Abstract
Background
Physical activity is important for weight control and good health; however, activity levels decline in the adolescent years, particularly in girls.
Design
Group randomized controlled trial
Setting/participants
Middle school girls with English-speaking skills and no conditions to prevent participation in physical activity in 36 schools in six geographically diverse areas of the United States. Random, cross-sectional samples were drawn within schools: 6th graders in 2003 (n=1721) and 8th graders in 2005 (n=3504) and 2006 (n=3502).
Intervention
A 2-year study-directed intervention (fall 2003 to spring 2005) targeted schools, community agencies, and girls to increase opportunities, support, and incentives for increased physical activity. Components included programs linking schools and community agencies, physical education, health education, and social marketing. A third-year intervention used school and community personnel to direct intervention activities.
Main outcome measures
The primary outcome, daily MET-weighted minutes of moderate-to-vigorous physical activity (MET-weighted MVPA), was assessed using accelerometry. Percent body fat was assessed using anthropometry.
Results
After the staff-directed intervention (pre-stated primary outcome), there were no differences (mean= −0.4, 95% CI= CI= −8.2 to 7.4) in adjusted MET-weighted MVPA between 8th-grade girls in schools assigned to intervention or control. Following the Program Champion–directed intervention, girls in intervention schools were more physically active than girls in control schools (mean difference 10.9 MET-weighted minutes of MVPA, 95% CI=0.52–21.2). This difference is about 1.6 minutes of daily MVPA or 80 kcal per week. There were no differences in fitness or percent body fat at either 8th-grade timepoint.
Conclusion
A school-based, community-linked intervention modestly improved physical activity in girls.
Introduction
Physical inactivity is an independent risk factor for cardiovascular and other diseases and a major contributor to obesity in adults.1 The health-related sequelae of physical inactivity—type 2 diabetes, high blood pressure, dyslipidemia, obesity, and sleep disorders—have increased in children and adolescents.2 About 6% to 20% of adolescents are physically inactive3; 17% of children and adolescents are overweight4; and 26% to 75% of overweight youths become obese adults.5 Effective interventions to increase physical activity among adolescents could reduce obesity prevalence and reduce disease risk in youth and adults.6
Despite the known health benefits, physical activity declines among youth in the U.S. as they grow through adolescence.7 The decline is more prevalent in girls than in boys, suggesting that interventions targeting girls are needed.8 Interventions to promote physical activity, generally directed to both boys and girls, have been conducted in school settings,9 but have met with limited success, perhaps because only about 30 hours per year of moderate-to-vigorous physical activity (MVPA) occur in physical education in schools.10, 11
Previous intervention studies have focused primarily on school settings. The Middle School Physical Activity and Nutrition (M-SPAN) study targeted physical activity change in physical education class and other periods throughout the school day and noted an increase in observer-recorded physical activity in the intervention schools relative to control schools for boys, but not for girls.12 The Child and Adolescent Trial for Cardiovascular Health (CATCH)13 and the Sports, Play and Active Recreation for Kids (SPARK)14 studies reported increased physical activity in physical education class in intervention compared to control schools. CATCH found a concomitant increase in vigorous physical activity from self-reported assessment that was sustained over additional follow-up periods.15 The Pathways study noted intervention–control differences in physical activity measured by self-report, but not accelerometry.16 The Lifestyle Education for Activity Program (LEAP), an environmental intervention, targeted girls in South Carolina high schools and found increased vigorous physical activity in intervention compared with control schools as measured by self-report.17 In Belgium, a middle school physical activity and healthy eating intervention showed positive intervention effects on physical activity for both boys and girls18 and on BMI for girls.19
The National Heart, Lung, and Blood Institute (NHLBI) sponsored the multi-center group-randomized Trial of Activity for Adolescent Girls (TAAG) to develop, implement, and evaluate an intervention that linked schools to community organizations to reduce the age-related decline in MVPA in middle school girls.20 TAAG was designed to overcome limitations in previous intervention studies following guidelines proposed by the CDC.21 Cooperative agreements funded field centers at the University of Arizona, San Diego State University, Tulane University, the University of Maryland, the University of Minnesota, and the University of South Carolina. The Coordinating Center was at the University of North Carolina, Chapel Hill. The NHLBI project office collaborated in the research. The purpose of this paper is to report the primary and secondary outcomes of TAAG.
Methods
Specific Objectives and Hypotheses
The primary aim of TAAG was to test an intervention to reduce by half the observed decline in MVPA experienced by adolescent girls. Based on prior data about the magnitude of decline, TAAG was powered to detect a difference of 14.5 MET-weighted minutes of MVPA, favoring girls in intervention schools compared to girls in control schools at the 8th grade.20, 22 One MET-minute represents one metabolic equivalent of energy expended for 1 minute. Secondary aims, at the individual level, were to examine the impact of the intervention on percent body fat, and at the school and community levels, to examine differences in the delivery of physical education classes and after-school physical activity programs. An additional secondary aim was to determine the effects on study outcomes after a third year of intervention directed by school and community staff.
Study Design
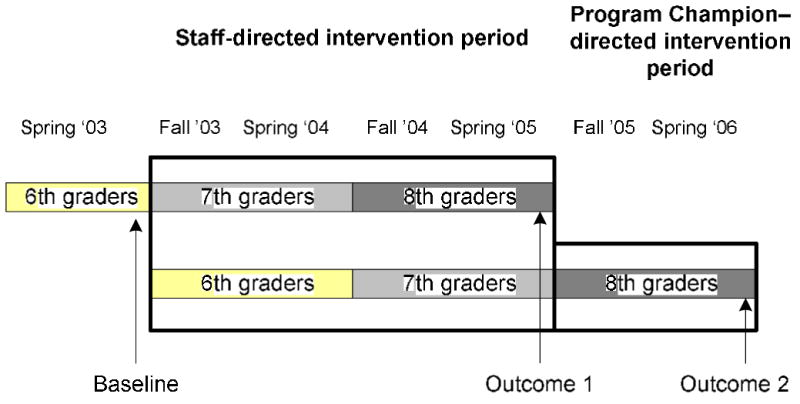
Six schools at each of the six field centers were randomized in equal numbers to either intervention or control condition after baseline measurements were collected.20,22 The TAAG staff-directed intervention began in fall 2003 and lasted through spring 2005 when the primary outcome data were collected. The intervention, as directed by school and community personnel (Program Champion–directed intervention), lasted from fall 2005 through spring 2006. Cross-sectional, random samples of girls were recruited for measurement in spring 2003 (6th grade), spring 2005 (8th grade), and spring 2006 (8th grade) (Figure 1). This repeated cross-sectional design was chosen both to allow us to assess intervention effects in the entire population of girls enrolled in the participating schools at the time of the surveys and to avoid the need for substantial imputation of missing data that would occur with a cohort design.20 Thus, 8th-grade girls measured in spring 2005 received 2 years of staff-directed intervention (7th and 8th grades), and girls measured in spring 2006 received 2 years of staff-directed intervention (6th and 7th grades) plus an additional year of Program Champion–directed intervention (8th grade). TAAG staff was blinded to the study outcomes until the 2006 data collection was complete. Control schools received a delayed intervention after all measurements were obtained.
Figure 1.

Trial of Activity for Adolescent Girls (TAAG) study design. Six schools at each field center were randomized into intervention or control condition after baseline measurements were collected in 6th-grade girls in fall 2003. After the staff-directed intervention during spring 2005 and again after the Program Champion–directed intervention in spring 2006, outcome measurements were obtained in separate sets of 8th-grade girls.
