Abstract
Few child asthma studies address the specific content and techniques needed to enhance child communication during asthma preventive care visits. This study examined the content of child and parent communications regarding their asthma management during a medical encounter with their primary care provider (PCP). The majority of parents and children required prompting to communicate symptom information to the PCP during the clinic visit. Some high-risk families may require an asthma advocate to ensure that the clinician receives an accurate report of child’s asthma severity and asthma control to ensure prescribing of optimal asthma therapy.
Keywords: childhood asthma, communication educational intervention, prompting
INTRODUCTION
Asthma is one of the most common chronic childhood illnesses and affects nearly 9 million U.S. children (1). Long-term asthma control is best achieved by receiving regular preventive medical care to monitor symptoms and medication use (2, 3). National asthma guidelines recommend that patients with asthma be evaluated by their primary care provider (PCP) at least once every 6 months not only to monitor symptom frequency but also to adjust therapy when indicated (4, 5). However, many children with asthma fail to receive regular medical evaluation to prevent acute asthma episodes (6, 7).
Effective preventive asthma care requires the parent or child to accurately relay the child’s symptom frequency, pattern of rescue and controller medication use, and level of asthma control to the PCP (8–10). In the past, parents have been the main communicator with the PCP and the child has been almost entirely ignored during medical visits resulting in the medical interaction dominated by the physician and parent (11). When children are encouraged to communicate, the amount and type of information conveyed to the clinician is usually limited. In children seeking emergency care for asthma the type of communication with the physician was primarily biomedical and limited in amount of communication, i.e., children spoke in only 12% of the statements to the provider with a mean of 20 statements per child as compared with 156 statements by the parents (12). The low degree of child interaction may be due to how the child is socialized to participate in the triadic interaction (provider-parent-child) (13). Encouraging the child to interact during the medical visit includes use of techniques such as creating a developmentally appropriate environment for the child to participate in the visit by emphasizing health promotion, self-confidence, and appropriate self-management skills (13). Despite these recommendations, few child asthma studies address the specific content and techniques needed to enhance child communication during asthma preventive care visits.
The purpose of this manuscript is to describe the content and implementation of an asthma educational intervention aimed at improving communication skills in school-age children with asthma and their parents enrolled in a randomized clinical trial and who were assigned to the asthma communication intervention group. Communication skills were taught to the children and parents to help convey asthma symptoms, activity limitation, medication use problems, and personal goal setting for asthma management during a non-urgent clinic visit with their primary care provider (PCP).
Methods
This is a cross-sectional analysis of a subgroup of children enrolled in the intervention arm of an ongoing randomized clinical trial of an asthma communication educational intervention. The educational intervention aimed to increase the frequency of child and/or parent communication with their PCP about the child’s symptoms, activity limitation, medication use, and personal goal for asthma management during non-urgent care clinic visits. The educational intervention was delivered by community nurse/health educators to school-age children with persistent asthma and their parents during four home visits and two clinic visits as described below. Baseline sociodemographic and health self-reported data were collected via face-to face or telephone parent interviews. Content of the communication between the parent-child-health care provider was obtained from data recorded by the nurse/health educator during the clinic visits as part of the intervention implementation protocol. Baseline survey and clinic observation data are presented in this manuscript.
Participants
Child participants and their parents were recruited from community pediatric practices and pediatric emergency departments (ED) of two urban university hospitals in Baltimore, Maryland, from December 2004 through December 2006. All children were enrolled in a randomized clinical trial to evaluate the effectiveness of an asthma communication educational intervention and randomized into the intervention group. Inclusion criteria included children 6 to 12 years of age with persistent asthma, current use of asthma medications, or having 1 or more ED visit or hospitalizations during the prior 12 months. Children assigned to the control group received standard asthma education without communication skills training during three home visits by a different nurse/health educator as an attention control intervention. Control group children were not accompanied during PCP clinic visits, therefore no data regarding child-parent-PCP communication were recorded for this group. The study protocol was approved by the Institutional Review Boards of the Johns Hopkins University Medical Institutions and the University of Maryland, School of Medicine. Informed consent was obtained from all participating parents and child assent from children 7 years of age or older.
Description of the Asthma Communication Educational Intervention
The child educational intervention was delivered by three nurse/health educators during four home visits (average length 30 minutes) and two clinic visits (average length 57 minutes). Nurse/health educators were supervised on a weekly basis by an asthma nurse specialist and protocol forms were reviewed for each patient on a monthly basis.
