Abstract
Objective
The current study investigated the self-reported temporal relationships of dieting, binge eating, and overweight in childhood.
Method
One hundred five non–treatment-seeking overweight children ages 6–13 years were interviewed with the children’s Eating Disorder Examination (ChEDE) and queried regarding dieting, loss of control (LOC) eating, and overweight history. Questionnaires of depressive symptoms, trait anxiety, and parent-reported problems were completed.
Results
Sixty percent of the children reported having attempted at least one diet. These children had higher ChEDE scores (global, p < .001), greater body mass index (BMI) and body fat mass (p ≤ .001), and a trend towards an earlier reported age of overweight onset (p = .06) compared with children who had never dieted. The 29.5% of children who reported LOC eating had significantly higher ChEDE scores (global, p < .001), ineffectiveness, negative self-esteem, and externalizing scores (all ps < .05) compared with those who had never experienced LOC eating. Most children reported becoming overweight before either dieting (79.4%) or experiencing LOC eating (63.6%). Among the 25.7% reporting both dieting and LOC eating, two thirds reported LOC eating before dieting. Participants who reported dieting before overweight had higher negative mood scores (p < .01). Children reporting dieting before LOC eating had higher ChEDE Weight Concern (p < .01) and global (p < .05) scores.
Discussion
For overweight, non–treatment-seeking children, both dieting and LOC eating are common. Dieting precedes the development of LOC eating only one third of the time, but is associated with greater disordered eating cognitions. The relationship between childhood-onset dieting and LOC eating in overweight children requires further investigation to determine the causal pathways for the subsequent development of eating disorders.
Keywords: middle childhood, overweight, dieting, loss of control, binge eating
Introduction
Dieting, subthreshold eating-disordered disturbance, and childhood obesity each has been identified as risk factors for the development of eating disorders (e.g., Fairburn et al., 1998; Fairburn, Welch, Doll, Davies, & O’Connor, 1997; Killen et al., 1996). However, the timing of their manifestation and the interactions between these risk factors in the development of eating and/or weight problems have remained largely unexplored in middle childhood.
Dieting in childhood is not uncommon (Hill, Oliver, & Rogers, 1992), and it has been reported that children as young as 8 years old engage in dieting behaviors (Hill & Pallin, 1998). Both retrospective and prospective studies in adolescents have found self-reported dieting to predict bulimic symptoms (Field, Camargo, Taylor, Berkey, & Colditz, 1999; Stice & Agras, 1998) and eating-related psychopathology (Leon, Fulkerson, Perry, Keel, & Klump, 1999; Patton, Johnson-Sabine, Wood, Mann, & Wakeling, 1990; Santonastaso, Friederici, & Favaro, 1999). Such results have been interpreted as consistent with restraint theory, which posits that dietary restriction should increase the risk for the onset of binge eating and bulimic pathology (Polivy & Herman, 1985). Although children with greater body mass are more likely to diet in proportion to their degree of obesity (Hill, Draper, & Stack, 1994; Patton et al., 1997), little is know about the relationship between dieting and disturbed eating in young overweight children, when dieting behaviors may first emerge.
Binge eating has also been found to occur before adolescence. Whether assessed by self-report questionnaires (Morgan et al., 2002) or interview methodology (Tanofsky-Kraff et al., 2004), the experience of loss of control (LOC) while eating, as opposed to the amount of food eaten, has been found to be significantly related to elevations in disturbed eating cognitions, depressive symptoms and anxiety, and to body adiposity. Among preadolescent children, those who are overweight are also significantly more likely to engage in LOC eating behaviors than their normal-weight counterparts (Tanofsky-Kraff et al., 2004).
Retrospective studies of overweight adults with binge eating disorder (BED) examining the perceived onset of dieting and binge eating suggest that different potential pathways to BED exist. In one path, dieting precedes the development of binge eating behavior, whereas along another path, binge eating appears to develop before dieting (Abbott et al., 1998; Grilo & Masheb, 2000; Marcus, Moulton, & Greeno, 1995; Spurrell, Wilfley, Tanofsky, & Brownell, 1997). For adult patients who reported binge eating before the onset of dieting behavior (≤ 50% of participants across studies), binge eating was described as first occurring between the ages of 11 and 13 years. Furthermore, those who reported early onset of binge eating met the criteria for BED at an earlier age (Abbott et al., 1998; Grilo & Masheb, 2000; Spurrell et al., 1997) and had a greater lifetime history of psychiatric disturbance (Spurrell et al., 1997) than patients who remembered dieting before binge eating. Finally, early reported onset of binge eating (at age ≤16 years) has been associated with poor treatment outcome (Agras et al., 1995; Safer, Lively, Telch, & Agras, 2002; Wilfley et al., 2004). Such findings are not consistent with restraint theory and have promoted researchers to examine other theoretical models that might explain the development of BED when binge eating occurs before the development of dieting.
Given that young, overweight children appear to be at greater risk than normal-weight children for dieting and LOC eating, examining the perceived temporal sequence of these behaviors may provide intervention targets for the prevention of greater eating disturbance or inappropriate weight gain. We interviewed non–treatment-seeking overweight (≥85th percentile for age, race, and gender) boys and girls, age 6–13 years, to obtain their self-reported dieting and overweight history and to determine the age of onset of LOC eating. Our primary aim was to relate the temporal sequence of self-reported dieting, LOC eating, and overweight to differences in eating-disordered cognitions, depressive symptoms, trait anxiety, parent-reported problems, and body composition. Based on retrospective studies of adults with BED, we hypothesized that similar percentages of participants would report dieting before LOC eating as those reporting LOC eating before dieting. We also hypothesized that those who reported LOC eating first would have similar levels of eating-disordered cognitions, but greater general psychopathology and an earlier reported onset of overweight than those who reported dieting first.
Methods
Participants
Individuals participating in ongoing metabolic studies at the National Institutes of Health (NIH; Bethesda, MD) served as participants (Feng et al., 2003). Children, regardless of weight status, were recruited through two waves of notices mailed to first-grade to fifth-grade children in the Montgomery County and Prince Georges County, Maryland, school districts and two mailings to local family physicians and pediatricians. Mailings to families requested participation of children willing to undergo collection of blood samples and X-rays for studies investigating hormone levels in children. Mailings to physicians requested assistance in identifying children willing to participate in similar studies. All recruitment materials specified that no treatment would be offered. Eighty-eight percent of participants studied were recruited through parent mailings and 12% were identified from physician referrals. None of the children accepted into the study were undergoing weight loss treatment. All were aware that they would not receive any type of treatment as part of the study protocol or after participation, but would be compensated financially for their time. Participants were medication free for ≥2 weeks before being studied and none had significant medical disease. Each child had normal hepatic, renal, and thyroid function. Children provided written assent and parents gave written consent for participation in the protocol. This study was approved by the institutional review board of the National Institutes of Child Health and Human Development.
