Abstract
As individuals who abuse methamphetamine (MA) often exhibit socially maladaptive behaviors such as violence and aggression, it is possible that they respond abnormally to social cues. To investigate this issue, we exposed 12 MA-dependent participants (abstinent 5-16 days) and 12 healthy comparison participants to fearful and angry faces while they performed an affect matching task during functional magnetic resonance imaging (fMRI). Although the groups did not differ in task performance, the healthy participants showed more task-related activity than the MA-dependent participants in a set of cortical regions consisting of the ventrolateral prefrontal cortex (VLPFC), temporoparietal junction (TPJ), anterior and posterior temporal cortex, and fusiform gyrus in the right hemisphere, and the cuneus in the left hemisphere. In contrast, the MA-dependent participants showed more task-related activity than the healthy participants in the dorsal anterior cingulate cortex (dACC). As expected, the task elicited activation of the amygdala in both groups; however, contrary to expectation, we found no difference between groups in this activation. Dorsal ACC hyperactivity, along with high self-ratings of hostility and interpersonal sensitivity in the MA-dependent group, suggest a hyper-sensitivity to socially threatening cues in the MA-dependent participants, while lower VLPFC activation could point to a deficit in integrating socio-emotional information and/or regulating this limbic hyperactivity. Additional activation differences in neural circuitry related to social cognition (TPJ, anterior, and posterior temporal cortex) suggest further socio-emotional deficits. Together, the results point to cortical abnormalities that could underlie the socially inappropriate behaviors often shown by individuals who abuse MA.
Keywords: methamphetamine, fMRI, faces, emotion regulation, social cognition
1. Introduction
Individuals who abuse methamphetamine (MA) often show evidence of socio-emotional disturbances during early abstinence, ranging from mood disturbances such as depression and anxiety during the first week of abstinence (London et al., 2004; Newton et al., 2004) to socially salient symptoms such as irritability and uncontrolled anger (Zweben et al., 2004). A combination of these negative mood states and socially maladaptive behaviors likely contributes to hostility, unmotivated interpersonal violence, and aggressive behavior, reported by individuals who currently abuse MA (Hall et al., 1996; Cohen et al., 2003) or previously were MA-dependent (Sekine et al., 2006). These behaviors are also observed in communities (for review, see Cretzmeyer et al., 2003; Maxwell, 2005), where MA abuse is associated with high rates of assault, weapons charges (Zweben et al., 2004), trauma center visits for physical attacks and intentional injuries (Tominaga et al., 2004; Zweben et al., 2004), and death from homicidal violence (Logan et al., 1998). As MA-dependent individuals are highly vulnerable to relapse during the early phases of abstinence (Huber et al., 1997), and negative mood states and antisocial behaviors can contribute to stress that may ultimately increase the risk of relapse (Shaham et al., 2000), investigation of the socio-emotional factors influencing behavior during this time, and of the neural systems underlying them, could help clarify potential relapse mechanisms.
Research on emotion regulation has converged on a set of brain regions that includes the prefrontal cortex (PFC), in particular orbital and ventrolateral regions (Blair, 2001), the anterior cingulate cortex (ACC), and the amygdala (see Davidson et al., 2000, for review). The model proposed by Davidson et al. (2000) suggests that dysfunction in any of these regions, or the connections between them, can lead to poor emotion regulation and increased propensity for impulsive aggression and violence, and neurocognitive models of reactive aggression in psychopathy corroborate this view (Blair, 2005). The descriptions of impulsive aggression in these models are reminiscent of the behavior of MA-dependent individuals in early abstinence, and indeed MA-abusing individuals exhibit structural and metabolic abnormalities in each of these regions when compared to healthy individuals.
Much of the relevant research involving PFC has focused on neurochemical deficits, such as lower serotonin concentration in postmortem tissue from individuals who had been current abusers of MA (Wilson et al., 1996), and deficits in currently abstinent MA-dependent individuals, including lower serotonin transporter (SERT) and dopamine transporter (DAT) binding (Sekine et al., 2003, 2006; 7 days – 5 years since last MA administration), lower white-matter markers for neuronal integrity and higher grey-matter markers for gliosis (Ernst et al., 2000; median time of abstinence = 4.25 months), and volumetric deficits (Thompson et al., 2004; within the first two weeks of abstinence). Functional neuroimaging studies of currently abstinent individuals have also begun to relate dysregulated regional cerebral glucose metabolism (rCMRglc) in PFC to mood and psychiatric symptoms (Volkow et al., 2001; London et al., 2004), and lower task-related activation to impaired decision-making after 6 – 46 days of sobriety (Paulus et al., 2002), suggesting that the structural deficits are functionally significant.
In limbic regions, low markers for neuronal integrity have been observed in the ACC of individuals abstinent 4 – 13 weeks (Nordahl et al., 2002), as well as low relative rCMRglc (London et al., 2004), and low grey-matter concentration in the first week of abstinence (Thompson et al., 2004), with the loci of dysregulated rCMRglc and grey-matter deficits overlapping in dorsal and subgenual portions. In addition, lower DAT and SERT binding (Sekine et al., 2003, 2006), and higher relative rCMRglc (London et al., 2004) were observed in the amygdala in recently abstinent MA-dependent individuals compared to healthy individuals.
Together, these abnormalities have been linked to MA-related behavioral problems during early abstinence, such as reduced harm avoidance (Goldstein et al., 2002), psychiatric symptoms (Sekine et al., 2001), aggressive symptoms (Sekine et al., 2006), mood disturbances (London et al., 2004), and poor decision-making (Paulus et al., 2002), and could represent the neural basis for the socially problematic behaviors described above. However, the nature of the functional deficits leading to socio-emotional disturbances in MA-dependent individuals has not been directly assessed.
The present study used a task containing stimuli with socio-emotional relevance – negative facial expressions – to probe the functional integrity of brain regions associated with socio-emotional processing in MA-dependent individuals. The task exposed MA-dependent and healthy participants to fearful and angry faces while they underwent functional magnetic resonance imaging (fMRI). In healthy individuals, processing of facial expressions is subserved by neural circuits that include those outlined by Davidson et al., 2000 (PFC, ACC, and amygdala), as well as regions involved in visual processing of faces and social cognition, such as the fusiform gyrus, parietal regions, and temporal regions (Haxby et al., 1996, 2002; Kesler-West et al., 2001; Keightley et al., 2003). Given the structural and metabolic abnormalities in relevant regions in MA-dependent individuals, the present study was expected to uncover task-related functional differences between MA-dependent and healthy individuals in these brain regions. Specifically, we expected limbic regions involved in emotional reactivity (e.g., ACC, amygdala) to be hyper-responsive in MA-dependent compared to healthy individuals, and prefrontal systems involved in planning and control of emotional reactivity to be less reactive. In addition, we expected measures of socially relevant behaviors, such as aggression and sensitivity to social distress, to relate to these differences in neural function.
2. Method
2.1 Participants
Twenty-four volunteers participated in the study. All participants were recruited via newspaper and Internet advertisements. After receiving a detailed description of the protocol, they provided written informed consent, following the guidelines of the UCLA Office for Protection of Research Subjects.
Twelve participants (5 female, 10 tobacco smokers, 33.75 ± 7.61 years old) were MA-dependent and not currently seeking treatment. They reported MA use of 4.60 ± 7.58 g per week (range = 0.5 - 28 g/wk). The remaining 12 participants (3 female, 9 tobacco smokers, 32.17 ± 9.27 years old) had no history of abuse of any illicit drugs, except for possible light use (≤ 1 joint per week) of marijuana; these participants comprised the healthy comparison group. Although the groups differed in years of education, with the healthy participants having on average 15.58 ± 1.98 years of education and the MA-dependent group 13 ± 1.65 years (t(22) = 3.48, p < .05), they did not differ significantly in age (t(22) < .5), gender composition (X2(1) < 1,), employment status (unemployed/full-time/part-time) (X2(2) = 4.44), income (t(22) < 1), or estimated IQ from the Shipley Institute of Living Scale (Shipley, 1940) (t(19) = 1.93), all p > .05.
