Abstract
Objective
This study sought to explore the relationship of workarounds related to the implementation of an electronic medication administration record and medication safety practices in five Midwestern nursing homes.
Design
As a part of a larger study, this qualitative evaluation was conducted to identify workarounds associated with the implementation of an electronic medication administration record. Data were collected using multimethods including direct observation, process mapping, key informant interviews, and review of field notes from medication safety team meetings.
Measurements
Open and axial coding techniques were used to identify and categorize types of workarounds in relation to work flow blocks.
Results
Workarounds presented in two distinct patterns, those related to work flow blocks introduced by technology and those related to organizational processes not reengineered to effectively integrate with the technology. Workarounds such as safety alert overrides and shortcuts to documentation resulted from first-order problem solving of immediate blocks. Nursing home staff as individuals frequently used first-order problem solving instead of the more sophisticated second-order problem solving approach used by the medication safety team.
Conclusion
This study provides important practical examples of how nursing home staff work around work flow blocks encountered during the implementation of technology. Understanding these workarounds as a means of first-order problem solving is an important consideration to understanding risk to medication safety.
Background
The Institute of Medicine (IOM) Report “To Err is Human” has sparked a nationwide focus on preventable medical error. 1 Among the medical error reported it has been noted that 25% of medication-related injury could have been prevented. 2 Adverse drug events often have been found to be preventable in both acute and long-term care settings. Thomas et al. 3 found that adverse drug events accounted for 19.3% of medication errors in hospital settings, with as many as 35.1% of those adverse drug events deemed to be preventable. Gurwitz et al. 4 determined that 42% of nursing home adverse drug events were preventable. Findings related to preventable medication error suggest that new systems of medication administration must be explored.
As new systems have been explored to support medication administration, technology has become a critical part of these discussions. 1 In response to ongoing patient safety challenges, health care organizations have implemented a variety of technological mechanisms to reduce medication errors such as computerized physician order entry, 5 electronic medication administration record, 6 and clinical decision support systems. 7 However, implementation of technology has not been without risk. As technology has been developed and tested, new types of medical error and risk for error have occurred. 8,9 Although some new risks were expected, 10 more research must be focused on the human-technology interface to maximize the impact of technology on medical error.
Understanding the Human–Technology Interface
The human-technology interface was addressed at a recent conference sponsored by the Agency for Healthcare Research and Quality (AHRQ). 11 The conference focused on two important themes. First, although technology is an important innovation, understanding how people use (or do not use) the technology is arguably more important, and second, there are unintended consequences that arise from technology implementation that may have critical implications for patient safety. 9 These considerations raise critical questions to providers as they seek to improve systems with technology.
Despite the widespread adoption of technology to reduce medication administration errors, 12-15 researchers have yet to adequately explore the impact of these technologies on underlying work process and work flow. Many systems implemented to reduce the opportunity for medication error function by introducing work flow blocks (i.e., computerized alerts or warnings) that force the health care professional to carefully reconsider a process that could be unsafe. 7 Work flow blocks, whether intentionally designed for safety or unintentional artifacts of ineffective technological designs, are extremely common and very disruptive to staff. Work flow blocks tend to distract staff from patient care issues and can result in errors. 16-18 To address this problem, many nurses engage in problem-solving behaviors that involve bypassing new technology or adapting work process so as to minimize disruption in work flow. 19,20 These problem-solving behaviors have been conceptualized as workarounds (WA); this study explores the manner in which technological WA are associated with medication safety risks.
Workarounds
Workarounds have been defined by Kobayashi et al. 21 as “informal temporary practices for handling exceptions to normal work flow” (pp. 1561). A common WA example would be overriding an alert to a potentially dangerous medication. Because there has been little attempt to capture the manner in which health care professionals work around such blocks to reduce disruptions, there has subsequently been no attempt to capture the extent to which WA can lead to patient safety concerns.
Exploration of WA, blocks, and the risk to patient safety is an important consideration as technology implementation moves forward in health care. As the literature has unveiled hidden risks associated with technology implementation, 9 there is a need to understand the manner in which health care professionals interact with new technology and how work processes are adjusted as a result of technology implementation. The purpose of this study is to describe the underlying nature of WA in relation to technology implementation of an electronic medication administration record in five Midwestern nursing homes and to identify the potential risks of WA on medication safety.
