Abstract
Background
Limited data are available describing contemporary trends in the utilization of diagnostic and interventional procedures in patients hospitalized with acute myocardial infarction (AMI). The objectives of our population-based investigation were to examine long-term trends (1986–2003) in the utilization of cardiac catheterization, percutaneous coronary interventions (PCI), and coronary artery bypass graft surgery (CABG) in a community sample of patients hospitalized with AMI. We examined the demographic and clinical characteristics of patients who received these diagnostic and interventional procedures and determined whether the profile of patients undergoing these procedures had changed over time.
Methods
The study sample consisted of 9,422 greater Worcester (MA) residents hospitalized with confirmed AMI at all metropolitan Worcester medical centers in 10 annual periods between 1986 and 2003. Information on patient demographics, clinical course, and treatment practices was obtained through the review of hospital medical records.
Results
Marked increases were observed in the utilization of cardiac catheterization (18.4% to 55.8%) and PCI (2.0% to 42.1%) between 1986 and 2003, respectively. Utilization of CABG showed modest increases in the early 1990's while its use was relatively stable thereafter. Several demographic and clinical characteristics were associated with the receipt of these diagnostic and interventional procedures.
Conclusions
The results of this study of patients hospitalized with AMI in a large Northeast community suggest evolving trends in the use of cardiac catheterization, PCI, and CABG. Despite these changing patterns, our findings suggest that there remains room for improvement in the therapeutic management of patients hospitalized with AMI, including certain high risk groups.
Introduction
Preventive activities directed towards coronary heart disease (CHD) in general, and acute myocardial infarction (AMI) in particular, as well as advances in treatment practices have resulted in declines in the mortality associated with acute CHD in the U.S. during the past several decades (1–6). Much of this improved survival can be attributed to the enhanced use of effective medications and treatment modalities, including diagnostic cardiac catheterization, percutaneous coronary interventions (PCI), and coronary artery bypass grafting (CABG).
In the U.S., the number of patients undergoing cardiac catheterization as well as PCI has progressively increased over the past two decades (1,5–11). On the other hand, the use of CABG has exhibited more divergent trends. While a number of studies have examined the use of these procedures in relation to various patient characteristics (10–14), few of these studies have been carried out from the more generalizable perspective of a community-based investigation or during recent time periods.
The Worcester Heart Attack Study is an ongoing, population-based investigation of residents from a large Northeastern metropolitan area who are hospitalized with AMI (15–17). Using data from the medical records of 9,422 greater Worcester residents hospitalized with validated AMI at all area medical centers in 10 annual periods between 1986 and 2003, we examined the evolving application of diagnostic cardiac catheterization and coronary interventional procedures in the greater Worcester (MA) population. In addition, we describe the demographic and clinical profile of patients receiving these procedures and examine whether this profile has changed over time.
Methods
The Worcester Heart Attack Study is examining changes over time in the descriptive epidemiology of CHD in residents of the Worcester metropolitan area hospitalized with a discharge diagnosis of AMI from all metropolitan Worcester hospitals (15–17). Originally, there were 16 health care facilities that were canvassed in this observational study; during more recent years fewer hospitals (n=11) have been providing care to greater Worcester residents due to hospital closures, mergers, or conversion to chronic care or rehabilitation facilities. Our original study sample consisted of residents of the Worcester metropolitan area hospitalized with validated AMI during 1975, 1978, 1981, 1984, 1986, 1988, 1990, 1991, 1993, 1995, 1997, 1999, 2001, and 2003 (15–17). We restricted the sample of the present report to patients hospitalized with AMI between 1986 and 2003, given the introduction of PCI to clinical practice for the management of patients with AMI in the mid-1980's.
The details of this study have been previously described (15–17). In brief, the medical records of residents of the Worcester metropolitan area (2000 census estimate = 478,000) hospitalized for possible AMI were individually reviewed and validated according to pre-defined diagnostic criteria based on clinical history, serum enzyme changes, and serial electrocardiographic findings. Cases of perioperative associated AMI were not included.
Data collection
Sociodemographic, medical history, and clinical data were abstracted from the hospital medical records of eligible patients by trained study physicians and nurses. Information was collected about patient's age, sex, body mass index, extent of prehospital delay, comorbidities, AMI order (initial versus prior) and type (Q wave versus non Q wave), occurrence of clinically significant hospital complications, and hospital survival status. Information about the use of cardiac catheterization, CABG, and PCI was collected through the review of nurse's and physician's progress notes as well as review of test results. Detailed information was not collected about the results of cardiac catheterization findings.
Data analysis
Differences in the distribution of demographic and clinical characteristics between patients receiving and not receiving selected cardiac procedures were examined through the use of chi-square and t tests for discrete and continuous variables, respectively. A logistic multivariable regression analysis was used to examine factors associated with the utilization of the cardiac procedures examined. The factors controlled for in our regression analyses included age, sex, payment method, history of angina, diabetes, heart failure, hypertension or stroke, and AMI order (initial vs. prior) and type (Q wave vs. non-Q wave). Since information about body mass index and duration of prehospital delay was not collected until more recent study years, and because there was a considerable amount of missing data with regards to these variables, we did not control for these factors in our regression analyses. In addition, since prior studies have shown differences in treatment practices and outcomes in patients with STEMI (ST segment elevation MI) and NSTEMI (Non ST segment elevation MI), we carried out a subgroup analysis in which we examined differences in procedure use in these patient populations between 1997 and 2003 when information about type of AMI was collected.
Results
Long-Term Trends in the Use of Cardiac Procedures
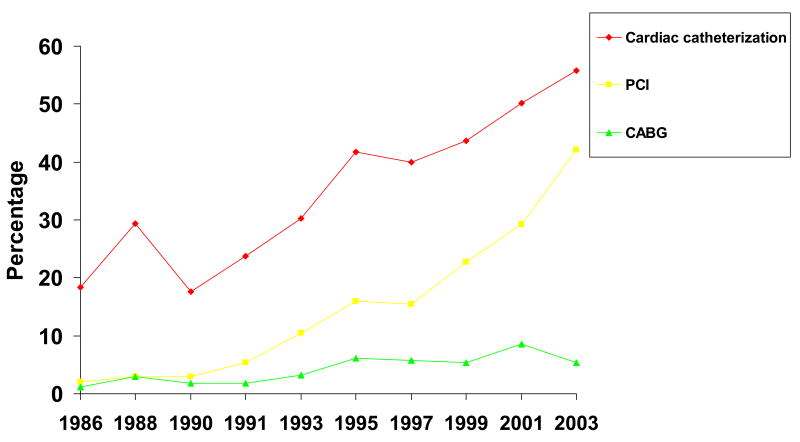
Over the period under study, we observed marked increases in the use of cardiac catheterization (18.4%–55.8%) and PCI (2.0%–42.1%) between 1986 and 2003, respectively. On the other hand, the utilization of CABG showed modest increases between 1991 and 1995 while the use of this revascularization procedure remained relatively stable during other study years (Figure 1). The proportion of patients who went on to receive a PCI after undergoing cardiac catheterization also increased dramatically over time, from 10.4% of patients who underwent catheterization in 1986/1988 to 67.0% of those undergoing cardiac catheterization during 2001 and 2003.
