Abstract
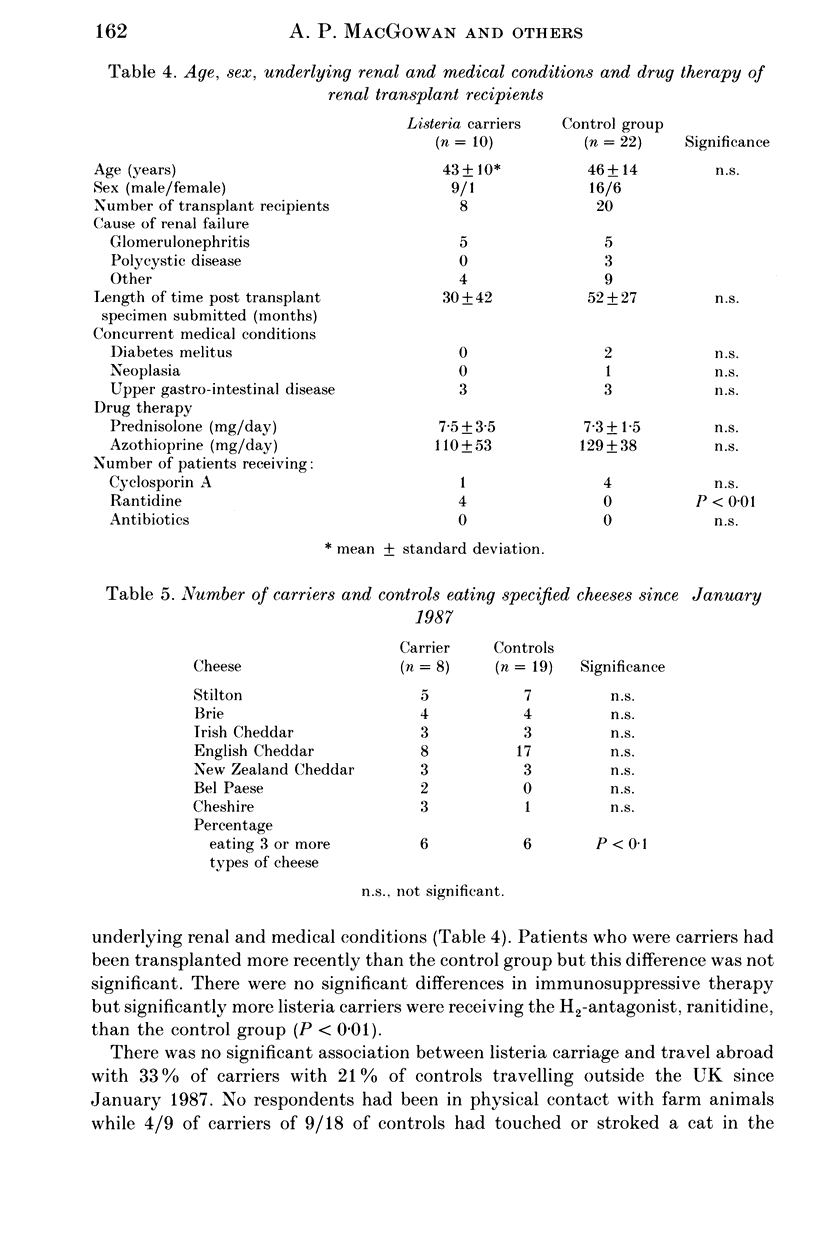
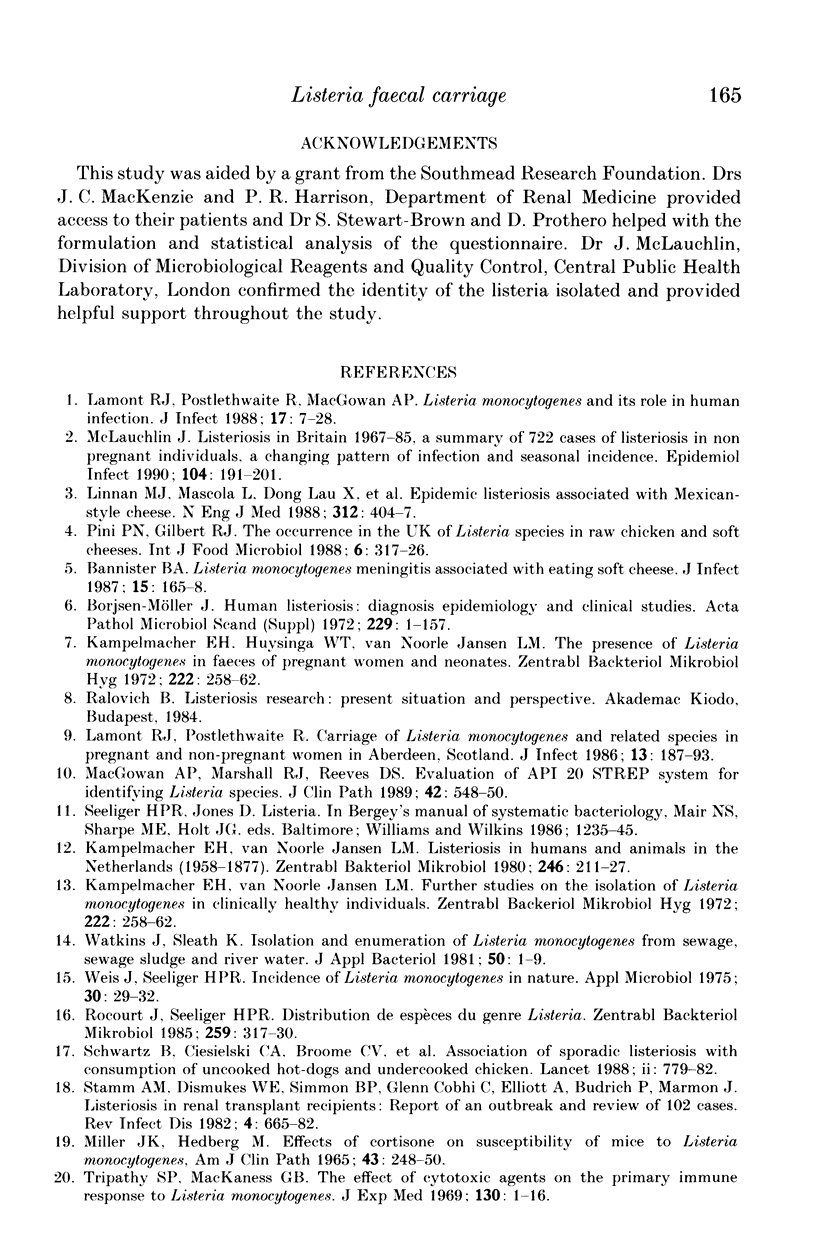
About 2.3% (16/700) of faecal specimens from renal transplant recipients and patients having home haemodialysis as well as patients attending their general practitioners with symptoms of gastroenteritis yielded Listeria species 40% of positive faeces contained more than one Listeria species or serovar. The proportion of positive specimens was similar in all three patient groups. Listeria were isolated from 5.6% (10/177) of renal transplant recipients on one or more occasions over the period of a year. The commonest species was L. monocytogenes and type 4b the commonest serovar. Carriage was more common in July and August than other times of year, and less than 28 weeks in duration. In renal transplant recipients carriage was positively related to treatment with ranitidine, consumption of more than three types of cheese in the previous 20 months, and consumption of English cheddar cheese more than once per week.