Method
Sample and Data Collection Procedures
Medication safety process reviews were completed in nursing homes participating in a larger medication safety grant funded by the Agency for Healthcare Research and Quality (AHRQ). The grant supported a partnership among five nursing homes, the University of Missouri-Columbia, and a technology vendor (Optimus EMR Inc., formerly OneTouch Technologies, Irvine, CA).
As part of the larger AHRQ study, each nursing home implemented a fully integrated electronic health record (EHR) and an electronic medication record (eMAR). The eMAR system, an electronic point of care tool, directed and recorded medication administration through a medication cart touch screen application on a wireless laptop computer. The eMAR system provided several alerts and signaling features that prompted staff of potential medication safety issues. Multidisciplinary medication safety teams were established in each nursing home before the implementation of technology and continued to meet monthly throughout the study with the goal of maximizing technology to impact medication safety. 6 Approval for this study was obtained by the University of Missouri Institutional Review Board.
The five Midwestern nursing homes were from three states and a mix of urban, rural, profit, and not-for-profit nursing homes. The nursing homes ranged from 60 to 200 beds. Although the nursing homes demonstrated risk-taking and innovation as they embraced the EHR, they faced the same organizational challenges as most nursing homes in terms of resources, leadership experiences, and staff turnover.
Workarounds were consistently noted across the five nursing homes in three routine aspects of the medication administration system. The three aspects of the medication administration system were those that encompassed medication order entry, the nursing home-pharmacy interface, and the actual delivery of the medication to the resident. The medication order entry included receiving the medication order from the physician, entering the medication order into eMAR, reconciling the medication order with the resident’s medical record, and communicating the new order to medication administration staff. The nursing home-pharmacy interface included communicating the new medication order to pharmacy, receiving the medication from pharmacy, and placing the medication on the medication cart in preparation for administration to the resident. The actual delivery of the medication to the resident included verifying the medication to be administered matched the order in eMAR following the five rights of medication administration (right resident, right medication, right dose, right route, and right time), and documenting the medication as given.
These three aspects of the medication administration system were explored using a mixed approach that included direct staff observations, process mapping, key informant interviews, and review of medication safety team field notes. The complete medication administration system was mapped before the implementation of technology and again six months after the implementation of technology to determine how critical aspects of the medication administration system had changed.
Direct observation of the medication administration process occurred through a naïve observation procedure. 22 A nurse from the research team observed the medication administration without prior knowledge of what medications were to be given. Inter-rater reliability was established for the naïve observation process through simultaneous observations and result comparisons between the research nurse and principal investigator across each of the five nursing homes. Before the implementation of technology, a total of 43 nursing home staff were observed to determine the current medication administration system in practice. At six months after implementation, a total of 45 nursing home staff were observed from the five nursing homes to determine how medication administration practices had changed with the addition of technology. Observations were conducted by either the research nurse or principal investigator with results comparison made after observation.
To supplement the direct observation, process mapping was completed for each nursing home by creating step-by-step flow diagrams of medication order entry, the nursing home-pharmacy interface, and actual delivery of the medication to the resident. Multiple iterations of the process mapping were completed with medication safety team member feedback integrated into each iteration until consensus was obtained. Key informant interviews were conducted to provide points of clarification to both the observations and process mapping.
In addition to direct observations, process mapping, and key informant interviews, medication safety team meeting field notes were reviewed to identify staff communication and discussion of related work flow blocks and WA. Work flow blocks were discussed as barriers encountered by staff members within the medication administration system. Workarounds were subsequently discussed by staff members as a means to get the work done in spite of the work flow block.
Analysis
Field notes from the feedback of nursing home staff during the process mapping provided initial insight to work flow blocks and WA experienced. Using the step-by-step process maps and identified work flow blocks and WA as a guide, field notes from the medication observations and the medication safety team meetings were then reviewed in depth to further explicate work flow blocks and related WA occurrences. An open coding technique was used to categorize data according to the identified work flow blocks and WA.
These categorized work flow blocks and WA were again reviewed with the medication safety team members using the process maps as a guide. The work flow blocks were further discussed for underlying cause and then linked to the type of WA that occurred as a result of the work flow block. An axial coding technique was used to identify and categorize the causal links between the work flow blocks and the WA events.