Procedure and Assessment
Participants were seen at the NIH Warren Grant Magnuson Clinical Center. All children underwent a medical history and a physical examination conducted by a pediatric endocrinologist or a trained pediatric nurse practitioner. Each child completed the children’s version of the Eating Disorder Examination (ChEDE), the Children’s Depression Inventory, and the State-Trait Anxiety Inventory for Children (STAIC).
The Eating Disorder Examination (EDE; Fairburn, & Cooper, 1993) adapted for children (ChEDE; Bryant-Waugh, Cooper, Taylor, & Lask, 1996) is an investigator-based interview that differs from the adult version only in that its script has been edited to make it more accessible to children aged 8–14 years and that two items that assess the critical overvaluation of shape and weight have been supplemented with a sort task. The ChEDE contains 21 items that assess disordered attitudes and behaviors related to eating, body shape, and weight, and 13 items designed to diagnose specific eating disorders as defined in the 4th ed. of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association [APA, 1994]). Responses are coded via four subscales: Restraint (dietary restraint, as measured by behavioral and/or cognitive restraint), Eating Concern, Shape Concern, and Weight Concern. An overall global score consisting of the average of the four subscales is generated. (For a detailed description of the ChEDE and its use in the current study, see Tanofsky-Kraff et al., 2004.)
The ChEDE had been used successfully in children as young as 6 years old (Tanofsky-Kraff et al., 2003, 2004). In a community sample of overweight and normal-weight children (6–13 years), the ChEDE revealed excellent interrater reliability (intraclass correlation) for subscales from .95 to .99 (all ps < .001) (Tanofsky-Kraff et al., 2004). Furthermore, the ChEDE demonstrated good internal consistency and discriminant validity in a sample of young girls (8–14 years) diagnosed with anorexia nervosa, selective eating, or food avoidance emotional disorder (Frampton, 1996).
Age of Onset Questions
We embedded questions regarding the age of onset of LOC eating (regardless of amount of food eaten), dieting, and overweight following the overeating section of the ChEDE, where the construct of LOC eating is explored and explicated for participants. We then queried participants on the specific nature of their first dieting attempt, how many dieting attempts they had made, and the length of their first diet. In addition, we asked each child which behaviors preceded the others. As child recall has not demonstrated strong validity in other areas of psychiatric disturbance (Agnold, Erkanli, Costello, & Rutter, 1996), we opted to interview each participant, in the same semistructured, investigator-based fashion as the ChEDE is administered. To assist the children in making the most accurate assessment of the age of onset of each behavior, we asked them to recall not only their age in years, but also their school grade, their teacher, and friends at the time, with the aim of anchoring their memory to a specific time period. If a response appeared questionable, we probed participants as to why they recalled each behavior occurring at the time period stated. If, based on the discretion of the research team, a participant’s response was unclear, that individual’s data were eliminated from the analyses. (For the complete series of questions, see Appendix 1.)
Growth Chart Data
After obtaining parental consent, we retrieved height and weight charts from children’s primary care providers for a subset (n = 25) of the sample to determine objectively when body mass index (BMI)-(SD) standard deviation score exceeded the 85th and 95th percentile for age, gender, and height. Using these data, children’s actual age when they became overweight was compared with their recall of the age at which they became overweight.
General Psychopathology
Children completed the Children’s Depression Inventory (CDI; Kovacs, 1982). The CDI is a 27-item self-rated measure of depressive feelings that generates a total score and five subscale scores (Negative Mood, Interpersonal Problems, Ineffectiveness, Anhedonia, and Negative Self-Esteem). They also completed the State-Trait Anxiety Inventory for Children, A-Trait scale (STAIC; Spielberger, Edwards, Lushene, Montuori, & Platzek, 1973), a 20-item self-report measure of trait anxiety developed for use with elementary school children. Parents were asked to complete the Child Behavior Checklist (CBCL; Achenbach & Elderbrock, 1991) for children 4–18 years old, an empirically derived measure with excellent norms that assesses a range of internalizing and externalizing symptoms.
Body Composition
Measurement of height (measured three times to the nearest 1 mm) was performed using a stadiometer (Holtain Ltd., Crymmych, Wales) calibrated before each child’s height measurement to the nearest 1 mm. Weight to the nearest 0.1 kg was obtained using a calibrated digital scale (Scale-Tronix, Wheaton, IL). From these measurements, BMI (kg/m2) was calculated.
Each participant also underwent dual-energy x-ray absorptiometry (DXA) using Hologic QDR-2000 or Hologic QDR 4500A equipment (Hologic, Waltham, MA) for determination of body fat mass and lean body mass. Findings from DXA fat mass measurements have demonstrated excellent reproducibility in children (Figueroa-Colon, Mayo, Treuth, Aldridge, & Weinsier, 1998). Pubertal breast and pubic hair stage were ascertained through physical examination by a pediatric endocrinologist or trained pediatric nurse practitioner to one of the five standards of Tanner (Marshall & Tanner, 1969, 1970). Testicular volume (in cubic centimeters) for boys was also assessed using an orchidometer. Pubertal stage and testicular volume can be considered surrogate measurements of neurocognitive maturity as well as objective measures of physical maturity (Marshall & Tanner, 1969).
Statistical Analyses
Spearman rho correlations were used to examine relationships between self-reported overweight onset and overweight onset based on medical growth charts. Comparisons between groups were performed using one-way analysis of variance (ANOVA) with a Bonferroni-Hochberg correction, a conservative test accounting for multiple comparisons applied to each family of post-hoc tests. Chi-square tests were used to compare the temporal sequence of reported dieting, LOC eating, and overweight. Relationships between the length and number of diets and the ChEDE scales were examined using bivariate correlations. A z score standardizing for age, gender, and race was used for BMI (BMI-SD; Frisancho, 1990). To determine relevant covariates, we entered age, race, socioeconomic status (SES), gender, and pubertal stage into each full model and removed the covariates that were not significant. In the analyses comparing children who had reportedly dieted in their lifetime with those who had not, age was a relevant covariate in examining CDI total and Anhedonia scores, and trait anxiety. For CBCL externalizing and total t scores analyses, BMI-SD served as a covariate. Effect sizes (r) are reported. Means adjusted for covariates are reported. Differences and associations between groups were considered significant when p values were ≤.05 and all tests were two-tailed.
