Abstract
Study Objectives:
Recent studies have shown that extended shifts worked by hospital staff nurses are associated with significantly higher risk of errors, yet little information is available about the ability to remain alert during the nurses' commutes following the completion of an extended work shift. The purpose of this study is to describe the prevalence of drowsy driving episodes and the relationship between drowsy driving and nurse work hours, alertness on duty, working at night, and sleep duration.
Participants:
Data were collected from 2 national random samples of registered nurses (n = 895).
Measurements and Results:
Full-time hospital staff nurses (n = 895) completed logbooks on a daily basis for 4 weeks providing information concerning work hours, sleep duration, drowsy and sleep episodes at work, and drowsy driving occurrences. Almost 600 of the nurses (596/895) reported at least 1 episode of drowsy driving, and 30 nurses reported experiencing drowsy driving following every shift worked. Shorter sleep durations, working at night, and difficulties remaining awake at work significantly increased the likelihood of drowsy driving episodes.
Conclusions:
Given the large numbers of nurses who reported struggling to stay awake when driving home from work and the frequency with which nurses reported drowsy driving, greater attention should be paid to increasing nurse awareness of the risks and to implementing strategies to prevent drowsy driving episodes to ensure public safety. Without mitigation, fatigued nurses will continue to put the public and themselves at risk.
Citation:
Scott LD; Hwang WT; Rogers AE; Nysse T; Dean GE; Dinges DF. The relationship between nurse work schedules, sleep duration, and drowsy driving. SLEEP 2007;30(12):1801-1807.
Keywords: Nurse work schedules, sleep duration, drowsy driving, motor vehicle crashes, staff nurse work hours
AT LEAST 100,000 AUTOMOBILE CRASHES, 40,000 INJURIES, AND 1550 FATALITIES EACH YEAR ARE ATTRIBUTABLE TO FALLING ASLEEP BEHIND THE WHEEL.1 These fatigue-related crashes tend to be serious, occur at high speeds, and usually involve only a single vehicle.1,2 The driver is usually alone and is less likely than an alert driver to take action to avoid a crash.1,3 Although drowsy driving more than quadruples the risk of a crash or near-crash,4 drowsy driving is quite common. For example, National Highway Traffic Safety Administration data have revealed that 37% of 103 million adults admit to falling asleep while driving at some point in their driving career.5 Sixty percent of the participants in the 2005 Sleep in America poll reported falling asleep while driving on roadways traveling at speeds of 55 mph or higher, and 11 million drivers have reported having a sleep-related motor vehicle crash (MVC) or near MVC.6 In fact, moderate to severe drowsiness accounted for 22% to 24% of all crashes and near-crashes observed in a recent naturalistic study of driver behavior.7
The prevalence of sleep-related MVCs is higher among individuals who are employed, working more than 60 hours per week,8 working irregular hours,9 and working at night,10 as well as those who are sleep deprived.8,11 Thus, it is not surprising that several studies have shown that medical residents have higher than expected rates of MVCs. The likelihood of a fatigue-related MVC is almost 7 times higher during residency than before residency (19.3% vs 4.1%; P < 0.001, odds ratio [OR] = 6.7).12 In addition, the risk of an MVC (OR = 2.3) or near-MVC (OR = 5.9) is significantly higher among residents whose work hours exceed 24 hours, compared with those who work less than 24 hours.13 In fact, for every extended shift worked in a month, the likelihood of an MVC is increased by 9.1%.13
These statistics are not unique to 1 medical specialty or subspecialty. Approximately 17% of emergency medicine and anesthesia residents have reported at least 1 sleep-related crash during their training program.12,14 All of the reported crashes occurred between 08:00 and 09:00 am (driving home following after call) in “moderate” to “no” traffic. Just under half (44%) of the pediatric residents surveyed at a large university medical center reported falling asleep at a stop light during their training program, and 49% reported falling asleep at the wheel (not necessarily at a stop light).15 The majority of emergency medicine (60%) and anesthesiology residents (78%)12,14 also report near-miss crashes associated with sleepiness, with one third of the anesthesiology residents reporting 5 or more near-miss events.14