The educational materials consisted of a child communication booklet written at a third-grade level with pictures, in which the child recorded his or her medications, asthma medications that were disliked and why, the child’s personal goal with a Polaroid picture of the study child demonstrating the goal (playing football, riding a bike, rollerblading, etc.), a diary of day and night asthma symptoms, and level of activity limitation for that day. The level of activity was measured on a Likert scale ranging from 1 to 5 with 1 indicating “low activity” and represented by a child sitting to 5 indicating “high activity” represented by a child jumping on a skateboard. Child figures used in the Likert scale of activity were stick figures with no cultural or gender bias. The communication booklet was used by the child as a cue card to talk with the PCP and convey symptom severity, problems with medications, and the child’s personal goal for treating their asthma so that the child and the PCP could mutually agree on an asthma management plan for the child. The communication booklet was pilot tested for readability and feasibility of use in a comparable clinic population as in the randomized clinical trial and minor changes were made to the booklet. Although other validated child asthma control instruments, such as the Child Asthma Control Test, were considered in the development of the communication booklet, these instruments do not assess medication use problems, i.e., forgetting doses, dislike of taste, inability to obtain prescription, or fear of side effects or assist the family and PCP to set the child’s personal goal for asthma care.
Despite reminding the families to bring the asthma communication booklet to each clinic visits, the intervention nurse/health educators maintained a copy of the booklet in case the child and family failed to bring the booklet to the clinic visit. Using the booklet, the child was taught communication skills via modeling, role-play, and feedback techniques. Specific skills included turn taking, eliciting attention, or requesting help and clarifying communication with the doctor. Turn taking was to be practiced in the home by having the child ask to have a turn talking with their parent at home between the educational home visits. Role playing practice was conducted with the nurse/health educator during home visits and endorsed that the child will be allowed and encouraged to talk with the provider. An example of eliciting attention or requesting help was modeled by teaching the child to ask the provider: “Dr. Jones, I don’t like the taste in my mouth after using my inhaler (i.e., inhaled corticosteroid). Can you help me get rid of this?” To clarify communication, the nurse would ask the child to rephrase his or her understanding of the treatment instructions at the end of the clinic visit and in the home. Parents were reminded at each home visit to practice turn taking with their child. However, parental adherence to home practice sessions were not recorded. Child communication skills were reinforced by the nurse/health educator during each of the four home visits. Adherence to practice sessions with the nurse/health educator was recorded on the home visit protocol checklist.
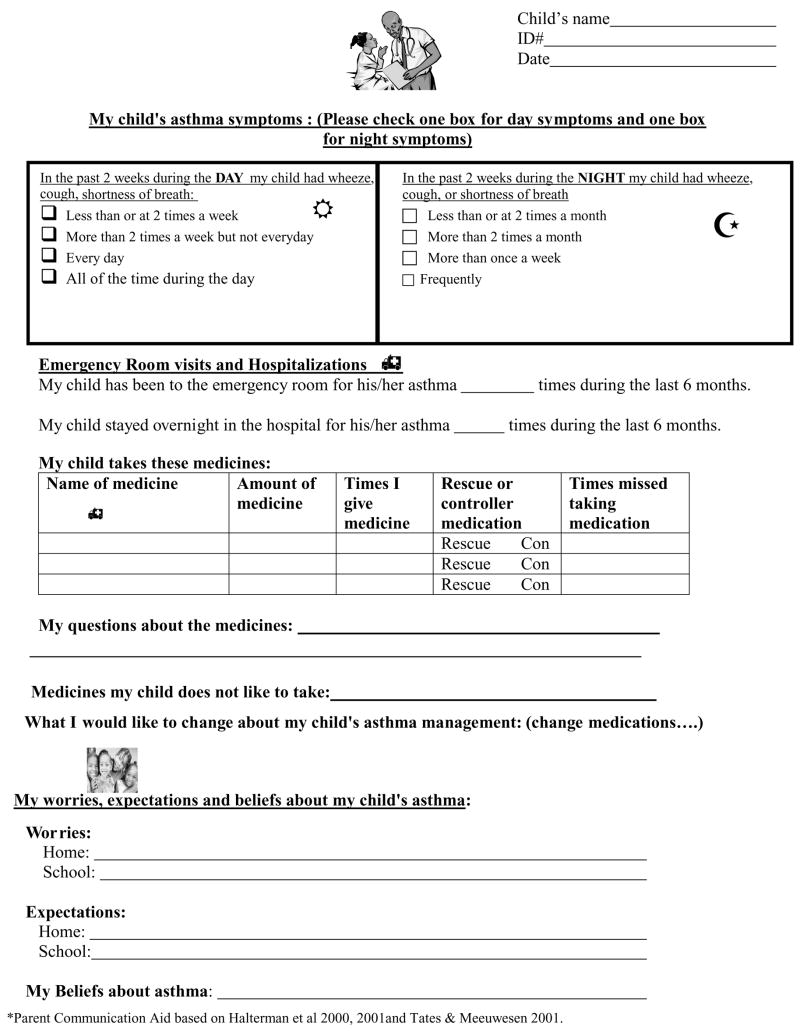
During the initial home visit, the nurse/health educator completes the “Notes to My Child’s Doctor” form (Figure 1) with parent assistance for use during the child’s asthma clinic visit. The “Notes to My Child’s Doctor” form lists the parent report of day and night time symptom frequency, current asthma medications used by the child, and parent worries, concerns, or myths about asthma that the parent wanted to share with the child’s PCP. The content on the form was based on review of several asthma action plans and interviews with parents regarding information they would like to convey to their child’s health care provider. The instrument, written at an 8th-grade level, was piloted tested in comparable low-income, low-literacy population as enrolled in the randomized clinical trial. This form served as a parent “cue” card during the clinic visit to (1) remind the parent of important information to relay to the PCP and (2) provide the PCP with symptom frequency to assign asthma severity and to review asthma medications in the home. The parent was instructed to talk with the child’s PCP as usual but to make sure that points on the form were addressed with the PCP.