Results
Of 412 non–treatment-seeking children recruited for metabolic studies, 105 (age = 6.1–13.8 years, range = 10.4 ± 1.6 years) who were overweight (BMI ≥85th percentile) served as participants. 1Children in the current study did not differ by age, race, gender, or SES compared with the 307 children who were not studied (data not shown). Almost all participants were African American (n = 43 [41%]) or Caucasian (n = 59 [56.2%]), and 2.8% (n = 3) identified themselves as other. The sample had a mean BMI-SD of +3.4 ± 2.4 (range = −0.4 to +12.9) and total percent body fat by DXA ranged from 14% to 58% (M ± SD = 40.3 ± 10.3). The 61 girls (58.1%) and 44 boys (41.9%) were of a similar socioeconomic background, with a median Hollings head Index score of 3 (range = 1–5), and varied in their pubertal development (girl’s breast tanner stage, 2.7 ± 0.90 [range = 1–5]; boy’s testicular volume (cc), 4.29 ± 3.8 [range = 1–15 cc]). According to their ChEDE interviews, none of the children in our sample met criteria for a DSM-IV eating disorder (APA, 2000).
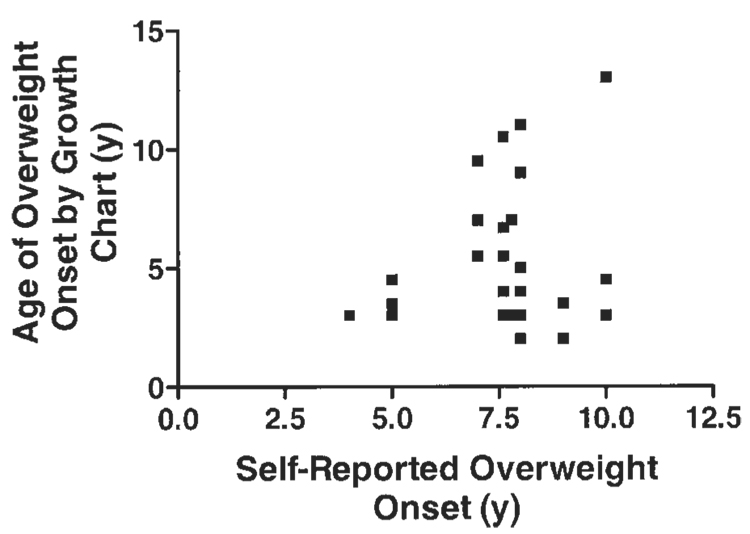
The mean reported age of overweight onset was 7.6 ± 2.1 years (range = 1–12 years). For the subset of participants for whom we retrieved growth charts (n = 25), children reported becoming overweight significantly later than documented by their physicians (5.4 ± 3.0 years for age when first exceeded BMI ≥85th percentile [range = 2–13 years], p = .002). Self-reported overweight onset was poorly correlated with the age at which BMI exceeded either the 85th percentile (r = −.06, p = .38; Figure 1) or the 95th percentile (r = −.17, p = .21) based on growth charts.
FIGURE 1.
Relationship between overweight onset as defined by the 85th percentile based on growth chart and self-reported overweight onset. R = −.06, p = .38.
To determine whether dieting and LOC eating behaviors were meaningful and distinguishable constructs in our sample, we compared children who had dieted with those who had never dieted and participants who had engaged in LOC eating with those who had never engaged in such behavior.
Dieting
Sixty-three (60%) children reported that they had attempted to lose weight by dieting at least once in their lifetime. Children who had dieted were not different in gender or race compared with other participants. The reported mean age of children’s first diet was 8.8 ± 1.8 years (range = 5–13 years), lifetime dieting attempts ranged from 1 attempt to 10 attempts (M = 2.6 ± 2.2), and length of first diet in days ranged from 1 day to 365 days (M = 42.5 ± 80.0). In describing their first dieting attempt, 52.9% reported making food changes only, such as eating smaller portions, avoiding foods, and eating healthier or lower fat foods, 25.5% reported making food changes and exercising, and the remainder (21.6%) reported following a structured diet program such as Slim Fast, Weight Watchers, Jenny Craig, or the Atkins diet. None engaged in unhealthy dieting behaviors.
When comparing children who had ever dieted with those who reportedly had never dieted, dieters were slightly older (10.8 ± 1.4 years vs. 10.0 ± 1.8 years; t = 2.5, p < .05), and had higher BMI-SD and greater percent body fat by DXA (both ps ≤ .001; Table 1). Furthermore, dieters had significantly higher Restraint, Shape Concern, Weight Concern, and global (all ps < .001) scores on the ChEDE (Table 1). Controlling for current age, dieters had a trend (p = .06) toward an earlier onset age of reported overweight. No differences were found between dieters and those who had never dieted on any of the CDI or CBCL scales or trait anxiety scale (Table 1).
TABLE 1.
Children reporting previous dieting
| Ever Diet (n = 63) | Never Diet (n = 42) | Statistic F | Effect Size (r) | |
|---|---|---|---|---|
| Reported age of onset | ||||
| Onset age of overweight (years) | 7.4 ± 2.2 | 8.5± 2.1 | 3.6* | −.25 |
| Onset age of dieting (years) | 8.8 ± 1.8 | — | — | — |
| Onset age of LOC (years) | 8.5 ± 2.0 | 7.8 ± .98 | 0.50 | .22 |
| Number of dieting attempts | 2.6 ± 2.2 | — | — | — |
| Length of first diet (days) | 42.5 ± 80.0 | — | — | — |
| Body composition | ||||
| BMI-SD | 4.1 ± 2.5 | 2.4 ± 2.0 | 12.9*** | .35 |
| DXA percent fat mass | 43.4 ± 8.8 | 35.8 ± 10.6 | 15.6*** | .36 |
| ChEDE subscales | ||||
| Restraint | 1.1 ± 1.0 | 0.24 ± 0.56 | 24.6*** | .47 |
| Eating Concern | 0.18 ± 0.32 | 0.08 ± 0.27 | 3.2 | .17 |
| Shape Concern | 1.1 ± 1.1 | 0.38 ± 0.70 | 14.4*** | .36 |
| Weight Concern | 1.7 ± 1.2 | 0.38 ± 0.77 | 40.3*** | .55 |
| ChEDE global score | 1.0 ± 0.75 | 0.27 ± 0.45 | 34.5*** | .51 |
| CDI | ||||
| Total | 5.9 ± 4.8 | 6.5 ± 5.4 | 0.02 | −.06 |
| Negative Mood | 1.2 ± 1.3 | 1.1 ± 0.93 | 0.50 | .04 |
| Interpersonal Problems | 0.45 ± 0.72 | 0.65 ± 1.1 | 1.2 | −.11 |
| Ineffectiveness | 1.0 ± 1.3 | 1.2 ± 1.6 | 0.38 | −.07 |
| Anhedonia | 2.4 ± 2.3 | 3.1 ± 2.8 | 0.24 | −.14 |
| Negative Self-Esteem | 0.71 ± 1.0 | 0.53 ± 0.81 | 0.96 | .10 |
| STAIC-Trait Anxiety | 33.1 ± 7.8 | 34.0 ± 8.0 | 0.06 | −.06 |
| CBCL | ||||
| Internalizing t-score | 53.0 ± 12.3 | 48.2 ± 11.0 | 4.0 | .20 |
| Externalizing t-score | 51.0 ± 9.7 | 47.1 ± 10.6 | 0.42 | .19 |
| Total t-score | 53.3 ± 10.4 | 46.4 ± 12.7 | 2.4 | .28 |
Note: Ever Diet = children reporting previous dieting; Never Diet = children denying past dieting; ChEDE = child’s version of the Eating Disorder Examination; CDI = Children’s Depression Inventory; STAIC = State-Trait Inventory for Children; BMI-SD = body mass index-Standard Deviation Score; CBCL = Child Behavior Checklist; LOC = loss of control eating; DXA = dual-energy X-ray absorptiometry. Analyses for the ChEDE Weight subscale and global score include DXA fat mass as a covariate; CDI total and Anhedonia and STAIC analyses include age as a covariate; analyses for CBCL externalizing and total t scores include BMI-SD as a covariate. For reported onset age of LOC analysis, Ever Diet (n = 27) and Never Diet (n = 6).
