Abstract
Studies using neuroimaging, electrophysiologic and cognitive measures have raised hopes for developing predictors of therapeutic response to antidepressants. Pretreatment measures of functional brain asymmetry have been found to be related to response to the selective serotonin reuptake inhibitor fluoxetine. This report examines the extent to which dichotic listening tests also predict clinical response to an antidepressant with a different mechanism of action, i.e., bupropion. Dichotic listening data were obtained for 17 unmedicated depressed patients who were subsequently treated with bupropion. Right-handed outpatients were tested on dichotic fused-words and complex-tones tests. Seven patients who responded to bupropion and 10 nonresponders did not differ in gender, age or education. Bupropion responders had significantly larger left-hemisphere advantage for perceiving words when compared to nonresponders, but there was no difference in their right-hemisphere advantage for tones. All patients having a left-hemisphere advantage above the normal mean responded to bupropion, whereas only 9% of patients below the normal mean responded to treatment. These findings should encourage further study of the clinical value of dichotic listening and other measures of functional brain asymmetry for identifying depressed patients who most benefit from treatment with different classes of antidepressants.
Keywords: depression, bupropion, treatment response, dichotic listening, hemispheric asymmetry
1. Introduction
Although a variety of antidepressants with different mechanisms of action are available for treatment of depression, clinicians have no way of knowing in advance whether or not a given patient will benefit from treatment with a specific agent. Patients often must endure a prolonged “trial and error” period before finding an effective antidepressant, and they may become increasingly hopeless if they fail to benefit and discontinue treatment. Studies using neuroimaging (Buchsbaum et al., 1997; Little et al., 2005; Mayberg et al., 1997; Saxena et al., 2003), electrophysiologic (Bruder et al., 2001; Pizzagalli et al., 2001; Cook and Leuchter, 2001; Kalayam and Alexopoulos, 2003), and neurocognitive (Dunkin et al., 2000; Taylor et al., 2006) measures of brain function suggest that pretreatment differences among depressed patients are associated with responsiveness to antidepressants, raising hopes for identifying predictors of clinical response to antidepressants. It is not, however, known whether these findings are associated with a specific class of antidepressants, e.g., selective serotonin reuptake inhibitors (SSRIs), or are common to antidepressants with different mechanisms of activity.
Studies using dichotic listening tests indicate that pretreatment measures of functional asymmetry of the right-left brain are related to subsequent responsiveness to treatment with the SSRI fluoxetine (Bruder et al., 1996; Stewart et al., 1999; Bruder et al., 2004). In dichotic listening tests, different stimuli (e.g., words or tones) are simultaneously presented to the left and right ears and the advantage for hearing items in the right or left ear, referred to as perceptual asymmetry (PA), provides a measure of the advantage of the contralateral hemisphere for processing verbal or tonal information. Unmedicated depressed patients at two clinical centers who subsequently responded favorably to fluoxetine differed from nonresponders in showing greater left-hemisphere advantage for perceiving dichotic words and less right-hemisphere advantage for perceiving complex tones (Bruder et al., 1996). This difference in dichotic listening between fluoxetine responders and nonresponders was replicated in two additional studies, and was found to be dependent on gender in both studies (Bruder et al., 2004). The heightened left-hemisphere advantage for words in fluoxetine responders was present among women but not men, whereas reduced right-hemisphere advantage for tones in responders was present among men but not women.
The clinical value of dichotic listening or other tests for predicting treatment response would be strengthened if they also indicated whether an alternative treatment would benefit patients who are not likely to respond to an SSRI, the usual initial treatment. This report presents dichotic listening data for patients who were treated with the bupropion after, in most cases, unsuccessful treatment with the SSRI fluoxetine. We examined whether dichotic listening tests obtained before treatment would predict clinical response to bupropion and, if so, whether differences between bupropion responders and nonresponders are similar to or different from those seen for fluoxetine.