Laboratory studies have demonstrated that periods of prolonged wakefulness e.g., 19 consecutive hours, can produce cognitive performance deficits comparable to those seen with a blood alcohol concentration of 0.05%.16,17 Being awake for more than 24 consecutive hours impairs reaction times to a level similar to those found with a blood alcohol concentration of 0.1%, which exceeds the legal standard for operating a motor vehicle in most states.16Arendt and colleagues18 have also demonstrated that resident physicians tested after a heavy call condition (34–36 consecutive hours) exhibited as many performance impairments, attention lapses, decreased vigilance, and simulated driving accidents as residents who consumed enough alcohol to produce a 0.05% blood alcohol concentration after working a light call schedule (4–6 consecutive hours). Not only were their reaction times lengthened and driving performance impaired, but lane and speed variability were significantly increased (27% and 71%, respectively). Even more significant, however, was the finding that residents were unable to accurately judge their level of impairment when tested after the heavy call condition. This inability to accurately judge impairment from inadequate sleep has been found in laboratory studies as well.19
Although resident fatigue is serious, resident physicians are not the only health care providers working long hours or driving home after a night shift. More than 56% of the registered nurses (RNs) in United States are employed in hospitals,20 with many hired to work nights or rotating shifts. Scheduled shifts may be 8, 10, or 12 hours and may not follow the traditional pattern of day, evening, or night shift patterns. Unanticipated double shifts (16 hours) and mandatory overtime are of particular concern, since prolonged periods of wakefulness have been associated with decreased cognitive and psychomotor performance.16,17
Information concerning the number of crashes and near-crashes experienced by hospital staff nurses driving home from work is limited. Most studies conducted among hospital staff nurses have focused on their ability to remain awake during traditional or rotating shifts.21–24 However, Novak and Auvil-Novak25 found that 95% of the intensive care nurses who participated in their examination of night shift workers (n = 45) reported automobile-related injuries and near accidents on the commute to and from work. One of the few studies that have examined shift work, sleepiness on duty, and sleep-related MVCs found that night shift nurses were more likely to fall asleep at work than were nurses who worked day, evening, or rotating shifts.24 Although the risk for a sleep-related MVC was present for all the nurse participants, rotating shift nurses were almost 4 times more likely (OR = 3.92) than nurses who worked either day/evening (OR = 2.38) or night (OR = 3.62) shifts to report nodding off while driving to and from work.
Furthermore, between 20% and 41% of the nurse participants reported near-miss automobile crashes.24 Day/evening rotators reported the fewest near misses, whereas the staff rotating through all 3 shifts reported the highest number of near-miss MVCs. Although Gold and colleagues24 found an association between type of shift, alertness, and drowsy driving, the investigators did not examine shift duration or the effect of shift length on driving performance. Therefore, the purpose of this study was to describe (1) the prevalence of drowsy driving episodes, (2) the relationship between nurse work hours and drowsy driving, (3) the relationship between level of alertness on duty and drowsy driving, and (4) the relationship between sleep duration and drowsy driving.
METHODS
The data used for this study were collected from 2 national random samples of RNs: 393 RNs who were randomly selected from the membership roster of the American Nurses Association (ANA) and 502 RNs who were randomly selected from the membership roster of the American Association of Critical Care Nurses (AACN).
Procedure
The study and eligibility criteria were explained in a cover letter and mailed to a random sample of 4320 ANA members, along with a demographic questionnaire. Approximately 9 months later, a similar mailing was sent to 5261 randomly selected members of the AACN. As a result, 1725 ANA members and 2184 AACN members expressed a desire to participate by returning their completed demographic questionnaire in a postage-paid envelope to the Survey Research Institute at Temple University in Philadelphia. Upon evaluation of eligibility, two 14-day logbooks, instructions for completing the logbooks, and postage-paid envelopes were mailed to 891 eligible ANA members and 1148 eligible AACN members (hospital staff nurse working full time and unit based).