p = .06.
p ≤ .001.
When examining the 63 children who had ever dieted, significant relationships were found between the number of dieting attempts and the ChEDE Restraint subscale (r = .36, p < .01) and global score (r = .29, p < .05). The length of first diet also significantly correlated with the Restraint (r = .32), Eating Concern (r = .29), and global (r = .30) scores (all ps < .05). No other relationships were detected.
LOC Eating
Thirty-one (29.5%) participants reported experiencing LOC eating at least once in their lifetime. Children who had experienced LOC eating were not biased by race or gender. The mean reported age of first LOC eating was 8.4 ± 1.9 years (range = 5–13 years). Children who had ever experienced LOC eating had significantly higher Restraint (p < .05), Eating Concern (p = .001), Shape Concern (p < .01), Weight Concern (p < .001), and global (p < .001) ChEDE scores compared with children who had never experienced LOC eating (Table 2). Furthermore, those who had ever experienced LOC eating had significantly higher CDI Ineffectiveness (p = .01) and Negative Self-Esteem (p < .05) scores and higher CBCL total (p = .01) and externalizing (p < .05) t scores. Groups did not differ on trait anxiety, reported onset age of overweight, or reported onset age of first diet.
TABLE 2.
Children reporting a history of LOC
| Ever LOC (n = 31) | Never LOC (n = 74) | Statistic F | Effect Size (r) | |
|---|---|---|---|---|
| Reported age of onset | ||||
| Onset age of overweight (years) | 7.3 ± 1.8 | 7.8 ± 2.4 | 0.88 | −.12 |
| Onset age of first diet (years) | 8.9 ± 1.9 | 8.7 ± 1.8 | 0.22 | .05 |
| Onset age of LOC (years) | 8.4 ± 1.9 | — | — | — |
| Number of dieting attempts | 3.1 ± 2.8 | 2.3 ± 1.6 | 2.1 | .08 |
| Length of first diet (days) | 48.6 ± 86.0 | 38.0 ± 76.5 | 0.22 | .06 |
| Body composition | ||||
| BMI-SD | 4.1 ± 2.3 | 3.2 ± 2.5 | 3.2 | .18 |
| Percent DXA fat mass | 29.8 ± 12.9 | 26.1 ± 14.8 | 0.94 | .13 |
| ChEDE subscales | ||||
| Restraint | 1.3 ± 1.1 | 0.62 ± 0.89 | 6.0* | .32 |
| Eating Concern | 0.34 ± 0.39 | 0.06 ± 0.21 | 21.4*** | .41 |
| Shape Concern | 1.3 ± 1.2 | 0.62 ± 0.93 | 10.5** | .30 |
| Weight Concern | 1.8 ± 1.3 | 0.91 ± 1.1 | 13.6*** | .35 |
| ChEDE global score | 1.2 ± 0.81 | 0.56 ± 0.65 | 15.9*** | .40 |
| Children’s Depression Inventory | ||||
| Total | 7.5 ± 4.6 | 5.5 ± 5.2 | 3.9 | .20 |
| Negative Mood | 1.5 ± 1.2 | 1.0 ± 1.1 | 3.5 | .21 |
| Interpersonal Problems | 0.57 ± 0.78 | 0.51 ± 0.95 | 0.16 | .03 |
| Ineffectiveness | 1.6 ± 1.5 | 0.85 ± 1.3 | 6.7** | .26 |
| Anhedonia | 2.8 ± 2.0 | 2.7 ± 2.7 | .06 | .02 |
| Negative Self-Esteem | 1.1 ± 1.3 | 0.46 ± 0.75 | 8.8** | .29 |
| STAIC-Trait Anxiety | 35.5 ± 6.7 | 32.9 ± 8.1 | 1.6 | .17 |
| Child Behavior Checklist | ||||
| Internalizing t-score | 53.7 ± 11.8 | 50.0 ± 12.0 | 2.0 | .15 |
| Externalizing t-score | 52.7 ± 9.6 | 48.1 ± 10.2 | 4.6* | .23 |
| Total t-score | 55.1 ± 10.4 | 48.6 ± 11.9 | 6.4** | .28 |
Note: p < 0.05.
p ≤ 0.01.
p ≤ 0.001.
Ever LOC= children reporting past loss of control eating; Never LOC= children reporting no loss of control eating episodes; BMI-SD = ; DXA = dual-energy x-ray absorptiometry; CHEDE children’s Eating Disorder Examination; STAIC Trait Inventory for Children. For reported first diet analysis, Ever LOC (n = 23) and Never LOC (n = 35).
Temporal Order of Reported Overweight, Dieting, and LOC Eating
Of the 63 dieters, 50 children reported becoming overweight before dieting, 3 reported dieting before becoming overweight (χ2 = 41.7; p < .001), and 10 children could not recall whether they dieted or became overweight first. Children who reported dieting before becoming overweight had significantly higher CDI Negative Mood scores than those who became overweight first (3.5 ± 0.71 vs. 1.2 ± 1.2), F(1,49) = 7.4, p < .01. No significant differences were found on any other demographic or dependent variable (data not shown). Of the group who had dieted, growth charts were retrieved for 13 participants. According to their growth charts, all but 1 child accurately reported the temporal sequence of the occurrence of their first diet and when they first became overweight.