Results
Workarounds presented in two distinct patterns: WA related to blocks introduced by technology and WA related to organizational processes that had not been reengineered to integrate effectively with the implementation of technology. Workarounds resulted as nursing home staff attempted to individually problem solve how to overcome a work flow block rather than seeking to identify and understand the underlying cause of the work flow block.
Workarounds Related to Technology Implementation
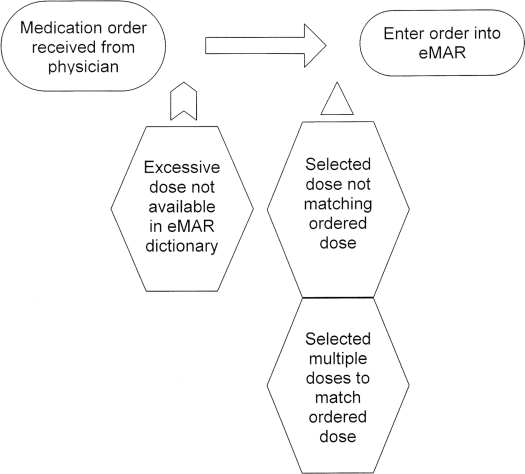
Workarounds related to technology implementation were the result of both intentional technology blocks designed to enhance resident safety and unintentional technology blocks resulting from ineffective technology design. For example, within the computerized order entry (COE) system, intentional blocks were designed to prevent ordering of excessive medication doses. To work around this block, one staff member reported intentionally selecting a medication dose in COE that did not match the physician’s order simply to get the medication “into the system.” As the incidence of excessive dosing was encountered, licensed staff from each of the five nursing homes were most often observed entering multiple doses of the same medication to obtain the full ordered dose instead of discussing the excessive ordered dose with the pharmacist or physician (▶).
Figure 1.
New medication order entry.
Another safety block designed by technology was a dual medication administration documentation system that first led staff to document preparation of the medication and then to return to document actual administration of the medication. This dual documentation system, designed to ensure that the medication prepared was actually the medication administered, was viewed as cumbersome by many staff because they had not documented in this manner before the implementation of technology. During observations in each of the five nursing homes, most staff documented both preparation and administration before actually administering the medications.
Another safety feature of the eMAR system forced the association of monitoring/assessment and medication administration to identify potential side effects and adverse events. The technology provided an intentional block to prevent documentation of the medication until assessment data was entered into the system. Medication administration staff now had to stop before medication administration and check vital signs or assess for clinical conditions such as pain or behaviors. Staff found this intentional block time consuming. Before eMAR, staff often disassociated monitoring parameters such as vital signs and assessments with the therapeutic impact of the medications by not routinely collecting assessment data during medication administration. Staff reported circumventing the intentional block by not entering necessary assessment parameters into the eMAR system.
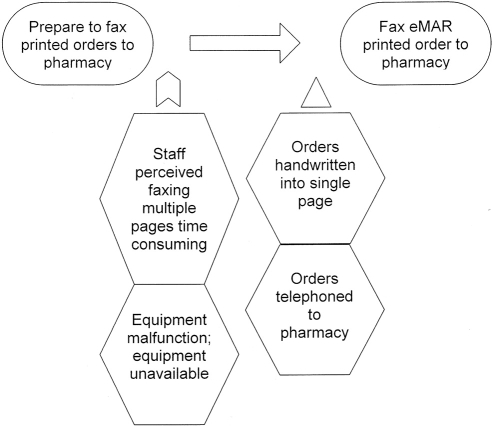
Unintentional technology blocks resulted in frustrated staff. An example of an unintentional block related to medication order printouts. On completion of each medication order, an individual sheet of paper was printed. This created large numbers of pages for a single set of new orders and complicated routine fax communication between the nursing home and pharmacy. This was compounded by inaccessible and limited fax capabilities in the nursing home. The unintentional block led many of the observed staff to call new orders to the pharmacy rather than fax printed orders, thus circumventing a critical safety feature of COE. In an extreme WA, a staff member in one nursing home reported rewriting new orders on a separate sheet of paper so that only one faxed sheet would have to be sent to pharmacy, once again working around the safety feature of COE (▶).
Figure 2.
Pharmacy and nursing home communication.