Eligibility and Recruitment
Public middle schools in which a majority of students lived in the surrounding community were eligible to participate. Additional school eligibility criteria included: (1) enrollment of at least 90 8th-grade girls, (2) yearly withdrawal rates less than 28%, (3) at least one semester of physical education required for each grade, and (4) willingness to sign a memorandum of understanding and accept random assignment of the school. TAAG schools represented the demographic and socioeconomic makeup of their school districts, with preference given to schools with greater racial/ethnic and socioeconomic diversity. Of the 68 schools invited to participate, 41 agreed and the 36 most conveniently accessed from the university-based research centers were selected. Details are presented elsewhere.23,24
Parental consent and student assent were obtained prior to each measurement period. A student was excluded if she had limited English-speaking skills, was unable to participate in physical education classes due to a medical condition or disability, or had contraindications for participating in a submaximal exercise test (2005 measurements only). The parental consent and student assent forms and the protocol were approved by the institutional review boards of all participating institutions in fall 2002 and annually thereafter.
TAAG Intervention
The TAAG intervention25 incorporated operant learning theory,26 social cognitive theory,27 organizational change theory,28 and the diffusion of innovation model29 in a social-ecologic framework.30–34 Intervention activities based on extensive formative research were targeted to create (1) environmental and organizational changes supportive of physical activity and (2) cues, messages, and incentives to be more physically active. Specifically, the intervention was designed to establish more opportunities, improve social support and norms, and increase self-efficacy, outcome expectations, and behavioral skills to foster greater MVPA.35–40 Girls were the focus of the intervention; however, health and physical education classes were part of the usual school curriculum and most included boys as well.
An innovative feature of the intervention was linking school and community agencies to develop and promote physical activity programs for girls. These programs were delivered both on and off school property, in most cases either before or after school. Immediately following randomization, intervention staff identified school and community partners to plan and implement programs and events. Community partners included the YMCA or YWCA, local health clubs, and community recreation centers. Examples of programs include lunch-time Dance Dance Revolution, after-school step-aerobics class, before-school open gym, basketball camp, touch football, and weekend canoe programs. Programs did not replace physical education class.
TAAG health education included six lessons in each of the 7th and 8th grades designed to enhance behavioral skills known to influence physical activity participation. Activity challenges associated with the lessons reinforced the contents, encouraged self-monitoring, and set goals for behavior change. To meet the varying formats in which health education was taught at the school, TAAG health education was offered in two forms: one for a traditional classroom setting and one for physical education class.
TAAG physical education class promoted MVPA for at least 50% of class time and encouraged teachers to promote physical activity outside of class. Physical education teachers were trained by TAAG interventionists on class management strategies, skill-building activities, the importance of engaging girls in MVPA during class, and the provision of appropriate equipment and choices of physical activity. TAAG promotions used a social marketing approach41 to promote awareness of and participation in activities through media and promotional events.38 TAAG promotions also provided schoolwide messages designed to increase the acceptance and support for physical activity for all girls.
A TAAG Program Champion component was developed to foster sustainability after the 2-year staff-directed intervention. This component was based on previous research suggesting that youth-based health promotion programs have a greater likelihood of being sustained if one or several individuals in the school or community take ownership of the program after the research-directed intervention phase has ended. Thus, TAAG investigators actively recruited and trained Program Champions during the staff-directed intervention phase as a way to promote maintenance of the program. Program Champions sustained program efforts by advocating for TAAG activities with policymakers and school- and community-level implementers.42–44 Each field center identified at least two Program Champions per school during the second year of the staff-directed intervention phase. Most of the Program Champions had been involved previously in the intervention as a physical education teacher or community liaison. They received additional training and worked with TAAG staff during the second year of the staff-directed intervention. During the third year, Program Champions continued existing intervention activities and developed new programs where possible with minimal support from TAAG staff. They received a modest stipend not exceeding $4000 per year.
Measurements
Measurements were taken during spring 2003, 2005, and 2006. Separate intervention and measurement staff were employed, and separate central training sessions were held to train and certify staff. These certified staff then trained additional site staff as needed. Periodic recertification ensured that performance standards were met continuously.
Race/ethnicity
Each girl responded to two questions. The first asked whether the girl thought of herself as Hispanic, Mexican American, or of Spanish origin. The second asked whether the girl thought of herself as white, black or African-American, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, or other.
Physical activity assessed by accelerometry
Physical activity was measured using Actigraph accelerometers (MTI model 7164). Each girl wore an accelerometer during waking hours for 7 consecutive days. Accelerometers were initialized to begin collecting data at 5:00 AM on the day after they were distributed; thus, data for 6 complete days were available for analysis. Data were collected and stored in 30-second intervals. Girls wore the accelerometer on their right hip, attached to a belt, except while bathing, swimming, or sleeping. Data were collected for 3–4 weeks in each school, with different girls measured each week. Intervention and control schools were measured at the same time; almost 90% of the girls were measured in the first 2 weeks, with the remainder scheduled over the next 2–3 weeks.
Accelerometry data were reduced using methods previously described.45,46 Briefly, missing accelerometry data within a girl’s 6-day record were replaced via imputation.47 Girls were included who had at least 1 full day of data out of the expected 6 days. On average, 12 hours (about 11%) were imputed per girl. The count threshold (counts/30 seconds) for MVPA was set at 1500 counts/30 seconds based on our previous work.45 This count represented approximately 4.6 METs, which separates slow (< 4.6 METs) and brisk (≥4.6 METs) walking. Daily MET-weighted minutes of MVPA were calculated by summing METS for MVPA over the entire day. Similar calculations were made for time period (6:00AM–9:00AM, 9:00AM–2:00PM, 2:00PM–5:00PM, 5:00PM–8:00 PM, 8:00PM–midnight) and for weekend versus weekday. Total physical activity was defined as the sum of light, moderate, and vigorous activity. Sedentary minutes were defined as the number of minutes with less than light activity.
Body composition
Standing height was measured without shoes using a portable stadiometer (Shorr Productions) to the nearest 0.1 cm. Body weight was assessed using a digital scale (Seca 880) and measured to the nearest 0.1 kg while the girl was dressed in light clothing without shoes. Triceps skinfold thickness was measured in triplicate on the right side of the body to the nearest 0.1 mm. BMI was calculated as weight (kg)/height (m2).48 Percent body fat was estimated from anthropometric measures using an equation that was developed for use in girls in this age range,49 and was highly correlated with percent body fat measured from dual energy X-ray absortiometry (DEXA) (r2=0.88, root mean square error [RMSE] =3.6%).
Process evaluation
Structured observations, questionnaires, semistructured interviews, and logs were developed to assess fidelity, dose, reach, and exposure of the intervention components. Trained observers visited health and physical education classes to determine the extent to which lessons were fully taught and intervention concepts were addressed. Questionnaires and interviews provided additional information, including use of TAAG materials, intervention acceptability, and number of TAAG programs. Data were collected at different time intervals depending on the structure of each intervention component. For example, attendance at TAAG programs was assessed continuously, whereas implementation of health education lessons was assessed yearly.
Activity in physical education class
Class-level physical activity in physical education class was measured by the system for observing fitness instruction time (SOFIT).50 A minimum of four physical education lessons were observed at each of the three visits to each intervention and control school during each of the three measurement semesters.
Statistical Methods
All inferential analyses employed mixed-model regression methods to reflect the group randomization and the nesting of students within schools, sites, and conditions.51 The analyses were conducted in two stages, as if there were no overlap among girls measured in the three cross-sectional samples.22 The analyses were performed separately for the two 8th-grade surveys, with each using the same 6th-grade survey to adjust for baseline.
