Abstract
The development of regional data-sharing among healthcare organizations is viewed as an important step in the development of health information technology (HIT), but little is known about this complex task. This is a case study of a regional perinatal data system that involved four hospitals, together responsible for over 10,000 births annually. Using standard qualitative methods, we chronicled project milestones, and identified 31 “critical incidents” that delayed or prevented their achievement. We then used these critical incidents to articulate six organizational capacity domains associated with the achievement of project milestones, and a seventh domain consisting of organizational incentives. Finally, we analyzed the relationship of milestone achievement to the presence of these capacities and incentives. This data center case suggests four requirements for sharing data across organizations: 1) a readiness assessment; 2) a perceived mandate; 3) a formal governance structure; and 4) a third party IT component.
Introduction
In 2004, the President of the United States established the Office of the National Coordinator for Health Information Technology (ONCHIT) to provide leadership for the national development of an interoperable health information technology (HIT). 1,2 The implementation of such a technology would improve “the coordination of care and information among hospitals, laboratories, physician offices, and other ambulatory care providers.” 3 To date, most research regarding the implementation of HIT has focused on intra-organizational efforts, and it is evident that many of these undertakings fail. 4 A systematic review of the literature found that the efficacy of HIT for healthcare quality improvement has primarily been demonstrated by only four benchmark institutions, and whether other institutions can demonstrate similar results is unclear. 5 Furthermore, only 1% of the systems studied in the review had “capabilities that allowed systems from different facilities to connect with each other and share data inter-operably.” 6 This literature suggests that further understanding is needed regarding organizational change, incentives, work redesign, human factors, and project management issues to ensure successful implementation of HIT on a national scale.
Case Description
The project, a perinatal data center, was intended to link data regarding mothers and newborns across four hospitals in the city of Los Angeles. The funder was a relatively new, publicly-funded philanthropic organization that was interested in tracking the provision of high quality obstetrical and newborn care to at-risk families. It was proposed that the data from Hospital A, an academic hospital with neonatal services, be linked first to Hospital B, an academic government hospital with both obstetrical and neonatal services and a delivery volume of about 1,200 births per year. Once successfully joined, two more community hospitals would be added, one with corporate ownership (Hospital C), and one with non-profit ownership (Hospital D). Hospitals C and D each had over 4,000 annual births and a high referral rate to the two academic hospitals.
Approximately $600,000 was provided to Hospital A over calendar years 2003–2004. Although the project was initiated as a feasibility study, some of the leadership had expected to achieve a working system within the study period. The content of the data to be shared was primarily limited to data that were already being collected as part of ongoing operations, and was intended to provide data only for research purposes or for feedback regarding hospital operations, such as quality improvement efforts. The data linkages would not be operable in real-time and would not be used for clinical care. Patient identifiers were required in order to link multiple births to the same mother, and to track newborns across hospitals.
Methods
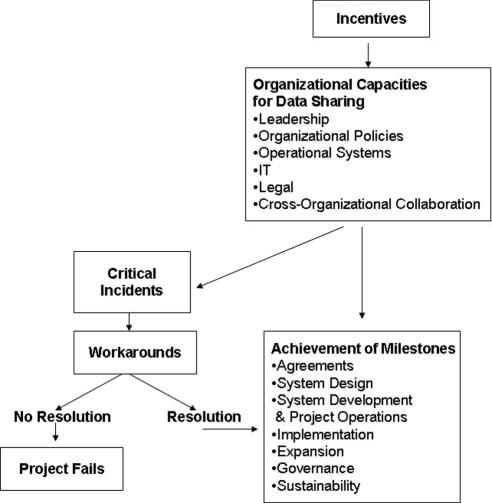
We used standard qualitative case study methodologies, 7 utilizing the conceptual framework in ▶ to guide our data collection efforts. This framework was developed from Snyder-Halpern’s framework for organizational readiness for IT innovation, 8 and it hypothesizes that adequate organizational capacities and incentives allow successful achievement of project milestones. In this case, these capacities and incentives usually operated on two levels: at the inter-organizational level of the project, and within each of the individual organizations.
Figure 1.
Conceptual framework.
We thoroughly reviewed all archival documents associated with the project, and conducted semi-structured interviews with available participants. The data sources that were used to examine the objectives and assess the progress of the project with respect to its milestones are listed in Appendix 1, available as a JAMIA online-only data supplement at www.jamia.org. This appendix also provides a summary of the evidence for the importance of organizational capacities by project milestone.