Another unintentional technology block related to the speed of the wireless connection and the design of the computer screens. To view specific aspects of the residents’ EHR, staff were required to switch from screen to screen. Rather than taking the time to view various screens, most staff were observed using handwritten notes and consulting other staff to obtain critical resident specific information.
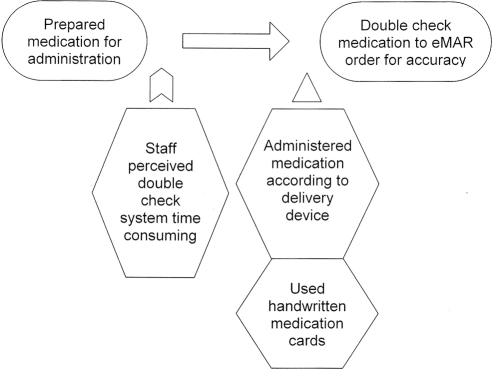
Workarounds Related to Ineffective Reengineering of Related Processes
Similar to WA occurring with technology, WA also existed when related processes had not been effectively reengineered. For example, although the preparation and administration documentation points could provide for a safety check to ensure that the residents were receiving the right medication, staff who perceived the double-check system as time consuming resolved this block by simply pulling medications from the medication drawers without any step for medication to order checking. In some cases staff relied on pretechnology double-check methods such as handwritten medication cards, which again circumvented the safety features provided through the implementation of technology (▶).
Figure 3.
Medication preparation.
Workarounds related to limited resources also existed such as inadequate fax machines. In one nursing home, 150 residents and their related medication orders were served by one fax machine on evenings and weekends. The work flow block introduced by limited fax capacity was resolved by many phone calls to pharmacy. Other nursing homes reported similar problems when fax machines were malfunctioning.
Discussion
When considering the phenomenon of WA in the context of implementing technology, both intentional and unintentional blocks must be considered. Workarounds related to intentional blocks such as overriding alerts for inappropriate dosing are of particular concern to safety in the nursing home. Judge et al. 23 found a relatively low response to medication safety alerts from prescribers when using COE in a long-term care setting. Although these computerized alerts offer important features to enhance resident safety, overriding the alert undermines the safety feature rendering it potentially useless.
Unintentional blocks also create staff frustration. In a study describing perceptions of staff involved in implementing of a computerized physician order entry (CPOE) system, Ash et al. 24 described unintentional technology blocks as “quirks in the system.” Staff discussed working around these blocks by “tricking the system” to get their work done. To reduce frustration, WA such as free text charting and using other staff to complete the work were perceived as necessary to successfully implement technology.
Workarounds that occur when related processes are not effectively reengineered also pose risk to medication safety. In a study identifying the role of CPOE in facilitating prescription error risk, Koppel et al. 9 found WA such as post hoc documentation and the use of parallel paper systems for documenting medication administration caused confusion and risk of information loss within the electronic system.
Understanding both conditions in which WA are likely to occur is critical for the successful merging of technology within an existing work flow. 25,26 In the present study, the introduction of the new technology resulted in two separate and distinct root causes for WA. The first cause was related to technological design, and the second cause was failure to reengineer related processes to interface with the implementation of the technologically driven medication administration system.
Workarounds and Problem-solving Behavior
Because the underlying goal of a WA is to complete a task despite a block, WA may be seen as important problem-solving behaviors within organizations. Initially, frustrated staff who were unable to get the work done associated all blocks with the implementation of technology. The blocks led to many types of WA. Workarounds are often considered first-order problem solving 20 in which staff create a mechanism to work around a problem without trying to change the underlying cause that created the problem. The challenge with first-order problem solving is that staff are often very good at quickly addressing problems in work flow (e.g., by engaging in WA), which can simply exacerbate operational failures. 27,28
Although staff are often effective at first-order problem solving, it was second-order problem solving that truly was able to integrate technology into the nursing home work flow. According to Tucker and Edmondson, 20 second-order problem solving attempts to get to the underlying root cause of the problem. Second-order problem solving occurred as underlying issues of work flow blocks were identified by the medication safety team members. The intentionally designed technological blocks were discussed in the context of WA. The work flow diagrams created by the medication safety teams facilitated integration of technology and work flow processes to maximize resident safety. In addition, the medication safety team created meaningful ways to inform and educate other staff about the blocks and how work flow had been adapted to ensure resident safety.
