Abstract
The importance of lifelong learning in medicine is well recognised. This article explores how junior doctors can develop learning strategies for use throughout their working life
Key points
Lifelong learning is a process of continuously scrutinising and building on your practice to be the best doctor you can be
Always have three questions in your mind: where am I going? how am I getting on? where to next?
Use electronic tools that provide filtered information at the point of care because you cannot hope to stay up to date on everything
Keep a learning portfolio so that you can see how you have already developed and how you can develop in the future
Keep your learning efforts alive by discussing them with your peers and supervisors
Most doctors are aware of the aphorism that learning should continue from the cradle to the grave. However, medical school does not prepare anyone fully for the responsibilities, long hours, and challenging tasks that qualification brings.1 2 The fittest survive by learning from their practice, whereas those who do not continue to learn become dissatisfied and burn out.3 Current restrictions in working hours, changes in the organisation of health care, shorter hospital stays, and the breakdown of the medical firm make it ever more necessary to learn efficiently from practice.4
Numerous editorials and descriptive articles have stated the importance of lifelong learning, but research has not yet provided a definitive answer to the question “How can trainees develop lifelong learning strategies?” We have drawn on medical education theory and empirical studies of both facilitating practice change and the effectiveness of feedback for best evidence on effective lifelong learning. Those sources show that one size does not fit all. Our article does not therefore offer quick fixes such as organising group learning sessions or purchasing a personal digital assistant, but rather it describes the continuous personal endeavour that lifelong learners face.
Lifelong learning: how best to do it
Learn in the workplace
Ideas about work based learning have moved from thinking of learners as solitary beings to thinking of them as members of “communities of practice”5 in which interaction with other doctors, nurses, and allied professionals of various levels of seniority shapes their personal and professional development.6 Learners, however, are sometimes more aware of lectures and courses as learning opportunities than they are of the “on the job” learning opportunities that they face all day. As a learner, you therefore need to capitalise on such opportunities by soliciting feedback, seeking out evidence of clinical effectiveness at the point of care, and participating fully in the educational activities of whichever community of practice you are currently working in.
Be in charge
To be an effective lifelong learner in the workplace, you have to make a conscious decision to direct your own development.7 Research in continuing medical education shows that doctors learn most when they are motivated enough to identify their own learning needs and meet those needs at their own pace.8 9 For trainees, that means turning workplace experiences into realistic and achievable learning objectives. When you finish rounds on the internal medicine ward, list the topics you need to learn more about; prioritise them, and write down one or two higher level learning objectives for the weeks to come; and set a date to finish them by. For example:
You just saw four patients with diabetic complications; do you really know everything you need to know about regulating blood glucose? If not, focus on diabetes
Do you feel defeated by that one patient who just didn’t seem to understand your explanations? Focus on communicating with patients
Are your rounds running late for the fourth time this week? Focus on time management
Did a teaching session identify a gap in your practical competence? Focus on clinical skills.
Use input from peers and seniors to identify your learning needs because a person’s ability to assess his or her own performance is limited.10 Keep a personal portfolio on an electronic organiser (and always keep that in your pocket) so you can note new goals and new learning points.
Seek input from others
Observing how other staff and patients respond to a situation can reinforce an existing perspective or open up a different one.6 It is up to you to examine and question your routines and interpretations.
However, not all types of feedback lead to improvements.11 A synthesis of 12 meta-analyses (196 studies and 6972 effect sizes) on the effectiveness of feedback defined some rules of play (see box)12:
Feedback can only build on previous experience. So if regulation of blood glucose is a new area for you, ask somebody skilled to show you how to do it rather than hoping you’ll just pick it up as you go
Seek feedback on your learning objective(s) to enable you to answer each of three inter-related questions (where am I going? how am I getting on? where to next?) If the first of those three questions relates to improving your communication with patients, then to answer the second question you need to ask someone to observe you and discuss with you their views on what you did. Select anybody you can learn from. Consultants or registrars may be the most obvious choices, but recognise the expertise of, say, an experienced nurse. Try to understand how these people do what you aspire to do, discuss with them how you might do it, and ask them to help you answer the third question (where to next?)