In the first stage, the dependent variable was regressed on school, time (6th or 8th grade), their interaction, and ethnicity; study condition was not included. The results of the first stage were two ethnically-adjusted mean values (6th grade and the first 8th-grade sample) for each of the 36 schools for the first set of analyses and for each of the 34 schools for the second set of analyses (6th grade and the second 8th-grade sample). Two schools in Louisiana were lost from the second set because they closed due to damage from Hurricane Katrina. No data for these schools were used, as their loss was unrelated to treatment and so ignorable.
The second-stage analysis was conducted on the adjusted means from the first stage. Finding no evidence of a differential intervention effect among the six sites, the follow-up school mean was regressed on condition, adjusting for the 6th-grade school mean and stratifying on site, which was modeled as a random effect.
For the assessment of accelerometry data, the analysis included an additional random effect for measurement week. In analyses without 6th-grade data, the first stage calculated race-adjusted school means at 8th grade, and the second stage analyzed those means with treatment condition as a fixed effect and site as a random effect.
Planned secondary analyses tested for differential effects by race and ethnic group; these analyses were restricted to whites, African Americans, and Hispanics because the sample size available for the other racial/ethnic groups was too small. The parametric analyses described above were also considered valid for analyzing ordinal data obtained through a Likert scale survey, such as the data for assessment of TAAG intervention reach.52
All analyses were conducted using SAS, version 9.1.3. Additional details on the analyses are available in two earlier publications.20, 22
Results
Study Sample
All 36 schools participated in the 6th-grade measurements during spring 2003 and in the 8th-grade measurements during spring 2005; however, only 34 schools participated in the 8th-grade measurements during spring 2006. During 2003 spring, 60 girls per school were randomly chosen. A total of 1721 (79.7%) of the 2160 eligible girls consented and participated in the measurement (Figure 2). During 2005 spring, 4123 girls were eligible for the student-level measurements, and 3504 (85.0%) consented and participated in the measurements (Figure 2). During 2006 spring, 3915 were eligible at the six study sites, and 3502 (89.5%) consented and participated in the measurements (Figure 2). The approximate doubling of the number of girls measured in each 8th-grade survey compared to the 6th-grade survey was purposeful and based on our determination that the smaller 6th-grade sample would have little adverse effect on power.20 The study population was diverse with the largest percentage of African-American girls in Louisiana and South Carolina and the largest percentage of Hispanic girls in California and Arizona (Table 1).
Figure 2.
Sample selection: spring 2003 baseline, 6th grade; spring 2005 follow-up, 8th grade; and spring 2006 follow-up, 8th grade.
Table 1.
Sample size at 6th grade (spring 2003) and 8th grade (spring 2005 and spring 2006) by site and ethnicity/race, Trial of Activity for Adolescent Girls (TAAG)
| White | African-American | Hispanic | Other* | Total | |
|---|---|---|---|---|---|
| Spring 2003** | |||||
| Arizona | 131 | 4 | 70 | 48 | 253 |
| California | 120 | 23 | 71 | 97 | 311 |
| Louisiana | 48 | 194 | 32 | 37 | 311 |
| Maryland | 126 | 72 | 26 | 41 | 265 |
| Minnesota | 232 | 4 | 7 | 40 | 283 |
| South Carolina | 137 | 108 | 6 | 47 | 298 |
| Total | 794 (46.1%) | 405 (23.5%) | 212 (12.3%) | 310 (18.0%) | 1721 |
|
| |||||
| Spring 2005** | |||||
| Arizona | 249 | 5 | 191 | 46 | 491 |
| California | 198 | 32 | 275 | 91 | 596 |
| Louisiana | 95 | 365 | 94 | 61 | 615 |
| Maryland | 293 | 153 | 95 | 92 | 633 |
| Minnesota | 503 | 15 | 38 | 81 | 637 |
| South Carolina | 240 | 201 | 45 | 46 | 532 |
| Total | 1578 (45.0%) | 771 (22.0%) | 738 (21.1%) | 417 (11.9%) | 3504 |
|
| |||||
| Spring 2006** | |||||
| Arizona | 255 | 9 | 196 | 38 | 498 |
| California | 219 | 38 | 310 | 103 | 670 |
| Louisiana | 74 | 152 | 97 | 53 | 376 |
| Maryland | 294 | 159 | 94 | 114 | 661 |
| Minnesota | 495 | 22 | 36 | 95 | 648 |
| South Carolina | 289 | 236 | 57 | 67 | 649 |
| Total | 1626 (46.4%) | 616 (17.6%) | 790 (22.6%) | 470 (13.4%) | 3502 |
Asian, American Indian, Multi-ethnic, or missing
In spring 2003, 60 randomly selected girls per school were recruited. In spring 2005 and spring 2006, 120 randomly selected girls per school were recruited.
Physical Activity
During spring 2005, after the first 2 years of intervention (prestated primary outcome), there was no difference (mean= −0.4, 95% CI= −8.2 to 7.4) in adjusted MET-weighted minutes of MVPA between 8th-grade girls in schools assigned to intervention or control. The average daily minutes of MET-weighted minutes of MVPA declined from 146 (±81.8) in 6th-grade girls to 136 (±74.3) in 8th-grade girls in 2005. However, during spring 2006, after 3 years of intervention, 8th-grade girls in the intervention schools had 10.9 more MET-weighted minutes of MVPA than 8th-grade girls in the control schools (p=0.03) (Table 2). The mean MET-weighted minutes of MVPA were about the same in intervention schools for both 8th-grade measurements, but were lower in control schools during the second measurement period, representing about a 15% decrease from 6th grade. The decrease in MET-weighted minutes of MVPA in intervention schools from 6th grade to 8th grade in 2006 was only 6%, or less than half that observed in the control schools.
Table 2.
Adjusted* mean minutes of physical activity per day at 6th grade (spring 2003) and 8th grade (spring 2005 and spring 2006) by treatment group, Trial of Activity for Adolescent Girls (TAAG)
| Intervention Mean | Control Mean | Difference
|
|||
|---|---|---|---|---|---|
| Mean | 95% CI | ||||
| MET-weighted minutes of MVPA | 6th grade** | 145.0 | 147.2 | −2.2 | −13.2, 8.9 |
| 8th grade—spring 2005 | 136.5 | 136.9 | −0.4 | −8.2, 7.4 | |
| 8th grade—spring 2006 | 136.4 | 125.5 | 10.9a | 0.5, 21.2 | |
| Minutes of MVPA | 6th grade | 23.7 | 23.7 | −0.0 | −1.7, 1.7 |
| 8th grade—spring 2005 | 22.2 | 22.4 | −0.2 | −1.4, 1.0 | |
| 8th grade—spring 2006 | 22.4 | 20.8 | 1.6a | 0.0, 3.3 | |
| Minutes of total PA | 6th grade | 366.4 | 368.3 | −2.0 | −12.2, 8.3 |
| 8th grade—spring 2005 | 317.7 | 325.6 | −7.9 | −14.9, −1.0 | |
| 8th grade—spring 2006 | 317.4 | 316.8 | 0.6 | −4.0, 5.3 | |
| Minutes of sedentary behavior | 6th grade | 456.5 | 458.0 | −1.5 | −10.8, 7.9 |
| 8th grade—spring 2005 | 510.5 | 514.0 | −3.5 | −11.1, 4.2 | |
| 8th grade—spring 2006 | 524.4 | 532.6 | −8.2a | −16.5, 0.0 | |
School means adjusted for race and measurement wave (most girls were measured over three to four nonconsecutive weeks) in Stage 1 model. These adjusted school means are the dependent variable in Stage 2 model, with treatment group and 6th grade level of physical activity (for 8th grade outcome) as fixed effects and school nested within site and site as random effects.