Inclusion criteria for MA-dependent participants included a diagnosis of MA dependence, as assessed by the Structured Clinical Inventory for DSM-IV (SCID-I) (First, 1996), self-reports of spending at least $100 on MA over the 30 days before enrollment in the study, and recent MA use, confirmed by a positive urine test for MA metabolites on admission. The MA-dependent participants resided at the UCLA General Clinical Research Center (GCRC) for 5-14 days (average 7.17 ± 2.5 days) before scanning. Abstinence from MA and other drugs of abuse (besides nicotine) during the course of the study was confirmed by urine drug screens every other day. Thus, at the time of scanning, participants had been MA-abstinent for 5-16 days (average 8.6 ± 3.5 days). The healthy comparison participants were also tested via urine screen for drug use prior to scanning, but did not reside at the GCRC.
Once the participants provided informed consent, a physical examination was performed and a medical history taken, including collection of samples for standard blood chemistry and hematology profiles. All participants had values within normal limits for hematocrit, plasma electrolytes, and markers for hepatic and renal function. Exclusion criteria following the examination included the use of medications that affect the central nervous system, cardiovascular, pulmonary or systemic disease, claustrophobia, pregnancy, and seropositive status for HIV.
Psychiatric diagnoses were established using the DSM-IV, with diagnoses for Axis I disorders determined using the SCID-I, and personality disorders evaluated using the SCID II (version 1) (First, 1997). A current Axis I diagnosis other than nicotine dependence, and MA dependence for the MA-dependent group, was exclusionary. Although none of the participants had current exclusionary Axis I diagnoses, three of the MA-dependent participants had a history of depressive episodes, and one MA-dependent participant had a history of anxiety disorder. None of the healthy participants had any histories of mood disorders, and none of the 24 participants met criteria for antisocial personality disorder, as assessed via the SCID II.
For both groups, light use of alcohol was allowed (< 7.5 drinks per week). All participants were right-handed, as determined by the Edinburgh Handedness Inventory (Oldfield, 1971).
2.2 Tasks
2.2.1 Task paired with fMRI
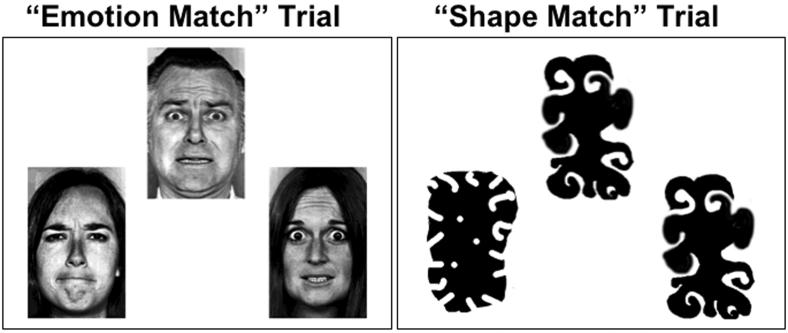
While undergoing fMRI, participants performed a visual matching task, adapted from Hariri et al. (2000), consisting of two types of trials: matching of emotional facial expressions (“Emotion Match” trials), and matching of irregular shapes (“Shape Match” trials) (Figure 1). During Emotion Match trials, the stimuli were images of faces, selected from the Ekman and Friesen face set (Ekman and Friesen, 1976). Only faces classified as having fearful, angry, or neutral expressions were displayed, with the target expression (described below) always being fear or anger. During Shape Match trials, the items were irregular black blobs. The conditions were named on the basis of the content of the stimuli, not the type of processing required; Emotion Match trials could evoke social as well as emotional processes, which could not be separated. The task can therefore be considered to tap social, emotional, or both processes.
Figure 1. Representative Emotion Match and Shape Match trials.
Target items are at the top of each display, and choice items at the bottom. In the Emotion Match trial (left panel), the target face and the choice face on the right both express fear, and are therefore a correct match. The choice face on the left expresses anger, and is therefore an incorrect match. In the Shape Match trial (right panel), the correct choice is the item on the right, as it corresponds in shape to the target item.
In each trial, the task for the participant was to match a target stimulus to one of two choice stimuli. Each trial began with the presentation of a target item centered in the upper portion of the visual field, and two choice items (one matching the target) presented in the lower right and left portion of the visual field. These items remained on the screen for 5 sec, after which the word “Respond” appeared next to the target item. The appearance of the word “Respond” was the cue for the participant to indicate which of the two choice items matched the target.
During Emotion Match trials, the task was to identify the choice face with an emotional expression that matched that on the target face. The person pictured in the target face was always different in identity from either of the individuals comprising the choice faces. During Shape Match trials, participants matched the items on the basis of shape.
Participants indicated their choice on a keypad in their right hand. A press with the index finger indicated the left choice item, while pressing with the middle finger indicated the right choice item. The participant's choice was displayed by an arrow pointing to the chosen item, but no feedback regarding accuracy was provided. Regardless of response time, the items and response cue remained on the screen for 2 sec after the response cue appeared. Finally, the display was cleared for a 1-sec inter-trial interval, for a total trial length of 8 sec.
Stimuli were delivered in a semi-block design, consisting of three trials per block, so that each block was 24 sec long. For each participant, the order of the blocks was chosen randomly from one of four pseudorandom orders. Participants completed two runs of the task, with each run consisting of 6 blocks of each type of trial (12 blocks/run total). Total scan length was therefore 9 min 36 sec, with an additional ∼1 min rest between runs. All participants but one experienced two identical runs, with the same block order in each; one participant completed two runs in which the block orders were different.
2.2.2 Out-of-scanner assessment
All participants completed a behavioral assessment on the day of admission to the study, including the Symptom Checklist 90 (SCL-90-R) (Derogatis et al., 1973) and Brief Symptom Inventory (BSI) (Derogatis and Melisaratos, 1983). Both of these questionnaires ask participants to self-report the severity of psychological symptoms experienced over the past 7 days (SCL-90-R) or 30 days (BSI), from a rating of 0 (“not at all”) to 4 (“extremely”). Symptom dimensions include somatization, obsessive-compulsive symptoms, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Due to the social nature of the hostility and interpersonal-sensitivity subscales, and their ability to quantitatively characterize the everyday social and aggressive behaviors of the participants outside of the fMRI setting, scores for these subscales were used for further analysis.
Participants also completed the Beck Depression Inventory (BDI; Beck et al., 1961), a self-rating questionnaire that assesses current depressive symptoms on a scale from 0 to 63, on the day of intake. Eight MA-dependent participants completed the BDI a second time, either on, or within 3 days of, the day of scanning. Nine MA-dependent participants also completed a MA withdrawal questionnaire (MAWQ) on the day of intake, as well as on, or within 3 days of, the day of scanning. The MAWQ includes an item for symptoms of fatigue, for which participants rated how tired they felt on a scale from 0 (“absent”) to 3 (“severe”).
2.3 MR Parameters
2.3.1 Stimulus parameters
Stimuli were presented to participants via a set of magnet-compatible VGA goggles (Resonance Technology, Northridge, CA). These goggles have a field of view of approximately 20° vertically and 30° horizontally, and display computer images at 800×600 pixel resolution. Responses were registered using a magnet-compatible two-button button box.
2.3.2 Scan parameters
All scanning was performed on a 3T head-only MRI device (Siemens Allegra; Erlangen, Germany). The scanning session included acquisition of a set of T2-weighted high-resolution echo-planar anatomical images covering the entire brain volume, which was used for spatial alignment. Functional images were acquired using a gradient-echo EPI sequence (45 slices, 2 mm thick/0.5 mm skip, pixels 3.125 mm2, TR/TE 2500/28 ms). For 17 participants, the slices were angled at approximately 30° toward coronal from the AC-PC line. For the remaining participants, slices were acquired parallel to the AC-PC line. Two identical functional runs, each with 115 volumes, were performed in sequence.
2.4 Data analysis
2.4.1 Task paired with fMRI
Response data were discarded for two participants in the MA-dependent group and one participant in the healthy group due to poor accuracy on shape match trials, indicating problems registering responses on the button box. Response accuracy and reaction time were analyzed using one-way repeated-measures ANOVAs with group (MA-dependent and Healthy) and trial type (Emotion Match and Shape Match) as factors.