Figure 1.
Notes to my child’s doctor.
An intervention nurse/health educator accompanied the family to the child’s clinic visit. The nurse/health educator was trained to prompt the child or parent to talk with the PCP if the asthma items included on the booklet or “Notes to My Child’s Doctor” in the intervention were not discussed. Every attempt was made for the child to attend a clinic visit with their regular PCP; however, due to scheduling issues some clinic visits occurred with another PCP in the same practice. If the clinic visit occurred with a different PCP, this was noted on the protocol clinic visit observation form. Between the two clinic visits the nurse/health educator would reinforce the communication skills of turn taking, eliciting help, and clarifying communication and review the child communication booklet with the child to plan how the child would communicate any neglected information for the second clinic visit. A similar procedure was conducted with the parent using the parent cue card.
Measures
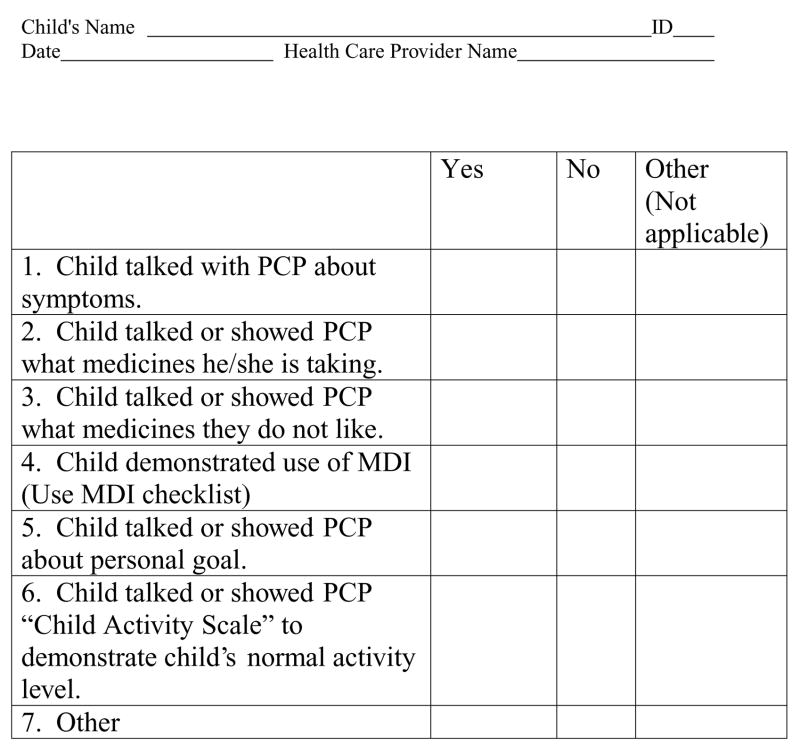
Child Clinic Communication Checklist
Intervention children were accompanied to all clinic visits by an intervention nurse/health educator who recorded communication behaviors on the Clinic Communication checklist (Figure 2) during the clinic visit and serves as the source of the communication content data presented in this manuscript. The checklist included the following items: child talked with PCP about (1) symptoms by showing diary sheets, (2) what medicines he or she is taking, (3) what medicines he or she does not like, (4) child demonstrated use of metered dose inhaler (MDI) with notation of accuracy of technique, (5) child listed personal goal for asthma treatment, and (6) child showed the PCP his or her normal activity level. When the child’s MDI technique was inaccurate the nurse was instructed to remind the child of the proper technique if not corrected by the PCP.