The mean values reported for a given row are comparable within a row because all were derived from the same analysis and standardized in the same way. However, the three rows represent three separate analyses so that arithmetic comparisons between rows are not appropriate for each outcome.
6th grade—spring 2003, n = 1603 girls had sufficient accelerometry data following imputation for occasionally missing values
8th grade—spring 2005, n = 3085 girls had sufficient accelerometry data following imputation for occasionally missing values
8th grade—spring 2006, n = 3378 girls had sufficient accelerometry data following imputation for occasionally missing values
p<0.05
Sixth-grade girls in control schools had 2.2 more MET-weighted minutes of MVPA than did girls in intervention schools (p>0.05) (Figure 3). By spring 2005, this difference decreased to 0.4 minutes of MET-weighted MVPA. By spring 2006, this difference was 10.9 mean MET-weighted minutes favoring the intervention schools.
Figure 3.

Differences in adjusted mean MET-weighted minutes of MVPA per day between intervention and control schools. The bars represent 95% CIs for the adjusted differences. Girls in control schools had 2.2 minutes more of MET-weighted minutes of MVPA during 6th grade baseline (p>0.05). By spring 2005, this difference decreased to 0.4 MET-weighted minutes of MVPA (p>0.05). By spring 2006, girls in intervention schools had 10.9 adjusted mean MET-weighted minutes of MVPA more than girls in control schools (p<0.05). MVPA, moderate-to-vigorous physical activity
A significant difference between intervention and control schools in spring 2006 also was noted for minutes of MVPA (p=0.049), but not for minutes of total physical activity. In addition, in spring 2006, the girls in the control schools had 8.2 more minutes of daily sedentary activities (p=0.050).
Race/Ethnicity and Physical Activity
There were no significant interactions between treatment and race/ethnicity for either the primary outcome variable or any of the secondary outcome variables (Table 3). There were statistically significant differences, however, in the number of MET-weighted minutes of MVPA among the three largest racial/ethnic groups. In the 6th-grade sample in 2003, African-American and white girls had a greater number of minutes of MET-weighted and unweighted minutes of MVPA in both the intervention and control groups than did Hispanic girls. After adjusting for 6th-grade activity differences, both MET-weighted minutes and unweighted minutes of MVPA were higher for white girls than for African-American and Hispanic girls in both spring 2005 and spring 2006.
Table 3.
Adjusted* mean minutes of physical activity per day at 6th grade (Spring 2003) and 8th grade (spring 2005 and spring 2006) by treatment group and race/ethnicity, Trial of Activity for Adolescent Girls (TAAG)
| Black (non-Hispanic) | Hispanic | White | |||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | ||
| Primary outcome | |||||||
| MET-weighted minutes of MVPA | 6th grade** | 148.5 | 152.4 | 141.9 | 127.2 | 148.9 | 157.8 |
| 8th grade—spring 2005 | 131.3 | 137.6 | 131.6 | 132.1 | 140.9 | 142.2 | |
| 8th grade—spring 2006 | 129.0 | 124.5 | 137.6 | 113.3 | 140.4 | 130.6 | |
| Secondary outcomes | |||||||
| Minutes of MVPA | 6th grade | 24.2 | 24.6 | 23.5 | 21.0 | 24.2 | 24.9 |
| 8th grade—spring 2005 | 21.6 | 22.6 | 21.8 | 21.6 | 22.8 | 23.0 | |
| 8th grade—spring 2006 | 21.3 | 20.9 | 23.1 | 18.9 | 23.0 | 21.3 | |
| Minutes of total PA | 6th grade | 365.2 | 370.6 | 363.2 | 360.9 | 367.3 | 365.8 |
| 8th grade—spring 2005 | 326.5 | 329.1 | 320.9 | 323.9 | 313.6 | 325.0 | |
| 8th grade—spring 2006 | 327.6 | 328.0 | 323.6 | 316.5 | 310.5 | 312.5 | |
| Minutes of sedentary behavior | 6th grade | 425.8 | 468.8 | 451.5 | 463.4 | 462.8 | 452.3 |
| 8th grade—spring 2005 | 506.3 | 513.3 | 513.3 | 516.2 | 507.8 | 511.2 | |
| 8th grade—spring 2006 | 528.6 | 529.9 | 514.5 | 529.0 | 523.6 | 532.5 | |
School means adjusted for race, and measurement wave (most girls were measured over three to four nonconsecutive weeks) in stage 1 model. These adjusted school means are the dependent variable in Stage 2 model, with treatment group and 6th grade level of physical activity (for 8th grade outcome) as fixed effects and school nested within site and site as random effects.
6th grade—spring 2003, n = 1603 girls had sufficient accelerometry data following imputation for occasionally missing values
8th grade—spring 2005, n = 3085 girls had sufficient accelerometry data following imputation for occasionally missing values
8th grade—spring 2006, n = 3378 girls had sufficient accelerometry data following imputation for occasionally missing values
There were no statistically race/ethnicity by treatment group interactions.
Time of Day and Physical Activity
The significant difference in the number of MET-weighted minutes of MVPA noted during spring 2006 was seen more during weekdays than weekends. Girls in intervention schools had 13.5 (95% CI=0.3 to 26.7) additional MET-weighted minutes of weekday MVPA and 1.6 (95% CI= −5.9 to 9.1) additional MET-weighted minutes of weekend MVPA than did girls in control schools. For weekday MVPA, about half of this difference, 7.3 MET-weighted minutes (95% CI=3.1 to 11.5) was reflected during the afternoon period (2:00PM–5:00PM). Although not statistically significant, there were 4.1 (95% CI= −3.1 to 11.4) more mean MET-weighted minutes of MVPA from 9:00AM to 2:00PM for girls in intervention compared with control schools. This latter finding also had been noted during spring 2005 when girls in intervention schools had 2.1 (95% CI= −1.6 to 5.8) MET-weighted minutes more MVPA than did girls in control schools.
Process Evaluation
During the staff-directed intervention, between 86% and 96% of teachers attended yearly health education and physical education training workshops and additional booster sessions. Most of those who missed the workshops attended make-up sessions. Across schools and sites, 93% and 89% of health education lessons were taught in Years 1 and 2, respectively, with 91% and 77% of 7th- and 8th-grade girls, respectively, receiving the lessons. Of the more than 300 yearly structured observations of physical education classes, TAAG strategies were observed in 66% (first year) and 68% (second year) of classes. One of the physical education intervention goals was for teachers to encourage girls to participate in more in-class and out-of-class physical activity. Observation of this behavior was recorded for both control and intervention schools. During the first 2 years of the intervention, encouragement of out-of-class physical activity was observed in 18.0% (first year) and 28.4% (second year) of physical education classes, but was not different in intervention compared to control school classes.
For each semester of the first 2 intervention years, the average number of programs created from linking schools with community agencies was 4.7, 7.6, 6.3, and 5.9 programs per school. Average program attendance per session by semester was 18.1, 11.5, 16.1, and 13.9 attendees/session. Table 4 indicates that girls in intervention schools were more aware of TAAG concepts than girls in control schools.
Table 4.