2. Methods
2.1 Subjects
Patients were right-handed depressed outpatients between the ages of 20 and 64 who were attending a university-affiliated research clinic. Patients were excluded for any of the following reasons: serious suicide risk, substance abuse disorders (including alcohol abuse) within the last 6 months, psychotic disorders, antisocial personality disorder, seizure disorder, organic mental disorder, history of head trauma, or other neurological disorder. They were also excluded if they had a hearing loss greater than 30 dB in either ear at 500, 1000 or 2000 Hz or if they had an ear difference greater than 10 dB. All participants gave written informed consent before participating in the study. Diagnostic assessment was by Structured Interview for Clinical Diagnosis, patient version (SCID-P; First et al., 1994), conducted by research psychiatrists before dichotic listening tests. Patients met DSM-IV criteria for major depressive disorder or, in one case, dysthymia. All findings reported below for the full sample were confirmed after excluding the one dysthymic patient.
Before being treated with bupropion, the patients participated in a fluoxetine treatment study (n=14) or were treated openly with fluoxetine (n=3). Their daily fluoxetine dose was titrated to a maximum of 40-80 mg over a period of up to 12 weeks. All but 4 of these patients were judged to be fluoxetine nonresponders using Clinical Global Impression Improvement (CGI-I) criteria of minimal or no improvement. The remaining 4 patients responded to fluoxetine treatment but relapsed or had side effects. These patients were subsequently treated with the SR formulation of bupropion. Twelve patients received bupropion within an 8 week open label study and 5 patients received open clinical treatment, beginning with a daily dose of 100 or 150 mg and titrating to a maximum dose of 400mg (except for one patient who received 600 mg). Only patients who received a minimum of 6 weeks of bupropion treatment are included in this report.
A research psychiatrist blind to dichotic listening data reviewed each patient’s chart to determine treatment response independent of knowledge of the dichotic listening results. To be considered a “responder” (R) the chart had to document a marked clinical improvement in the patient’s depression, as indicated by chart notes such as “depression much improved”, “remitted”, “no longer depressed”, “feeling well” or similar assessments within four weeks of the patient starting on their maximal dose. In addition, improvement had to be sustained for at least 4 weeks. In four cases where there was not 4 weeks follow-up after their initial benefit, their response was determined to be as indicated in their last chart note. Patients judged to be a “nonresponder” (NR) had descriptors indicating minimal or no clinical improvement, including “no benefit”, “no change”, “minimal improvement” or “much worse”. In most cases, a treatment call was based on outcome at end of 8th week of treatment or in four patients who stopped treatment at the 7th week, the last available visit brought forward.
2.2 Procedure
Dichotic listening tests were administered during a pretreatment session before patients received treatment with fluoxetine and then bupropion. Patients were unmedicated a minimum of 7 days before dichotic listening testing, although most patients were drug-free for a considerably longer period or were not previously treated with an antidepressant. No patient was tested within 6 weeks of receiving fluoxetine or 1 week of receiving other antidepressants and no patient had received a monoamine oxidase inhibitor. All patients and controls were tested on the dichotic fused words and complex tones tests described below, with the order of the tests counterbalanced across subjects.
The Fused Rhymed Words Test (Wexler and Halwes, 1983) consists of 15 different single-syllable word pairs, in which each member of every pair differs from the other only in the initial consonant (e.g., coat, goat). All words begin with one of six stop consonants (b, d, p, t, g, k) and are natural speech spoken by a male voice. When dichotically presented, the members of each pair fuse into a single percept. Participants indicate what word they heard by marking a line through it on a prepared answer sheet that has four possible responses, both members of the dichotic pair and two other words differing from the dichotic stimuli only in the initial consonant. Following practice trials, each participant received four 30-item blocks for a total of 120 trials. Orientation of headphones was reversed after the first and third quarters to control for channel differences and ear of presentation. The words were presented via a matched pair of TDH-49 headphones at a comfortable level of 75 dB sound pressure level (SPL).
The Complex Tone Test (Sidtis, 1981) requires participants to compare the pitch of a binaural complex tone with the pitches of a dichotic pair of complex tones presented 1 second earlier. Subjects point to a response card labeled Yes when the probe tone is the same as either member of the previous dichotic pair or to a card labeled No when it differs from both. The complex tones are square waves with fundamental frequencies corresponding to eight notes in the octave between C4 and C5. After 16 binaural and 16 dichotic practice trails, participants were tested on four blocks of 28 trials in which half of the probe tones matched a member of the dichotic pair and half did not. Orientation of headphones was reversed after the first and third blocks. The tones were presented at 74 dB SPL.