Analyses of “critical incidents” have played an important role in the understanding and improvement of patient care processes, 9 and HIT has adopted this terminology in reference to computer system implementation. 10 In this context, critical incidents are problematic situations that require resolution in order to achieve project milestones. How and if these critical incidents are resolved not only tells us whether or not the organization has the capacity to mobilize its resources and generate a workaround for the problem, but also whether it has strong enough incentives to do so. Through analysis of the critical incidents that arose during the case, we uncovered details of the organizational capacities and incentives that appear necessary to achieve an inter-hospital clinical information system. A total of 31 critical incidents and their workarounds are described in Table 1, available as a JAMIA online-only data supplement at www.jamia.org. Table 1 also includes the organizational capacities and incentives that were tested by these critical incidents.
Discussion
As organizations and funders prepare to embark on inter-organizational data-sharing endeavors, there are many lessons to be learned from past undertakings. Four of these lessons are illustrated by this case. The first two operate at both intra- and inter-organizational levels, and the second two are specifically relevant to inter-organizational systems.
Readiness Assessment
First, the case of this multi-hospital data center is consistent with current research showing that the detailed work involved in such an endeavor is often overlooked. 11 When such a project is first proposed, funding must be sought, either internally or externally, and an agreement developed. That agreement occurs between the leadership of the project, the organizations that will be providing the patient data, and potentially an external funder. It may also include some third parties, such as legal or IT consultants. Not incorporated at this time are the numerous formal and informal agreements that must also be negotiated among those running the project and other “in-house” organizational staff. These may include lawyers, doctors, nurses, medical records staff, bioengineers, IT staff, vice presidents, department and division heads, financial officers, IRB officers, and risk managers. Our case suggests that the demands placed by such a project may be quite burdensome, and are likely to conflict with current work processes or require additional effort on behalf of many individuals. In this case, such demands remained unmentioned or unexplored until funding was secured. Then, once funded, these demands were addressed on an ad hoc basis, with the project team working largely “under the radar” in an effort to gain cooperation. This led to many critical incidents in the project timeline: since cooperation was not predictable, the project team was constantly devising creative workarounds to keep the project on track. A large number of the critical incidents encountered in this case were specifically related to problems occurring across participating organizations, such as differences in Institutional Review Board (IRB) requirements, and disagreements regarding governance structures, finances, and personnel commitments.
These complex challenges suggest that any organization considering whether to help launch or join an existing data sharing collaborative should first undertake a careful evaluation of its own organizational capacities and incentives. A “readiness” assessment of the gap between what is present and what is planned technically must be met with a similar assessment of the gap between organizational capacities as they are, and as they will need to be to complete the project. 12 Furthermore, the project team must determine if the incentive structure is adequate to bridge these gaps. Such a readiness assessment would achieve a realistic appraisal of the likelihood for cooperation among the various intra- and inter-organizational constituents.
We derived a set of constituent dimensions of organizational capacities and incentives for clinical data-sharing from our study of this case which is included in Appendix 2, available as a JAMIA online-only data supplement at www.jamia.org. These dimensions may serve as a framework for initiating readiness assessment discussions as organizations contemplate sharing clinical data across their own departments and across organizations.
Perceived Mandate
Committed top-level leadership appears to be essential for successful system implementation. Some of the problems that plagued this project could only have been overcome with committed top-level leadership, such as the struggle for adequate resources and the turnover of key project personnel.
Inclusion of the project within the strategic plan of each participating organization, and holding specific administrators accountable for its implementation, would have indicated the presence of internal operational incentives for the organization, and could have assured ongoing funding. External incentives, such as regional mandates for data-sharing to facilitate regulatory efforts, are likely to be even more compelling for such data sharing efforts. Recently, the California Department of Health Services required participation in state-wide data-sharing activities to obtain Medicaid reimbursement for neonatal intensive care units (NICU), 13 which brought about nearly universal NICU participation. 14
With respect to achieving accountability, funding mechanisms need careful consideration. Brailer, in his assessment of the disbanding of a large inter-organizational clinical data sharing effort, stressed the importance of using contracts instead of grants, “since grants do not provide mechanisms for accountability the way that contracts do.” 15
Formal Governance Structure
Another important lesson about the data-sharing operations of a collaborative is that long-term viability, and perhaps even early cooperative behavior and trust, is likely to require a formal, and potentially, independent governance structure. In this case, leadership from multiple hospitals had different visions and expectations of the project, creating conflicts regarding who should be providing further resources and support. Governance discussions suffered because the leadership was reluctant to create the rules and policies for sharing clinical data in a way that was acceptable to all hospitals. The establishment of a governance structure before undertaking the technical development of a data-sharing system would have resolved these issues much sooner, as it requires that the founding members agree upon joint objectives, resources and responsibilities.