Of the 31 children who had reported ever experiencing LOC eating, 21 reported becoming overweight before LOC eating, 6 reported LOC eating before becoming overweight (χ2 = 8.3; p < .01), and 4 could not recall their temporal sequence. No significant differences were found between groups on any dependent variable (data not shown). Of children who had ever experienced LOC eating, seven growth charts were retrieved and all but 1 child accurately reported that they were overweight before self-reported LOC.
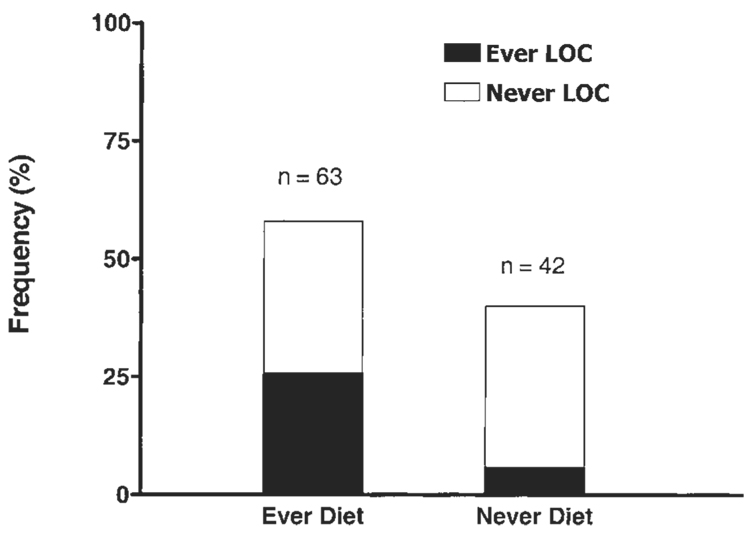
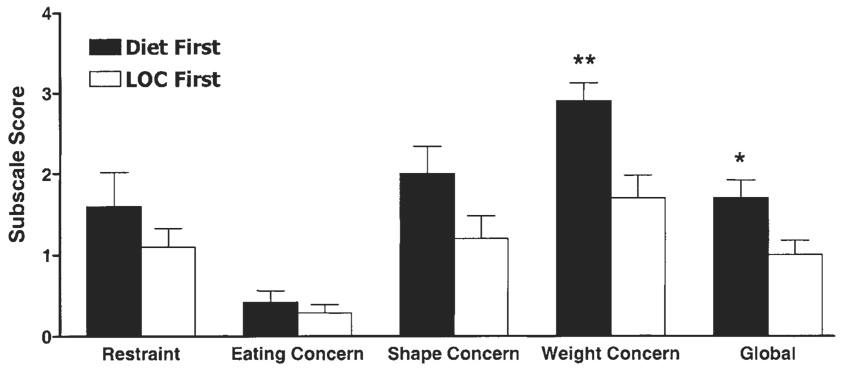
Twenty-seven children (25.7% of the total sample) had reportedly both dieted in their lifetime and experienced LOC eating. Six children had experienced LOC eating without also dieting, so that only 19.5% of those who had reportedly experienced LOC eating had not dieted in their lifetime (Figure 2). Of the 27 children who had both dieted and experienced LOC eating, 18 reported overweight before either LOC eating or dieting, 9 reported having dieted before LOC eating (Diet First), and 18 reported LOC eating before dieting (LOC First) (χ2 = 3.0 for Diet First vs. LOC First; p = 0.08). Compared with the LOC First group, the Diet First group had significantly greater ChEDE Weight Concern (p < .01) and global (p < .05) scores (Figure 3). No other group differences were detected (data not shown).
FIGURE 2.
Relationships between dieting and loss of control (LOC) eating in overweight children. Ever LOC = children who reported at least one episode of LOC eating; Never LOC = children who reported no such episodes; Ever Diet = children who reported attempting at least one diet; Never Diet = children who reported no dieting attempts.
FIGURE 3.
Children’s Eating Disorder Examination (ChEDE) scores of children who reported both dieting and loss of control (LOC) eating. Diet First = children whose first attempted diet preceded their first LOC eating episode; LOC First = children whose first LOC eating episode preceded their first attempted diet. **p < .01; *p < .05, Diet First vs. LOC First.
Discussion
Examining the perceived temporal sequence of dieting, LOC eating, and overweight in non–treatment-seeking overweight children, we found that most reported becoming overweight (and by growth chart data were actually overweight) before dieting or LOC eating, and many children (65%) reported engaging in LOC eating before dieting. Participants who reported dieting before overweight onset had significantly higher CDI Negative Mood scores, and children who reported dieting before LOC eating had broadly higher ChEDE scores and significantly higher Weight Concern and global scores.
Consistent with previous studies (Hill & Pallin, 1998; Hill et al., 1992;), we found that a substantial percentage of overweight children report previous dieting attempts. Unlike adolescent surveys (Brugman et al., 1997; French, Perry, Leon, & Fulkerson, 1995; Story & Neumark-Sztainer, 1998), the children in our sample did not report engaging in unhealthy weight control behaviors such as use of diet pills, fasting, or purging, but rather reported the types of dietary changes that may be recommended for pediatric obesity treatment. However, these findings may be a reflection of parental control over their children’s behaviors. We found that children who stated they had dieted were heavier and scored higher on the ChEDE subscales than those who denied past dieting, suggesting that early dieting in overweight children could be a marker for future eating disturbance, although longitudinal studies are needed to make this determination.
Not surprisingly, most children reported overweight before dieting. However, adolescent and adult research has been inconsistent regarding whether obesity leads to binge eating for most individuals (Fairburn, Cooper, Doll, & Welch, 1999; Fairburn et al., 1998; Vogeltanz-Holm et al., 2000) or whether binge eating is a risk factor for overweight (Field et al., 2003) (Stice, Cameron, Killen, Hayward, & Taylor, 1999; Stice, Presnell, & Spangler, 2002). One study querying the parents of obese treatment-seeking children also found that overweight typically preceded binge eating (Decaluwe & Braet, 2003). The observation that 3 children who reported dieting before becoming overweight had higher CDI Negative Mood scores suggests the possibility that weight control efforts before overweight may be associated with greater psychological problems, although these findings must be interpreted cautiously given the few children in the sample. Nevertheless, these findings are intriguing and point to the possibility that weight status in childhood may have implications regarding the developmental pathways to eating disturbance. Along one trajectory, overweight may be a risk factor for eating and weight disorders, such as bulimia nervosa or BED, whereas another pathway, more common in normal weight children, may begin with restrictive eating behaviors.