2.4.2 fMRI image analysis
All analyses were performed using SPM2 (Wellcome Department of Imaging Neuroscience, London), with the exception of spatial normalization, which was performed using the FSL software package (FMRIB Group, Oxford). First, all functional scans were spatially aligned to the first image of the series to correct for motion. Of the 48 scans acquired (2 per participant, 12 participants per group), one showed movement of >2.5 mm (the thickness of one slice) and was excluded from further analysis for this reason. The remaining images were then normalized to a standard spatial template and smoothed using a 10 mm full-width at half-maximum (FWHM) Gaussian kernel.
Functional data were analyzed using the general linear model. Each participant's functional images were entered into a random effects model, using two box-car functions as regressors: one for Emotion Match blocks and one for Shape Match blocks (each boxcar had a length of 24 sec). Regressors were convolved with a canonical hemodynamic response function (HRF) provided by SPM2 in order to approximate a physiologically accurate blood flow response against which to regress the signal timecourse (Friston et al., 1994). The GLM was applied at each voxel, and parameters estimated on a per-voxel basis.
The resulting statistical maps were then entered into a second-level random effects ANOVA combining all single-subject data for each group, and t-tests were performed to assess differences within and between groups. Results were assessed at a statistical threshold of p < .005 (uncorrected) with a cluster extent of 10 contiguous voxels (Forman et al., 1995).
Region of interest (ROI) analyses were performed using the MarsBaR toolbox (Brett et al., 2002). Anatomical images of bilateral amygdalae served as a priori ROIs, while the remaining ROIs were functional clusters identified in the random effects analyses. BOLD signal change values were extracted at each voxel in an ROI, averaged across all voxels in the ROI image, and analyzed using SPSS 11 (Chicago, IL).
2.4.3 Out-of-scanner assessment
Due to the skewed distribution of SCL-90 and BSI scores across participants, raw scores for the Hostility (HOS) and Interpersonal Sensitivity (I-S) subscales were analyzed using nonparametric methods (Mann-Whitney U). BDI and MAWQ scores were analyzed using two-sample t-tests to test for differences between groups, and paired t-tests to test for differences between study days.
3. Results
3.1 Participants
On the day of intake, the MA-dependent participants had significantly higher scores on the BDI (mean score = 10.92 ± 10.08) than the healthy participants (mean score = 2.33 ± 2.87; t(22) = 2.84, p < 05). However, on the day of scanning, BDI scores had decreased significantly in the MA-dependent participants (mean score = 4.44 ± 4.88; t(8) = 2.45, p < .05), so that scores were no different from scores of the healthy participants on intake (t(19) = 1.25, p > .05). In addition, scores for the fatigue item on the MAWQ showed a significant decrease between the day of intake (mean score = 1.63 ± 1.30) and the day of scanning (mean score = 0.5 ± .76; t(7) = 3.21, p < .05). These results indicate that the fatigue and depressive symptoms associated with early abstinence from MA (Newton et al., 2004) had resolved by the time of testing.
3.2 Task paired with fMRI
The healthy participants responded to Emotion Match trials with a mean accuracy of 91.9% (SEM = 2.79) and reaction time (RT) of 495.45 msec (SEM = 26.62), and Shape Match trials with a mean accuracy of 99.5% (SEM = .45) and RT of 490.04 msec (SEM = 35.55). The MA-dependent participants responded to Emotion Match trials with a mean accuracy of 90.1% (SEM = 2.93) and RT of 577.25 msec (SEM = 27.91), and Shape Match trials with a mean accuracy of 99.4% (SEM = .47) and RT of 542.63 msec (SEM = 37.29). Accuracy did not differ significantly between groups (p > .5), and although there was a significant effect of trial type (F(1) = 17.8, p < .05), there was no Group * Trial Type interaction (p > .5). RT showed no effect of group, trial type, or Group * Trial Type interaction (all p > .1).
3.3 Imaging results
Within-group one-sample t-tests of Emotion Match > Shape Match contrasts revealed similar patterns of task-related activity in the two groups (Table 1), with healthy and MA-dependent participants showing activation of left amygdala, bilateral ventrolateral and dorsolateral prefrontal cortex (inferior and middle frontal gyri), dorsomedial and precentral frontal regions, parietal cortex including the precuneus, and occipital regions including the cuneus and lingual gyrus. In addition to these effects that were common to the two groups, participants in the healthy group showed significant activation of the right amygdala, right precentral gyrus, and left middle/superior temporal gyri; MA-dependent participants additionally showed significant activation of bilateral parahippocampal gyri, left thalamic regions bordering the putamen, bilateral occipitotemporal regions, and cerebellum.
Regions showing task-related activity during Emotion Match relative to Shape Match trials: Within-groups analysis.
| Healthy Group |
MA-dependent Group |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Region | BA | MNI coordinates |
t | cluster size |
BA | MNI coordinates |
t | cluster size |
||||
| x | y | z | x | y | z | |||||||
| Both Groups | ||||||||||||
| L amygdala | −22 | −4 | −18 | 3.98 | 79 | −22 | −6 | −16 | 3.94 | 41 | ||
| R IFG/MFG | 9, 47 | 44 | 4 | 26 | 8.36 | 2368 | 46/47 | 28 | 28 | −6 | 10 | 2483 |
| 10 | 38 | 50 | 0 | 3.6 | 21 | |||||||
| L IFG/MFG | 47/46/45/10/9 | −46 | 46 | −6 | 6.56 | 1891 | 9/6/46 | −56 | 22 | 28 | 12.6 | 4653 |
| L MFG/precentral gyrus |
6 | −38 | −4 | 50 | 3.82 | 32 | ||||||
| medial PFC | 8 | 0 | 28 | 46 | 3.34 | 20 | 8,6,9 | −6 | 18 | 46 | 8.53 | 759 |
| 32 | −8 | 12 | 46 | 3.35 | 11 | |||||||
| R cuneus/precuneus/ lingual gyrus |
19/18 | 42 | −42 | 24 | 8.66 | 3858 | 7/40/18 | 32 | −58 | 44 | 6.66 | 1042 |
| 19 | 50 | −74 | 2 | 4.18 | 80 | 19 | 16 | −64 | −6 | 4.1 | 49 | |
| L cuneus/precuneus/ lingual gyrus |
19 | −28 | −68 | 40 | 6.42 | 811 | 7 | −8 | −70 | 40 | 9.23 | 2264 |
| 19/18 | −20 | −100 | 18 | 4.36 | 229 | |||||||
| 19/18 | 2 | −76 | −4 | 8.46 | 737 | |||||||
| Healthy Group Only | ||||||||||||
| R amygdala | 22 | −4 | −16 | 4.3 | 52 | |||||||
| R MFG/precentral gyrus |
6 | 40 | −4 | 50 | 3.76 | 118 | ||||||
| L MTG | 21 | −48 | −46 | 8 | 4.9 | 22 | ||||||
| L STG | 22 | 62 | −50 | 14 | 3.9 | 83 | ||||||
| MA Group Only | ||||||||||||
| L PHG | 27 | −22 | −30 | −4 | 4.9 | 303 | ||||||
| R PHG | 27 | 18 | −24 | −10 | 3.92 | 30 | ||||||
| 28 | 18 | −14 | −10 | 3.5 | 14 | |||||||
| L thalamus/putamen | −16 | −10 | 4 | 4.03 | 66 | |||||||
| L occipitotemporal cortex | 39/37 | −58 | −52 | 8 | 6.99 | 319 | ||||||
| R occipitotemporal cortex |
37 | 38 | −50 | −22 | 4.97 | 361 | ||||||
| L cerebellum | −42 | −46 | −26 | 11.6 | 227 | |||||||
Note: MNI coordinates are of peak voxel in cluster. BA = Brodmann Area; L = left; R = right; IFG = inferior frontal gyrus; MFG = middle frontal gyrus; PFC = prefrontal cortex; MTG = middle temporal gyrus; STG = superior temporal gyrus; PHG = parahippocampal gyrus.