Figure 1.
Use of Cardiac Procedures in Patients Hospitalized With Acute Myocardial Infarction: Worcester Heart Attack Study
Characteristics of Patients Receiving Diagnostic and/or Interventional Procedures
Younger patients, men, and overweight patients were more likely to receive these procedures than respective comparison groups (Table I). Patients with a history of heart failure, stroke, or previous MI were less likely to undergo these procedures than patients without these prior conditions.
Table I.
Characteristics of Patients Receiving Cardiac Diagnostic and Interventional Procedures: Worcester Heart Attack Study
| Feature | Cardiac Catheterization | p-value | PCI | p-value | CABG | p-value |
|---|---|---|---|---|---|---|
| Age (years) | % receiving | % receiving | % receiving | |||
| <55 | 60.8 | <0.01 | 31.9 | <0.01 | 4.6 | <0.01 |
| 55–64 | 50.8 | 22.6 | 6.3 | |||
| 65–74 | 39.4 | 16.3 | 6.0 | |||
| 75–84 | 26.1 | 11.2 | 3.9 | |||
| ≥85 | 9.4 | 5.5 | 0.5 | |||
| Sex | ||||||
| Male | 43.0 | <0.01 | 19.5 | <0.01 | 5.3 | <0.01 |
| Female | 28.9 | 13.6 | 3.4 | |||
| Payment Method | ||||||
| Private Payment | 48.8 | 0.39 | 21.9 | <0.01 | 5.0 | <0.01 |
| Private Insurance | 47.7 | 17.2 | 3.9 | |||
| Blue Cross | 42.7 | 18.8 | 3.4 | |||
| Medicaid | 44.7 | 19.7 | 5.7 | |||
| Medicare | 26.6 | 10.4 | 3.3 | |||
| HMO | 49.5 | 26.7 | 6.8 | |||
| Prehospital Delay | ||||||
| <2 hrs | 44.0 | <0.01 | 21.7 | <0.01 | 4.2 | .08 |
| 2–3.9 hrs | 42.2 | 17.0 | 5.7 | |||
| 4–5.9 hrs | 40.0 | 18.0 | 4.0 | |||
| ≥6 hrs | 38.0 | 14.7 | 5.7 | |||
| Body Mass Index | ||||||
| <25 | 35.9 | <0.01 | 19.0 | <0.01 | 4.5 | <0.01 |
| 25–29.9 | 55.1 | 30.3 | 6.8 | |||
| ≥30 | 61.1 | 34.7 | 8.5 | |||
| Comorbidities | ||||||
| Angina | ||||||
| Yes | 38.2 | 0.18 | 15.4 | <0.05 | 6.8 | <0.01 |
| No | 36.7 | 17.5 | 3.8 | |||
| Diabetes | ||||||
| Yes | 35.5 | <0.05 | 14.1 | <0.01 | 6.0 | <0.01 |
| No | 37.7 | 18.1 | 3.9 | |||
| Heart Failure | ||||||
| Yes | 19.2 | <0.01 | 7.7 | <0.01 | 2.5 | <0.01 |
| No | 41.5 | 19.2 | 5.0 | |||
| Stroke | ||||||
| Yes | 23.7 | <0.01 | 10.0 | <0.01 | 2.9 | <0.01 |
| No | 38.7 | 17.8 | 4.7 | |||
| Hypertension | ||||||
| Yes | 37.6 | 0.21 | 16.9 | 0.79 | 5.2 | <0.01 |
| No | 36.3 | 17.1 | 3.5 | |||
| MI Order | ||||||
| Initial | 39.3 | <0.01 | 19.3 | <0.01 | 4.7 | 0.32 |
| Prior | 33.0 | 12.6 | 4.2 | |||
| MI Type | ||||||
| Q wave | 40.4 | <0.01 | 20.7 | <0.01 | 4.1 | 0.12 |
| Non Q wave | 35.2 | 14.9 | 4.8 |
In examining patient characteristics associated with the receipt of PCI, patients presenting to Central Massachusetts hospitals less than 2 hours from the onset of acute coronary symptoms were more likely to receive a PCI than those who presented after more prolonged delay. Patients with a history of angina or diabetes, and those with a prior or non-Q-wave MI, were less likely to undergo these procedures than respective comparison groups. Patients with private insurance were more likely to receive a PCI than uninsured patients or patients with Medicaid insurance. Patients with Medicare insurance were least likely to undergo a PCI.
Receipt of CABG was associated with a variety of patient characteristics. Patients 55–74 years old were more likely to undergo CABG while patients with Medicare insurance were least likely to undergo CABG (Table I). Patients with prior angina, diabetes, or hypertension were more likely to undergo CABG whereas patients with a history of stroke or heart failure were less likely to undergo CABG.
Changes in the Profile of Patients Undergoing Cardiac Procedures Over Time
Changes in the clinical and demographic profile of patients undergoing these cardiac procedures over time were examined (Table II). For ease of data interpretation, and to coincide with changes in treatment practices over time, we examined data from our first 2 study years (1986/88), midpoint (1993/95), and most recent study years (2001/2003). Utilization of each of these procedures increased in every patient subset assessed. Marked increases in the use of cardiac catheterization and PCI were particularly noted in the elderly, women, patients with Medicare or Medicaid, and in patients with a history of diabetes or heart failure.
Table II.
