Am Diet Assoc. 1995;95(6):700–701. doi: 10.1016/S0002-8223(95)00192-1. [DOI] [PubMed] [Google Scholar]
- 5.van de Laar FA, Akkermans RP, van Binsbergen JJ. Limited evidence for effects of diet for type 2 diabetes from systematic reviews. Eur J Clin Nutr. 2007;61(8):929–937. doi: 10.1038/sj.ejcn.1602611. [DOI] [PubMed] [Google Scholar]
- 6.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: results of the cross-national Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22(10):1379–1385. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 7.Glasgow RE, Hampson SE, Strycker LA, Ruggiero L. Personal-model beliefs and social-environmental barriers related to diabetes self-management. Diabetes Care. 1997;20(4):556–561. doi: 10.2337/diacare.20.4.556. [DOI] [PubMed] [Google Scholar]
- 8.Thanopoulou A, Karamanos B, Angelico F, Assaad-Khalil S, Barbato A, Del Ben M, Djordjevic P, Dimitrijevic-Sreckovic V, Gallotti C, Katsilambros N et al. Nutritional habits of subjects with Type 2 diabetes mellitus in the Mediterranean Basin: comparison with the non-diabetic population and the dietary recommendations. Multi-centre study of the Mediterranean Group for the Study of Diabetes (MGSD) Diabetologia. 2004;47(3):367–376. doi: 10.1007/s00125-003-1316-0. [DOI] [PubMed] [Google Scholar]
- 9.Snoek FJ. Barriers to good glycaemic control: the patient's perspective. Int J Obes Relat Metab Disord. 2000;24(Suppl 3):S12–S20. doi: 10.1038/sj.ijo.0801421. [DOI] [PubMed] [Google Scholar]
- 10.Yannakoulia M. Eating behavior among type 2 diabetic patients: a poorly recognized aspect in a poorly controlled disease. Rev Diabet Stud. 2006;3(1):11–16. doi: 10.1900/RDS.2006.3.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vijan S, Stuart NS, Fitzgerald JT, Ronis DL, Hayward RA, Slater S, Hofer TP. Barriers to following dietary recommendations in type 2 diabetes. Diabet Med. 2005;22(1):32–38. doi: 10.1111/j.1464-5491.2004.01342.x. [DOI] [PubMed] [Google Scholar]
- 12.Williamson AR, Hunt AE, Pope JF, Tolman NM. Recommendations of dietitians for overcoming barriers to dietary adherence in individuals with diabetes. Diabetes Educ. 2000;26(2):272–279. doi: 10.1177/014572170002600207. [DOI] [PubMed] [Google Scholar]
- 13.Spikmans FJ, Brug J, Doven MM, Kruizenga HM, Hofsteenge GH, van Bokhorst-van der Schueren MA. Why do diabetic patients not attend appointments with their dietitian? J Hum Nutr Diet. 2003;16(3):151–158. doi: 10.1046/j.1365-277x.2003.00435.x. [DOI] [PubMed] [Google Scholar]
- 14.Stott NC, Rees M, Rollnick S, Pill RM, Hackett P. Professional responses to innovation in clinical method: diabetes care and negotiating skills. Patient Educ Couns. 1996;29(1):67–73. doi: 10.1016/0738-3991(96)00935-4. [DOI] [PubMed] [Google Scholar]
- 15.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 16.Kollia M, Gioxari A, Maraki M, Kavouras SA. Development, validity and reliability of the Harokopio Physical Activity Questionnaire in Greek adults. Athens. 8th Panhellenic Congress on Nutrition and Dietetics; 2006. [Google Scholar]
- 17.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 18.Miller WR, Rollnick S. Motivational Interviewing: preparing people for change. The Guilford Press; New York: 2002. [Google Scholar]
- 19.Doherty Y, Hall D, James PT, Roberts SH, Simpson J. Change counselling in diabetes: the development of a training programme for the diabetes team. Patient Educ Couns. 2000;40(3):263–278. doi: 10.1016/s0738-3991(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 20.Raji A, Gomes H, Beard JO, MacDonald P, Conlin PR. A randomized trial comparing intensive and passive education in patients with diabetes mellitus. Arch Intern Med. 2002;162(11):1301–1304. doi: 10.1001/archinte.162.11.1301. [DOI] [PubMed] [Google Scholar]
- 21.Goudswaard AN, Stolk RP, Zuithoff NP, de Valk HW, Rutten GE. Long-term effects of self-management education for patients with Type 2 diabetes taking maximal oral hypoglycaemic therapy: a randomized trial in primary care. Diabet Med. 2004;21(5):491–496. doi: 10.1111/j.1464-5491.2004.01153.x. [DOI] [PubMed] [Google Scholar]
- 22.Hanefeld M, Fischer S, Schmechel H, Rothe G, Schulze J, Dude H, Schwanebeck U, Julius U. Diabetes intervention study. Multi-intervention trial in newly diagnosed NIDDM. Diabetes Care. 1991;14(4):308–317. doi: 10.2337/diacare.14.4.308. [DOI] [PubMed] [Google Scholar]
- 23.Pedersen O, Gaede P. Intensified multifactorial intervention and cardiovascular outcome in type 2 diabetes: the Steno-2 study. Metabolism. 2003;52(8 Suppl 1):19–23. doi: 10.1016/s0026-0495(03)00213-0. [DOI] [PubMed] [Google Scholar]
- 24.D'Eramo-Melkus GA, Wylie-Rosett J, Hagan JA. Metabolic impact of education in NIDDM. Diabetes Care. 1992;15(7):864–869. doi: 10.2337/diacare.15.7.864. [DOI] [PubMed] [Google Scholar]
- 25.Matchar DB, Keefe KJ, McCrory DC, Scipio CD, Cooper K, Kolimaga JT, Huntington AC. Use of behavioral therapies for treatment of medical disorders: part 1. Impact on management of patients with diabetes mellitus. Technology assessment. Agency for Healthcare Research and Quality; Rockville, MD: 2004. http://www.ahrq.gov/clinic/ta/diabetes/ [PubMed] [Google Scholar]