Retrospective studies examining the onset ages of dieting, binge eating, and overweight in adults with BED have found no differences between the eating-disordered cognitions of individuals who report binge eating before dieting compared with those who report dieting before binge eating (Grilo & Masheb, 2000; Spurrell et al., 1997). Our findings in children without clinical eating disorders differ from these adult BED studies. It has been posited that once eating-disordered symptoms reach clinical significance, the temporal sequence of binge eating and dieting may not affect current distress (Spurrell et al., 1997). Moreover, the mean age of the participants in the aforementioned adult studies ranged from 39 years to 44 years. As the children in our sample were considerably closer in age to the milestones they were asked to recall, their reports of the order of events might be anticipated to be more accurate than adult retrospective recall. Alternatively, our overweight, non–treatment-seeking sample may differ from participants in the adult literature, many of whom were not overweight during childhood.
Also notable were findings that children who reported dieting before LOC eating had significantly higher ChEDE Weight Concern scores, because elevated Weight Concern scores and thin body preoccupation are believed to place individuals at risk for the development of eating disorders (Killen et al., 1994, 1996; McKnight Investigators, 2003). If the overweight children who reported dieting before LOC eating develop eating disorders in the future, our findings may offer preliminary support for restraint theory (Polivy & Herman, 1985) and the cognitive-behavioral model (Fairburn, 2002) which propose that eating disorders occur in response to the application of excessive dietary restraint resulting from elevated weight concern.
Almost twice as many children in our sample reported LOC eating before dieting, suggesting that should these participants develop eating disorders in the future, a model other than (or in addition to) restraint theory would warrant consideration (Wilfley, Pike, & Striegel-Moore, 1997). However, unlike the BED literature, which suggests that adults who binge eat before dieting have greater lifetime psychopathology (Spurrell et al., 1997), no differences were found on variables of depressive symptoms, trait anxiety, or parent-reported problems based on whether LOC eating or dieting occurred first in our sample. Given the mean age of our participants and that none of the children were seeking treatment, it is perhaps not surprising that significant psychological problems, which typically manifest in adolescence, have yet to develop in young children, or are not detected by their parents. Longitudinal investigations are required to determine whether theories other than the restraint model predict the development of a full-syndrome eating disturbance.
The strengths of the current study include the use of interview methodology for the investigation of eating-disordered pathology and the racially diverse sample. The primary limitation of the study is the use of retrospective recall and self-reported variables, in particular, overweight. Although self-reported age of onset for overweight did not correlate well with growth chart data, children appeared to have accurately recalled the temporal sequence of overweight with dieting and LOC eating. Given that the objective measures of child overweight indicated that most of the participants were very young when they reached the 85th percentile (70% were between 2 and 5 years according to growth chart data), it is not surprising that children relied on their own perception of what age they became overweight, as neither children nor adults typically have recall of events before the age of 5 years (Brewin, Andrews, & Gotlib, 1993). In addition, it has been proposed (but not tested) that long-term memory is not stored by calendar dates or a stream of isolated events, but rather as temporal-causal sequences (Bradburn, 2000). Based on our consistent findings on temporal sequence using both self-reported and growth chart overweight onset, we believe that the perceived temporal sequence (our primary variable of interest) of overweight, dieting, and LOC eating was accurately reported. Furthermore, unlike the development of excess adiposity, dieting and LOC eating both involve actively engaging in specific behaviors and the mean age of our sample was quite close to the reported onset ages of these investigated phenomena. Research has shown that time is related to the accuracy of recall because the more recently an event occurred (within the past 2–3 years), the easier it is to recall (Bradburn, Rips, & Shevell, 1987). Finally, our use of the semistructured interview format to query participants, a methodology recommended to enhance recall (Brewin et al., 1993), coupled with detailed probing to anchor children’s recall to specific time frames (e.g., first dieting attempt and surrounding context), increases the likelihood that onset ages of these variables were accurately reported relative to one another.
Other limitations are that children were not recruited in a truly population-based fashion, although they were aware that they would not be receiving any weight loss treatment in return for their participation. Nonetheless, because the families in our sample chose to respond to our notices, they may be unique in other ways, limiting the external validity of the study.
We conclude that, for overweight, non–treatment-seeking children, both dieting and LOC eating are common and are associated with eating-disordered cognitions, and that children perceive dieting as an event that precedes the development of LOC eating only one third of the time. However, it is the perception of early-onset dieting that is most associated with eating-disordered distress during middle childhood. These data may support the importance of restraint theory as well as other models for the development of eating disorders. Longitudinal research is required to clarify the multiple potential pathways that may lead to the development of eating disorders in adolescence or adulthood.
Acknowledgments
Supported by Z01-HD-04-00641 (J.A.Y.) and by the National Center for Minority Health and Health Disparities (J.A.Y.).
Appendix 1
Age of Onset of any Eating-Disordered Behavior, Overweight, and Dieting
If no objective (OBE) or subjective bulimic episodes (SBE) exist:
• Did you ever feel a loss of control like I described – where you felt like you just could not stop eating? (use analogies to describe loss of control [LOC] eating)
___Yes ___No
If yes:
• In what grade (or at what age) do you first remember feeling that way?
___Grade (ask child to recall class teacher, etc. to anchor age) ___Age
If determine that any eating-disordered behavior (SBE or OBE) or an eating disorder exist:
• In what grade (or at what age) were you when you first began eating like we just talked about? (review type of pathologic eating behavior if unclear to child)
___Grade (ask child to recall class teacher, etc. to anchor age) ___Age
Briefly note pathologic eating behavior OR check applicable eating disorder:
___OBE ___SBE ___LOC only ___binge eating disorder ___bulimia nervosa ___anorexia nervosa
Age of onset of overweight:
• In what grade (or at what age) do you first remember being overweight?
___Grade (ask child to recall class teacher, etc. to anchor age) ___Age
Age of onset of dieting: (Some of these questions and the Restraint subscale questions might seem somewhat redundant, however, ask them anyway to confirm that dieting existed and when it did.)
• Have you ever tried to diet or eat less than you would like to lose weight or keep your weight at a certain number for any reason? If says no, Have you ever spent time thinking about it and trying to do it, but were not able to?
___Yes ___No
If says yes to either question, For what reason?
Note whether or not reason was to control shape/weight:
• How many different times have you tried to diet or eat less than you would like (even if you did not do it) or have dieted?
___Number of times
• In what grade (or at what age) were you when you first dieted or avoided eating, even if you were unable to do it?
___Grade (ask child to recall class teacher, etc. to anchor age) ___Age
If applicable, For how long did you try to diet or try to eat less than you would like? (Determine length of time.)