For feedback to be effective, it needs to be directed at the task as a whole or at certain aspects of the task, and not at the person who performed it. Various meta-analyses have shown that positive or negative feedback about yourself (such as “great effort!” or “you’ll never be good at doing rounds”) is largely ineffective.11 13 In the case of finishing rounds on time, ask what it is that you are doing that makes you run late (the task); ask how to strike a balance between attention to individual patients and being fair to the whole group of patients (processes needed to understand the task); and ask how you can monitor and adjust the pace of rounds as you go along (self regulation in performing the task).
Directions for feedback
Challenge yourself, look for feedback, but remember:
If you are inexperienced, first get instructions, then get feedback
Feedback answers three questions: where am I going? how am I getting on? where to next?
Get feedback directed at: (a) the task, (b) processes needed to understand the task, (c) self regulation in performing the task
Use evidence at the point of care
The evidence based practice movement set out primarily to improve health care, but its aims provide an excellent model for learning from practice. It urges doctors to use the challenges and surprises that they encounter in practice to formulate questions and find valid answers that they can then apply to patients.14 Evidence based practice at the point of care is not necessarily straightforward, however. Green and colleagues showed that residents pursued only 80 of 277 identified questions and used very few evidence based practice sources.15 Research into information seeking behaviour on the internet found that only 9% of 2500 physicians in the United States searched for information during a patient encounter.16 The greatest barriers were a lack of available information or a glut of it. How can we improve the application of evidence based practice at the point of care?
The classic approach (critical appraisal of primary literature using the “populations, intervention, comparison, outcome” format) is impractical for bedside use.17 Slawson and Shaughnessy suggested that doctors need several skills to use evidence based practice at the point of care: the ability to select and use “foraging” and “hunting” tools and to make “sensible decisions by combining the best patient-oriented evidence with patient-centered care.”17 The authors described foraging tools as those that filter information for relevance and validity (such as DailyPOEMs (www.infopoems.com) and Journal Watch (www.jwatch.org)) and hunting tools as those that “present prefiltered information easily at the point of care” (such as Dynamed (www.ebscohost.com/dynamed) and InfoRetriever)).
Stay on track
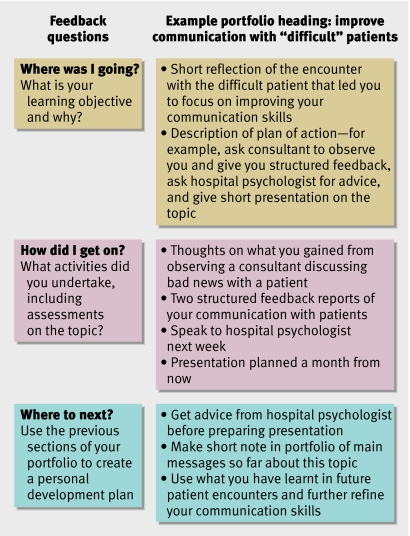
Work related activities are both a starting point for learning and an opportunity to refine and consolidate what you learnt earlier.5 A portfolio can help you to formulate and structure your learning targets and keep track of how well you are meeting them. For example, you can make a short note of the rules of thumb you developed to regulate the blood glucose levels of patients with diabetes. Writing a case report for your portfolio on a patient who had his left foot amputated as a result of neuroischaemic ulceration can lead to “management of deep tissue infections” as a new learning objective. A portfolio can help you decide whether your previous learning outcomes have been of use in practice; if not, you need to reconsider your learning habits. A portfolio provides you (and your educational supervisor) with evidence to look back on your learning and evaluate it (see figure):
Answering the three feedback questions by using your portfolio
“Where was I going?” This can be a short reflection on, say, an encounter with a “difficult” patient that led to you to focus on improving your communication skills
“How did I get on?” You can think about, for example, what you gained from observing a consultant discussing bad news with a patient, and two structured feedback reports of your communication with patients
“Where to next?” The information collected in your portfolio helps to make your development more tangible and provides the input for discussing your personal development plan with an educational supervisor.
Do not invest energy in the pursuit of goals that are irrelevant to practice or personal development. Portfolios can keep you on track.
What are the challenges?