2.3 Statistical Analyses
Correct responses in the words and tones tests were computed for right- and left-ear presentations. These scores were used to compute an index of perceptual asymmetry, PA= 100 (Right Correct - Left Correct)/(Right Correct + Left Correct). A 2 by 2 repeated measures ANOVA was performed using one between-subject variable of Bupropion Response (R, NR) and one repeated-measure variable of Test (words, tones), with PA scores being the dependent variable. If a significant interaction of Bupropion Response and Test was present, separate t-tests were planned to evaluate whether responders and nonresponders differed on the individual dichotic tests.
The potential value of PA scores for predicting therapeutic response to bupropion was examined using a χ2 test to compare response rates of patients with PA scores above versus below the mean for healthy adults. Sensitivity, specificity, positive predictive value and negative predictive value were also computed.
3. Results
There were 7 bupropion responders (5 men) who did not differ significantly from the 10 nonresponders (6 men) in gender, age (R mean= 43.3 yrs, SD=12.1; NR mean=40.5 yrs, SD=9.7; t=0.53, df=15, ns), education (R mean= 16.7 yrs, SD=3.2; NR mean=14.9 yrs, SD=2.3; t=1.36, df=15, ns) or handedness laterality quotient (R mean= 84.4, SD= 21.0; NR mean= 84.7, SD=18.2; t=0.03, df=15, ns) on the Edinburgh Inventory (Oldfield, 1971). The responder and nonresponder groups also had comparable diagnoses. All met DSM-IV criteria for MDD, except for one nonresponder who met criteria for dysthymia. Two responders also had a panic disorder and three nonresponders had comorbid anxiety disorders (panic disorder, social phobia or obsessive-compulsive disorder). Two patients in each group met DSM-IV criteria for atypical depression and an additional two responders and three nonresponders showed the essential feature of reactivity of mood and one of four associated features of atypical depression (Liebowitz et al., 1984). The responders and nonresponders also did not differ in pretreatment severity of depression on the Beck Depression Inventory (BDI; Beck et al., 1961) in the baseline session, when dichotic listening tests were performed (R mean= 19.4, SD=8.0; NR mean= 25.8, SD=9.1; t=1.49, df=15, ns). Also, pretreatment BDI scores were not related to PA for either words (r= -0.05, ns) or tones (r= -0.04, ns).
Figure 1 gives the PA scores for bupropion responders and nonresponders on the dichotic word and tone tests. Dashed lines show the mean left-hemisphere advantage for words (i.e., positive PA scores) and right-hemisphere advantage for tones (i.e., negative PA scores) for 101 normal adults tested in our laboratory (Bruder et al., 2004). The patients also showed the expected difference in PA for words and tones (main effect of Test: F= 31.17, df= 1,15, P<.001). There was also a significant interaction between Bupropion Response and Test (F= 6.99, df=1,15, P=.018). Separate analyses of PA scores for each test showed that responders had markedly larger left-hemisphere advantage for words when compared to nonresponders (t=4.06, df= 15, P=.001), but there was no group difference in right-hemisphere advantage for tones (t= 0.36, df= 15, ns), which accounts for this interaction. Although gender was not included as a variable in the ANOVA because cell sizes would be too small, inspection of the data for individual men (closed points) and women (open points) in Figure 1 suggests that gender was not a factor. The 5 male responders had significantly larger left-hemisphere advantage for words when compared to the 6 male nonresponders (t=2.62, df=9, P<.05) and the same difference was seen between 2 female responders and 4 female nonresponders (t= 4.86, df=4, P<.01).
Figure 1.