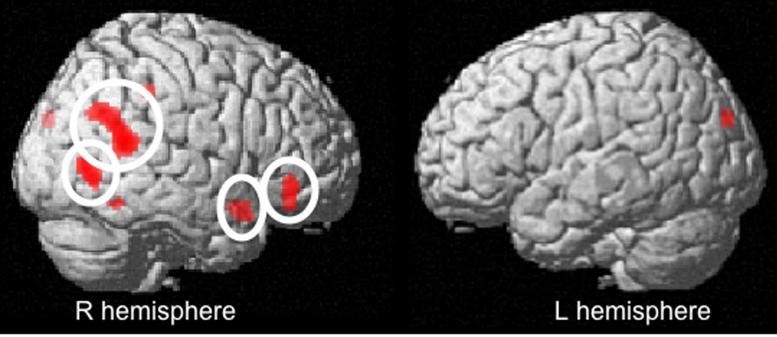
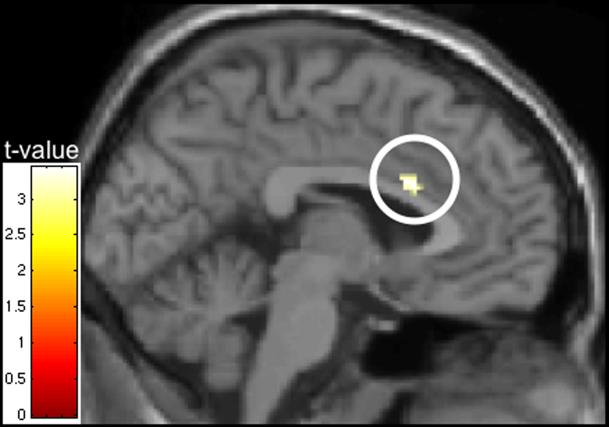
Between-groups two-sample t-tests of the Emotion Match > Shape Match contrasts revealed a set of cortical regions in which the healthy comparison participants showed more activity than the MA-dependent participants (Table 2, Figure 2). These regions included right ventrolateral prefrontal cortex (RVLPFC), right temporoparietal junction (TPJ; consisting of posterior superior temporal gyrus, angular/supramarginal gyri, and inferior parietal lobule), right temporal pole (consisting of anterior inferior and middle temporal gyri), right fusiform gyrus, and left cuneus. Contrasting MA-dependent > healthy participants revealed only a single region of higher activity in the MA-dependent than the healthy participants: dorsal anterior cingulate cortex (dACC) (Table 2, Figure 3).
Regions showing task-related activity during Emotion Match relative to Shape Match trials: Between-groups analysis
| Region | BA | MNI coordinates |
t | cluster size |
||
|---|---|---|---|---|---|---|
| x | y | z | ||||
| Healthy > MA | ||||||
| R VLPFC | 47 | 48 | 38 | −6 | 3.6 | 81 |
| R ST/angular/supramarginal gyrus | 39/22 | 64 | −48 | 14 | 3.93 | 289 |
| R IPL/supramarginal gyrus | 40 | 42 | −36 | 38 | 2.97 | 26 |
| R STG | 38 | 40 | 10 | −20 | 2.9 | 67 |
| R ITG/MTG | 19/37 | 54 | −66 | −2 | 3.12 | 162 |
| R fusiform gyrus | 37 | 58 | −54 | −16 | 2.88 | 10 |
| L cuneus | 19 | −16 | −88 | 26 | 3.85 | 34 |
| MA > Healthy | ||||||
| Anterior cingulate cortex | 24 | −2 | 16 | 20 | 3.04 | 22 |
Note: MNI coordinates are of peak voxel in cluster. BA = Brodmann Area; L = left; R = right; VLPFC = ventrolateral prefrontal cortex; ST = superior temporal; IPL = inferior parietal lobule; STG = superior temporal gyrus; ITG = inferior temporal gyrus; MTG = middle temporal gyrus.
Figure 2. Healthy > MA Contrast.
Healthy participants (control) show greater task-related activity than MA-dependent participants during Emotion Match (relative to Shape Match) trials in a set of cortical regions consisting of right ventrolateral prefrontal cortex, anterior and posterior lateral temporal cortex, and temporoparietal junction (circled), as well as fusiform gyrus and left cuneus. Image thresholded at p < .005 with a 10-voxel cluster extent, and rendered on the SPM2 single-subject template.
Figure 3. MA > Healthy Contrast.
Dorsal ACC is the only region in which MA-abusing participants show more task-related activity than healthy (control) participants during Emotion Match (relative to Shape Match) trials. Image thresholded at p < .005 with a 10-voxel cluster extent, and overlaid on the SPM2 single-subject template.
Since the original hypotheses predicted differences in amygdala activation between groups, region-of-interest (ROI) analyses were performed in anatomically defined amygdala ROIs (traced in MNI space) applied to participants' individual Emotion Match > Shape Match contrast images. While bilateral amygdala activation (as indexed by the magnitude of parameter estimates for the Face > Shape Match contrast) tended to be lower in the MA-dependent participants than the healthy participants, this finding was not statistically significant (left amygdala: healthy group mean = .668, MA mean = .314, t(22) = 1.308, p = .164; right amygdala: healthy group mean = .475, MA mean = .165, t(22) = 1.207, p = .119) .
Given the involvement of RVLPFC and dACC in social threat processing and risk for aggression (Eisenberger et al., 2003, 2007), exploratory ROI analyses were performed in the RVLPFC and dACC clusters significant in the between-groups whole-brain contrasts. Parameter estimates were extracted and averaged across all voxels in the cluster as an indicator of signal change. Regression analysis was performed, modeling activity in the dACC as a function of activity in the RVLPFC, group, and the interaction between these two variables. Only study group was a significant predictor of dACC activity (t(20) = 2.17, p < .05).
3.4 Out-of-scanner assessment
Scores on the SCL-90 and BSI Hostility (HOS) and Interpersonal Sensitivity (I-S) subscales were skewed, such that most scores fell in a low range of 0-5, and a small number of scores fell in a very high range of up to 24. For this reason, parametric t-tests could not be performed to test for differences between groups. However, separating the data into those from participants with low scores (0-5) and those with high scores (>5), respectively, revealed that on all subscales, the low-scoring group contained all 12 of the healthy participants, and that the high-scoring group consisted of only MA-dependent participants (4 participants each for BSI HOS, BSI I-S, and SCL-90 HOS, and 6 participants for SCL-90 I-S). Mann-Whitney U tests revealed that mean rank tended to be higher in the MA-dependent than healthy comparison group, and the difference was statistically significant for the BSI I-S subscale (U = 34.0, p < .05). To test the relationship between scores on the subscales and regional brain activity during the Emotion Match task, Mann-Whitney U tests were performed, comparing ROI parameter estimates between low-scoring (0-5) and high-scoring (>5) individuals in the MA-dependent group (the test could not be performed on data from the healthy comparison group, since none of the participants were high-scoring). Results showed that mean rank for dACC activity was significantly higher in individuals with high scores on SCL-90 HOS, SCL-90 I-S, BSI HOS, and BSI I-S (all U = 4.0, all p < .05). The only other relationship that emerged between self-reports and regional brain activity was between SCL-90 I-S and RVLPFC, showing a trend towards lower rank for RVLPFC activation in MA-dependent individuals with high self-reports of interpersonal sensitivity (U = 7.0, p = .093). Although intriguing, these results were computed using small samples and yielded small or trend effects, and should therefore be considered preliminary.
4. Discussion
Matching emotional facial expressions produced task-related neural activity that is typical of facial affect processing in a group of MA-dependent participants in early abstinence, as well as a group of healthy comparison participants. Both groups exhibited activation in ventral temporal cortex, linked to face detection and recognition (Haxby et al., 1996; Kanwisher et al., 1997), amygdala, linked to emotional responsivity to threatening facial expressions (Adolphs et al., 1994, 2003; Morris et al., 1996), dorsomedial PFC, linked to the formation of mental representations about the internal states of others (Frith and Frith, 2001; Ochsner et al., 2004), and dorsolateral PFC and parietal cortex, which participate in cognitive and executive processes necessary for successful task performance (Kane and Engle, 2002).