Second-order problem solving was enhanced by the presence of the medication safety team. In most cases, competing demands, the absence of front-line managers in the problem-solving process, and the inability of staff to independently be vigilant impedes second-order problem solving. 28 Although members of the medication safety team became effective at second-order problem solving, those outside of the medication safety team were not. These staff continued to attempt first-order problem solving strategies, particularly early in the implementation phase of the project. To bring all staff into second-order problem solving and related solutions required open communication in which staff talked openly about the blocks they faced. Nurse leaders and medication safety team members served as conduits to the remainder of the staff in providing ongoing information about the integration of technology and existing processes and provided critical opportunities for all staff to be able to fully disclose their concerns related to underlying issues. This culture of safety orientation also facilitated more discussion about potential medication errors (near misses) and other adverse drug events. 29
As noted by Roberto et al., 30 open discussion increases the likelihood that organizations will detect and address ambiguous threats, a signal of an operational problem that may suggest future harm. By carefully monitoring work flow and discussing blocks, staff can identify potential threats where WA may be signaling a potential resident safety risk. These investigators suggest that organizations that take these early threats seriously are better equipped to manage solutions to the threat and minimize downstream damage.
Roberto et al. 30 identify the potential utility of WA in diagnosing and addressing work flow problems that lead to patient risks, ultimately impacting patient safety. To the extent that procedures are put in place to identify blocks, they can either be eliminated or better justified to eliminate WA. Moreover, careful study of WA may actually suggest better and safer ways to get the work done; however, this is only possible when attempts are made to capture them.
Limitations and Suggestions for Future Research
We recognize a number of limitations to the present study, including the limited number of staff observations that occurred across the five nursing homes. As such, the analysis in this study was a secondary analysis of field and meeting notes as well as process mapping; it is possible that the true frequency of WA occurrences was not captured and that additional WA were not documented. Additionally, isolated WA, such as the staff member who rewrote new orders on a separate piece of paper, may simply be outliers given a specific situation. Along those lines, although similar WA occurrences were noted across each of the five nursing homes, WA appear to be locally based; that is, they are dependent on the specific work processes, work context, and individual staff members involved. As a result, although we believe the types of WA we have documented will generalize to other settings, the specific examples of WA may not. Future research that confirms the nature of WA in other settings will be valuable in supporting a more general WA framework.
Conclusion
This study provides important practical examples of how nursing home staff work around work flow blocks encountered during the implementation of technology. Understanding these WA as a means of first-order problem solving is an important consideration to understanding the risk to medication safety. As new technologies are introduced, continued monitoring to identify work flow is needed so appropriate changes can be made to address the underlying problems that create work flow blocks ultimately leading to potential WA. 2 Additionally, as technology is implemented, organizational processes that will interface with the technology must be carefully reengineered to reduce the unintended consequences of change. 8
Footnotes
Supported by the Agency for Healthcare Research and Quality (5 UC1 S1428102).
Amy Vogelsmeier is a 2005-2007 John A. Hartford Building Academic Geriatric Nursing Capacity Pre-Doctoral Scholar.
References
- 1.Institute of Medicine To Err is Human: Building a Safer Health SystemWashington, DC: National Academy Press; 1999.
- 2.Institute of Medicine Preventing Medication Errors: Quality Chasm SeriesWashington, DC: National Academies Press; 2006.
- 3.Thomas EJ, Studdert DM, Burstin HR, et al. Incidence and types of adverse events and negligent care in Utah and Colorado Med Care 2000;38:261-271. [DOI] [PubMed] [Google Scholar]
- 4.Gurwitz JH, Field TS, Judge J, et al. The incidence of adverse drug events in two large academic long-term care facilities Am J Med 2005;118:251-258. [DOI] [PubMed] [Google Scholar]
- 5.Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors J Am Med Assoc 1998;280:1311-1316. [DOI] [PubMed] [Google Scholar]
- 6.Scott-Cawiezell J, Madsen R, Pepper GA, Vogelsmeier A, Petroski G, Zellmer D. Using an electronic medication administration record to improve nursing home medication safety. Jt Comm J Qual Patient Saf In review. [DOI] [PubMed]
- 7.Kaushal R, Bates DW. Information technology and medication safety: what is the benefit? Qual Saf Health Care 2002;11:261-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors J Am Med Inform Assoc 2004;11:104-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors J Am Med Assoc 2005;293:1197-1203. [DOI] [PubMed] [Google Scholar]
- 10.AHRQ Press-release: New AHRQ funded study on computerized order entry finds clues that could lead to errors, points to opportunities for improvedAvailable at:http://www.ahrq.gov/news/press/pr2005/cpoer.htm 2005. Accessed October 20, 2006.