Measures of TAAG intervention reach* at 8th grade (spring 2005 and spring 2006) by treatment group, Trial of Activity for Adolescent Girls (TAAG)
| Spring 2005 (n = 3504) | Spring 2006 (n = 3502) | |||||||
|---|---|---|---|---|---|---|---|---|
| Difference | Difference | |||||||
| During this school year … | Intervention mean** | Control mean** | mean | 95% CI | Intervention mean** | Control mean** | mean | 95% CI |
| 1. …some lessons included physical activity for homework. | 3.1 | 2.4 | 0.7a | (0.4, 0.9) | 2.5 | 2.4 | 0.1 | −0.2, 0.3 |
| 2. …in class we were given pedometers to help us monitor our own physical activities and set goals for daily steps. | 4.2 | 1.8 | 2.4a | (2.0, 2.7) | 2.7 | 1.9 | 0.8a | 0.4, 1.2 |
| 3. …in class we learned about light, moderate, and vigorous physical activity. | 4.1 | 2.6 | 1.4a | (1.2, 1.7) | 3.1 | 2.7 | 0.5a | 0.2, 0.7 |
| 4. … when we do group activities in physical education class, the size of groups is usually small. | 3.6 | 3.2 | 0.4a | (0.2, 0.7) | 3.3 | 3.2 | 0.1 | −0.1, 0.4 |
| 5. …my physical education teacher encourages me to be physically activity outside of physical education class. | 3.7 | 3.3 | 0.4a | (0.2, 0.7) | 3.4 | 3.4 | 0.1 | −0.2, 0.3 |
| 6. … my physical education teacher encourages us to keep moving in physical education class. | 4.1 | 3.8 | 0.3a | (0.0, 0.5) | 4.0 | 3.9 | 0.0 | −0.2, 0.2 |
| 7. …there are many ways for me to be physically active at school when not in class. | 3.6 | 3.4 | 0.3a | (0.1, 0.4) | 3.5 | 3.5 | 0.0 | −0.2, 0.1 |
Scale for all responses ranges from 1 = ‘Disagree a lot’ to 5 = ‘Agree a lot’
School means adjusted for race in stage 1 model. These adjusted school means are the dependent variable in Stage 2 model, with treatment group as fixed effect and school nested within geographic location and site as random effects
p<0.05
During the Program Champion–directed phase, there were no mandated health education or physical education training workshops; however, 51% of 8th-grade girls were taught the health education lessons. There was an average of 4.6 programs per school in the fall 2005 and 4.9 programs in spring 2006. Attendance at programs was not documented in this phase of the intervention. Out-of-class physical activity encouragement by physical education teachers was observed in 16.4% of physical education classes. As shown in Table 4, differences in awareness of TAAG intervention activities diminished in spring 2006.
Physical Education Class
Physical education classes were observed at each intervention and control school at 6th-grade and 8th-grade measurement (Table 5). The percentage of time devoted to MVPA during physical education class was about 4% greater in intervention than control schools at both 8th-grade periods, and was statistically significant (p=0.025) during spring 2006.
Table 5.
Mean percent of time in moderate to vigorous and vigorous activity in physical education classes at 6th grade (spring 2003) and 8th grade (spring 2005 and spring 2006) by treatment group, Trial of Activity for Adolescent Girls (TAAG)
| Intervention mean | Control mean | Difference
|
||
|---|---|---|---|---|
| mean | 95% CI | |||
| 6th grade (n=431) | 38.1 | 38.0 | −0.1 | −4.9, 4.8 |
| 8th Grade—spring 2005 (n=430) | 42.2 | 38.3 | 3.9 | −1.6, 9.4 |
| 8th Grade—spring 2006 (n=352) | 40.4 | 36.3 | 4.1a | 0.5, 7.7 |
p< 0.05 (spring 2003)
Body Composition and Fitness
Height increased by about 7.5 cm and weight increased by about 10 kg for students from 6th to 8th grade. Triceps skinfold thickness was about 4–5 cm greater at 8th grade than at 6th grade. Percent body fat increased from about 28 % at 6th grade to about 31% at 8th grade (Table 6). Changes were similar in the intervention and control schools.
Table 6.
Body composition at 6th grade (spring 2003) and 8th grade (spring 2005 and spring 2006) by treatment group, Trial of Activity for Adolescent Girls (TAAG)
| Intervention mean** | Control mean** | Difference | |||
|---|---|---|---|---|---|
| mean | 95% CI | ||||
| Age (years) | 6th grade*** | 11.9 | 12.0 | −0.0 | −0.1, 0.2 |
| 8th grade—spring 2005 | 14.0 | 14.0 | 0.0 | −0.0, 0.1 | |
| 8th grade—spring 2006 | 14.0 | 14.0 | 0.0 | −0.1, 0.1 | |
| Height (cm) | 6th grade | 152.3 | 152.4 | −0.1 | −0.8, 0.6 |
| 8th grade—spring 2005 | 160.1 | 160.2 | −0.1 | −0.8, 0.6 | |
| 8th grade—spring 2006 | 159.7 | 159.9 | −0.2 | −0.9, 0.5 | |
| Weight (kg) | 6th grade | 48.6 | 49.1 | −0.5 | −2.5, 1.5 |
| 8th grade—spring 2005 | 58.4 | 59.1 | −0.6 | −1.7, 0.4 | |
| 8th grade—spring 2006 | 58.4 | 58.2 | 0.2 | −1.2, 1.6 | |
| BMI (kg/m2) | 6th grade | 20.7 | 20.9 | −0.2 | −1.0, 0.6 |
| 8th grade—spring 2005 | 22.7 | 22.9 | −0.2 | −0.6, 0.2 | |
| 8th grade—spring 2006 | 22.8 | 22.7 | 0.1 | −0.4, 0.7 | |
| Triceps skinfold thickness (mm) | 6th grade | 17.2 | 17.4 | −0.2 | −1.4, 1.0 |
| 8th grade—spring 2005 | 21.2 | 21.6 | −0.3 | −1.2, 0.6 | |
| 8th grade—spring 2006 | 21.2 | 20.8 | 0.4 | −0.5, 1.4 | |
| * Percent body fat | 6th grade | 27.8 | 28.1 | −0.3 | −1.7, 1.2 |
| 8th grade—spring 2005 | 31.5 | 31.8 | −0.3 | −1.2, 0.6 | |
| 8th grade—spring 2006 | 31.5 | 31.3 | 0.2 | −0.6, 1.1 | |
Percent body fat = −23.911 + 2.283 * BMI + 1.917 * triceps – 0.057 * (BMI * triceps) – 0.492 * age –3.122 * black_race
School means adjusted for race in stage 1 model. These adjusted school means are the dependent variable in Stage 2 model, with treatment group as a fixed effect and school nested within geographic location and site as random effects.
6th grade—spring 2003 (n=1721)
8th grade—spring 2005 (n=3504)
8th grade—spring 2006 (n=3502)
None of the differences were statistically significant (p>0.05).
Discussion
Over the 3 years of TAAG, there was a modestly higher level of physical activity for girls in intervention schools compared to girls in control schools. In 6th grade, girls in control schools had about 2.2 MET-weighted minutes more per day of MVPA than did girls in intervention schools. At the end of the staff-directed intervention, there was less than 1 MET-weighted-minute-per-day difference between girls in the two sets of schools (prestated primary outcome); however, at the end of the Program Champion–directed intervention, girls in intervention schools had almost 11 MET-weighted minutes more per day of MVPA than did girls in control schools. This is equivalent to 3.5 minutes of brisk walking per day.
One explanation for detecting an intervention effect in 2006 but not in 2005 is that the girls in control schools measured in spring 2005 were unusually physically active. If true, this is likely to have been by chance. An alternative explanation is that the girls, some of whom were recruited in 2003, were more active because they had been previously exposed to TAAG recruitment activities. Recruitment of girls in 2003, which occurred prior to randomization, tended to have more enthusiasm-generating activities to introduce TAAG to the schools compared with recruitment strategies used in subsequent years. Although this explanation is consistent with the results, it is not very plausible. Recruitment activities are not likely to influence physical activity 2 years later.