Despite these similarities in activation patterns among groups, the two groups differed in activation of a number of cortical regions linked to affective and social cognitive processing. These differences did not stem from mood disorders in the MA-dependent sample, as volunteers with current psychiatric diagnoses were excluded from the study, and MA-dependent participants had recovered from abstinence-related depression and fatigue. Instead, activation differences are likely to reflect differences in processing of socio-emotional information.
The ventrolateral prefrontal cortex (VLPFC), which showed more task-related activity in the healthy than in the MA-dependent participants, has consistently been implicated in affect processing (Phan et al., 2002), in particular in relation to emotional facial expressions (Nakamura et al., 1999; Iidaka et al., 2001; Kesler-West et al., 2001; Keightley et al., 2003; Phillips et al., 2004; Ishai et al., 2005). VLPFC has been suggested to represent an endpoint for the distributed networks involved in emotion recognition, where the information contained in emotional faces can be integrated for further processing (Sprengelmeyer et al., 1998), or to participate in the semantic processing of this information (Hornak et al., 1996). The ability to effectively process or interpret socio-emotional information could therefore be compromised in MA-dependent individuals, owing to a functional deficit in this region.
Alternatively, VLPFC involvement has been associated with regulation of emotional -- particularly aggressive (Blair, 2005) -- impulses, with right VLPFC (RVLPFC) thought to exert top-down inhibitory control over limbic structures (Hariri et al., 2000; Eisenberger et al., 2003). RVLPFC projects to limbic regions of the brain (Carmichael and Price, 1995; Cavada et al., 2000; Vogt and Pandya, 1987), inhibiting amygdala reactivity during intentional (Ochsner et al., 2004) and unintentional (Lieberman et al., 2007) regulation of affect, as well as the anterior cingulate cortex during placebo analgesia (Lieberman et al., 2004) and regulation of social threat (Eisenberger et al., 2003). In addition, RVLPFC has been implicated in motor response inhibition (Ma et al., 2003; Eagle et al., 2004; Aron et al., 2004), and regulation of impulsively aggressive behaviors (Bufkin and Luttrell, 2005; Raine et al., 1998; Pietrini et al., 2000). Notably, chronic stimulant administration to animals, and stimulant abuse by humans, are associated with both deficits in inhibitory function (Jentsch et al., 2002; Goldstein & Volkow, 2002; Salo et al., 2005; Monterosso et al., 2005) and structural deficits in RVLPFC (Thompson et al., 2004). Although the current study was not designed to detect an inhibitory contribution of RVLPFC, future studies could determine whether the difference in task-related RVLPFC activation found here reflects a regulatory deficit over limbic structures (amygdala and/or dACC).
Of particular interest is the potential regulation of dACC, which was more active in the MA-dependent than healthy participants in the present study. Dorsal ACC plays a role in pain and distress (Rainville et al., 1997), including social distress (Eisenberger et al., 2003, 2007). In a study of social rejection (Eisenberger et al., 2003), healthy individuals who felt distressed by an exclusionary experience exhibited dACC activation; however, individuals who activated RVLPFC more during the social exclusion showed less activation in dACC and reported less social distress, suggesting that RVLPFC regulated the distress of socio-emotional threat. A later study (Eisenberger et al., 2007) found relationships between dACC reactivity during social exclusion, self-reports of social sensitivity and trait aggression, and genetic factors previously linked to aggressive behavior, further suggesting that dACC activation reflects social hyper-reactivity that can lead to aggressive behavior. The present findings parallel these results, as the MA-dependent participants showed higher dACC activation than the healthy participants, and behavioral measures hinted at higher interpersonal sensitivity. In addition, those individuals in the MA-dependent group who gave particularly high self-reports of hostility and interpersonal sensitivity showed the highest dACC activation, and those who had high interpersonal sensitivity scores tended to have the lowest RVLPFC activity. In light of these preliminary self-report findings, higher dACC and lower RVLPFC activity in the MA-dependent participants could point to a disruption in the system implicated in socio-emotional regulation (Eisenberger et al., 2003), indicating a potential mechanism underlying the mood disturbances and socially maladaptive behaviors often exhibited by MA-dependent individuals.
The remaining regions showing more task-related activity in the healthy participants than the MA-dependent participants – temporoparietal junction (TPJ), superior temporal sulcus (STS), and temporal pole – are often implicated in social cognition, particularly in understanding the motivations and emotional states of others (“theory of mind”) (Ochsner et al., 2004; Gallagher and Frith, 2003; Fletcher et al., 1995; Brunet et al., 2000). Theory of mind is thought to rely heavily on dorsomedial PFC (Frith and Frith, 2001), which was in fact active in both groups. However, it also involves mentally representing the internal states of others, and constructing a coherent model about their beliefs, which has been shown to depend on the integrity of the TPJ (Saxe et al., 2004; Vollm et al., 2006; Saxe and Kanwisher, 2003; Samson et al., 2004; Saxe and Wechsler, 2005). Our finding that MA-dependent participants activate these regions less than healthy participants suggests a functional impairment that could interrupt or impede the construction of such mental-state representations. The facial expression matching task is not commonly thought to engage theory of mind processing; however, these activation differences between groups could point to a spontaneous engagement of some social cognitive processes by the healthy participants that are impaired in the MA-dependent participants (although comparable dorsomedial PFC activations point to some theory of mind processing in both groups). This impairment in some aspects of social cognitive processing could, in turn, lead MA-dependent individuals to respond inappropriately to what others are expressing.
Contrary to expectation, we did not find reliable between-groups differences in amygdala activation during facial affect matching, despite previous findings that MA-dependent participants have abnormal glucose metabolism in this region (London et al., 2004). Although amygdala activation tended to be lower in the MA-dependent participants than the healthy participants during Emotion Match trials, this difference was not significant. It is possible that adequate amygdala responsivity to threatening facial expressions is preserved in MA-dependent individuals, consistent with the finding that some, but not all, functions of the amygdala are impaired in reactive aggression with psychopathy (Blair, 2005), and that it is perhaps amygdala downregulation, rather than activation, that is impacted in MA-dependent individuals. Contributing factors may also have included poor signal-to-noise ratio, as signal dropout can be a problem in acquisition of amygdala fMRI images, small sample size, or habituation to repeated and/or prolonged presentation of faces within each block (Wright et al., 2001; Fischer et al., 2003).
In sum, although the capacity to activate the amygdala in response to negative facial expressions appears equivalent in individuals who abuse MA and individuals who do not, differences exist in a set of cortical regions necessary for experiencing social threat (dACC), integrating and/or regulating emotional information (RVLPFC), and more general social cognitive functions (temporal regions and TPJ).
Behavioral performance differences between Emotion Match and Shape Match trials suggest that the two types of trials differed in difficulty, so that active regions in the Emotion Match > Shape Match contrast could reflect higher attentional or processing demands, independent of the effects of emotion. However, the results are highly consistent with the imaging literature focusing on facial affect. In addition, the contrasts of interest were between the two groups of participants, and as no effect of group, or group X trial type interaction were found in the behavioral data, potential differences in difficulty between the two trial types are expected to subtract out.
An alternative interpretation of the group differences in task-related brain activity could be simple strategy differences in performing the task. However, equivalent task accuracy, along with biochemical differences between groups in relevant regions, point to functional deficits in the MA-dependent group, rather than a voluntary strategy difference. An additional alternative interpretation is based on the fact that, as with most fMRI data, imaging data were analyzed using subtractive logic (statistical maps for Shape Match trials were subtracted from statistical maps for Emotion Match trials). Thus, observed differences are open to two interpretations, as group differences attributed to processing of faces could have in fact been due to differences in processing of shapes. It is, however, not likely to be the case, as, for example, there is no evidence to suggest that matching shapes would induce more limbic activity than processing emotional information, for which the limbic system is specialized. Similarly, greater activation in one group than the other could also reflect less de-activation. Moreover, interpretation of functionality of a region on the basis of BOLD signal change is inferential, so that a number of task-related (or unrelated) functions could have been supported by activation of a given region. For example, dACC is often thought of as important in cognitive control, and an emotion regulation region, and the link to socio-emotional threat inferred through previous findings (e.g., Eisenberger et al., 2003, 2007). Future research will need to address direct links between regions and their function in socio-emotional regulation by testing specific hypotheses in specific regions. Another potential source of group differences in brain activity is the psychiatric history of the MA-dependent sample, as some mood disorders have been associated with altered brain structure and function (e. g., Leppanen et al., 2004). While none of the participants had a current psychiatric diagnosis, three of the MA-dependent participants had histories of depressive episodes, and one had a history of anxiety disorder. These histories did not appear to impact the results of the present sample, however, as removal of the participants from the whole-brain random effects analysis did not qualitatively change the results. Finally, the relatively small number of Emotion Match trials, relatively limited sample size of 12 per group, and relatively liberal threshold of p < .005 suggest an increased possibility for Type I and Type II errors to occur. While use of a blocked design and inclusion of a cluster-size threshold of 10 contiguous voxels (which helps protect against false positives (Forman et al., 1995) and has been used in previous studies (Eisenberger et al., 2003; Lieberman et al., 2004)) can partly alleviate these concerns, the limitations should be borne in mind when considering the present results.