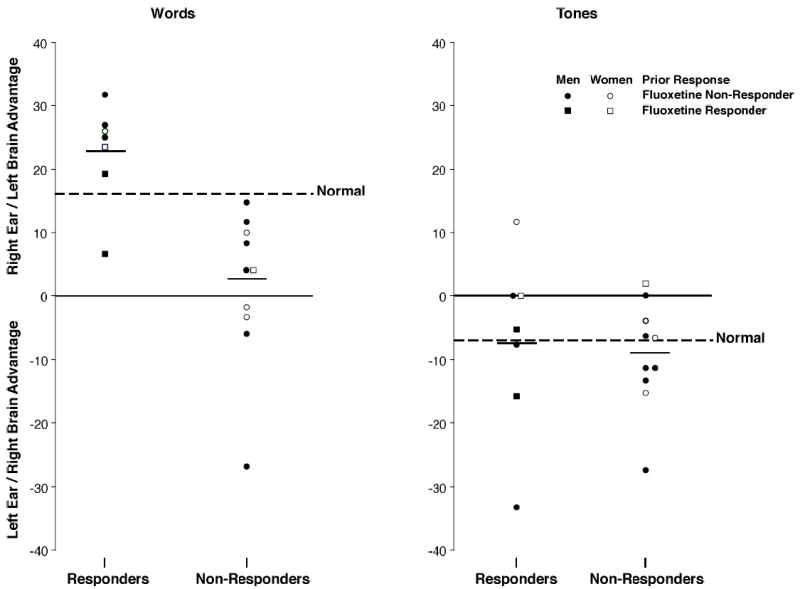
PA scores for individual bupropion responders and nonresponders, and mean PA score for 101 normals on the fused-words and complex-tones tests.
Among patients who previously failed to benefit from fluoxetine (circles in Figure 1), all those who subsequently responded to bupropion had a marked left-hemisphere advantage for words that was greater than the normal mean (dashed line). In contrast, all those who did not respond to bupropion had little or no left-hemisphere advantage, i.e., their PA scores were less than the normal mean. Patients who failed to respond to fluoxetine tended to show a normal right-hemisphere advantage for tones, which did not differ between bupropion responders and nonresponders.
Given the marked difference between bupropion responders and nonresponders in PA scores for words, we further evaluated their potential value for predicting outcome of treatment. As in our prior studies (Bruder et al., 2004), we used the mean PA score for normals (dashed line in Figure 1) as a cutoff score for dividing patients into those with relatively large versus small left-hemisphere advantage and a comparison was made of their treatment response. All 6 of the patients with a left-hemisphere advantage above the normal mean responded to bupropion, whereas only one of 11 patients with a left-hemisphere advantage less than the normal mean responded to bupropion (χ2= 13.25, p<.001). Thus, using this cutoff score to predict bupropion response, the words test had high sensitivity (85.7%), specificity (100%), positive predictive value (100%), and negative predictive value (90.9%).
We also examined whether or not there were differences between bupropion responders and nonresponders in absolute accuracy scores for perceiving tones presented to the left and right ear. A 2 (Bupropion Reponse) by 2 (Ear) ANOVA revealed the expected left ear (right hemisphere) advantage for tones (F=9.49, df= 1,15, P<.01), but there was no significant difference in accuracy between groups (F=1.04, df=1,15, ns). There was also no Bupropion Response by Ear interaction (F= 0.35, df=1,15, ns), which supports the lack of a group difference in right hemisphere advantage for tones. Since words on the Fused Rhymed Words Test fuse to form a single percept and subjects report only a single word on each trial, they are close to 100% correct for reporting the word heard in either ear and therefore the above analysis was not performed for the word test. There was no difference in the number of errors made by responders (mean= 1.7, SD=2.3) and nonresponders (mean= 2.2, SD= 2.7; t= 0.38, df=15, ns).
4. Discussion
This study presents the first evidence that pretreatment asymmetry on a dichotic words test predicts who will or will not benefit from secondary treatment with the antidepressant bupropion. Among depressed patients, most of whom failed to respond to fluoxetine, those who subsequently responded to bupropion had markedly larger left hemisphere advantage for words when compared to nonresponders. All patients having above normal left hemisphere advantage for words responded well to treatment with bupropion, whereas those having less than normal or no left hemisphere advantage had only a 9% response rate to bupropion. The words test showed both high sensitivity (87.5%) and specificity (100%) for predicting response to buproprion. The value of dichotic listening tests for predicting clinical response to the SSRI fluoxetine was demonstrated in our prior studies (Bruder et al., 1996; Bruder et al., 2004). Across two studies, the words test showed moderately high sensitivity (76.3%) and specificity (85.7%) for predicting response to fluoxetine in women, but not in men. Examination of the treatment response for patients with less than normal left hemisphere advantage (Figure 1) indicates that the word test has high negative predictive value (i.e., nonresponder rate for patients predicted to be nonresponders) for both bupropion (90.9%) and fluoxetine (81.8%). Thus, the dichotic word test may prove to be particularly useful as a clinical predictor of patients who are likely to be treatment resistant to these antidepressants.