The length of time girls were exposed to the TAAG intervention was different for girls measured in 2005 versus 2006. Girls measured in 2005 did not receive TAAG messages or a new school environment during their first year in middle school; indeed, except for the spring 6th-grade measurement recruitment activities, their initial exposure occurred the next fall in 7th grade. Intervention girls measured in spring 2006 entered a TAAG intervention school as 6th graders (fall 2003) just as the TAAG intervention was getting started. Their entire middle school experience occurred in a school that was saturated with messages about the value of being active and with concentrated efforts to create a social norm for girls to be active. Creating environmental change at both the social and physical levels is most important during key transitional times of adolescence.53 The ability to change behavior may have been constrained by the expectation and social norms that they learned in their 6th-grade year.
Another possible explanation for the findings could be due to an unanticipated consequence of attribution procedures used to replace occasional missing accelerometer data. Girls measured in 2005 were not as compliant with wearing the accelerometers as girls measured in 2006, nor were they as compliant with wearing the accelerometers as those in the control schools. To ensure that attribution procedures were not obscuring an intervention effect, additional analyses, eliminating attribution of missing accelerometer data altogether, were conducted. Those analyses resulted in findings similar to those reported here, so attribution of occasional missing accelerometer data does not appear to be an explanation for the results reported here.
The differences in the racial makeup of the schools included in the 2005 and 2006 analyses may be a possible explanation for the differences in physical activity in the control schools in 2005 compared to 2006. The two schools that closed because of Hurricane Katrina enrolled predominantly African-American students, and data show that MVPA was higher in the 2005 control condition, more so among African-American students than among Hispanic or white students. Additional analyses of the 2005 data were conducted after removing these two schools, and the results did not change; thus, differences in the racial makeup of the schools included in the 2005 and 2006 analyses do not provide an explanation for the results.
Finally, the possible impact of school self-selection and the differential recruitment of girls were considered. As only 41 of 68 schools that were contacted ultimately agreed to be in the study, there is the prospect of a volunteer bias limiting external validity. Nevertheless, this represents a substantial proportion (60%) of eligible schools. All were aware that there was an equal chance of being in either the intervention or control condition, thereby minimizing any potential threats to validity. Recruitment was more effective at the 2006 follow-up than at the 2005 follow-up. Four of six sites exceeded the 80% recruitment criterion in spring 2005, increasing to five of six sites in spring 2006, with all five of these sites actually exceeding 90% recruitment. Improved recruitment techniques and/or greater receptivity may have contributed to the improved results in 2006, but only if it was more likely that less-active girls in the control condition in 2006 were recruited. It is unlikely, however, that such a selective recruitment pattern occurred.24
The greatest difference between intervention and control schools in MET-weighted minutes of MVPA occurred on weekdays between 2PM and 5PM. Girls in intervention schools averaged 7.3 more minutes of MET-weighted minutes of MVPA than girls in the control schools. This time period corresponds to after school, which is when the majority of TAAG programs were held. This pattern was present in 2005, although not significant, and it was both present and significant in 2006. This finding offers additional support for concluding that the TAAG intervention was effective.
The similarity in the physical activity outcomes for the intervention schools in 2005 and 2006 suggests that the Program Champions were able to sustain the intervention sufficiently to maintain the MVPA levels observed when the intervention was directed by program staff. Although there was a decline in intervention implementation and reach in 2006 compared with 2005, the Program Champions may have tailored the programs to the unique needs of their schools, communities, and girls in ways that resulted in maintained MVPA. More research is needed to examine the utility and effectiveness of identifying and training school and community-based program champions during a staff-directed intervention.
Conclusion
Although the TAAG intervention was intense and well-received by the middle school girls, the results, although statistically significant for the 2006 measurements, were modest. The difference in daily minutes of MVPA for girls in intervention schools compared to girls in control schools was only 1.6 minutes. Because activities at or above moderate intensity expend approximately 30 kJ/min (7.17 kcal/min) in adolescent girls,54 this would translate into 80 kcal/week or 2880 kcal/36-week of additional energy expenditure. Assuming that a 3500-kcal decrease in energy expenditure leads to an average of 0.454 kg (1 pound) weight gain as fat, these results suggest that an increase of this magnitude could prevent a weight gain of 0.82 kg per year. Although this amount is small on an individual basis, it could be substantial at the population level. Small population shifts in physical activity, if sustained for enough time, can have important public health implications, particularly in addressing the obesity epidemic. Using National Health and Nutrition Examination Survey (NHANES) data, Wang et al.55 reported a 0.43 kg/year excess weight gain over a 10-year period for children aged 2 to 7 years. This corresponds to excess energy of 110–165 kcal per day. Although this age group is younger compared to the girls in TAAG, children gain more weight between ages 9–12 years56; hence, a more physically active lifestyle would be more crucial at the middle school ages. TAAG also showed a reduction of 8.2 minutes of sedentary behavior in girls in the intervention schools compared with those in the control schools during spring 2006.
The lack of a difference in change in body composition with modest changes in physical activity is not surprising. In a recent study of adolescent girls, increases in the percent of physical education class time in MVPA did not result in changes in BMI, body composition, or fitness related to standard physical education.57 It was unlikely that the TAAG intervention would have an effect on body composition, but these measures were included to better understand the overall potential of TAAG.
Broader-scope and longer health behavior interventions such as TAAG require time and money. In times of shrinking budgets for public school programs, all except a few basic non-academic activities are targeted for cuts, and children and parents must either fund participation themselves or accept that schools will do little more than traditional teaching. Health-related programs either must be designed so as to require little extra expenditure, or effective advocacy must be undertaken to allow them to compete for necessary resources. Creating interventions with sufficient potency to influence all students in the school is a continuing challenge.
Acknowledgments
Drs. Elder, Lohman, Lytle, Pratt, Pate, Stevens, Webber, and Young had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding/Support: This study was funded by the following cooperative agreements from the National Heart, Lung and Blood Institute: U01 HL066855 (Tulane University); U01HL066845 (University of Minnesota); U01HL066852 (University of South Carolina); U01HL066853 (University of North Carolina at Chapel Hill); U01HL066856 (San Diego State University); U01HL066857 University of Maryland); U01HL066858 (University of Arizona).
Role of the Sponsor: The Project Office at the National Heart, Lung, and Blood Institute was an equal partner in the design and implementation of the trial and in the analysis and interpretation of the data. They also approved the final version of the manuscript.
We thank the faculty and staff of the 36 schools that participated in the trial. We thank all of the girls who participated in the interventions and measurements. Participants in the TAAG Collaborative Research Group and contributors to the work reported in this publication include the following:
San Diego State University, San Diego, California: John P. Elder, MPH, PhD (principal investigator); Terry Conway, PhD; Thomas McKenzie, PhD; Jamie Moody, MS; Julie Pickrel, MPH; James F. Sallis Jr., PhD; Jean G. Williston, MEd.
Tulane University, New Orleans, Louisiana: Larry S. Webber, PhD (principal investigator); Sandra Cameron, RN; Donna Donovan; Jewel Harden, Med; Carolyn C. Johnson, PhD; Janell Jones; Rochelle Kielbon; Patricia King, MPH; Vivian G. Marino, Med; Latricia Olivier, MEd; Sheryl Pedersen, MPH; Janet C. Rice, PhD; Lakesha Stevenson, BS; Patricia Strikmiller, MS; Louisiana State University Health Sciences Center: Ariane Bedimo-Rung, PhD; Melinda Sothern, PhD; University of New Orleans: J. Mark Loftin, PhD.
University of Arizona, Tucson, Arizona: Timothy G. Lohman, PhD (principal investigator), Rob Blew, MS, Stuart Cohen, EdD, Ellen Cussler, MS, Janis Eklung, MS, Scott Going, PhD, Michele Graves, Melanie Hingle, MPH, RD, Vinson Lee, BA, Lauve Metcalfe, MS, Jennifer Reeves, MEd, Kenneth Schachter, MD, MBA, Lisa Staten, PhD, Greg Welk, PhD.