___Days ___Months ___Years
• In either case, What did you do to diet? or What did you do when you tried to diet? If more than one attempt, Can you tell me about the first time you tried to diet? Include the following probes as needed:
Sometimes people will count calories or fat, or just eat less food overall. Other times, people will try to do these things, but are not able to. Please explain to me, as best as you can exactly what you do or think, even if you are not able to do what you are thinking or trying to do. What happened to your weight?
Explain specific behavior (obtain as much detail as possible)
• IF APPLICABLE:
Which came first (Use all probes related to age and grade to help the child recall)
Trying your best to remember, do you think that you dieted or tried to diet before you were overweight? Or, do you think that you were overweight before you tried to diet or did diet? (Check one)
___Dieted/tried to diet first ___Overweight first
Trying your best to remember, do you think that you dieted or tried to diet before you did this type of eating (review LOC)? Or, do you think that you did this type of eating (review type of pathologic eating behavior or LOC), before you tried to diet or did diet? (Check one)
___Dieted/tried to diet first ___Eating disorder/eating-disordered behavior first
Trying your best to remember, do you think that you did this type of eating (review LOC) before you were overweight? Or, do you think that you were overweight before you did this type of eating (review type of pathologic eating behavior or LOC)? (Check one)
___Eating disorder/eating-disordered behavior first ___Overweight firs
Footnotes
Current Centers for Disease Control terminology indicate that children with a BMI ≥85th percentile are at risk for overweight and those with a BMI ≥95th percentile are overweight However, for the purposes of the current article, we will refer to children with a BMI ≥85th percentile as overweight.
Portions of this manuscript were presented at the 2003 International Conference on Eating Disorders, Denver, Colorado, May 29–June 1.
Dr. Jack A. Yanovski is a Commissioned Officer in the U.S. Public Health Service, Department of Health and Human Services.
References
- Abbott DW, de Zwaan M, Mussell MP, Raymond NC, Seim HC, Crow SJ, Crosby RD, Mitchell JC. Onset of binge eating and dieting in overweight women: Implications for etiology, associated features and treatment. Journal of Psychosomatic Research. 1998;44(3–4):367–374. doi: 10.1016/s0022-3999(97)00261-4. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Elderbrock C. Burlington, VT: University of Vermont Press; 1991. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. [Google Scholar]
- Agnold A, Erkanli A, Costello EJ, Rutter M. Precision, reliability and accuracy in the dating of symptom onsets in child and adolescent psychopathology. Journal of Child Psychology and Psychiatry. 1996;37:657–664. doi: 10.1111/j.1469-7610.1996.tb01457.x. [DOI] [PubMed] [Google Scholar]
- Agras WS, Telch CF, Arnow B, Eldredge K, Detzer MJ, Henderson J, et al. Does interpersonal therapy help patients with binge eating disorder who fail to respond to cognitive-behavioral therapy? Journal of Consulting and Clinical Psychology. 1995;63(3):356–360. doi: 10.1037//0022-006x.63.3.356. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Washington, DC: Author; 2000. Diagnostic and statistical manual of mental disorders DSM-IV-TR. [Google Scholar]
- Bradburn NM. Temporal representation and event dating. In: Stone AA, Turkkan JS, Bachrach CA, Jobe JB, Kurtzman HS, Cain VS, editors. The science of self-report. Mahwah, NJ: Erlbaum; 2000. pp. 49–61. [Google Scholar]
- Bradburn NM, Rips LJ, Shevell SK. Answering autobiographical questions: The impact of memory and inference on survey responses. Science. 1987;236:157–161. doi: 10.1126/science.3563494. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience: A reappraisal of retrospective reports. Psychological Bulletin. 1993;113(1):82–98. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- Brugman E, Meulmeester JF, Spee-van der Wekke A, Beuker RJ, Zaadstra BM, Radder JJ, et al. Dieting, weight and health in adolescents in The Netherlands. International Journal of Obesity Related Metabolic Disorders. 1997;21(1):54–60. doi: 10.1038/sj.ijo.0800363. [DOI] [PubMed] [Google Scholar]
- Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the Eating Disorder Examination with children: A pilot study. International Journal of Eating Disorders. 1996;19(4):391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Decaluwe V, Braet C. Prevalence of binge-eating disorder in obese children and adolescents seeking weight-loss treatment. International Journal of Obesity Related Metabolic Disorders. 2003;27(3):404–409. doi: 10.1038/sj.ijo.0802233. [DOI] [PubMed] [Google Scholar]
- Fairburn C, Doll H, Welch S, Hay P, Davies B, O’Connor M. Risk factors for binge eating disorder: A community-based, case-control study. Archives of General Psychiatry. 1998;55(5):425–432. doi: 10.1001/archpsyc.55.5.425. [DOI] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive-behavioral therapy for bulimia nervosa. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity: A comprehensive handbook. 2nd ed. New York: Guilford Press; 2002. pp. 302–307. [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment and treatment. 12th ed. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Fairburn CG, Cooper Z, Doll HA, Welch SL. Risk factors for anorexia nervosa: Three integrated case-control comparisons. Archives of General Psychiatry. 1999;56(5):468–476. doi: 10.1001/archpsyc.56.5.468. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Welch SL, Doll HA, Davies BA, O’Connor ME. Risk factors for bulimia nervosa. A community-based case-control study. Archives of General Psychiatry. 1997;54(6):509–517. doi: 10.1001/archpsyc.1997.01830180015003. [DOI] [PubMed] [Google Scholar]
- Feng N, Adler-Wailes D, Elberg J, Chin JY, Fallon E, Carr A, et al. Sequence variants of the POMC gene and their associations with body composition in children. Obesity Research. 2003;11(5):619–624. doi: 10.1038/oby.2003.89. [DOI] [PubMed] [Google Scholar]
- Field AE, Camargo CA, Taylor CB, Berkey CS, Colditz GA. Relation of peer and media influences to the development of purging behaviors among preadolescent and adolescent girls. Archives of Pediatric and Adolescent Medicine. 1999;153:1184–1189. doi: 10.1001/archpedi.153.11.1184. [DOI] [PubMed] [Google Scholar]
- Field AE, Austin SB, Taylor CB, Malspeis S, Rosner B, Rockett HR, Gillman MW, Colditz GA. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112:900–906. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- Figueroa-Colon R, Mayo MS, Treuth MS, Aldridge RA, Weinsier RL. Reproducibility of dual-energy X-ray absorptiometry measurements in prepubertal girls. Obesity Research. 1998;6:262–267. doi: 10.1002/j.1550-8528.1998.tb00348.x. [DOI] [PubMed] [Google Scholar]