The difference in asymmetry for perceiving dichotic words between patients who do or do not respond favorably to bupropion is in general similar to that previously seen for fluoxetine (Bruder et al., 1996; Bruder et al., 2004). This may suggest a common element in pathophysiology of patients who respond to these different classes of antidepressant. In this regard, an extensive STAR*D clinical trial found that depressed patients who had unsuccessful treatment with an SSRI showed about the same remission of symptoms after switching to a different SSRI, bupropion or venlafaxine (Rush et al., 2006).
The gender differences for predicting response to fluoxetine (Bruder et al., 2004) do not, however, appear to hold for bupropion. Our prior studies showed that heightened left-hemisphere advantage for dichotic words predicted positive fluoxetine response for women but not men. In the current study, 3 of the 4 patients with a left hemisphere advantage greater than normal who nevertheless failed to respond to fluoxetine were men (see Figure 1). Although sample sizes were small, men who responded to bupropion had significantly larger left-hemisphere advantage for words when compared to nonresponders and this difference was also apparent for women. Also, men who responded to fluoxetine differed from nonresponders in showing reduced right-hemisphere advantage for dichotic tones (Bruder et al., 2004), whereas this difference was not found between bupropion responders and nonresponders. Given that most of the patients who were treated with bupropion had previously failed to respond to fluoxetine, their normal right-hemisphere advantage is understandable. Thus, men who have both larger than normal left-hemisphere advantage for words and right-hemisphere advantage for tones may benefit more from treatment with bupropion than fluoxetine. Women who have a larger than normal left-hemisphere advantage for words would be expected to respond well to fluoxetine, but if they fail to respond, they should nonetheless benefit from treatment with bupropion, whereas those with little or no left-hemisphere advantage may have a poor response to either antidepressant. Although increased left-hemisphere advantage for words appeared to be present for both men and women who responded to bupropion, a study in a larger sample is needed to more adequately evaluate gender effects for this medication.
An important question that needs further research is why hemispheric asymmetry for perceiving dichotic words is related to outcome of treatment with antidepressants. Pretreatment differences in dichotic listening asymmetry between fluoxetine responders and nonresponders did not change following treatment, which suggests that they represent stable, trait characteristics (Bruder et al., 1996). We hypothesized that a characteristic tendency for relatively greater left than right hemisphere activation is associated with better treatment response. This hypothesis is supported by electrophysiologic evidence of differences in hemispheric asymmetry between fluoxetine responders and nonresponders (Bruder et al., 2001). Moreover, neuroimaging studies have found that differences in hemispheric activity in left frontal or temporal lobe regions are related to response to SSRI or other antidepressants (Buchsbaum et al., 1997; Hoehn-Saric et al., 2001; Little et al., 2005). One possible explanation for these findings is that neurotransmitter systems affected by antidepressants may have an asymmetric distribution in the brain or may be asymmetrically disturbed in treatment responsive or nonresponsive subtypes of depression.
Some limitations of this study should also be discussed. First, the patients in this study were participants in an open label study or received open clinical treatment. Although they received systematic treatment with bupropion, there was no active control (e.g., an SSRI) or placebo control group. We therefore can not rule out possible placebo effects and the specificity of the findings to bupropion will need further study. Second, all patients were treated with fluoxetine, most of whom failed to respond, before being treated with bupropion. This limits the generalizability of the findings to patients receiving secondary treatment with bupropion. Third, the categorization of the patients’ treatment response was based on chart review. A psychiatrist, who was blind to the dichotic listening data, gave a treatment response call on the basis of the patient’s global clinical improvement. Although we did not use a predetermined fixed-time point for deciding treatment outcome (e.g., see Papakostas et al., 2006), our goal was to obtain the best possible estimate of clinical response over a relatively narrow treatment trial (7-11 weeks). Fourth, given that all patients were treated with fluoxetine before receiving bupropion, it is possible that fluoxetine was still active and there was an interaction between fluoxetine and bupropion effects. However, the dichotic listening tests were administered before either treatment, and the treatment response call was not made until after patients had received at least 7 weeks of treatment with bupropion alone. Fifth, the number of patients in this study was small. The number of responders and nonresponders are, however, not unlike those in many prior studies of this kind and the sample sizes were sufficient to demonstrate significant differences between bupropion responders and nonresponders. A prospective, double-blind study with larger samples, in which patients are randomly assigned to treatment with either bupropion or an SSRI, is clearly needed to confirm the value of the dichotic word test for predicting response to treatment with these different antidepressants.