University of Maryland, College Park, Maryland: Deborah R. Young, PhD (principal investigator), Daheia Barr-Anderson, PhD, Sarah Camhi, MS, Tavon English, BA, Mira Grieser, MHS, Catherine Gurgol, MS, JoAnn Kuo, MPH, Berenice Rushovich, MSW, Brit I. Saksvig, PhD, Shumei Shang, MS, Jana Sharp, MPH, Carolyn C. Voorhees, PhD, Heidi Wilkes, MS; Johns Hopkins Bloomberg School of Public Health: Cheryl Alexander, PhD (deceased), Joel Gittelsohn, PhD, Margarita S. Treuth, PhD.
University of Minnesota, Minneapolis, Minnesota: Leslie A. Lytle, PhD (principal investigator), Joy Ahern, BA, Julie Hawkins, BS, Martha Kubik, PhD, Stacey Moe, MPH, Helen Nelson, MS, Dianne Neumark-Stzainer, PhD, Cheryl Perry, PhD, Jeanna Rex, MS, Kathryn Schmitz, PhD.
University of South Carolina, Columbia, South Carolina: Russell R. Pate, PhD (principal investigator), Cheryl Addy, PhD, Andrea Dunn, PhD, Gwen Felton, PhD, Rod Dishman, PhD, Marsha Dowda, DrPH, Dale Murrie, MAT, Deborah Parra-Medina, PhD, Karin Pfeiffer, PhD, Abby Reid, MS, Ruth Saunders, PhD, Laverne Shuler, BE.
Coordinating Center, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina: June Stevens, PhD (principal investigator), Chris Baggett, MS, James A. Bartow, Hope Bryan, MS, Diane J. Catellier, DrPH, Nancy S. Cohn, Derek Coombs, MPH, Christine E. Cox, PhD, C.E. Davis, PhD, Kelly R. Evenson, PhD, Carol A. Ford, MD, Linda Hartig, David Hill, Jung Sun Lee, PhD, James Locklear, William McGee, Robert G. McMurray, PhD, Terry Mehlman, Jesse Metzger, Kurt M. Ribisl, PhD, Kimberly B. Ring, MPH, Sherry Roberts, Kathy Roggenkamp, MS, Sherry L. Salyer, MA, Allan B. Steckler, DrPH, Dawn D. Stewart, MS, Susan G. Strohlein, MS, Daniel R Taber, MPH, Olivia Thomas, PhD, Dianne S. Ward, EdD; Ohio State University: David M. Murray, PhD.
Project Office, National Heart, Lung, and Blood Institute, Bethesda, Maryland: Charlotte A. Pratt, PhD (project officer), Robin Boineau, MD, Jared B. Jobe, PhD, Peter G. Kaufmann, PhD, Denise Simons-Morton, MD, PhD, Elaine Stone, PhD, Song Yang, PhD.
Data and Safety Monitoring Committee: Stephen Fortmann, MD (chairperson), Tom Baranowski, PhD, Bettina Beech, DrPH, Henry Feldman, PhD, Patty Freedson, PhD, Ken Resnicow, PhD.
No financial disclosures were reported by the authors of this paper.
Footnotes
The full text of this article is available via AJPMOnline at www.ajpm-online.net; 1 unit of Category-1 CME credit is also available with details on the website.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fletcher G. Physical inactivity as a risk factor for cardiovascular disease. Am J Med. 1999;107(2A):S10–S11. doi: 10.1016/s0002-9343(99)00136-9. [DOI] [PubMed] [Google Scholar]
- 2.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 3.Caspersen CJ, Pereria MA, Curran KM. Changes in physical activity patterns in the United States, by sex and cross-sectional age. Med Sci Sports Exerc. 2000;32(9):1601–9. doi: 10.1097/00005768-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 5.Obarzanek E. Obesity in children, adolescents and families. In: Fletcher GF, Grundy SM, Hyman LL, editors. Obesity: Impact on Cardiovascular Diseases. Armonk NY: Futura Publishing Company; 1999. pp. 31–53. [Google Scholar]
- 6.American Academy of Pediatrics, Council on Sports Medicine and Fitness and Council on School Health Policy Statement. Active healthy living: prevention of childhood obesity through increased physical activity. Pediatrics. 2006;117:1834–42. doi: 10.1542/peds.2006-0472. [DOI] [PubMed] [Google Scholar]
- 7.Kimm SY, Glynn NW, Kriska AM, et al. Decline in physical activity in black girls and white girls during adolescence. N Engl J Med. 2002;47(10):709–15. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- 8.Sallis JF, Zakarian JM, Hovell MF, Hofstetter CR. Ethnic, socioeconomic, and sex differences in physical activity among adolescents. J Clin Epidemiol. 1996;49:125–34. doi: 10.1016/0895-4356(95)00514-5. [DOI] [PubMed] [Google Scholar]
- 9.Stone EJ, McKenzie TL, Welk GJ, Booth ML. Effects of physical activity interventions in youth: review and synthesis. Am J Prev Med. 1998;15(4):298–315. doi: 10.1016/s0749-3797(98)00082-8. [DOI] [PubMed] [Google Scholar]
- 10.McKenzie TL, Catellier DJ, Conway T, et al. Girls’ activity levels and lesson contexts in middle school PE: TAAG baseline. Med Sci Sports Exerc. 2006;38(7):1229–35. doi: 10.1249/01.mss.0000227307.34149.f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKenzie TL, Marshall SJ, Sallis JF, Conway TL. Student activity levels, lesson context and teacher behavior during middle school physical education. Res Q Exerc Sport. 2000;71:249–59. doi: 10.1080/02701367.2000.10608905. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie TL, Sallis JF, Prochaska JJ, Conway TL, Marshall SJ, Rosengard P. Evaluation of a two-year middle-school physical education intervention: M-SPAN. Med Sci Sports Exerc. 2004;36(8):1382–8. doi: 10.1249/01.mss.0000135792.20358.4d. [DOI] [PubMed] [Google Scholar]
- 13.Luepker RV, Perry CL, McKinlay, et al. Outcomes of a field trial to improve children’s dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health: CATCH collaborative group. JAMA. 1996;275(10):768–76. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 14.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, Hovell MF. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students: sports, play and active recreation for kids. Am J Public Health. 1997;87(8):1328–34. doi: 10.2105/ajph.87.8.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nader PR, Stone EJ, Lytle LA, et al. Three-year maintenance of improved diet and physical activity: the CATCH cohort. Arch Pediatr Adolesc Med. 1999;153:695–704. doi: 10.1001/archpedi.153.7.695. [DOI] [PubMed] [Google Scholar]
- 16.Caballero B, Clay T, Davis SM, et al. Pathways Study Research Group. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78(5):1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pate RR, Ward DS, Saunders RP, Felton G, Dishman RK, Dowda M. Promotion of physical activity among high-school girls: a randomized controlled trial. Am J Public Health. 2005;95(9):1582–87. doi: 10.2105/AJPH.2004.045807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haerens L, Deforche B, Maes L, Cardon G, Stevens V, De Bourdeaudhuij I. Evaluation of a 2-year physical activity and healthy eating intervention in middle school children. Health Educ Res. 2006;21(6):911–21. doi: 10.1093/her/cyl115. [DOI] [PubMed] [Google Scholar]
- 19.Haerens L, Deforche B, Maes L, Stevens V, Cardon G, De Bourdeaudhuij I. Body mass effects of a physical activity and healthy food intervention in middle schools. Obesity. 2006;14(5):847–54. doi: 10.1038/oby.2006.98. [DOI] [PubMed] [Google Scholar]
- 20.Stevens J, Murray DM, Catellier DJ, et al. Design of the Trial of Activity in Adolescent Girls (TAAG) Contemp Clin Trials. 2005;26(2):223–33. doi: 10.1016/j.cct.2004.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Center for Chronic Disease Prevention and Health Promotion, CDC. Guidelines for school and community programs to promote lifelong physical activity among young people. J Sch Health. 1997;67:202–19. doi: 10.1111/j.1746-1561.1997.tb06307.x. [DOI] [PubMed] [Google Scholar]