Trends in the characteristics of patients undergoing cardiac procedures: Worcester Heart Attack Study
| Cardiac Catheterization | PCI | CABG | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | 1986/88 | 1993/95 | 2001/03 | P value for trend | 1986/88 | 1993/95 | 2001/03 | P value for trend | 1986/88 | 1993/95 | 2001/03 | P value for trend |
| Age (years) | % | % | % | % | % | % | % | % | % | |||
| <55 | 43.6 | 60.3 | 82.4 | <.001 | 8.1 | 25.2 | 63.24 | <.001 | 3.3 | 5.2 | 6.2 | <.001 |
| 55–64 | 33.3 | 50.6 | 70.9 | 2.5 | 19.1 | 51.9 | 2.5 | 7.9 | 8.6 | |||
| 65–74 | 23.6 | 38.6 | 64.6 | 2.3 | 13.0 | 38.2 | 2.0 | 5.2 | 12.6 | |||
| 75–84 | 8.6 | 22.9 | 42.1 | 0 | 7.5 | 24.9 | 0.7 | 3.5 | 6.3 | |||
| ≥85 | 0.7 | 2.8 | 19.8 | 0 | 1.4 | 13.4 | 0 | 0 | 0.9 | |||
| Sex | ||||||||||||
| Male | 28.8 | 41.8 | 60.1 | <.01 | 3.4 | 15.3 | 41.0 | 0.07 | 1.9 | 5.3 | 8.4 | 0.49 |
| Female | 15.8 | 27.7 | 43.7 | 1.0 | 10.4 | 28.3 | 1.9 | 3.7 | 5.2 | |||
| Payment Method | ||||||||||||
| Private Payment | 42.8 | 46.2 | 61.9 | <.001 | 0 | 18.5 | 45.2 | <.001 | 3.6 | 1.5 | 7.2 | <.01 |
| Private Insurance | 37.4 | 52.8 | 74.2 | 7.2 | 19.5 | 51.6 | 1.2 | 3.5 | 9.7 | |||
| Blue Cross | 38.0 | 43.0 | 67.1 | 6.5 | 19.8 | 50.0 | 3.2 | 3.3 | 7.0 | |||
| Medicaid | 18.5 | 52.3 | 82.9 | 3.7 | 18.2 | 50.0 | 0 | 9.1 | 11.4 | |||
| Medicare | 13.0 | 27.8 | 40.2 | 0.2 | 9.7 | 25.3 | 0.6 | 3.9 | 4.6 | |||
| HMO | 26.0 | 51.4 | 58.4 | 3.5 | 19.7 | 40.0 | 2.2 | 8.1 | 8.8 | |||
| Prehospital Delay | ||||||||||||
| <2 hrs | 30.1 | 43.8 | 61.3 | 0.33 | 3.5 | 19.7 | 43.6 | 0.30 | 2.3 | 2.5 | 7.1 | 0.30 |
| 2–3.9 hrs | 31.9 | 39.0 | 64.8 | 2.4 | 10.4 | 41.9 | 1.9 | 6.8 | 9.3 | |||
| 4–5.9 hrs | 21.6 | 37.3 | 63.5 | 3.4 | 15.9 | 41.7 | 1.1 | 4.0 | 6.1 | |||
| ≥6 hrs | 19.8 | 34.5 | 63.1 | 1.9 | 10.3 | 41.9 | 2.6 | 6.6 | 9.6 | |||
| BMI* | ||||||||||||
| <25 | 33.2 | 41.4 | 12.9 | 28.2 | 4.9 | 5.0 | ||||||
| 25–29.9 | 47.9 | 62.1 | 18.0 | 44.2 | 6.8 | 7.2 | ||||||
| ≥30 | 57.1 | 66.5 | 22.2 | 44.5 | 8.4 | 8.9 | ||||||
| Comorbidities | ||||||||||||
| Angina | ||||||||||||
| Yes | 25.2 | 36.1 | 53.6 | <.01 | 2.4 | 11.2 | 33.3 | 0.33 | 2.4 | 7.8 | 9.5 | 0.13 |
| No | 22.9 | 35.9 | 52.7 | 2.5 | 14.1 | 36.0 | 1.7 | 3.4 | 6.2 | |||
| Diabetes | ||||||||||||
| Yes | 19.3 | 34.3 | 49.8 | <.001 | 0.8 | 9.0 | 29.8 | <.001 | 1.7 | 6.8 | 8.5 | 0.24 |
| No | 24.9 | 36.6 | 54.4 | 3.0 | 14.9 | 38.2 | 2.0 | 3.8 | 6.2 | |||
| Heart Failure | ||||||||||||
| Yes | 5.2 | 19.5 | 28.5 | <.001 | 0 | 4.9 | 16.0 | <.01 | 1.0 | 4.1 | 3.5 | 0.97 |
| No | 24.6 | 39.6 | 60.6 | 2.8 | 15.1 | 41.6 | 2.0 | 4.8 | 8.1 | |||
| Stroke | ||||||||||||
| Yes | 12.8 | 22.2 | 32.5 | 0.65 | 4.8 | 5.7 | 18.8 | 0.54 | 1.6 | 3.6 | 3.1 | 0.48 |
| No | 24.6 | 37.5 | 55.8 | 2.2 | 14.1 | 37.7 | 1.9 | 4.7 | 7.5 | |||
| Hypertension | ||||||||||||
| Yes | 23.2 | 34.7 | 50.3 | <.001 | 2.7 | 11.5 | 31.9 | <.001 | 2.0 | 5.5 | 7.0 | 0.10 |
| No | 23.8 | 37.7 | 59.2 | 2.2 | 15.6 | 44.1 | 1.8 | 3.5 | 7.0 | |||
| MI Order | ||||||||||||
| Initial | 23.8 | 38.4 | 57.1 | 0.46 | 3.4 | 15.1 | 39.9 | 0.23 | 1.9 | 4.6 | 7.7 | 0.28 |
| Recurrent | 22.8 | 31.9 | 45.3 | 0.4 | 10.2 | 27.2 | 2.0 | 4.6 | 5.7 | |||
| MI Type | ||||||||||||
| Q wave | 24.5 | 41.7 | 72.8 | <.001 | 3.4 | 18.7 | 58.6 | <.001 | 1.4 | 5.0 | 7.3 | <.01 |
| Non Q wave | 22.6 | 32.5 | 47.8 | 1.5 | 9.9 | 29.4 | 2.4 | 4.4 | 6.8 | |||
BMI data not recorded before 1993
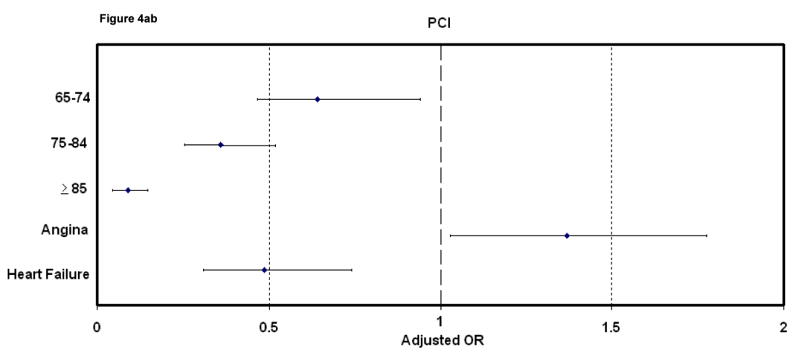
Factors Associated with Receipt of Selected Procedures
In a series of multivariable adjusted regression analyses, older patients had a lower likelihood of undergoing cardiac catheterization and PCI than younger patients (Figure 2). Patients 65–74 years old were more likely to undergo CABG than younger or older patients. Men were significantly more likely to undergo cardiac catheterization and/or CABG, but not PCI, than women. In comparison with uninsured patients, patients with private insurance were more likely to receive a PCI than uninsured patients or patients with Medicaid or Medicare insurance.