Three hundred thirty-nine subjects from the first wave of data collection (ANA sample) returned both logbooks, and 54 completed only 1 of the 2 logbooks, for a return rate of 44.1% for at least 1 diary and a return rate of approximately 40% for both diaries. Likewise, 382 members of the AACN sample returned both logbooks, and 120 completed only 1 of the 2 logbooks, for a return rate of 43.7% for at least 1 diary and a return rate of approximately 33% for both diaries. Consequently, the final dataset comprised information about 11,334 work shifts obtained from 895 full-time hospital staff nurses in direct-care roles (Table 1). Nurses who were employed in specialized roles, such as administrative or advanced practice positions, were not included in this study. This study was approved by the Institutional Review Boards at the University of Pennsylvania and Grand Valley State University. Subjects were paid $140 for their participation.
Table 1.
Clinical Practice Areas of Study Participants
| Practice area | Number (%) |
|---|---|
| Critical care | 592 (66.1) |
| Combined ICU/CCU | 188 (31.8) |
| ICU | 173 (29.2) |
| Surgical ICU | 89 (15.0) |
| CCU | 56 (9.5) |
| Pediatric ICU | 32 (5.4) |
| Medical ICU | 31 (5.3) |
| Neonatal ICU | 5 (0.8) |
| Other | 18 (3.0) |
| Medical-Surgical | 108 (12.1) |
| Surgery | 47 (5.3) |
| Obstetrics/labor – delivery | 40 (4.5) |
| Psychiatric/mental health | 22 (2.4) |
| Pediatrics | 10 (1.1) |
| Other | 71 (7.9) |
| Missing | 5 (0.6) |
ICU refers to intensive care unit; CCU, coronary care unit
Participants
Both the ANA sample of 393 RNs and the AACN sample of 502 RNs consisted of predominantly Caucasian (79% vs 87%) women (92% vs 93%), in their mid-40s (mean age of 44.8). On average, the participants were experienced RNs, having been in practice between 17 and 18 years (17.2 ± 10 vs 18.4 ± 8.5). All of the participants were employed full time, which was defined as at least 36 hours per week, and the majority were employed by medium-sized (100–300 beds) or large (> 300 bed) hospitals.
Instruments
Logbooks were used to collect information about hours worked (both scheduled and actual hours), sleep/wake patterns, drowsiness and sleep episodes at work, errors, and drowsy driving episodes on a daily basis. In particular, the participants completed all work-related questions and questions about difficulties remaining awake while on duty and during their commute home (Items 16–41). On days off, the nurse participants only completed questions regarding sleep/wake patterns, mood, and caffeine intake (Items 1–15). A more detailed description of the logbooks and their reliability is available in Rogers et al.26
Data Analyses
Data from demographic questionnaires and logbooks were summarized using descriptive statistics and frequency tables. Sleep duration was calculated from the nurses' daily reports of when they went to bed and when they got out of bed, as well as when they napped. A work shift was classified as a night shift if the nurse reported working at least 6 hours between the hours of 22:00 and 08:00. All other shifts were categorized as nonnight shifts.
The variables of interest for this analysis include the frequency of drowsy driving, drowsiness on duty, falling asleep on duty, the number of hours worked, and total sleep duration. Drowsiness was defined as a positive response to the logbook question, “Did you have to struggle to stay awake at work today?” Episodes of falling asleep on duty were identified by a positive response to the question, “Did you fall asleep at work today?” A positive response to the question, “Did you have difficulty with drowsiness when you were driving home from work today?” was used to measure the prevalence of drowsy driving. The time when participants reported that their work shift ended was used to estimate the time of day when reported drowsy driving episodes occurred.
A positive response to the question, “Did you have an accident or near-accident when you were driving home from work today” was used to assess the frequency of MVC/near-MVCs. Given that this question did not allow distinction between an occurrence of an MVC versus a near-MVC and that documentation of actual MVC occurrence was not collected, only limited analysis of this variable was performed.