- 22.Murray DM, Catellier DJ, Hannan PJ, et al. School-level intraclass correlation for physical activity in adolescent girls. Med Sci Sports Exerc. 2004;36(5):876–82. doi: 10.1249/01.mss.0000126806.72453.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Young DR, Felton GM, Grieser M, et al. Policies and opportunities for physical activity in middle school environments. J Sch Health. 2007;77:41–7. doi: 10.1111/j.1746-1561.2007.00161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elder JP, Shuler L, Moe SC, et al. Recruiting a diverse group of middle school girls into the Trial of Activity for Adolescent Girls (TAAG) J Sch Health. 2007 doi: 10.1111/j.1746-1561.2008.00339.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elder JP, Lytle L, Sallis JF, et al. A description of the social-ecological framework used in the Trial of Activity for Adolescent Girls (TAAG) Health Educ Res. 2007;22:155–65. doi: 10.1093/her/cyl059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Skinner BF. Science and human behavior. New York: Macmillan; 1953. [Google Scholar]
- 27.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986. [Google Scholar]
- 28.Goodman RM, Steckler A, Kegler MC. Mobilizing organizations for health enhancement: Theories of organizational change. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: theory, research, and practice. 2. San Francisco: Jossey-Bass; 1997. [Google Scholar]
- 29.Rogers EM, Rogers E. Diffusion of Innovations. 5. New York: The Free Press; 2003. [Google Scholar]
- 30.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 31.Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. Am Psychol. 1992;47(1):6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 32.Richard L, Potvin L, Kishchuk N, Prlic H, Green LW. Assessment of the Integration of the Ecological Approach in Health Promotion Programs. Am J Health Promot. 1996;10:318–28. doi: 10.4278/0890-1171-10.4.318. [DOI] [PubMed] [Google Scholar]
- 33.Sallis JF. Age-related decline in physical activity: a synthesis of human and animal studies. Med Sci Sports Exerc. 2000;32:1598–1600. doi: 10.1097/00005768-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Sallis JF, Owen N. Ecological models of health behavior. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: theory, research, and practice. 3. San Francisco: Jossey-Bass; 2002. pp. 462–84. [Google Scholar]
- 35.Saunders RP, Moody J. Community agency survey formative research results from the TAAG study. Health Educ Behav. 2006;33:12–24. doi: 10.1177/1090198105282410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grieser M, Vu MB, Bedimo-Rung AL, et al. Physical activity attitudes, preferences, and practices in African American, Hispanic, and Caucasian girls. Health Educ Behav. 2006;33:40–51. doi: 10.1177/1090198105282416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moe SG, Pickrel J, McKenzie TL, Strikmiller PK, Coombs D, Murrie D. Using school-level interviews to develop a multi-site PE intervention program. Health Educ Behav. 2006;33:52–65. doi: 10.1177/1090198105282418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Staten LK, Birnbaum AS, Jobe JB, Elder JP. A typology of middle school girls: audience segmentation related to physical activity. Health Educ Behav. 2006;33:66–80. doi: 10.1177/1090198105282419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vu MB, Murrie D, Gonzalez V, Jobe JB. Listening to girls and boys talk about girls’ physical activity behaviors. Health Educ Behav. 2006;33:81–96. doi: 10.1177/1090198105282443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Young DR, Johnson CC, Gittelsohn J, et al. Data to action: using formative research to develop intervention programs to increase physical activity in adolescent girls. Health Educ Behav. 2006;33:97–111. doi: 10.1177/1090198105282444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kotler P, Zaltman G. Social marketing: an approach to planned social change. J Mark. 1971;35(3):3–12. [PubMed] [Google Scholar]
- 42.Smith DW, Steckler A, McCormick LK, McLeroy KR. Disseminating comprehensive school health curricula: lesson learned from the North Carolina School Health and Tobacco Education Project. J Health Educ. 1995;26(1):26–36. [Google Scholar]
- 43.Parcel GS, O’Hara-Tompkins NM, Harrist RB, et al. Diffusion of an effective tobacco prevention program, Part II: evaluation of the adoption phase. Health Educ Res. 1995;10(3):297–307. doi: 10.1093/her/10.3.297. [DOI] [PubMed] [Google Scholar]
- 44.Osganian SK, Parcel GS, Stone EJ. Institutionalization of a school health promotion program: background and rationale of the CATCH-ON study. Health Educ Behav. 2003;30:410–17. doi: 10.1177/1090198103252766. [DOI] [PubMed] [Google Scholar]
- 45.Treuth MS, Schmitz K, Catellier DJ, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc. 2004;36:1259–66. [PMC free article] [PubMed] [Google Scholar]
- 46.Catellier DJ, Hannan PJ, Murray DM, et al. Imputation of missing data when measuring physical activity by accelerometry. Med Sci Sports Exerc. 2005;37:S555–S562. doi: 10.1249/01.mss.0000185651.59486.4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dempster AP, Laird NM, Rubin DB. Maximum likelihood from incomplete data via the EM algorithm. J R Stat Soc Ser B. 1977;39:1–38. [Google Scholar]
- 48.Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign IL: Human Kinetics; 1988. [Google Scholar]
- 49.Loftin M, Nichols J, Going S, et al. Comparison of the validity of anthropometric and bioelectrical impedance equations to assess body composition in adolescent girls. Int J Body Compos. 2007;5:1–8. [PMC free article] [PubMed] [Google Scholar]
- 50.McKenzie TL, Sallis JF, Nader PR. SOFIT system for observing fitness instruction time. J Teach Phys Educ. 1991;11:195–205. [Google Scholar]
- 51.Murray DM. Design and analysis of group-randomized trials. New York NY: Oxford University Press; 1998. [Google Scholar]
- 52.Gregoire TG, Driver BL. Analysis of ordinal data to detect population differences. Psychol Bull. 1987;101(1):159–65. [Google Scholar]
- 53.Perry CL. Preadolescent and adolescent influences on health. In: Smedley BD, Syme SL, editors. Promoting health: intervention strategies from social and behavioral research. Washington DC: Institute of Medicine, National Academies Press; 2001. pp. 217–53. [PubMed] [Google Scholar]
- 54.Schmitz KH, Treuth M, Hannan P, et al. Predicting energy expenditure from accelerometry counts in adolescent girls. Med Sci Sports Exerc. 2005;37(1):155–61. doi: 10.1249/01.MSS.0000150084.97823.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among U.S. children: a counterfactual approach. Pediatrics. 2006;118(6):e1721–33. doi: 10.1542/peds.2006-0682. [DOI] [PubMed] [Google Scholar]
- 56.Thompson DR, Obarzanek E, Franko DL, et al. Childhood overweight and cardiovascular disease risk factors: The National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 2007;150(1):18–25. doi: 10.1016/j.jpeds.2006.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Young DR, Phillips JA, Yu T, Haythornthwaite JA. Effects of a life skills intervention for increasing physical activity in adolescent girls. Arch Pediatr Adolesc Med. 2006;160(12):1255–61. doi: 10.1001/archpedi.160.12.1255. [DOI] [PubMed] [Google Scholar]