Figure 2.
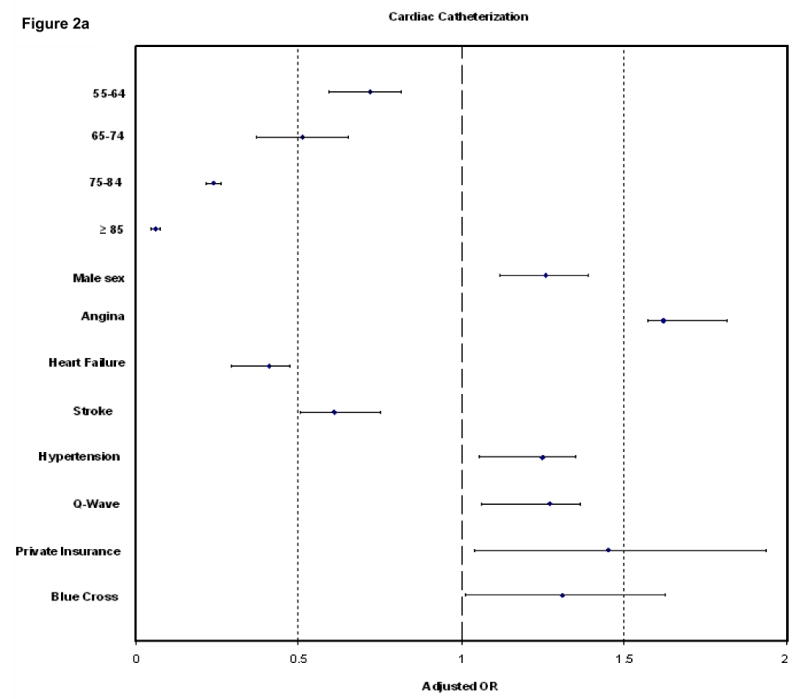
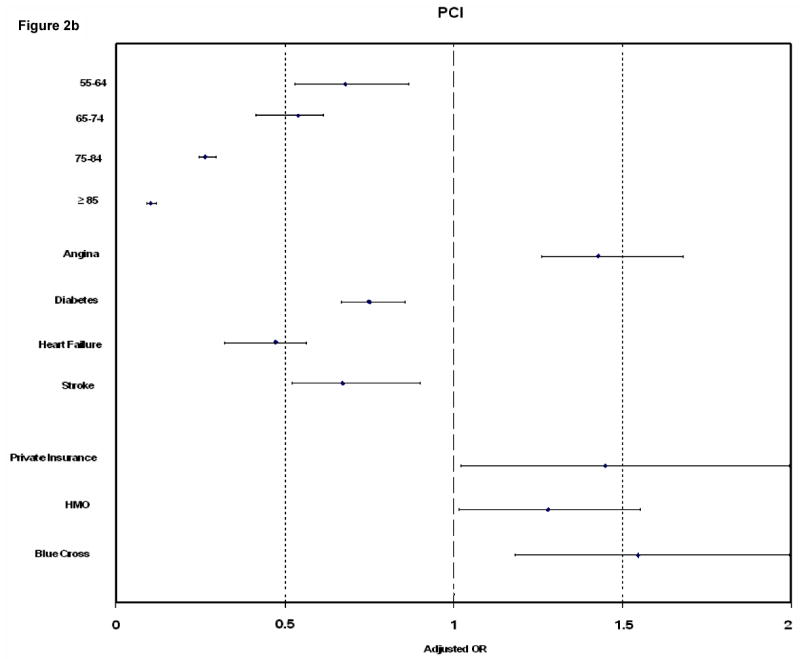
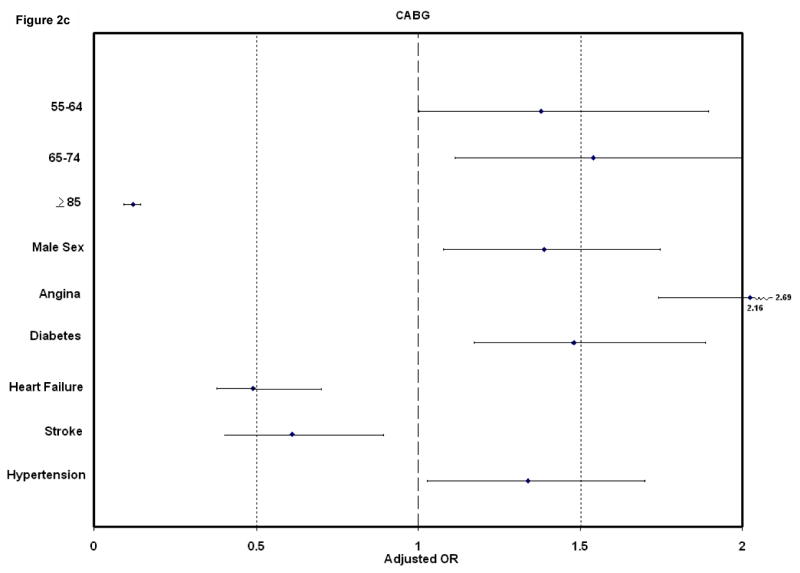
Factors Associated With Selected Cardiac Procedures in Patients Hospitalized With Acute Myocardial Infarction: Worcester Heart Attack Study
Patients with a history of heart failure and stroke were less likely to receive each of these procedures, while patients with prior angina were more likely to undergo them. Patients with a history of hypertension were more likely to receive cardiac catheterization or CABG as compared to those without prior hypertension. Lastly, patients with a Q-wave MI were more likely to undergo a PCI, but less likely to undergo CABG, than patients with a non-Q wave MI.