Univariate analyses were conducted to examine the relationship between the probability of drowsy driving with shift duration, drowsiness and sleep episodes at work, and total sleep time using generalized estimating equation (GEE) logistic regression models. The magnitude of the association was estimated by ORs and the associated 95% confidence intervals. The approach of GEEs was used to account for nondependence between multiple shifts worked by the same nurse while still providing valid and robust estimates of OR for nonindependence between repeated measures.27
Multivariate procedures were conducted to examine adjusted relationships between drowsy driving and work hours, night versus non-night shift, level of alertness (reports of drowsiness or sleep episodes) at work, and sleep duration while controlling for demographic variables including age, years experience as an RN, marital status, and dependent care responsibilities. Because the demographic characteristics and results from separate analysis using the ANA and the AACN samples were comparable, the final analysis was completed as an aggregate sample. Significance tests were 2-tailed, with an alpha level established a priori at 0.05.
RESULTS
Of the 895 hospital staff nurses who participated in this study, 596 (66.6%) reported at least 1 episode of drowsy driving, and 30 nurses reported experiencing drowsy driving following every shift they worked during the 4-week data-collection period. On average, nurses reported experiencing an episode of drowsy driving 1 out of every 4 shifts they worked (26.1%). Although the 1-way commute averaged 27.1 ± 16.9 minutes (median = 22.5; range 2–120 minutes), 67 nurses reported commute times of 60 minutes or more.
MVCs and Near-MVCs
Almost 16% (141/895) of the nurses reported experiencing at least 1 MVC/near-MVC during the 4-week data collection period, whereas 57 nurses reported 2 or more MVC/near-MVCs. One nurse reported 13 MVC/near-MVCs. Of the 596 nurses who reported at least 1 episode of drowsy driving, 127 (21%) also reported at least 1 MVC/near-MVC. As a result, 281 episodes of MVCs/near-MVCs were reported during the study period. The majority of the MVC/near-MVCs occurred following shifts that exceeded 12.5 hours in duration (59%) or were completed during the night (55%). In addition, the likelihood of an MVC/near-MVC significantly increased with longer shift durations. The risk for an MVC/near-MVC almost doubled (OR = 1.84; P = 0.03) when driving following shifts that exceeded 12.5 hours in duration (Table 2).
Table 2.
Relationship Between Shift Duration and MVC or Near-MVC
| Hours worked | Shifts with MVC or near/MVC |
OR (95% CI) | P Value | |
|---|---|---|---|---|
| No | % | |||
| ≤ 8.5 | 20 | 15.7 | 1.00 | |
| > 8.5 - < 12.5 | 96 | 22.3 | 1.40 (0.84–2.33) | 0.20 |
| ≥ 12.5 | 166 | 31.3 | 1.84 (1.06–3.20) | 0.03 |
MVC refers to motor vehicle crash; OR, odds ratio; CI, confidence interval.
Drowsy Driving and Shift Duration
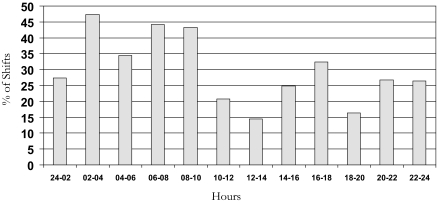
On average, the respondents worked 11.92 + 2.28 hours each shift. However, nurse work hours exceeded 12.5 hours for 53.9% (6111/11,334) of the shifts worked. Nurses reported experiencing drowsy driving even when working shorter shifts, e.g. 8.5 hours or shorter (Table 3). Nevertheless, the risk for a drowsy driving episode doubled when nurses worked 12.5 or more consecutive hours (OR = 2.00; P <0.0001). Working at night also significantly increased the risk for a drowsy driving incident (OR = 3.96; 95% confidence interval = 3.24–4.84). In fact, 136 of the 171 nurses who worked only night shifts (79.5%) reported at least 1 episode of drowsy driving. It is also important to note that 308 nurses who worked exclusively nonnight shifts (58.0%) struggled to stay awake at least once during their commutes from work. Consequently, drowsy driving episodes occurred following 30% of the shifts worked between 06:00 and 24:00. The proportion of work shifts with drowsy driving reports by time of day is presented in Figure 1.
Table 3.