Such a governance structure establishes an overarching mechanism for obtaining and administering funds. This case demonstrates that project funds must be available prior to contracting with a potential funder, in order to determine the scope of work. Further funds, to determine the feasibility of the system’s objectives, to examine the potential data to be shared, to determine capacities and incentives of the participants, and to help create the governance structure, would be optimal, as these tasks all must occur in advance of designing a system.
Formal Third Party IT Component
The need for patient identifiers in order to link mother and newborn, and to follow patients across hospitals had serious technical implications, and raised the level of expertise required from IT personnel. Hospital policies were also challenged because patients could now be identified, which escalated scrutiny and uncertainty on behalf of IRB members and personnel contributing data, and generated different requirements at different hospitals. These findings suggest the need for a highly experienced and resilient external IT component of the system. The IT entity should not only have an independent fiduciary responsibility to each participating hospital for the standardization, organization, maintenance, aggregation, and release of data, but also must be enabled to respond to the needs of the collaborative as a whole.
Conclusion
In summary, this case demonstrates the complexity of clinical data-sharing, both within and across organizations. The ability to achieve project milestones depends heavily on organizational capacities, and on the incentives to dedicate the required resources to surmount the many associated challenges. Policy makers addressing national HIT strategies must recognize the complexity of the effort and the magnitude of the required investment if we wish to reach the goal of nation-wide interoperable HIT.
References
- 1.Press Briefing by Scott McClellan, April 27, 2004http://www.whitehouse.gov/news/releases/2004/04/print/20040427-3.htmlAccessed Oct 3, 2007.
- 2.Office of the National Coordinator for Health Information Technology (ONC), Missionhttp://www.hhs.gov/healthit/mission.htmlAccessed Oct 3, 2007.
- 3.Executive Order: Incentives for the Use of Health Information Technology and Establishing the Position of the National Health Information Technology Coordinator, Section 1e. April 27, 2004http://www.whitehouse.gov/news/releases/2004/04/print/20040427-4.htmlAccessed Oct 3, 2007.
- 4.Office of the National Coordinator for Health Information Technology (ONC), Barriers to Adoptionhttp://www.hhs.gov/healthit/barrierAdpt.htmlAccessed Oct 3, 2007.
- 5.Chaudry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care Ann Intern Med 2006;144:E12-E22. [DOI] [PubMed] [Google Scholar]
- 6.Chaudry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care Ann Intern Med 2006;144:E12-E22pE14. [DOI] [PubMed] [Google Scholar]
- 7.Stake RE. The Art of Case Study ResearchThousand Oaks: Sage Publications; 1995.
- 8.Snyder-Halpern R. Indicators of organizational readiness for clinical information technology/systems innovation: A Delphi study Int J Med Inform 2000;63:179-204. [DOI] [PubMed] [Google Scholar]
- 9.O’Connor J, Jeavons S. Nurses’ perceptions of critical incidents J Adv Nursing 2003;41(1):53-62. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan B. Addressing organizational issues into the evaluation of medical systems J Am Med Inform Assoc 1997;4(2):94-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiner BJ, Savitz LA, Bernard S, Pucci LG. How do integrated delivery systems adopt and implement clinical information systems Health Care Manage Rev 2004;29(1):51-66. [DOI] [PubMed] [Google Scholar]
- 12.Heeks R. Health information systems: Failure, success and improvisation Int J Med Inform 2006;75:125-137. [DOI] [PubMed] [Google Scholar]
- 13.HRIF Program Reporting Requirements, CCS High Risk Infant Follow-up Programhttp://www.dhs.ca.gov/PCFH/CMS/hrif/default.htm 2006. Accessed Oct 3, 2007.
- 14.Calfornia Perinatal Quality Care Collaborative, Overviewhttp://www.cpqcc.org/overview.htm 2006. Accessed Oct 3, 2007.
- 15.Brailer DJ. From Santa Barbara to Washington: A person’s and a nation’s journey toward portable health information. Health Affairs 26(5): w581-w588 (published online 1 Aug 2007);10.1377/hlthaff.26.5.w581. [DOI] [PubMed]