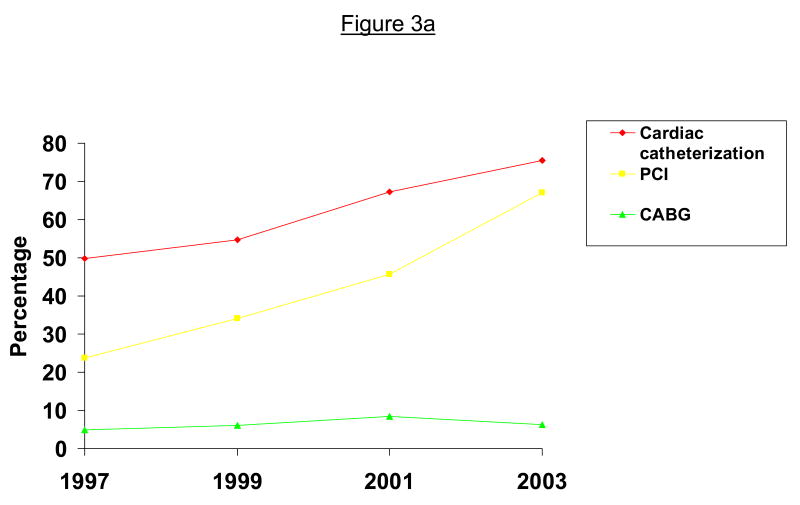
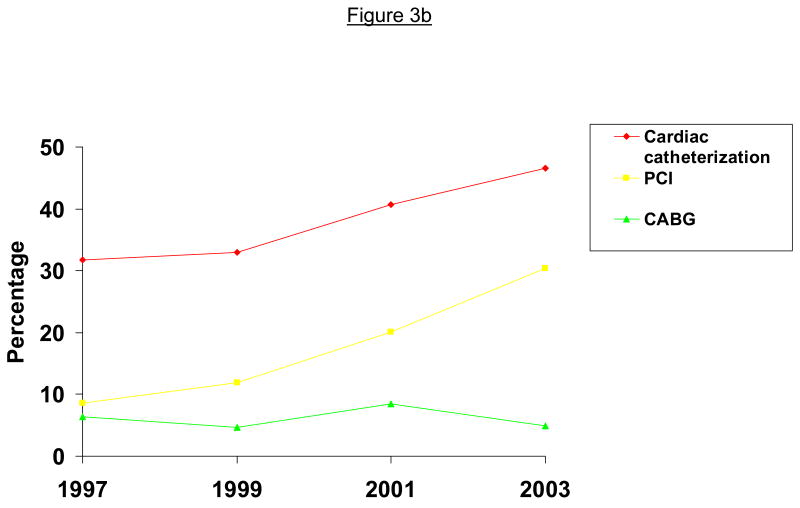
Use of Diagnostic and Interventional Procedures in Patients with STEMI and NSTEMI
Due to potential differences in the management and outcomes of patients with a STEMI or a NSTEMI, we examined use of these procedures separately in these patient populations. Cardiac catheterization and PCI were used more frequently in the diagnosis and treatment of patients with a STEMI than among those with a NSTEMI (Figures 3a and 3b). The use of these procedures increased markedly in patients with both types of MI between 1997 and 2003. The use of CABG did not differ between STEMI and NSTEMI patients.
Figure 3a.
Use of Cardiac Procedures in Patients Hospitalized With ST-Segment Elevation Acute Myocardial Infarction: Worcester Heart Attack Study
Figure 3b.
Use of Cardiac Procedures in Patients Hospitalized With Non ST-Segment Elevation Acute Myocardial Infarction: Worcester Heart Attack Study
In both the STEMI (Figure 4a) and NSTEMI (Figure 4b) patient populations, the demographic and clinical characteristics previously associated with the utilization of cardiac catheterization and PCI in our total study sample continued to be observed.
Figure 4a.
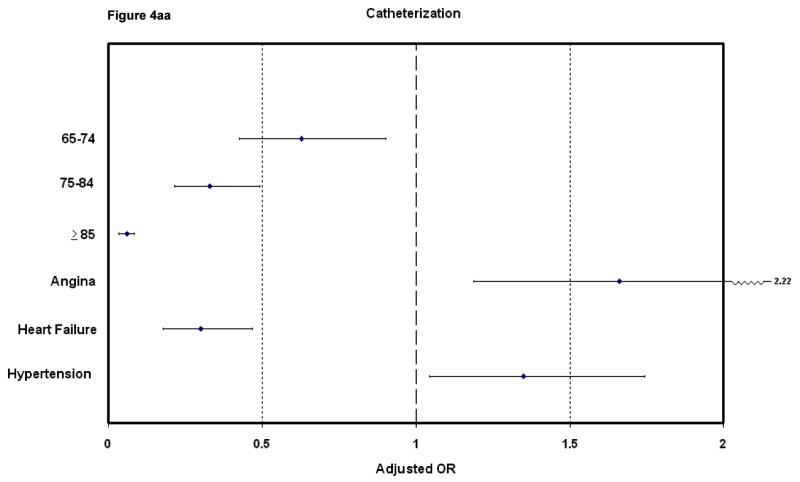
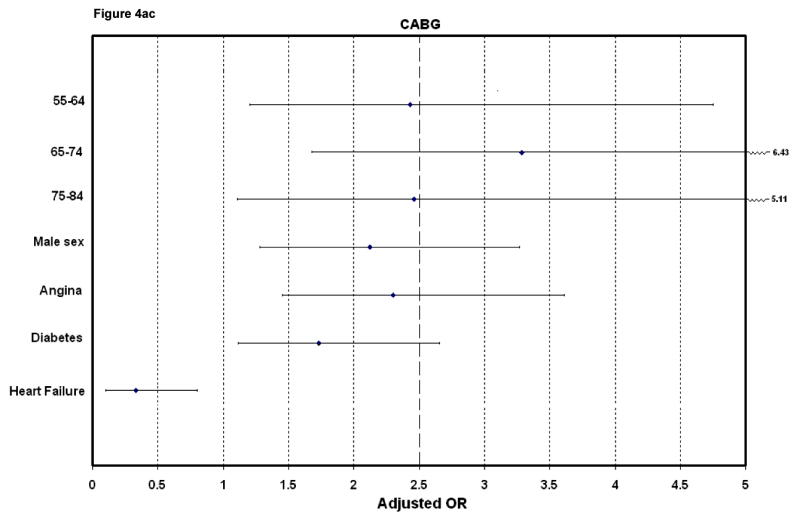
Factors Associated With the Use of Selected Cardiac Procedures in Patients With ST-Segment Elevation Acute Myocardial Infarction: Worcester Heart Attack Study
Figure 4b.