Figure 2.
Checklist for child asthma communication during clinic visit.
Data Analysis
Frequency of the content of communication during asthma clinic visits including if the child talked or showed the PCP symptoms, level of activity limitation, medications used, if child demonstrated metered dose inhaler (MDI) technique, discussion of personal goal for asthma, and number to times the child and/or parent required prompting during the clinic visit was examined. Mean length of clinic visits was calculated. Anecdotal comments recorded during each clinic visit were reviewed. All data analyses were performed using SPSS version 14.0 software (14).
Results
Sociodemographic and Health Characteristics
Of the 121 children assigned to intervention group, data are available for a subgroup of 89 children who were randomized into the intervention group and have completed the study to date. As seen in Table 1, at baseline, most children were male (61%), African American (93%), Medicaid insured (84%) and lived with a parent who was employed (51%), achieved a high school or higher educational level (64%), and earned less than $ 40,000 household income (65%). Almost one third (30%) of children resided in households with one or more smokers. Of note, almost one of six (17%) parents reported having their electricity discontinued during the past 6 months and 30% reported living in an unsafe neighborhood.
Table 1.
Sociodemographic and health characteristics of child sample at baseline based on parental self-report (N = 121).
| Sociodemographic characteristics | Number (%) |
|---|---|
| Gender | |
| Male | 74 (61.2) |
| Race/ethnicity | |
| African American | 113 (93.4) |
| White | 3 (2.5) |
| Other | 5 (4.1) |
| Number of household members | |
| 2–4 | 53 (43.8) |
| 5–7 | 59 (48.8) |
| 8 or more | 9 (7.4) |
| Health insurance | |
| Medicaid | 102 (84.3) |
| Private or self-pay | 16 (13.2) |
| Self-pay or don’t know/missing | 3 (2.5) |
| Paternal/legal guardian educational level | |
| < High school | 44 (36.4) |
| High school grad or GED | 45 (37.2) |
| Some college or higher | 32 (26.4) |
| Parent employed | |
| Yes | 62 (51.2) |
| Household income | |
| < $ 20,000 | 53 (43.8) |
| $ 20,000–39,999 | 25 (20.7) |
| ≥ $ 40,000 | 10 (8.3) |
| Refused or missing | 33 (27.2) |
| Number of smokers in household | |
| No smokers | 67 (70.5) |
| 1 smoker | 13 (13.7) |
| 2 or more smokers | 15 (15.8) |
| Housing/neighborhood conditions | |
| Electricity cut off | 21 (17.4) |
| Lost housing | 7 (5.8) |
| Moved within last 6 months | 23 (19.0) |
| Unsafe neighborhood per parent report | 37 (30.6) |
| Health characteristics | |
| Daytime symptoms last 30 days | |
| None | 18 (14.9) |
| 1–4 days | 62 (51.2) |
| 5–10 days | 20 (16.5) |
| 11–29 days | 10 (8.3) |
| 30 days (daily symptoms) | 11 (9.1) |
| Night time symptoms last 30 nights | |
| None | 30 (24.8) |
| 1–4 nights | 57 (47.1) |
| 5–10 nights | 19 (15.7) |
| 11–29 nights | 9 (7.4) |
| 30 nights (nightly symptoms) | 6 (5.0) |
| Asthma limit activity of child | |
| Yes | 76 (62.8) |
| Asthma out of control | |
| All/a lot/some of the time | 36 (29.8) |
| A little/none of the time | 85 (70.3) |
| Specialty care within past 2 years | |
| Yes | 29 (23.9) |
| Number of ED visits last 6 months | |
| 0 | 14 (11.6) |
| 1–2 | 73 (60.3) |
| 3 or more | 34 (28.1) |
| Number of visits to PCP last 6 months | |
| 0 visits | 21 (17.4) |
| 1–2 visits | 74 (61.2) |
| 3 or more visits | 26 (21.4) |
| Rescue medication use frequency | |
| All/a lot/some of the time | 77 (63.6) |
| A little/none of the time | 44 (36.4) |
| Controller medication use | |
| Yes | 84 (69.4) |
| Oral steroid courses last 6 months (N = 118) | |
| None | 21 (17.8) |
| 1–2 | 73 (61.9) |
| 3 or more | 24 (20.3) |
| Primary care practitioner characteristics | |
| Length of time PCP has treated child (N = 120) | |
| <1 year | 19 (15.8) |
| 1–2 years | 18 (15.0) |
| 3–5 years | 21 (17.5) |
| 5 or more years | 62 (51.7) |
| Easy to travel to PCP | |
| Never/sometimes | 31 (25.6) |
| Often/almost always/always | 88 (72.7) |
| Missing | 2 (1.7) |
| PCP knows your concerns about your child | |
| Never/sometimes | 21 (17.4) |
| Often/almost always/always | 99 (81.8) |
| Missing | 1 (0.8) |
| My PCP gave my family information to relieve specific worries | |
| Disagree/strongly disagree/no opinion | 27 (22.3) |
| Agree/strongly agree | 93 (76.9) |
| Missing | 1 (0.8) |
| Parent confident they can give preventive medications | |
| Disagree/strongly disagree/no opinion | 59 (48.8) |
| Agree/strongly agree | 61 (50.4) |
| Missing | 1 (0.8) |
Asthma morbidity was high in this child sample. Most children reported one to four symptom days during the last 30 days (51%), yet 17% reported symptom days for more than one third of the days during the past month. Night symptoms were slightly less frequent with most parents (47%) reporting their child had night symptoms at four or less nights during the last 30 days. Almost two thirds of children (63%) reported some activity restriction due to asthma. However, this was discordant with the fact that only 30% of parents reported their child’s asthma as out of control from some to all of the time. Emergency department (ED) use was high in this sample; 88% reported an ED visit within the past 6 months. However, few children (24%) received specialty care within the past 2 years. At baseline, most children (83%) had seen their PCP within the past 6 months.