Relationship Between Shift Duration and Drowsy Driving
| Hours worked | Shifts with drowsy driving |
OR (95% CI) | P Value | |
|---|---|---|---|---|
| No. | % | |||
| ≤ 8.5 | 203 | 15.7 | 1.00 | |
| > 8.5 - < 12.5 | 923 | 22.3 | 1.35 (1.03–1.77) | 0.028 |
| ≥ 12.5 | 1793 | 31.3 | 2.00 (1.61–2.32) | < 0.0001 |
OR refers to odds ratio; CI, confidence interval.
Figure 1.
Reports of Drowsy Driving by Time of Day
Drowsy Driving and Alertness on Duty
Almost two thirds (65.8%) of the nurses (589/895) reported struggling to stay awake at work at least once during the study period, and 16.9% (151/895) of the nurses actually fell asleep at least once during their work shift. Nurses reported drowsiness on duty during 2271 of 11,160 shifts (20%), whereas actual sleep episodes occurred during 447 of 11,160 shifts (4%). Although nurses might be expected to report difficulties staying awake during the night shift, 47% (970/2078) of the drowsy episodes and 28% (118/415) of the sleep episodes occurred between 06:00 and 24:00.
Nurses who struggled to stay awake at work were significantly more likely to report struggling to stay awake driving home after work. In particular, the likelihood of a drowsy driving incident was tripled (OR = 3.37; P < 0.0001) when nurses experienced episodes of drowsiness at work (Table 4). The risk for a drowsy driving episode was also increased when nurses reported falling asleep on duty (OR = 1.31; P = 0.02).
Table 4.
Relationship Between Drowsy Driving and Decreased Vigilance on Duty
| Vigilance on duty | Shifts with drowsy driving, no. (%) | OR | P Value |
|---|---|---|---|
| Struggled to stay awake | |||
| No | 1611 (18.2) | 1.00 | |
| Yes | 1299 (57.7) | 3.37 | < 0.001 |
| Fell asleep | |||
| No | 2717 (25.6) | 1.00 | |
| Yes | 183 (41.4) | 1.31 | 0.02 |
OR refers to odds ratio.
Drowsy Driving and Sleep Duration
Although research on the effects of chronic sleep restriction has revealed that most adults require at least 7 to 8 hours of sleep each night to avoid developing chronic sleep debt with its accompanying performance deficits,19,28 the hospital staff nurses in our study frequently obtained less sleep than this critical threshold. Study participants averaged 6.70 ± 1.79 hours of sleep, including naps, on workdays and frequently reported to work with limited amounts of sleep (median sleep duration = 6.5 hours). Only 186 of the 895 participants (20.8%) reported obtaining at least 6.0 hours of sleep prior to every shift they worked.
Nurses who reported being drowsy driving home from work averaged 6.33 ± 2.10 hours of sleep. In comparison, nurses who did not experience drowsiness while driving obtained almost 7 hours of sleep (mean = 6.83 ± 1.63 hours). The risk for a drowsy driving episode increased by 9% for each hour of sleep lost.
Total and Adjusted Effects on Drowsy Driving
Multivariate regression analyses were performed to further examine the effects of the study variables on drowsy driving. Shift and sleep duration, alertness at work, and working at night remained significantly associated with drowsy driving episodes after controlling for all study variables, as well as age and dependent care responsibilities of the nurse participants. Alertness at work (i.e., drowsiness or sleep episodes) (OR = 2.93; P < 0.0001) and working at night (OR = 2.74; P < 0.0001) had the largest adjusted effects on drowsy driving when compared with work hours (OR = 1.53; P < 0.0001) and sleep duration (OR = 0.93; P < 0.0001). Based on these results, nurses who worked extended hours, worked at night, struggled to remain alert at work, or obtained less sleep were more likely to experience a drowsy driving episode.