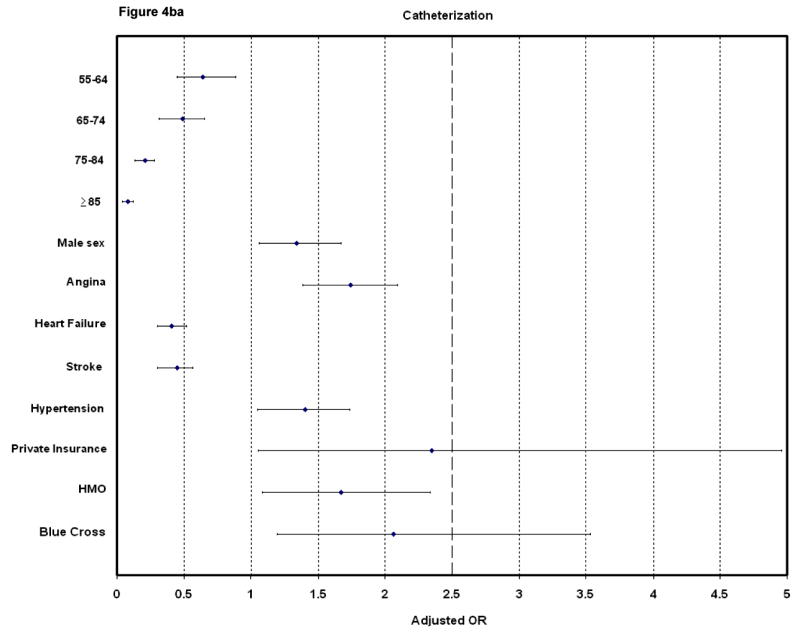
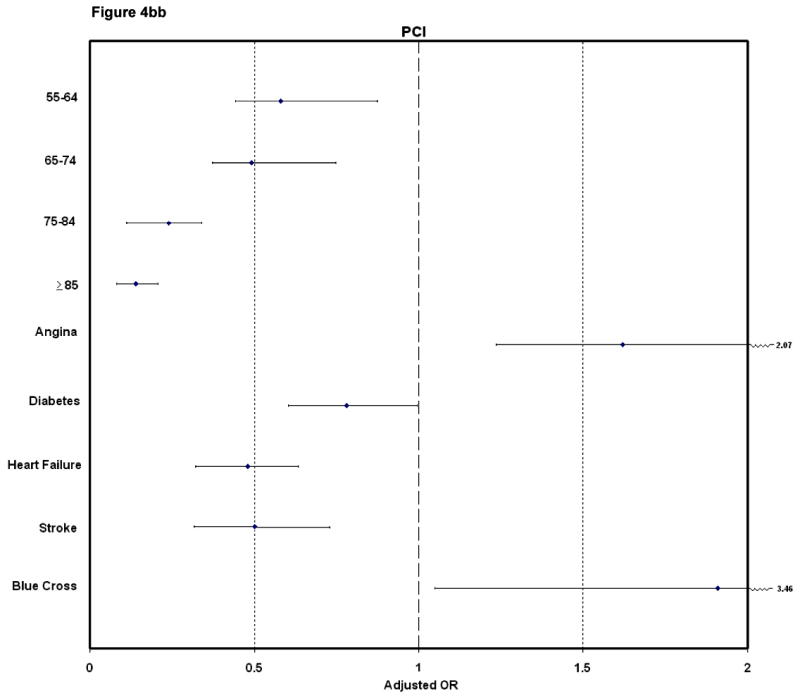
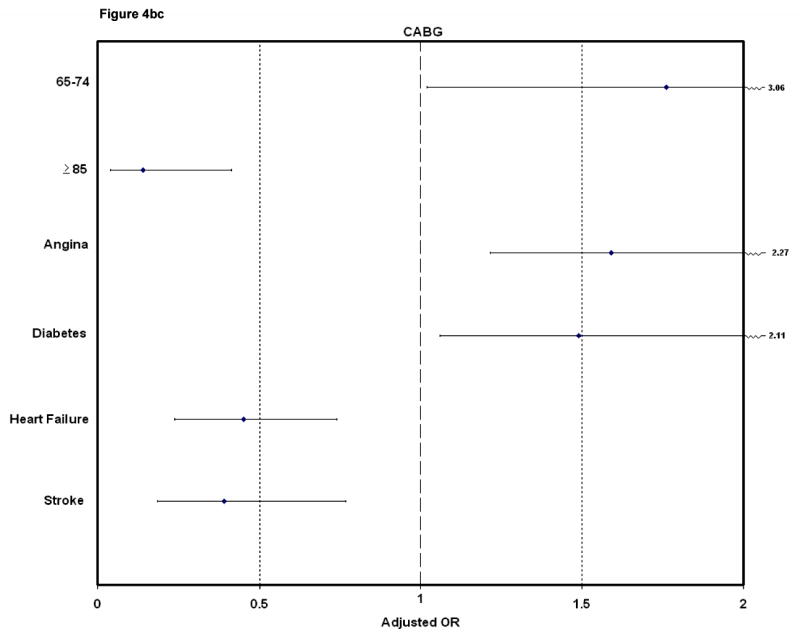
Factors Associated With the Use of Selected Cardiac Procedures in Patients With Non ST-Segment Elevation Acute Myocardial Infarction: Worcester Heart Attack Study
Discussion
The results of this study among residents of a large urban Northeastern community hospitalized with AMI suggest marked increases in the use of cardiac catheterization and PCI over time with only slight increases in the use of CABG, particularly during the early nineties. Although the utilization of cardiac catheterization and PCI increased in all patient subsets examined, the most notable increases occurred in women, the elderly, and patients with Medicare or Medicaid insurance. These changing trends resulted in narrowing of previously observed disparities in the care patterns of these groups.
Changing trends in the use of procedures for the diagnosis and management of patients hospitalized with AMI
In agreement with national trends (1), we observed marked increases in the use of cardiac catheterization for the evaluation of patients with AMI and in the utilization of PCI for their treatment. Recent findings from the National Registry of Myocardial Infarction demonstrated an increase in the utilization of primary PCI, modest increases in PCI, but declines in the use of CABG and coronary arteriography in patients hospitalized with AMI between 1990 and 1999 (5).