Rescue medication, short-acting beta-agonist medications, were used at some to all of the time by almost two thirds of children (64%) during the past 6 months. Controller medication use was reported by 69% of children. Most children (82%) reported one or more courses of oral corticosteroids during the last 6 months.
Characteristics of the Primary Care Practitioner (PCP) Relationship
Most children reported a long relationship (5 or more years) with their PCP and reported no problems with traveling to their PCP (73%). Most children (83%) were evaluated by their regular PCP during either of the observed clinic visits. The remainder of children (17%) were seen by a physician covering the community practice or hospital resident clinic. Parents reported that they believed the child’s PCP knew their concerns about their child’s asthma at a level of often/almost always or always (82%) and most (77%) reported their child’s PCP provided the family with information to relieve specific worries about their asthma.
Characteristics of the Intervention Clinic Visits
Overall 60% of children completed at least one intervention clinic visit and 27% completed two clinic visits over the 6-month study period with the nurse/health educator accompanying the family to the PCP visits. As seen in Table 2, during the first clinic visit, most children talked with the PCP about their symptoms (83%), talked about or showed the specific asthma medications they were taking (79%), talked about their personal goal for asthma treatment (72%), and showed their normal activity level using the specific activity scale (66%). Fewer children demonstrated use of their MDI (47%) or talked about asthma medicines they disliked (40%). These rates of communicating specific information did not change during the second clinic visit (Table 3). Prompting was required by most parents at both visits (first visit: 87%, second visit: 79%). Child prompting was also high at clinic visits (first visit: 80%, second visit: 96%). Average length of clinic visits were high at mean of 63.47 minutes for first visits and 49.34 minutes for second visits.
Table 2.
Characteristics of child communication for clinic visit 1* (N = 53).
| Characteristic | Yes |
|---|---|
| 1. Child talked with PCP about symptoms. | 44 (83%) |
| 2. Child talked with/showed PCP medicines he/she is taking. | 42 (79%) |
| 3. Child talked with/showed PCP what medicines they do not like. | 21 (40%) |
| 4. Child demonstrated use of MDI. | 25 (47%) |
| 5. Child talked with/showed PCP personal goal. | 38 (72%) |
| 6. Child talked with/showed PCP “Child Activity Scale.” | 35 (66%) |
Without prompting.
Table 3.
Characteristics of child communication for clinic visit 2.* (N = 24).
| Characteristics | Yes |
|---|---|
| 1. Child talked with PCP about symptoms. | 21 (88%) |
| 2. Child talked with/showed PCP medicines he/she is taking. | 19 (79%) |
| 3. Child talked with/showed PCP medicines they do not like. | 9 (37%) |
| 4. Child demonstrated use of MDI. | 11 (46%) |
| 5. Child talked with/showed PCP personal goal. | 16 (67%) |
| 6. Child talked with/showed PCP “Child Activity Scale.” | 15 (63%) |
Without prompting.
Anecdotal Comments from Clinic Visits
Anecdotally, the nurses often reported the child and or the parent failed to bring the communication cue materials to the clinic visits so the nurse was required to use her copy of the communication booklet for the family to use. Additionally, parents did not bring the child’s medicines or peak flow meter to the visit for the provider to observe device use technique. Often the provider did not ask to review inhaler technique and asked the intervention nurse to review technique in the home. Finally, many common nonasthma diagnoses required attention during the clinic visits including obesity, eczema, behavior problems, injury prevention, dental problems, and school issues.