DISCUSSION
The high number of nurses who report struggling to stay awake at least once during a 28-day data-collection period and the high number of shifts involved suggests that nurse drowsiness when driving home from work poses a significant hazard to both nurses themselves and the general public. More than two thirds of our participants reported struggling to stay awake driving home at least once during the data-gathering period. The proportion of nurses reporting drowsy driving episodes in this study is higher than the proportion reported in the general public in a four-week period (27%)29 and higher than the proportion reported for nurses in an earlier study.24 Two factors could explain the higher rates of drowsy driving among nurses: the use of different research methodologies and an increase in the number of nurses working 12-hour shifts in the 15 years since the Gold et al24 study. Participants in their study were asked to recall if they had nodded off driving home in the year prior to the study, whereas participants in our study were asked to document on a daily basis if they had struggled to stay awake driving home. This prospective assessment may have allowed us to capture a more accurate prevalence of drowsy driving among nurses. Whether nurses experienced drowsiness while driving or actually nodded while off driving home, both studies provide evidence of the risk to personal and public safety from fatigued nurses.
Our findings suggest that extended work hours may be a significant factor among hospital staff nurses. We found that 12-hour shifts, the most common scheduling pattern for hospital nurses in the United States, increased the risk of drowsy driving and the potential for an MVC/near-MVC. The findings are similar to those of Barger and colleagues13 who identified an association between extended work hours and the risk of a fatigue-related incident while driving. The likelihood of medical residents to fall asleep while driving (OR = 2.39) or stopped for traffic (OR = 3.69) significantly increases when they work 5 or more extended shifts in a month.13 Given that 53.9% of the nurses' work shifts involved extended durations (> 12.5 hours) in a 4-week period, the likelihood of a fatigue-related driving incident among nurses is apparent.
Nurses who worked extended shifts (≥ 12.5 hours) also reported difficulty staying awake at work almost 1 of every 3 shifts worked, compared with nurses who worked less than 12.5 hours. Nurses who reported decreased alertness on duty (drowsiness or sleep episodes at work) were also more likely to struggle to stay awake driving home from work.
The time of day that nurses worked was identified as an important factor. Nurses working night shifts were almost 4 times more likely to report difficulties staying awake driving home, as compared with nurses who did not work during the night. Since sleep propensity/circadian drive for sleep is the greatest during the early morning hours, it is not surprising that nurses who left work between the hours of 02:00 and 06:00 reported struggling to stay awake almost half the time during their drive home. Given that both shift duration and time of work shift are problematic, the combination of long work hours and working at night make driving home particularly hazardous.
Finally, shorter sleep durations were associated with greater risks of struggling to stay awake driving home. Nurses who reported struggling to stay awake reported sleeping, on average, 30 minutes less than those who were able to remain alert. The sleep durations of nurses reporting drowsy driving were similar to those reported earlier for critical care nurses who reported difficulties remaining alert on duty, making an error, or catching themselves making an error.30 Even though alertness at work and working at night had larger adjusted effects on drowsy driving than did sleep duration, it is important to note that the risk of a drowsy driving episode increased by 9% for every hour of sleep loss.
Awareness that sleepiness from work-rest schedules represents a significant risk to driving safety has increased markedly in recent years, as is evident in the development of policies and laws to curb this risk.31 The findings of this study suggest that nurses are not immune to the fatigue-related driving risks posed by work-rest schedules.
The study is limited by a reliance on self-report data from a relatively small number of hospital staff nurses and may not be representative of the work schedules and driving habits of other hospital staff nurses in the United States. However, the demographic characteristics and work hours reported by our sample are comparable with data reported by the National Sample Study of Registered Nurses,32 a probability-based sample, and other recent studies of nurse work hours.33
Unfortunately, the demographic information collected from the nurse participants did not include alcohol consumption, medication use, medical conditions, or history of snoring/sleep apnea. Future studies should include an examination of these variables and their relationship with drowsy driving among hospital staff nurses.
Because we asked about MVCs/near-MVCs as a combined question, we were not able to ascertain the actual prevalence of MVCs. Moreover, without documentation to substantiate the actual occurrence of an MVC, our analysis of MVCs was limited and must be interpreted with caution. Nevertheless, our findings do suggest that the likelihood of an MVC/near-MVC increases with extended work hours. Based on our data and the data presented in the tables by Gold et al,24 we believe it is safe to assume that many of the nurses reporting difficulties staying awake driving home, as well as the number of nurses whose shift durations exceeded 12.5 hours, were at risk for a fatigue-related crash. Slightly less than one third of the nurses participating in Gold et al's study (31.8%)24 reported difficulties nodding off when driving to and from work during the year prior to the study, yet one quarter of their participants reported having at least 1 near miss MVC due to sleepiness (25.5%). With the percentage of nurses reporting actual crashes due to sleepiness or experiencing episodes of drowsiness while driving, it is probable that an increase in sleep-related MVC rates among nurses may occur.