Despite these caveats, the present study identifies functional differences between MA-dependent and healthy comparison participants in brain regions linked to emotion integration and/or cognitive control, social threat perception, and social cognition, and is the first to do so in the context of responsivity to facial expressions. Such deficits may lead to inappropriate socio-emotional behaviors associated with MA use, potentially contributing to states of stress and increased risk of relapse.
Acknowledgements
Research was supported by NIH grants R01 DA 020726 (EDL), R01 DA 15179 (EDL), P20 DA 022539 (EDL), and MOI RR 00865 (UCLA GCRC). DEP was supported in part by T32 MH 015795.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adolphs R. Is the human amygdala specialized for processing social information? Ann. N. Y. Acad. Sci. 2003;985:326–340. doi: 10.1111/j.1749-6632.2003.tb07091.x. [DOI] [PubMed] [Google Scholar]
- Adolphs R, Tranel D, Damasio H, Damasio AR. Impaired recognition of emotion in facial expressions following bilateral damage to the human amygdala. Nature. 1994;372:613–614. doi: 10.1038/372669a0. [DOI] [PubMed] [Google Scholar]
- Aron AR, Robbins TW, Poldrack RA. Inhibition and the right inferior frontal cortex. Trends Cogn. Sci. 2004;8:170–177. doi: 10.1016/j.tics.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch. Gen. Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Blair RJ. Neurocognitive models of aggression, the antisocial personality disorders, and psychopathy. J. Neurol. Neurosurg. Psychiatry. 2001;71:727–31. doi: 10.1136/jnnp.71.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair RJ. Applying a cognitive neuroscience perspective to the disorder of psychopathy. Dev. Psychopathol. 2005;17:865–91. doi: 10.1017/S0954579405050418. [DOI] [PubMed] [Google Scholar]
- Brett M, Anton J, Valabregue R, Poline J. Region of interest analysis using an SPM toolbox; Paper presented at the 8th International Conference on Functional Mapping of the Human Brain; Sendai, Japan. June 2.2002. [Google Scholar]
- Brunet E, Sarfati Y, Hardy-Bayle MC, Decety J. A PET investigation of the attribution of intentions with a nonverbal task. Neuroimage. 2000;11:157–166. doi: 10.1006/nimg.1999.0525. [DOI] [PubMed] [Google Scholar]
- Bufkin JL, Luttrell VR. Neuroimaging studies of aggressive and violent behavior: current findings and implications for criminology and criminal justice. Trauma Violence Abuse. 2005;6:176–191. doi: 10.1177/1524838005275089. [DOI] [PubMed] [Google Scholar]
- Carmichael ST, Price JL. Limbic connections of the orbital and medial prefrontal cortex in macaque monkeys. J. Comp. Neurol. 1995;363:615–641. doi: 10.1002/cne.903630408. [DOI] [PubMed] [Google Scholar]
- Cavada C, Company T, Tejedor J, Cruz-Rizzolo RJ, Reinoso-Suarez F. The anatomical connections of the Macaque monkey orbitofrontal cortex. A review. Cereb. Cortex. 2000;10:220–242. doi: 10.1093/cercor/10.3.220. [DOI] [PubMed] [Google Scholar]
- Cohen JB, Dickow A, Horner K, Zweben JE, Balabis J, Vandersloot D, Reiber C. Abuse and violence history of men and women in treatment for methamphetamine dependence. Am. J. Addict. 2003;12:377–385. [PubMed] [Google Scholar]
- Cretzmeyer M, Sarrazin MV, Huber DL, Block RI, Hall JA. Treatment of methamphetamine abuse: research findings and clinical directions. J. Subst. Abuse Treat. 2003;24:267–277. doi: 10.1016/s0740-5472(03)00028-x. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Putnam KM, Larson CL. Dysfunction in the neural circuitry of emotion regulation – a possible prelude to violence. Science. 2000;289:591–594. doi: 10.1126/science.289.5479.591. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Covi L. SCL-90: An outpatient psychiatric rating scale – preliminary report. Psychopharmacol. Bull. 1973;9:13–28. [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol. Med. 1983;13:595–605. [PubMed] [Google Scholar]
- Eagle DM, Baunez C, Shah AP, Lehmann O, Robbins TW. Inhibitory control in rats performing a stop-signal reaction time task: Differential effects of lesions of the orbitofrontal cortex, infralimbic cortex and subthalamic nucleus. Soc. Neurosci. Abstr. 2004;30:781. [Google Scholar]
- Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt? An fMRI study of social exclusion. Science. 2003;302:290–292. doi: 10.1126/science.1089134. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Way BM, Taylor SE, Welch WT, Lieberman MD. Understanding genetic risk for aggression: Clues from the brain's response to social exclusion. Biol. Psychiatry. 2007;61:1100–1108. doi: 10.1016/j.biopsych.2006.08.007. [DOI] [PubMed] [Google Scholar]
- Ekman P, Friesen WV. Pictures of facial affect. Consulting Psychologists Press; Palo Alto, CA: 1976. [Google Scholar]
- Ernst T, Chang L, Leonido-Yee M, Speck O. Evidence for long-term neurotoxicity associated with methamphetamine abuse: A 1H MRS study. Neurology. 2000;54:1344–1349. doi: 10.1212/wnl.54.6.1344. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (SCID-IP, Version 2.0) Biometrics Research Department, New York State Psychiatric Institute; New York, NY: 1996. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II): User's Guide. American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Fischer H, Wright CI, Whalen PJ, McInerney SC, Shin LM, Rauch SL. Brain habituation during repeated exposure to fearful and neutral faces: a functional MRI study. Brain Res. Bull. 2003;59:387–392. doi: 10.1016/s0361-9230(02)00940-1. [DOI] [PubMed] [Google Scholar]
- Fletcher PC, Happe F, Frith U, Baker SC, Dolan RJ, Frackowiak RS, Frith CD. Other minds in the brain: a functional imaging study of “theory of mind” in story comprehension. Cognition. 1995;57:109–128. doi: 10.1016/0010-0277(95)00692-r. [DOI] [PubMed] [Google Scholar]
- Forman SD, Cohen JD, Fizgerald M, Eddy WF, Mintun MA, Noll DC. Improved assessment of significant activation in functional magnetic resonance imaging (fMRI): Use of cluster-size threshold. Magn. Reson. Med. 1995;33:636–647. doi: 10.1002/mrm.1910330508. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Jezzard P, Turner R. Analysis of functional MRI time-series. Human Brain Mapping. 1994;1:153–171. [Google Scholar]
- Frith U, Frith C. The biological basis of social interaction. Curr. Dir. Psychol. Sci. 2001;10:151–155. [Google Scholar]
- Gallagher HL, Frith CD. Functional imaging of ‘theory of mind.’. Trends Cogn. Sci. 2003;7:77–83. doi: 10.1016/s1364-6613(02)00025-6. [DOI] [PubMed] [Google Scholar]