Discussion
Our data indicate that children and parents can be educated to communicate effectively with the child’s PCP and provide him or her with important health information including symptom frequency, activity limitation, current asthma medication use, and concerns about medication use using an intensive home-based educational intervention. Communicating symptom frequency and limitation of activity is congruent with the updated NAEPP guidelines (5) that base asthma severity and control on impairment such as limitation of activity and risk for adverse events such as increased symptoms (5) and guide appropriate therapy. Although the majority of parents and children required prompting by the nurse to communicate symptom information to the PCP during the clinic visit, three of four parents discussed asthma medications with the PCP. Prompting by the nurse for children to talk with the PCP increased from the initial to second clinic visit suggesting children may require repeated practice and encouragement to talk with health care providers. In a recent study, prompting physicians about asthma severity and asthma care guidelines at the time of the child’s office visit by research staff yielded increased discussion of asthma prevention, increased use of asthma action plans, and cigarette smoke reduction counseling yet made no difference in the rate of initiating or stepping up a preventive asthma medication (15, 16). This suggests that physician prompting may be insufficient for a change in preventive asthma medications and that the family may need to advocate the change in medication. Having a child advocate, i.e., a nurse or health educator, present during the clinic visit to advocate a change in preventive asthma medication when indicated and specify the rationale for the change may be the level of intervention required for high-risk children to receive appropriate preventive asthma care. Roter (17) suggests that certain physician communication behaviors can enhance patient participation in the medical visits and contribute to patient engagement in decision making. Yet, in a study of adult patients including minority subjects, physicians provided more patient-centered care to patients they perceived as better communicators (18) supporting the need to improve patient communication skills for medical visits, particularly in low-income, low-literacy populations as targeted in this study.
Interestingly, the length of the clinic visits in our study was very high (mean 63.47, SD 23.6 minutes, range 25–140 minutes) in contrast to the mean of 17.7 to 18.3 minutes reported for well child care visits (19) and 12.2 minutes noted in pediatric acute care visits (20). One explanation for the increased length of clinic visits was the presence of a health professional observing the PCP who may have taken more time teaching the family, which is more time-consuming than that performed during a routine 15- to 20-minute non-urgent asthma clinic visit. However, a 20-minute clinic visit represents the minimum amount of time to teach basic asthma management and observe device technique as recommended by national asthma guidelines (5). Shorter clinic visits in adults were associated with less patient and physician participation (21); however, in children, longer visits were associated with more child, physician, and parent participation (20). Our data support the Institute of Medicine’s (IOM) concern that shorter visits may be a barrier to effective partnership communication (22) in that in three of four parents in our study discussed asthma medications with their child’s PCP but only after prompting by the intervention nurse.
Our data support that school-age children can participate in self-management decisions and education if supported by parent or advocate. Increasingly research is indicating that school-age children with asthma are dependable, valuable, and accurate reporters of their asthma symptoms and health status (10,23,24) and are also being acknowledged as active participants in decisions about their own health care (11,13). Facilitating child communication with their PCP requires teaching the child effective communication skills. Bandura’s Social Learning Theory (25, 26) highlights the importance of modeling behavior and providing reinforcers for effective communication. Any underachievement in basic skills, i.e., inability to identify colors, may interfere with communicating types of inhaler medications. Modeling of communication behaviors by role- playing is a positive force in shaping the performance of school-age children. Use of cue cards, as reported in this study, is one method to enhance child communication (27, 28).
Of note is the high nonadherence to (1) parent transporting the communication booklet to the physician visits and (2) attendance of the second clinic visit. Failure of parents to bring the communication booklet and “Notes to My Doctor Form” to the visits may indicate lack of cultural relevance of the booklet to this population or lack of importance to the family. Alternatively, overestimation of family organization skills may have contributed to the communication cue cards not being transported to the clinic visit. Many reasons may have contributed to the low attendance of the second clinic visit and include parental lack of appreciation of the need for asthma care if the child is no longer sick, cost of transportation to the clinic, and lack of endorsement of the need for follow-up by community PCPs (29, 30). Common system and organizational barriers to preventive care appointments reported by urban families of children with asthma included lack of available appointments, long wait times to schedule with PCP and inconvenient hours (31). Unfortunately, barriers to the PCP visits were primarily unknown in this sample. Anecdotal reports revealed that some parents requested appointments with PCPs, yet some PCPs were instructing parents that their child did not need to be evaluated for asthma since the child was asymptomatic. This is incongruent with the updated NAEPP guidelines that recommend regular monitoring of asthma control at 1- to 6-month intervals for appropriate adjustments in therapy (5). Other critical barriers included family crises due to parent illness, loss of housing. We noted that 30% of families lived in an unsafe neighborhood and 65% earned less than $40,000.