- Frampton I. Unpublished clinical doctoral dissertation. England, Bristol: University of Bristol; 1996. Are overvalued ideas about weight and shape overvalued ideas in the diagnosis of eating disorder? Evidence from early onset anorexia nervosa. [Google Scholar]
- French SA, Perry CL, Leon GR, Fulkerson JA. Dieting behaviors and weight change history in female adolescents. Health Psychology. 1995;14(6):548–555. doi: 10.1037//0278-6133.14.6.548. [DOI] [PubMed] [Google Scholar]
- Frisancho AR. Ann Arbor, MI: The University of Michigan Press; 1990. Anthropometric standards for the assessment of growth and nutritional status. [Google Scholar]
- Grilo CM, Masheb RM. Onset of dieting versus binge eating in outpatients with binge eating disorder. International Journal of Obesity Related Metabolic Disorders. 2000;24(4):404–409. doi: 10.1038/sj.ijo.0801171. [DOI] [PubMed] [Google Scholar]
- Hill AJ, Draper E, Stack J. A weight on children’s minds: Body shape dissatisfactions at 9-years old. International Journal of Obesity Related Metabolic Disorders. 1994;18(6):383–389. [PubMed] [Google Scholar]
- Hill AJ, Oliver S, Rogers PJ. Eating in the adult world: The rise of dieting in childhood and adolescence. British Journal of Clinical Psychology. 1992;31(Pt 1):95–105. doi: 10.1111/j.2044-8260.1992.tb00973.x. [DOI] [PubMed] [Google Scholar]
- Hill AJ, Pallin V. Dieting awareness and low self-worth: Related issues in 8-year-old girls. International Journal of Eating Disorders. 1998;24(4):405–413. doi: 10.1002/(sici)1098-108x(199812)24:4<405::aid-eat7>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, et al. Weight concerns influence the development of eating disorders: A 4-year prospective study. Journal of Consulting and Clinical Psychology. 1996;64(5):936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel KF, Hammer LD, et al. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: A three-year prospective analysis. International Journal of Eating Disorders. 1994;16(3):227–238. doi: 10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory. 1982 Unpublished manuscript. [Google Scholar]
- Leon GR, Fulkerson JA, Perry CL, Keel PK, Klump KL. Three to four year prospective evaluation of personality and behavioral risk factors for later disordered eating in adolescent girls and boys. Journal of Youth and Adolescence. 1999;28:181–196. [Google Scholar]
- Marcus MD, Moulton MM, Greeno CG. Binge eating onset in obese patients with binge eating disorder. Addict Behaviors. 1995;20(6):747–755. doi: 10.1016/0306-4603(95)00104-2. [DOI] [PubMed] [Google Scholar]
- Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Archives of Disorders of Childhood. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Archives of Disorders of Childhood. 1970;45:13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight Investigators. Risk factors for the onset of eating disorders in adolescent girls: Results of the McKnight longitudinal risk factor study. American Journal of Psychiatry. 2003;160(2):248–254. doi: 10.1176/ajp.160.2.248. [DOI] [PubMed] [Google Scholar]
- Morgan C, Yanovski S, Nguyen T, McDuffie J, Sebring N, Jorge M, et al. Loss of control over eating, adiposity, and psychopathology in overweight children. International Journal of Eating Disorders. 2002;31(4):430–441. doi: 10.1002/eat.10038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. Journal of the American Medical Association. 2002;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- Patton GC, Carlin JB, Shao Q, Hibbert ME, Rosier M, Selzer R, et al. Adolescent dieting: Healthy weight control or borderline eating disorder? Journal of Child Psychology and Psychiatry. 1997;38(3):299–306. doi: 10.1111/j.1469-7610.1997.tb01514.x. [DOI] [PubMed] [Google Scholar]
- Patton GC, Johnson-Sabine E, Wood K, Mann AH, Wakeling A. Abnormal eating attitudes in London schoolgirls—a prospective epidemiological study: Outcome at twelve month follow-up. Psychological Medicine. 1990;20:383–394. doi: 10.1017/s0033291700017700. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Dieting and binging. A causal analysis. American Psychologist. 1985;40(2):193–201. doi: 10.1037//0003-066x.40.2.193. [DOI] [PubMed] [Google Scholar]
- Safer DL, Lively TJ, Telch CF, Agras WS. Predictors of relapse following successful dialectical behavior therapy for binge eating disorder. International Journal of Eating Disorders. 2002;32(2):155–163. doi: 10.1002/eat.10080. [DOI] [PubMed] [Google Scholar]
- Santonastaso P, Friederici S, Favaro A. Full and partial syndromes in eating disorders: A 1-year prospective study of risk factors among female students. Psychopathology. 1999;32(1):50–56. doi: 10.1159/000029067. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Edwards CD, Lushene RE, Montuori J, Platzek D. Palo Alto, CA: Consulting Psychologist Press; 1973. STAIC preliminary manual. [Google Scholar]
- Spurrell EB, Wilfley DE, Tanofsky MB, Brownell KD. Age of onset for binge eating: Are there different pathways to binge eating? International Journal of Eating Disorders. 1997;21(1):55–65. doi: 10.1002/(sici)1098-108x(199701)21:1<55::aid-eat7>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Stice E, Agras WS. Predicting onset and cessation of bulimic behaviors during adolescence: A longitudinal grouping analysis. Behavior Therapy. 1999;29:257–276. [Google Scholar]
- Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. Journal of Consulting and Clinical Psychology. 1999;67:967–974. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychology. 2002;21(2):131–138. [PubMed] [Google Scholar]
- Story M, Neumark-Sztainer D. Diet and adolescent behavior: Is there a relationship? Adolescent Medicine. 1998;9(2):283–298. [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Morgan CM, Yanovski SZ, Marmarosh C, Wilfley DE, Yanovski JA. Comparison of assessments of children’s eating-disordered behaviors by interview and questionnaire. International Journal of Eating Disorders. 2003;33(2):213–224. doi: 10.1002/eat.10128. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating disordered behaviors, body fat, and psychopathology in overweight and normal weight children. Journal of Consulting and Clinical Psychology. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogeltanz-Holm ND, Wonderlich SA, Lewis BA, Wilsnack SC, Harris TR, Wilsnack RW, Kristjanson AF. Longitudinal predictors of binge eating, intense dieting, and weight concerns in a national sample of women. Behavior Therapy. 2000;31:221–235. [Google Scholar]
- Wilfley DE, Pike KM, Striegel-Moore RH. Toward an integrated model of risk for binge eating disorder. Journal of Gender, Culture, and Health. 1997;2:1–3. [Google Scholar]
- Wilfley DE, Saelens BE, Stein RI, Mockus DS, Welch RR, Matt GE. Prediction of treatment outcome of group interpersonal and group cognitive-behavioral psychotherapy for overweight individuals with binge eating disorder. 2000 unpublished manuscript. [Google Scholar]