In an editorial, Rubinow (2006) commented that the promise of the STAR*D trial may be in the identification of predictors of antidepressant response, which would permit more individualized treatment of depressed patients. Our findings should encourage further study of the clinical value of dichotic listening and other measures of functional brain asymmetry for identifying depressed patients who will most benefit from treatment with different classes of antidepressants.
Acknowledgments
This research was supported in part by a National Institute of Mental Health grant MH36295.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bruder GE, Otto MW, Stewart JW, McGrath P, Fava M, Rosenbaum JF, Quitkin FM. Dichotic listening before and after fluoxetine treatment for major depression: relations of laterality to therapeutic response. Neuropsychopharmnacology. 1996;15:171–179. doi: 10.1016/0893-133X(95)00180-L. [DOI] [PubMed] [Google Scholar]
- Bruder GE, Schneier FR, Stewart JW, McGrath PJ, Quitkin F. Left hemisphere dysfunction during verbal dichotic listening tests in patients who have social phobia with or without comorbid depressive disorder. American Journal of Psychiatry. 2004;161:72–78. doi: 10.1176/appi.ajp.161.1.72. [DOI] [PubMed] [Google Scholar]
- Bruder GE, Stewart JW, Tenke CE, McGrath PJ, Leite P, Bhattacharya N, Quitkin FM. Electroencephalographic and perceptual asymmetry differences between responders and nonresponders to an SSRI antidepressant. Biological Psychiatrty. 2001;48:416–425. doi: 10.1016/s0006-3223(00)01016-7. [DOI] [PubMed] [Google Scholar]
- Buchsbaum MS, Wu J, Siegel BV, Hackett E, Trenary M, Abel L, Reynolds C. Effect of sertraline on regional metabolic rate in patients with affective disorder. Biological Psychiatry. 1997;41:15–22. doi: 10.1016/s0006-3223(96)00097-2. [DOI] [PubMed] [Google Scholar]
- Cook IA, Leuchter AF. Prefrontal changes and treatment response prediction in depression. Seminars in Clinical Neuropsychiatry. 2001;6:113–120. doi: 10.1053/scnp.2001.21844. [DOI] [PubMed] [Google Scholar]
- Dunkin JJ, Leuchter AF, Cook IA, Kasi-Godey JE, Abrams M, Rosenberg-Thompson S. Executive dysfunction predicts nonresponse to fluoxetine in major depression. Journal of Affective Disorder. 2000;60:13–23. doi: 10.1016/s0165-0327(99)00157-3. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. The structural clinical interview for DSM-IV Axis I Disorders – Patient Edition (SCID-I/P, Version 2. 0) Biometric Research Department, New York State Psychiatric Institute; New York, N.Y: 1994. [Google Scholar]
- Hoehn-Saric R, Schlaepfer TE, Greenberg BD, McLoed DR, Pearlson GD, Wong SH. Cerebral blood flow in obsessive-compulsive patients with major depression: effect of treatment with sertraline or desipramine on treatment responders and non-responders. Psychiatry Research: Neuroimaging. 2001;108:89–100. doi: 10.1016/s0925-4927(01)00114-7. [DOI] [PubMed] [Google Scholar]
- Kalayam B, Alexopoulos GS. A preliminary study of left frontal region error negativity and symptom improvement in geriatric depression. American Journal of Psychiatry. 2003;160:2054–2056. doi: 10.1176/appi.ajp.160.11.2054. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR, Quitkin FM, Stewart JW, McGrath PJ, Harrison WM, Rabkin J, Tricamo E, Markowitz JS, Klein DF. Phenelzine v imipramine in atypical depression: A preliminary report. Archives of General Psychiatry. 1984;41:669–677. doi: 10.1001/archpsyc.1984.01790180039005. [DOI] [PubMed] [Google Scholar]