Throughout their career, doctors need to work hard at taking advantage of the constant learning opportunities that arise. Lifelong learners’ biggest achievement is finding the motivation to keep questioning their actions and knowledge. Lifelong learning means striking the right balance between confidence and doubt. It is easiest to find this balance if you work with people who support and value questioning behaviour.18 If that working culture does not exist, it is difficult for a trainee to create it. Nevertheless, it is essential to develop the confidence to doubt your own practice even when patients, nurses, and peers expect you to behave with apparent certainty.2 19
Contributors: Both authors contributed to the conception and writing of this article. PWT is the guarantor.
Competing interests: None declared.
Provenance and peer review: Commissioned and externally peer reviewed.
This series aims to help junior doctors in their daily tasks and is based on selected topics from the UK core curriculum for foundation years 1 and 2, the first two years after graduation from medical school.
References
- 1.Prince KJ, Boshuizen HP, van der Vleuten CP, Scherpbier AJ. Students’ opinions about their preparation for clinical practice. Med Educ 2005;39:704-12. [DOI] [PubMed] [Google Scholar]
- 2.Brown J, Chapman T, Graham D. Becoming a new doctor: a learning or survival exercise? Med Educ 2007;41:653-60. [DOI] [PubMed] [Google Scholar]
- 3.Becker JL, Milad MP, Klock SC. Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol 2006;195:1444-9. [DOI] [PubMed] [Google Scholar]
- 4.Bannon M. What’s happening in postgraduate medical education? Arch Dis Child 2006;91:68-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wenger E. Communities of practice: learning, meaning, and identity Cambridge: Cambridge University Press, 1998
- 6.Teunissen PW, Scheele F, Scherpbier AJ, van der Vleuten CP, Boor K, van Luijk SJ, et al. How residents learn: qualitative evidence for the pivotal role of clinical activities. Med Educ 2007;41:763-70. [DOI] [PubMed] [Google Scholar]
- 7.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 2004;1988:S1-12. [DOI] [PubMed] [Google Scholar]
- 8.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA 1995;274:700-5. [DOI] [PubMed] [Google Scholar]
- 9.Mazmanian PE, Davis DA. Continuing medical education and the physician as a learner: guide to the evidence. JAMA 2002;288:1057-60. [DOI] [PubMed] [Google Scholar]
- 10.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA 2006;296:1094-102. [DOI] [PubMed] [Google Scholar]
- 11.Kluger AN, DeNisi A. The effects of feedback interventions on performance: historical review, a meta-analysis and a preliminary feedback intervention theory. Psychological Bulletin 1996;119:254-84. [Google Scholar]
- 12.Hattie J, Timperley H. The power of feedback. Review of Educational Research 2007;77:81-112. [Google Scholar]
- 13.Wilkinson SS. The relationship of teacher praise and student achievement: a meta-analysis of selected research. Dissertation Abstracts International 1981;41:3998 [Google Scholar]
- 14.Sackett DL, Straus SE, Scott Richardson W, Rosenberg W, Haynes RB. Evidence-based medicine: how to practice and teach EBM Edinburgh: Churchill-Livingstone, 2000
- 15.Green ML, Ciampi MA, Ellis PJ. Residents’ medical information needs in clinic: are they being met? Am J Med 2000;109:218-23. [DOI] [PubMed] [Google Scholar]
- 16.Bennett NL, Casebeer LL, Zheng S, Kristofco R. Information-seeking behaviors and reflective practice. J Contin Educ Health Prof 2006;26:120-7. [DOI] [PubMed] [Google Scholar]
- 17.Slawson DC, Shaughnessy AF. Teaching evidence-based medicine: should we be teaching information management instead? Acad Med 2005;80:685-9. [DOI] [PubMed] [Google Scholar]
- 18.Dornan T, Boshuizen H, King N, Scherpbier A. Experience-based learning: a model linking the processes and outcomes of medical students’ workplace learning. Med Educ 2007;41:84-91. [DOI] [PubMed] [Google Scholar]
- 19.Teunissen PW, Boor K, Scherpbier AJJA, van der Vleuten CPM, van Diemen-Steenvoorde JAAM, van Luijk SJ, et al. Attending doctors’ perspective on how residents learn. Med Educ 2007;41:1050-8. [DOI] [PubMed] [Google Scholar]