Generalizability of the study results is limited owing to several factors. First, the health characteristics and medication use of the sample are based on parental recall and may result in the under- or overestimation of the child’s symptom frequency and health care utilization. Poor parental adherence with transporting the communication booklet to the clinic visits indicates the problem of relying on low-income, low-literacy families to bring home health records to medical visits. Alternative methods of conveying health information to the physician, i.e., electronic information, will need to be tested in future interventions. In addition, the cross- sectional design and increased length of clinic visits both limit the generalizability beyond this sample of high-risk children. The increased length in clinic visit time is most likely due to the bias introduced during the clinic visits by the physicians who felt obligated to spend more time with patients secondary to being observed. Nevertheless, we believe that the descriptive data from this study provide some insight into the difficulty in treating inner-city children with asthma.
Despite these limitations, there are several important clinical implications. School-age children should be participating in providing asthma health information to their PCP and participating in self-management decisions when age appropriate. Of note, children’s ability and accuracy at reporting symptoms decreases as their asthma severity increases (10, 23). Children with more severe asthma may require an advocate to accompany them to clinic visits to ensure that the clinician receives an accurate report of the child’s asthma severity and control for prescribing optimal asthma therapy.
In conclusion, children and parents can be educated to communicate effectively with the child’s PCP and provide important health information about symptom frequency, current asthma medication use, and personal goals for asthma management. Although the majority of parents and children required prompting by the nurse to communicate symptom information to the PCP during the clinic visit, most parents discussed asthma medications with the PCP one critical component of asthma management.
References
- 1.Bloom B, Dey AN. Summary health statistics for U. S. children: National Health Interview Survey, 2004. National Center for health Statistics Vital Health Stat. 2006;10:4–5. [PubMed] [Google Scholar]
- 2.Baren JM, Boudreaux ED, Brenner BE, Cydulka RK, Rowe BH, Clark S, Camargo CA. Randomized controlled trial of emergency department interventions to improve primary care follow-up for patients with acute asthma. Chest. 2006;129:257–265. doi: 10.1378/chest.129.2.257. [DOI] [PubMed] [Google Scholar]
- 3.Weinberg M. What prevents hospitalization and relapse from asthma? Ann Allergy Asthma Immunol. 1998;81:187–189. doi: 10.1016/S1081-1206(10)62811-6. [DOI] [PubMed] [Google Scholar]
- 4.United States Department of Health and Human Services (USDHHS) Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. National Asthma Education and Prevention Program. National Institutes of Health Publication 97-4051,1997. [Google Scholar]
- 5.National Heart, Lung, and Blood Institute. National Asthma Education and prevention Program (NAEPP) Full Report of the Expert Panel 3: Guidelines for the Diagnosis and Management of Asthma (EPR-3) Aug, 2007. [Google Scholar]
- 6.Butz AM, Tsoukleris M, Donithan M, Hsu V, Mudd K, Zuckerman I, Bollinger ME. Patterns of inhaled anti-inflammatory medication use in young underserved children with asthma. Pediatrics. 2006;118:2504–2513. doi: 10.1542/peds.2006-1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halterman JS, Yoos L, Sidora K, Kitzman H, McMullen A. Medication use and health care contacts among symptomatic children with asthma. Amb Pediatrics. 2001;1:275–279. doi: 10.1367/1539-4409(2001)001<0275:muahcc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 8.Halterman JS, Yoos HL, Kaczorowski JM, McConnochie K, Holzhauer RJ, Conn KM, Lauver S, Szilagyi PG. Providers underestimate symptom severity among urban children with asthma. Arch Pediatric Adoles Med. 2002;156:141–146. doi: 10.1001/archpedi.156.2.141. [DOI] [PubMed] [Google Scholar]
- 9.Yoos HL, McMullen A. Symptom perception and evaluation in childhood Asthma. Nurs Res. 1999;48:2–8. doi: 10.1097/00006199-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Yoos HL, Kitzman H, McMullen A, Sidora K. Symptom perception in childhood asthma: how accurate are children and their parents? J Asthma. 2003;40:27–39. doi: 10.1081/jas-120017204. [DOI] [PubMed] [Google Scholar]