This paper describes a little recognized hazard to the safety of nurses and the general public. Given the large numbers of nurses who reported struggling to stay awake when driving home from work and the frequency with which nurses reported drowsy driving, greater attention should be paid to increasing nurse awareness of the risks and preventing drowsy driving. Nurses who fail to get sufficient sleep, work extended shifts (e.g., 12 hours or longer), work night shifts, or have difficulty remaining awake on duty should be particularly careful driving home or consider taking a short nap at the end of their shift before attempting to drive home.
ACKNOWLEDGMENTS
Financial Support for this study was provided by the Agency for Health Care Research and Quality grant (HS11963-01-Rogers) and an American Nurses Foundation Grant (Scott).
Footnotes
Disclosure Statement
This was not an industry supported study. Dr. Dinges has received research support from Cephalon; has participated in speaking engagements for Cephalon and Jazz Pharmaceuticals; and has consulted for Cephalon, Merck, Novartis, Pfizer, GlaxoSmithKline, Mars Masterfoods, and Proctor – Gamble. The other authors have indicated no financial conflicts of interest.
REFERENCES
- 1.NCSDR/NHTSA Expert Panel on Driver Fatigue. Drowsy driving and automobile crashes. Washington: National Highway Transportation Safety Administration; 1997. [Google Scholar]
- 2.Pack AI, Pack AM, Rodgman E, et al. Characteristics of crashes attributed to the driver having fallen asleep. Accid Anal Prev. 1995;27:769–775. doi: 10.1016/0001-4575(95)00034-8. [DOI] [PubMed] [Google Scholar]
- 3.McCartt AT, Rohrbaugh JW, Hammer MC. Factors associated with falling asleep at the wheel among long-distance truck drivers. Accid Anal Prev. 2000;32:493–504. doi: 10.1016/s0001-4575(99)00067-6. [DOI] [PubMed] [Google Scholar]
- 4.National Highway Traffic Safety Administration. Washington: US Department of Transportation; 2006. The impact of driver inattention on near-crash/crash risk. DOT HS 810 594. [Google Scholar]
- 5.National Safety Council. Drowsy driving. [Accessed on May 24, 2006]; Available at: http://www.nsc.org/library/facts/drowsy_driving.htm.
- 6.National Sleep Foundation. 2005 Sleep in America poll. [Accessed on April 20, 2005]; Available at: http://www.sleepfoundation.org/site/c.huIXKjM0IxF/b.2419039/k.14E4/2005_Sleep_in_America_Poll.htm.