- Little JT, Ketter TA, Kimbrell TA, Dunn RT, Benson BE, Willis MW, Luckenbaugh DA, Post RM. Biological Psychiatry. 2005;57:220–228. doi: 10.1016/j.biopsych.2004.10.033. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Brannan SK, Tekell JL, Silva JA, Mahurin RK, McGinnis S, Jerabek PA. Regional metabolic effects of fluoxetine in major depression: serial changes and relationship to clinical response. Biological Psychiatry. 2000;159:728–737. doi: 10.1016/s0006-3223(00)01036-2. [DOI] [PubMed] [Google Scholar]
- Oldfield RC. The assessment and analysis of handedness: The Edinburgh Inventory. Neuropsychologia. 1971;9:97–113. doi: 10.1016/0028-3932(71)90067-4. [DOI] [PubMed] [Google Scholar]
- Papakostas GI, Worthington JJ, III, Iosifescu DV, Kinrys G, Burns AM, Fisher LB, Homberger CH, Mischoulon D, Fava M. The combination of duloxetine and bupropion for treatment-resistant major depressive disorder. Depression and Anxiety. 2006;23:178–181. doi: 10.1002/da.20181. [DOI] [PubMed] [Google Scholar]
- Pizzagalli D, Pascual-Marqui RD, Nitschke JB, Oakes TR, Larson CL, Abercrombie HC, Schaefer SM, Koger JV, Benca RM, Davidson RJ. Anterior cingulate activity as a predictor of degree of treatment response in major depression: evidence from brain electrical tomography analysis. American Journal of Psychiatry. 2001;158:405–415. doi: 10.1176/appi.ajp.158.3.405. [DOI] [PubMed] [Google Scholar]
- Rubinow DR. Treatment strategies after SSRI failure – good news and bad news. The New Journal of Medicine. 2006;354(12):1305–1307. doi: 10.1056/NEJMe068029. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Wisniewski SR, Stewart JW, Nierenberg AA, Thase ME, Ritz L, Biggs MM, Warden D, Luther JF, Shores-Wilson K, Niederehe G, Fava M. Bupropion-SR, Sertraline, or Venlafaxine-XR after failure of SSRIs for depression. The New England Journal of Medicine. 2006;354(12):1231–1242. doi: 10.1056/NEJMoa052963. [DOI] [PubMed] [Google Scholar]
- Saxena S, Brody AL, Ho ML, Zohrabi N, Maidment KM, Baxter LR. Differential brain metabolic predictors of response to paroxetine in obsessive-compulsion disorder versus major depression. American Journal of Psychiatry. 2003;160:522–532. doi: 10.1176/appi.ajp.160.3.522. [DOI] [PubMed] [Google Scholar]
- Sidtis JJ. The complex tone test: implications for the assessment of auditory laterality effects. Neuropsychologia. 1981;19:103–112. doi: 10.1016/0028-3932(81)90050-6. [DOI] [PubMed] [Google Scholar]
- Stewart JW, Quitkin FM, McGrath PJ, Bruder GE. Do tricyclic responders have different brain laterality? Journal of Abnormal Psychology. 1999;108:707–710. doi: 10.1037//0021-843x.108.4.707. [DOI] [PubMed] [Google Scholar]
- Taylor BP, Bruder GE, Stewart JW, McGrath PJ, Halperin J, Ehrlichman H, Quitkin FM. Psychomotor slowing as a predictor of fluoxetine nonresponse in depressed outpatients. American Journal of Psychiatry. 2006;163:73–78. doi: 10.1176/appi.ajp.163.1.73. [DOI] [PubMed] [Google Scholar]
- Wexler BE, Halwes T. Increasing the power of dichotic methods. The fused rhymed words test. Neuropsychologia. 1983;21:59–66. doi: 10.1016/0028-3932(83)90100-8. [DOI] [PubMed] [Google Scholar]