Investigators from the Minnesota Heart Study evaluated trends in the use of diagnostic and interventional procedures in Twin Cities' residents hospitalized with acute coronary disease between 1985 and 1997 (6). Increases in the use of coronary angiography (22% to 59% in men and 18% to 57% in women) and angioplasty (5%–34% in men and 5%–33% in women) were observed between the initial and most recent year under study. Increases in the use of CABG were observed in men (5%–10%) while the use of CABG remained stable in women (7%–8%) over the period under study.
The utilization of cardiac catheterization in elderly Medicare beneficiaries in the U.S. increased appreciably between 1993 and 2001 while the use of PCI increased twofold (from 6 to 12 procedures per 1000 beneficiaries) over this period (7). The use of CABG showed only modest increases between 1993 and 2001.
Differences in practice standards between New England and other regions of the U.S. need to be considered when comparing our findings to national or other regional investigations (18,19). Physicians in New England have been previously shown to utilize thrombolytic and coronary reperfusion therapy less frequently, but effective cardiac medications more often, than physicians from other regions of the U.S.
Factors Associated with the Use of Cardiac Procedures
A variety of demographic and clinical factors were associated with use of the cardiac procedures examined in the present study. Elderly patients were less likely to receive any of these cardiac procedures, a finding consistent with the results of other investigations (7–12,18,19).
Men were more likely to receive any of these cardiac procedures than women in our study, a difference noted in many previous investigations (6–14,18,19). A previous study examining trends between men and women in the use of cardiac procedures between 1995 and 2001 in patients hospitalized with AMI from the Nationwide Inpatient Sample found that, after controlling for several factors, women underwent cardiac catheterization, coronary angioplasty, and stent placement at essentially similar rates with men; women were approximately one-fifth less likely to undergo CABG than men (11).
We observed marked differences in the use of these cardiac procedures in overweight and obese patients compared to patients of lower body weight. In an examination of elderly Medicare patients hospitalized for AMI in the mid-1990's in hospitals with invasive cardiac capabilities, patients with a normal BMI were less likely to receive these procedures than those who were overweight (13).
Several AMI associated clinical features are associated with cardiac procedure utilization. An evaluation of procedure use in a single Veteran's Affairs Hospital in the early to mid-1990's found that patients with a Q-wave or STEMI were more likely to undergo a PCI whereas those with a history of heart failure were less likely to undergo a PCI (20). Patients with diabetes were less likely to undergo cardiac catheterization or receive a PCI, but were more likely to receive a CABG, than patients without diabetes, findings similar to the results of our study.
Cardiac interventions are highly recommended for patients at increased risk for future coronary events (2,3). Investigators from the Global Registry of Acute Coronary Events study found that cardiac catheterization and PCI were primarily utilized in low risk patients hospitalized with an acute coronary syndrome (21). We also found a higher use of these procedures in lower risk patients.
The use of coronary reperfusion or revascularization therapy is recommended for patients with STEMI, especially in emergent settings, but the effectiveness of their use in patients with NSTEMI is under debate (2,3). We, along with several other investigations (20,21), found that although cardiac catheterization and subsequent PCI use is greater among patients with STEMI, it is being used increasingly often in patients with NSTEMI. This practice is supported by clinical trial data demonstrating the superiority of routine cardiac catheterization in patients with NSTEMI compared to a more conservative approach (22,23). The clinical and demographic characteristics associated with the use of these procedures were consistent among these patients although several factors appear to play a stronger role in NSTEMI patients.
While we can only speculate about those factors which may have contributed to observed trends in procedure utilization over time in our study, including hospital reimbursement procedures, willingness to perform procedures in different at risk groups, issues related to patient acceptability of different procedures, and generally greater adherence to evidence-based medications and therapeutic procedures over time, we briefly describe the results of previous clinical trials which have contributed to an increasing knowledge base about the benefits of various treatment approaches in patients with acute coronary disease.
Several randomized trials have examined the effects of an invasive treatment strategy in comparison with medical therapy in patients with unstable angina and NSTEMI. These trials were reported in the published literature between 1994 (TIMI IIIB) and 2002 (RITA 3) (24,25). Patients treated with an invasive management strategy experienced slightly lower death rates and risk of nonfatal MI at 6 weeks and 1 year after trial enrollment and in the risk of subsequent hospitalizations (24). In the most recent of these trials, an early invasive treatment strategy in patients with unstable angina or non ST-segment elevation AMI was associated with lower 5 year death rates compared with the use of conservative therapy (25).
Comparative effects of the use of PCI relative to thrombolytic therapy have been examined in a large number of randomized trials. In the PAMI trial, which was published in 1993, patients undergoing a PCI fared better with regards to in-hospital mortality and the 2 year risk of recurrent ischemia/infarction or death in comparison to patients treated with clot lysing therapy (26). A decade later, the DANAMI-2 trial reinforced the superiority of primary PCI, particularly when combined with stent placement, as compared to thrombolysis for the treatment of ST-segment elevation AMI (27).
The effects of coronary angioplasty in comparison with CABG have been examined in patients with an acute coronary syndrome during the mid-1990's (28,29). In the RITA trial (28), the long-term outcomes of patients randomly assigned to PCI or CABG were similar. In the BARI trial, which compared the effectiveness of PCI versus CABG in more symptomatic and severely diseased patients, the 5 year death rate was higher for patients treated with PCI than CABG (29). However, when diabetic patients were eliminated from further analysis, the primary trial outcomes were similar between the 2 treatment groups.
Study Limitations
The limitations of this large observational study include the lack of data on physician characteristics, patient preferences, and information about other situational, financial, or attitudinal factors that may be related to the treatment decision making process in the setting of AMI.
Conclusions
The results of our community-wide investigation demonstrate the changing utilization of cardiac procedures in patients hospitalized with AMI. These changes, together with the demographic and clinical characteristics associated with receipt of these procedures, should be considered when planning the future role of these procedures in the treatment of patients hospitalized with AMI, especially in the context of evolving systems of health care delivery and cost containment strategies.