- 11.Tates K, Meeuwesen L. Doctor-parent-child communication: a (re) view of the literature. Soc Sci Med. 2001;52:839–851. doi: 10.1016/s0277-9536(00)00193-3. [DOI] [PubMed] [Google Scholar]
- 12.Wissow LS, Roter D, Bauman LJ. Patient-provider communication during the emergency department care of children with asthma. The National Inner-city Asthma Study. National Institute of Allergy and Infectious Disease, NIH Med Care. 1998;36:1439–1450. doi: 10.1097/00005650-199810000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Tates K, Meeuwesen L. “Let mum have her say”: turntaking in doctor-parent-child communication. Patient Educ Counseling. 2000;40:151–162. doi: 10.1016/s0738-3991(99)00075-0. [DOI] [PubMed] [Google Scholar]
- 14.SPSS Inc. Statistical Package for Social Science Version 14.0.1. Chicago, IL: 2005. [Google Scholar]
- 15.Halterman JS, McConnochie KM, Conn KM, Yoos HL, Callahan PM, Neely TL, Szilagyi PG. A Randomized trial of primary care provider prompting to enhance preventive asthma therapy. Arch Pediatric Adoles Med. 2005;159:422–427. doi: 10.1001/archpedi.159.5.422. [DOI] [PubMed] [Google Scholar]
- 16.Halterman JS, Fisher S, Conn KM, Fagnano M, Lynch K, Marky A, Szilagyi PG. Improved preventive care for asthma: a randomized trial of clinician prompting in pediatric offices. Arch Pediatric Adoles Med. 2006;160:1018–1025. doi: 10.1001/archpedi.160.10.1018. [DOI] [PubMed] [Google Scholar]
- 17.Roter D. The medical visit context of treatment decision-making and the therapeutic relationship. Health Expect. 2000;3:17–25. doi: 10.1046/j.1369-6513.2000.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Street RL, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Social Sci Med. 2007;65:586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olson LM, Inkelas M, Halfon N, Schuster MA, O’Connor KG, Mistry R. Overview of the content of health supervision for young children reports from parents and pediatricians. Pediatrics. 2004;113:1907–1916. [PubMed] [Google Scholar]
- 20.Cox ED, Smith MA, Brown RL, Fitzpatrick MA. Effect of gender and visit length on participation in pediatric visits. Patient Educ Counseling. 2007;65:320–328. doi: 10.1016/j.pec.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians’ participatory decision-making style. Med Care. 1995;33:1176–1187. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: Committee on Health Literacy and Board on Neuroscience and Behavioral Health; 2004. [Google Scholar]
- 23.Olson LM, Radecki L, Frinter MP, Weiss K, Korfmacher J, Siegel RM. At what age can children report dependably on their asthma health status? Pediatrics. 2007;119:e93–e102. doi: 10.1542/peds.2005-3211. [DOI] [PubMed] [Google Scholar]
- 24.Winkelstein ML, Huss K, Butz AM, Eggleston P, Vargas P, Rand CS. Factors associated with medication self-administration in children with asthma. Clin Pediatrics. 2000;39:337–345. doi: 10.1177/000992280003900603. [DOI] [PubMed] [Google Scholar]
- 25.Bandura A, editor. Psychological Modeling. Chicago: Atherton, Aldine; 1971. [Google Scholar]
- 26.Bandura A. Self-efficacy and the Exercise of Control. New York: Freeman Press; 1997. [Google Scholar]
- 27.Bowen CJ, Howie PM. Context and cue cards in young children’s testimony: a comparison of brief narrative elaboration and context reinstatement. J Appl Psychol. 2002;87:1077–1085. doi: 10.1037/0021-9010.87.6.1077. [DOI] [PubMed] [Google Scholar]
- 28.Dorado JS, Saywitz KJ. Interviewing preschoolers from low and middle-SAS communities: a test of the narrative elaboration recall improvement techniques. J Clinic Child Psychol. 2001;30:568–580. doi: 10.1207/S15374424JCCP3004_12. [DOI] [PubMed] [Google Scholar]
- 29.Smith SR, Jaffe DM, Fisher EB, Trinkaus KM, Highstein G, Strunk RC. Improving follow-up for children with asthma after an acute emergency department visit. J Pediatrics. 2004;145:772–777. doi: 10.1016/j.jpeds.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 30.Smith SR, Highstein GR, Jaffe DM, Fisher EB, Strunk RC. Parental impressions of the benefits (Pros) and Barriers (Cons) of follow-up care after an acute emergency department visit for children with asthma. Pediatrics. 2002;110:323–330. doi: 10.1542/peds.110.2.323. [DOI] [PubMed] [Google Scholar]
- 31.Zorc JJ, Scarfone RJ, Li Y. Predictors of primary care follow-up after a pediatric emergency visits for asthma. J Asthma. 2005;42:571–576. doi: 10.1080/02770900500215947. [DOI] [PubMed] [Google Scholar]