- 11.AHRQ AHRQ National Resource Center for Health ITAvailable at:http://healthit.ahrq.gov 2006. Accessed October 20, 2006.
- 12.Kaushal R, Barker KN, Bates DW. How can information technology improve patient safety and reduce medical errors in children’s health care? Arch Pediatr Adolesc Med 2001;155:1002-1007. [DOI] [PubMed] [Google Scholar]
- 13.Karsh B, Holden RJ. New technology implementation in health careIn: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Mahwah, NJ: Lawrence Erlbaum; 2007.
- 14.Puckett F. Medication-management component of a point-of-care information system Am J Health Syst Pharm 1995;52:1305-1309. [DOI] [PubMed] [Google Scholar]
- 15.Wald H, Shojania KG. Prevention of misidentificationsIn: Shojania KG, Duncan BW, McDonald KM, Wachter RW, editors. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Rockville, MD: Agency for Healthcare Research and Quality; 2001. [PMC free article] [PubMed]
- 16.Carayon P, Gürses AP. A human factors engineering conceptual framework of nursing workload and patient safety in intensive care units Intens Crit Care Nurs 2005;21:284-301. [DOI] [PubMed] [Google Scholar]
- 17.Gürses AP, Carayon P. ICU nursing workload: causes and consequences Grant Final Report to the Agency for Healthcare Research and Quality. 2005(1 R03 HS014517). [PubMed]
- 18.Potter P, Wolf L, Boxerman S, et al. Understanding the cognitive work of nursing in the acute care environment J Nurs Admin 2005;35:327-335. [PubMed] [Google Scholar]
- 19.Patterson ES, Rogers ML, Chapman RJ, Render M. Compliance with intended use of bar code medication administration in acute and long-term care: an observational study Human Factors 2006;48:15-22. [DOI] [PubMed] [Google Scholar]
- 20.Tucker AL, Edmondson AC. Managing routine exceptions: a model of nursing problem solving behavior Adv Health Care Manag 2002;3:87-113. [Google Scholar]
- 21.Kobayashi M, Fussell SR, Xiao Y, Seagull J. Work coordination, work flow, and workarounds in a medical contextCHI late breaking results. New York: ACM Press; 2005. pp. 1561-1564.
- 22.Barker KN, McConnell WE. Detecting errors in hospitals Am J Hosp Pharm 1962;19:361-369. [Google Scholar]
- 23.Judge J, Field TS, DeFlorio M, Laprino J, Auger J, Rochon P. Prescribers’ responses to alerts during medication ordering in the long term care setting J Am Med Inform Assoc 2006;13:385-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ash JS, Gorman PN, Lavelle M, et al. A cross-site qualitative study of physician order entry J Am Med Inform Assoc 2003;10:188-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aarts J, Doorewaard H, Berg M. Understanding implementation: the case of a computerized physician order entry system in a large Dutch university medical center J Am Med Inform Assoc 2004;11:207-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aarts J, Ash J, Berg M. Extending the understanding of computerized physician order entry: implications for professional collaboration, work flow and quality of care Int J Med Inform 2007;76(Suppl 1):S4-S13. [DOI] [PubMed] [Google Scholar]
- 27.Tucker AL. The impact of operational failures on hospital nurses and their patients J Operations Manage 2004;22:151-169. [Google Scholar]
- 28.Tucker AL, Edmondson AC. Why hospitals don’t learn from failures: organizational and psychological dynamics that inhibit system change Cal Manage Rev 2003;45:55-72. [Google Scholar]
- 29.Edmondson AC. Speaking up in the operating room: how team leaders promote learning in interdisciplinary action teams J Manage Stud 2003;40:1419-1452. [Google Scholar]
- 30.Roberto MA, Bohmer RMJ, Edmondson AC. Facing ambiguous threats Harv Bus Rev 2006;84:106-113. [PubMed] [Google Scholar]