Acknowledgments
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area and through funding support provided by the National Institutes of Health (RO1 HL35434).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Heart Association. Heart Disease and Stroke Statistics. 2006 Update. A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. [DOI] [PubMed] [Google Scholar]
- 2.Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) J Am Coll Cardiol. 1996;28:1328–428. doi: 10.1016/s0735-1097(96)00392-0. [DOI] [PubMed] [Google Scholar]
- 3.Ryan TJ, Antman EM, Brooks NH, et al. 1999 update: ACC/AHA Guidelines for the Management of Patients With Acute Myocardial Infarction: Executive Summary and Recommendations: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) Circulation. 1999;100:1016–30. doi: 10.1161/01.cir.100.9.1016. [DOI] [PubMed] [Google Scholar]
- 4.Heidenreich PA, McClellan M. Trends in treatment and outcomes for acute myocardial infarction: 1975–1995. Am J Med. 2001;110:165–74. doi: 10.1016/s0002-9343(00)00712-9. [DOI] [PubMed] [Google Scholar]
- 5.Rogers WJ, Canto JG, Lambrew CT, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–63. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 6.McGovern PG, Jacobs DR, Jr, Shahar E, et al. Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: the Minnesota Heart Survey. Circulation. 2001;104:19–24. doi: 10.1161/01.cir.104.1.19. [DOI] [PubMed] [Google Scholar]
- 7.Lucas FL, DeLorenzo MA, Siewers AE, et al. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113:374–9. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ulrich MR, Brock DM, Ziskind AA. Analysis of trends in coronary artery bypass grafting and percutaneous coronary intervention rates in Washington state from 1987 to 2001. Am J Cardiol. 2003;92:836–9. doi: 10.1016/s0002-9149(03)00895-6. [DOI] [PubMed] [Google Scholar]
- 9.Perschbacher JM, Reeder GS, Jacobsen SJ, et al. Evidence-based therapies for myocardial infarction: secular trends and determinants of practice in the community. Mayo Clin Proc. 2004;79:983–91. doi: 10.4065/79.8.983. [DOI] [PubMed] [Google Scholar]
- 10.Pilote L, Saynina O, Lavoie F, et al. Cardiac procedure use and outcomes in elderly patients with acute myocardial infarction in the United States and Quebec, Canada, 1988 to 1994. Med Care. 2003;41:813–22. doi: 10.1097/00005650-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Bertoni AG, Bonds DE, Lovato J, et al. Sex disparities in procedure use for acute myocardial infarction in the United States, 1995 to 2001. Am Heart J. 2004;147:1054–60. doi: 10.1016/j.ahj.2003.11.019. [DOI] [PubMed] [Google Scholar]
- 12.Avezum A, Makdisse M, Spencer F, et al. GRACE Investigators. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE) Am Heart J. 2005;149:67–73. doi: 10.1016/j.ahj.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 13.Yancy WS, Jr, Olsen MK, Curtis LH, et al. Variations in coronary procedure utilization depending on body mass index. Arch Intern Med. 2005;165:1381–7. doi: 10.1001/archinte.165.12.1381. [DOI] [PubMed] [Google Scholar]
- 14.Vaccarino V, Rathore SS, Wenger NK, et al. National Registry of Myocardial Infarction Investigators. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–82. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldberg RJ, Gore JM, Alpert JS, et al. Recent changes in the attack rates and survival rates of acute myocardial infarction (1975–1981): The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 16.Goldberg RJ, Yarzebski J, Lessard D, et al. A two-decades (1975–1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: A community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 17.Spencer FA, Lessard D, Yarzebski J, et al. Decade-long changes in the use of combination evidence-based medical therapy at discharge for patients surviving acute myocardial infarction. Am Heart J. 2005;150:838–44. doi: 10.1016/j.ahj.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Krumholz HM, Chen J, Rathore SS, et al. Regional variation in the treatment and outcomes of myocardial infarction: investigating New England's advantage. Am Heart J. 2003;146:242–9. doi: 10.1016/S0002-8703(03)00237-0. [DOI] [PubMed] [Google Scholar]
- 19.Guadagnoli E, Hauptman PJ, Ayanian JZ, et al. Variation in the use of cardiac procedures after acute myocardial infarction. N Engl J Med. 1995;333:573–8. doi: 10.1056/NEJM199508313330908. [DOI] [PubMed] [Google Scholar]
- 20.Mickelson JK, Blum CM, Geraci JM. Acute myocardial infarction: clinical characteristics, management and outcome in a metropolitan Veterans Affairs Medical Center teaching hospital. J Am Coll Cardiol. 1997;29:915–25. doi: 10.1016/s0735-1097(97)00034-x. [DOI] [PubMed] [Google Scholar]
- 21.Fox KA, Anderson FA, Dabbous OH, et al. Intervention in acute coronary syndromes: do patients undergo intervention on the basis of their risk characteristics? The Global Registry of Acute Coronary Events (GRACE) Heart. 2006 June 6; doi: 10.1136/hrt.2005.084830. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cannon CP, Weintraub WS, Demopoulos LA, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001;344:1879–87. doi: 10.1056/NEJM200106213442501. [DOI] [PubMed] [Google Scholar]
- 23.Braunwald E, Antman EM, Beasley JW, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Unstable Angina) ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction—2002: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Unstable Angina) Circulation. 2002;106:1893–1900. doi: 10.1161/01.cir.0000037106.76139.53. [DOI] [PubMed] [Google Scholar]
- 24.Effects of tissue plasminogen activator and a comparison of early invasive and conservative strategies in unstable angina and non-Q-wave myocardial infarction. Results of the TIMI IIIB Trial. Thrombolysis in Myocardial Ischemia. Circulation. 1994;89:1545. doi: 10.1161/01.cir.89.4.1545. [DOI] [PubMed] [Google Scholar]
- 25.Fox K, Poole-Wilson P, Henderson R, et al. Interventional versus conservative treatment for patients with unstable angina or non-ST-elevation myocardial infarction: the British Heart Foundation RITA 3 randomized trial. Lancet. 2002;360:743. doi: 10.1016/s0140-6736(02)09894-x. [DOI] [PubMed] [Google Scholar]
- 26.Grines CL, Browne KF, Marco J, et al. Primary Angioplasty in Myocardial Infarction Study Group. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. N Engl J Med. 1993;328:673. doi: 10.1056/NEJM199303113281001. [DOI] [PubMed] [Google Scholar]
- 27.Andersen HR, Nielsen TT, Rasmussen K, et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349:733. doi: 10.1056/NEJMoa025142. [DOI] [PubMed] [Google Scholar]
- 28.The Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med. 1996;335:217. doi: 10.1056/NEJM199607253350401. [DOI] [PubMed] [Google Scholar]
- 29.Coronary angioplasty versus coronary artery bypass surgery: the Randomized Intervention Treatment of Angina (RITA) trial. Lancet. 1993;341:573. [PubMed] [Google Scholar]