Full text
PDF







Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bannister B. A. Listeria monocytogenes meningitis associated with eating soft cheese. J Infect. 1987 Sep;15(2):165–168. doi: 10.1016/s0163-4453(87)93181-1. [DOI] [PubMed] [Google Scholar]
- Breer C., Schopfer K. Listeria and food. Lancet. 1988 Oct 29;2(8618):1022–1022. doi: 10.1016/s0140-6736(88)90775-1. [DOI] [PubMed] [Google Scholar]
- Ho J. L., Shands K. N., Friedland G., Eckind P., Fraser D. W. An outbreak of type 4b Listeria monocytogenes infection involving patients from eight Boston hospitals. Arch Intern Med. 1986 Mar;146(3):520–524. [PubMed] [Google Scholar]
- Kampelmacher E. H., van Noorle Jansen L. M. Listeriosis in humans and animals in the Netherlands (1958-1977). Zentralbl Bakteriol A. 1980 Mar;246(2):211–227. [PubMed] [Google Scholar]
- Lamont R. J., Postlethwaite R. Carriage of Listeria monocytogenes and related species in pregnant and non-pregnant women in Aberdeen, Scotland. J Infect. 1986 Sep;13(2):187–193. doi: 10.1016/s0163-4453(86)93121-x. [DOI] [PubMed] [Google Scholar]
- Lamont R. J., Postlethwaite R., MacGowan A. P. Listeria monocytogenes and its role in human infection. J Infect. 1988 Jul;17(1):7–28. doi: 10.1016/s0163-4453(88)92236-0. [DOI] [PubMed] [Google Scholar]
- MILLER J. K., HEDBERG M. EFFECTS OF CORTISONE ON SUSCEPTIBILITY OF MICE TO LISTERIA MONOCYTOGENES. Am J Clin Pathol. 1965 Mar;43:248–250. doi: 10.1093/ajcp/43.3.248. [DOI] [PubMed] [Google Scholar]
- MacDonald T. T., Carter P. B. Cell-mediated immunity to intestinal infection. Infect Immun. 1980 May;28(2):516–523. doi: 10.1128/iai.28.2.516-523.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacGowan A. P., Marshall R. J., Reeves D. S. Evaluation of API 20 STREP system for identifying Listeria species. J Clin Pathol. 1989 May;42(5):548–550. doi: 10.1136/jcp.42.5.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLauchlin J. Human listeriosis in Britain, 1967-85, a summary of 722 cases. 2. Listeriosis in non-pregnant individuals, a changing pattern of infection and seasonal incidence. Epidemiol Infect. 1990 Apr;104(2):191–201. doi: 10.1017/s0950268800059355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pini P. N., Gilbert R. J. The occurrence in the U.K. of Listeria species in raw chickens and soft cheeses. Int J Food Microbiol. 1988 Jun;6(4):317–326. doi: 10.1016/0168-1605(88)90025-6. [DOI] [PubMed] [Google Scholar]
- Rocourt J., Seeliger H. P. Distribution des espèces du genre Listeria. Zentralbl Bakteriol Mikrobiol Hyg A. 1985 May;259(3):317–330. [PubMed] [Google Scholar]
- Schwartz B., Ciesielski C. A., Broome C. V., Gaventa S., Brown G. R., Gellin B. G., Hightower A. W., Mascola L. Association of sporadic listeriosis with consumption of uncooked hot dogs and undercooked chicken. Lancet. 1988 Oct 1;2(8614):779–782. doi: 10.1016/s0140-6736(88)92425-7. [DOI] [PubMed] [Google Scholar]
- Sizmur K., Walker C. W. Listeria in prepacked salads. Lancet. 1988 May 21;1(8595):1167–1167. doi: 10.1016/s0140-6736(88)91983-6. [DOI] [PubMed] [Google Scholar]
- Stamm A. M., Dismukes W. E., Simmons B. P., Cobbs C. G., Elliott A., Budrich P., Harmon J. Listeriosis in renal transplant recipients: report of an outbreak and review of 102 cases. Rev Infect Dis. 1982 May-Jun;4(3):665–682. doi: 10.1093/clinids/4.3.665. [DOI] [PubMed] [Google Scholar]
- Tripathy S. P., Mackaness G. B. The effect of cytotoxic agents on the primary immune response to Listeria monocytogenes. J Exp Med. 1969 Jul 1;130(1):1–16. doi: 10.1084/jem.130.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins J., Sleath K. P. Isolation and enumeration of Listeria monocytogenes from Sewage, Sewage Sludge and River Water. J Appl Bacteriol. 1981 Feb;50(1):1–9. doi: 10.1111/j.1365-2672.1981.tb00865.x. [DOI] [PubMed] [Google Scholar]
- Weis J., Seeliger H. P. Incidence of Listeria monocytogenes in nature. Appl Microbiol. 1975 Jul;30(1):29–32. doi: 10.1128/am.30.1.29-32.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]