- 7.Klauer SG, Dingus TA, Neale VL, et al. Washington: National Highway Traffic Safety Administration; 2006. The impact of driver inattention on near-crash/crash risk: an analysis using the 100 car naturalistic driving study data. DOT HS 810 594. [Google Scholar]
- 8.Stutts JC, Vaughn BV. Why do people have drowsy driving crashes? Input from drivers who just did. Washington: AAA Foundation for Traffic Safety; 1999. [Google Scholar]
- 9.Brown ID. Driver fatigue. Hum Factors. 1994;36:298–314. doi: 10.1177/001872089403600210. [DOI] [PubMed] [Google Scholar]
- 10.Horne J, Reyner L. Vehicle accidents related to sleep: a review. Occup Med. 1999;56:289–294. doi: 10.1136/oem.56.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Philip P, Sagaspe P, Taillard J, et al. Fatigue, sleepiness, and performance in simulated versus real driving conditions. Sleep. 2005;28:1511–1516. doi: 10.1093/sleep/28.12.1511. [DOI] [PubMed] [Google Scholar]
- 12.Kowalenko T, Haas-Kowalenko J, Rabinovich A, et al. Emergency medicine related MVCs—Is sleep deprivation a risk factor? Acad Emerg Med. 2000;7:451. [PubMed] [Google Scholar]
- 13.Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125–135. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 14.Geer RT, Jobes DR, Tew JD, et al. Incidence of automobile accidents involving anesthesia residents after on-call duty cycles. Anesthesiology. 1997;87:A938. [Google Scholar]
- 15.Marcus CL, Loughlin GM. The effect of sleep deprivation on driving safety in house-staff. Sleep. 1996;19:763–766. doi: 10.1093/sleep/19.10.763. [DOI] [PubMed] [Google Scholar]
- 16.Dawson D, Reid K. Fatigue, alcohol, and performance impairment. Nature. 1997;388:235. doi: 10.1038/40775. [DOI] [PubMed] [Google Scholar]
- 17.Williamson AM, Feyer AM. Moderate sleep deprivation produces impairments to cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med. 2000;57:649–655. doi: 10.1136/oem.57.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arendt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA. 2005;294:1025–1033. doi: 10.1001/jama.294.9.1025. [DOI] [PubMed] [Google Scholar]
- 19.Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–126. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 20.Washington: US Department of Health and Human Services, Health Resources and Services Administration; 2006. Preliminary findings: the registered nurse population: national sample of registered nurses—March 2004. [Google Scholar]
- 21.Totterdell P, Spelten E, Barton J, Smith L, Folkard S. On-shift and daily variations in self-report and performance measures in rotating-shift and permanent night nurses. Work Stress. 1995;9:187–197. [Google Scholar]
- 22.Takahashi M, Arito H, Fukudo H. Nurses' workload associated with 16-h night shifts. Effects of a nap taken during the shift. Psychiatry Clin Neurosci. 1999;53:223–225. doi: 10.1046/j.1440-1819.1999.00545.x. [DOI] [PubMed] [Google Scholar]
- 23.Borges FN, Fischer FM. Twelve-hour night shifts of healthcare workers: a risk to the patients? Chronobiol Int. 2003;20:351–360. doi: 10.1081/cbi-120019341. [DOI] [PubMed] [Google Scholar]
- 24.Gold DR, Rogacz S, Bock N, Tosteson TD, Speizer FE, Czeisler C. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health. 1992;82:1011–1014. doi: 10.2105/ajph.82.7.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Novak RD, Auvil-Novak SE. Focus group evaluation of night nurse shiftwork difficulties and coping strategies. Chronobiol Int. 1996;13:457–463. doi: 10.3109/07420529609020916. [DOI] [PubMed] [Google Scholar]
- 26.Rogers AE, Hwang W-T, Scott LD, Aiken LH, Dinges DF. The working hours of hospital staff nurses and patient safety. Health Aff. 2004;23:202–212. doi: 10.1377/hlthaff.23.4.202. [DOI] [PubMed] [Google Scholar]
- 27.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 28.Dinges DF, Baynard M, Rogers NL. Chronic sleep deprivation. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: Elsevier Saunders; 2005. pp. 67–76. [Google Scholar]
- 29.National Sleep Foundation. Sleep in America poll. [Accessed on January 10, 2004]; Available at: http://www.nationalsleepfoundation.org/publications/2001poll.cfm.
- 30.Rogers AE. Hospital staff nurses regularly report fighting to stay awake on duty. Sleep. 2003:A423. [Google Scholar]
- 31.Walsh JW, Dement WC, Dinges DF. Sleep medicine, public policy, and public health. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: Elsevier Saunders; 2005. pp. 648–656. [Google Scholar]
- 32.Spratley E, Johnson A, Sochalski J, Fritz J, Spenser W. Washington: US Department of Health and Human Services, Health Resources and Services Administration; 2001. The registered nurse population: national sample of registered nurses—March 2000. [Google Scholar]
- 33.Kramer M, Schmalenberg C. Staff nurses identify essentials of magnetism. In: McClure ML, Hinshaw AS, editors. Magnet hospitals: attraction and retention of professional nurses. Washington: American Nurses Association; 2002. pp. 25–59. [Google Scholar]