- Goldstein RZ, Volkow ND. Drug addiction and its underlying neurobiological basis: neuroimaging evidence for the involvement of the frontal cortex. Am. J. Psychiatry. 2002;159:1642–1652. doi: 10.1176/appi.ajp.159.10.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RZ, Volkow ND, Chang L, Wang GJ, Fowler JS, Depue RA, Gur RC. The orbitofrontal cortex in methamphetamine addiction: involvement in fear. Neuroreport. 2002;13:2253–2257. doi: 10.1097/01.wnr0000044215.09266.bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Hando J, Darke S, Ross J. Psychological morbidity and route of administration among amphetamine users in Sydney, Australia. Addiction. 1996;91:81–87. doi: 10.1046/j.1360-0443.1996.9118110.x. [DOI] [PubMed] [Google Scholar]
- Hariri AR, Bookheimer SY, Mazziotta JC. Modulating emotional responses: effects of a neocortical network on the limbic system. Neuroreport. 2000;11:43–48. doi: 10.1097/00001756-200001170-00009. [DOI] [PubMed] [Google Scholar]
- Haxby JV, Ungerleider LG, Horwitz B, Maisog JM, Rapoport SI, Grady CL. Face encoding and recognition in the human brain. Proc. Natl. Acad. Sci. U S A. 1996;93:922–927. doi: 10.1073/pnas.93.2.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haxby JV, Hoffman EA, Gobbini ML. Human neural systems for face recognition and social communication. Biol. Psychiatry. 2002;51:59–67. doi: 10.1016/s0006-3223(01)01330-0. [DOI] [PubMed] [Google Scholar]
- Hornak J, Rolls ET, Wade D. Face and voice expression identification in patients with emotional and behavioural changes following ventral frontal lobe damage. Neuropsychologia. 1996;34:247–261. doi: 10.1016/0028-3932(95)00106-9. [DOI] [PubMed] [Google Scholar]
- Huber A, Ling W, Shoptaw S, Gulati V, Brethen P, Rawson R. Integrating treatments for methamphetamine abuse: a psychosocial perspective. J. Addict. Dis. 1997;16:41–50. doi: 10.1080/10550889709511142. [DOI] [PubMed] [Google Scholar]
- Iidaka T, Omori M, Murata T, Kosaka H, Yonekura Y, Okada T, Sadato N. Neural interaction of the amygdala with the prefrontal and temporal cortices in the processing of facial expressions as revealed by fMRI. J. Cognitive Neurosci. 2001;13:1035–1047. doi: 10.1162/089892901753294338. [DOI] [PubMed] [Google Scholar]
- Ishai A, Schmidt CF, Boesiger P. Face perception is mediated by a distributed cortical network. Brain Res. Bull. 2005;67:87–93. doi: 10.1016/j.brainresbull.2005.05.027. [DOI] [PubMed] [Google Scholar]
- Jentsch JD, Olausson P, De La Garza R, Taylor JR. Impairments of reversal learning and response perseveration after repeated, intermittent cocaine administrations to monkeys. Neuropsychopharmacology. 2002;26:183–190. doi: 10.1016/S0893-133X(01)00355-4. [DOI] [PubMed] [Google Scholar]
- Kane MJ, Engle RW. The role of prefrontal cortex in working-memory capacity, executive attention, and general fluid intelligence: an individual-differences perspective. Psychon. Bull. Rev. 2002;9:637–71. doi: 10.3758/bf03196323. [DOI] [PubMed] [Google Scholar]
- Kanwisher N, McDermott J, Chun MM. The fusiform face area: a module in human extrastriate cortex specialized for face perception. J. Neurosci. 1997;17:4302–4311. doi: 10.1523/JNEUROSCI.17-11-04302.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keightley ML, Winocur G, Graham SJ, Mayberg HS, Hevenor SJ, Grady CL. An fMRI study investigating cognitive modulation of brain regions associated with emotional processing of visual stimuli. Neuropsychologia. 2003;41:585–596. doi: 10.1016/s0028-3932(02)00199-9. [DOI] [PubMed] [Google Scholar]
- Kesler-West ML, Andersen AH, Smith CD, Avison MJ, Davis CE, Kryscio RJ, Blonder LX. Neural substrates of facial emotion processing using fMRI. Brain Res. Cogn. Brain Res. 2001;11:213–226. doi: 10.1016/s0926-6410(00)00073-2. [DOI] [PubMed] [Google Scholar]
- Leppanen J, Milders M, Bell J, Terriere E, Hietanen J. Depression biases the recognition of emotionally neutral faces. Psychiatry Res. 2004;128:123–133. doi: 10.1016/j.psychres.2004.05.020. [DOI] [PubMed] [Google Scholar]
- Lieberman MD, Jarcho JM, Berman S, Naliboff B, Suyenobu BY, Mandelkern M, Mayer E. The neural correlates of placebo effects: A disruption account. Neuroimage. 2004;22:447–455. doi: 10.1016/j.neuroimage.2004.01.037. [DOI] [PubMed] [Google Scholar]
- Lieberman MD, Eisenberger NI, Crockett MJ, Tom SM, Pfeifer JH, Way BM. Putting feelings into words: affect labeling disrupts amygdala activity in response to affective stimuli. Psychol. Science. 2007;18:421–428. doi: 10.1111/j.1467-9280.2007.01916.x. [DOI] [PubMed] [Google Scholar]
- Logan BK, Fligner CL, Haddix T. Cause and manner of death in fatalities involving methamphetamine. J. Forensic Sci. 1998;43:28–34. [PubMed] [Google Scholar]
- London ED, Simon SL, Berman SM, Mandelkern MA, Lichtman AM, Bramen J, Shinn AK, Miotto K, Learn J, Dong Y, Matochik JA, Kurian V, Newton T, Woods R, Rawson R, Ling W. Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Arch. Gen. Psychiatry. 2004;61:73–84. doi: 10.1001/archpsyc.61.1.73. [DOI] [PubMed] [Google Scholar]
- Ma CL, Qi XL, Peng JY, Li BM. Selective deficit in no-go performance induced by blockade of prefrontal cortical alpha 2-adrenoceptors in monkeys. Neuroreport. 2003;14:1013–1016. doi: 10.1097/01.wnr.0000070831.57864.7b. [DOI] [PubMed] [Google Scholar]
- Maxwell JC. Emerging research on methamphetamine. Curr. Opin. Psychiatry. 2005;18:235–242. doi: 10.1097/01.yco.0000165592.52811.84. [DOI] [PubMed] [Google Scholar]
- Monterosso JR, Aron AR, Cordova X, Xu J, London ED. Deficits in response inhibition associated with chronic methamphetamine abuse. Drug Alcohol Depend. 2005;79:273–277. doi: 10.1016/j.drugalcdep.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Morris JS, Frith CD, Perrett DI, Rowland D, Young AW, Calder AJ, Dolan RJ. A differential neural response in the human amygdala to fearful and happy facial expressions. Nature. 1996;383:812–815. doi: 10.1038/383812a0. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Kawashima R, Ito K, Sugiura M, Kato T, Nakamura A, Hatano K, Nagumo S, Kubota K, Fukuda H, Kojima S. Activation of the right inferior frontal cortex during assessment of facial emotion. J. Neurophysiol. 1999;82:1610–1614. doi: 10.1152/jn.1999.82.3.1610. [DOI] [PubMed] [Google Scholar]
- Newton TF, Kalechstein AD, Duran S, Vansluis N, Ling W. Methamphetamine abstinence syndrome: preliminary findings. Am. J. Addict. 2004;13:248–255. doi: 10.1080/10550490490459915. [DOI] [PubMed] [Google Scholar]
- Nordahl TE, Salo R, Possin K, Gibson DR, Flynn N, Leamon M, Galloway GP, Pfefferbaum A, Spielman DM, Adalsteinsson E, Sullivan EV. Low N-acetyl-aspartate and high choline in the anterior cingulum of recently abstinent methamphetamine-dependent subjects: a preliminary proton MRS study. Psychiatry Res. 2002;116:43–52. doi: 10.1016/s0925-4927(02)00088-4. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Knierim K, Ludlow DH, Hanelin J, Ramachandran T, Glover G, Mackey SC. Reflecting upon feelings: An fMRI study of neural systems supporting the attribution of emotion to self and other. J. Cognitive Neurosci. 2004;16:1746–1772. doi: 10.1162/0898929042947829. [DOI] [PubMed] [Google Scholar]
- Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9:97–113. doi: 10.1016/0028-3932(71)90067-4. [DOI] [PubMed] [Google Scholar]
- Paulus MP, Hozack NE, Zauscher BE, Frank L, Brown GG, Braff DL, Schuckit MA. Behavioral and functional neuroimaging evidence for prefrontal dysfunction in methamphetamine-dependent subjects. Neuropsychopharmacology. 2002;26:53–63. doi: 10.1016/S0893-133X(01)00334-7. [DOI] [PubMed] [Google Scholar]
- Phan KL, Wager T, Taylor SF, Liberzon I. Functional neuroanatomy of emotion: a meta-analysis of emotion activation studies in PET and fMRI. Neuroimage. 2002;16:331–348. doi: 10.1006/nimg.2002.1087. [DOI] [PubMed] [Google Scholar]
- Phillips ML, Williams LM, Heining M, Herba CM, Russell T, Andrew C, Bullmore ET, Brammer MJ, Williams SC, Morgan M, Young AW, Gray JA. Differential neural responses to overt and covert presentations of facial expressions of fear and disgust. Neuroimage. 2004;21:1484–1496. doi: 10.1016/j.neuroimage.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Pietrini P, Guazzelli M, Basso G, Jaffe K, Grafman J. Neural correlates of imaginal aggressive behavior assessed by positron emission tomography in healthy subjects. Am. J. Psychiatry. 2000;157:1772–1781. doi: 10.1176/appi.ajp.157.11.1772. [DOI] [PubMed] [Google Scholar]
- Raine A, Meloy JR, Bihrle S, Stoddard J, LaCasse L, Buchsbaum MS. Reduced prefrontal and increased subcortical brain functioning assessed using positron emission tomography in predatory and affective murderers. Behav. Sci. Law. 1998;16:319–332. doi: 10.1002/(sici)1099-0798(199822)16:3<319::aid-bsl311>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MC. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997;277:968–971. doi: 10.1126/science.277.5328.968. [DOI] [PubMed] [Google Scholar]
- Salo R, Nordahl TE, Moore C, Waters C, Natsuaki Y, Galloway GP, Kile S, Sullivan EV. A dissociation in attentional control: evidence from methamphetamine dependence. Biol. Psychiatry. 2005;57:310–313. doi: 10.1016/j.biopsych.2004.10.035. [DOI] [PubMed] [Google Scholar]
- Samson D, Apperly IA, Chiavarino C, Humphreys GW. Left temporoparietal junction is necessary for representing someone else's belief. Nat. Neurosci. 2004;7:499–500. doi: 10.1038/nn1223. [DOI] [PubMed] [Google Scholar]
- Saxe R, Kanwisher N. People thinking about thinking people: The role of the temporo-parietal junction in “theory of mind.”. Neuroimage. 2003;19:1835–1842. doi: 10.1016/s1053-8119(03)00230-1. [DOI] [PubMed] [Google Scholar]
- Saxe R, Carey S, Kanwisher N. Understanding other minds: Linking developmental psychology and functional neuroimaging. Annu. Rev. Psychol. 2004;55:87–124. doi: 10.1146/annurev.psych.55.090902.142044. [DOI] [PubMed] [Google Scholar]
- Saxe R, Wexler A. Making sense of another mind: The role of the right temporo-parietal junction. Neuropsychologia. 2005;43:1391–1399. doi: 10.1016/j.neuropsychologia.2005.02.013. [DOI] [PubMed] [Google Scholar]
- Sekine Y, Iyo M, Ouchi Y, Matsunaga T, Tsukada H, Okada H, Yoshikawa E, Futatsubashi M, Takei N, Mori N. Methamphetamine-related psychiatric symptoms and reduced brain dopamine transporters studied with PET. Am. J. Psychiatry. 2001;158:1206–1214. doi: 10.1176/appi.ajp.158.8.1206. [DOI] [PubMed] [Google Scholar]
- Sekine Y, Minabe Y, Ouchi Y, Takei N, Iyo M, Nakamura K, Suzuki K, Tsukada H, Okada H, Yoshikawa E, Futatsubashi M, Mori N. Association of dopamine transporter loss in the orbitofrontal and dorsolateral prefrontal cortices with methamphetamine-related psychiatric symptoms. Am. J. Psychiatry. 2003;160:1699–1701. doi: 10.1176/appi.ajp.160.9.1699. [DOI] [PubMed] [Google Scholar]
- Sekine Y, Ouchi Y, Takei N, Yoshikawa E, Nakamura K, Futatsubashi M, Okada H, Minabe Y, Suzuki K, Iwata Y, Tsuchiya KJ, Tsukada H, Iyo M, Mori N. Brain serotonin transporter density and aggression in abstinent methamphetamine abusers. Arch. Gen. Psychiatry. 2006;63:90–100. doi: 10.1001/archpsyc.63.1.90. [DOI] [PubMed] [Google Scholar]
- Shaham Y, Erb S, Stewart J. Stress-induced relapse to heroin and cocaine seeking in rats: a review. Brain Res. Brain Res. Rev. 2000;33:13–33. doi: 10.1016/s0165-0173(00)00024-2. [DOI] [PubMed] [Google Scholar]
- Shipley WC. A self-administering scale for measuring intellectual impairment and deterioration. J. Psychol. 1940;9:371–377. [Google Scholar]
- Sprengelmeyer R, Rausch M, Eysel UT, Przuntek H. Neural structures associated with recognition of facial expressisons of basic emotions. Proc. R. Soc. Lond. B Biol. Sci. 1998;265:1927–1931. doi: 10.1098/rspb.1998.0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson PM, Hayashi KM, Simon SL, Geaga JA, Hong MS, Sui Y, Lee JY, Toga AW, Ling W, London ED. Structural abnormalities in the brains of human subjects who use methamphetamine. J. Neurosci. 2004;24:6028–6036. doi: 10.1523/JNEUROSCI.0713-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tominaga GT, Garcia G, Dzierba A, Wong J. Toll of methamphetamine on the trauma system. Arch. Surg. 2004;139:844–847. doi: 10.1001/archsurg.139.8.844. [DOI] [PubMed] [Google Scholar]
- Vogt BA, Pandya DN. Cingulate cortex of the Rhesus monkey: II. Cortical afferents. J. Comp. Neurol. 1987;262:271–289. doi: 10.1002/cne.902620208. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Chang L, Wang GJ, Fowler JS, Ding YS, Sedler M, Logan J, Franceschi D, Gatley J, Hitzemann R, Gifford A, Wong C, Pappas N. Low level of brain dopamine D2 receptors in methamphetamine abusers: Association with metabolism in the orbitofrontal cortex. Am. J. Psychiatry. 2001;158:2015–2021. doi: 10.1176/appi.ajp.158.12.2015. [DOI] [PubMed] [Google Scholar]
- Vollm BA, Taylor AN, Richardson P, Corcoran R, Stirling J, McKie S, Deakin JF, Elliott R. Neuronal correlates of theory of mind and empathy: a functional magnetic resonance imaging study in a nonverbal task. Neuroimage. 2005;29:90–8. doi: 10.1016/j.neuroimage.2005.07.022. [DOI] [PubMed] [Google Scholar]
- Wilson JM, Kalasinsky KS, Levey AI, Bergeron C, Reiber G, Anthony RM, Schmunk GA, Shannak K, Haycock JW, Kish SJ. Striatal dopamine nerve terminal markers in human, chronic methamphetamine users. Nat. Med. 1996;2:699–703. doi: 10.1038/nm0696-699. [DOI] [PubMed] [Google Scholar]
- Wright CI, Fischer H, Whalen PJ, McInerney SC, Shin LM, Rauch SL. Differential prefrontal cortex and amygdala habituation to repeatedly presented emotional stimuli. Neuroreport. 2001;12:379–383. doi: 10.1097/00001756-200102120-00039. [DOI] [PubMed] [Google Scholar]
- Zweben JE, Cohen JB, Christian D, Gallloway GP, Salinardi M, Parent D, Iguchi M. Psychiatric symptoms in methamphetamine users. Am. J. Addict. 2004;13:181–190. doi: 10.1080/10550490490436055. [DOI] [PubMed] [Google Scholar]