Abstract
Study Objectives:
Complex sleep apnea is defined as sleep disordered breathing secondary to simultaneous upper airway obstruction and respiratory control dysfunction. The objective of this study was to assess the utility of an electrocardiogram (ECG)-based cardiopulmonary coupling technique to distinguish obstructive from central or complex sleep apnea.
Design:
Analysis of archived polysomnographic datasets.
Setting:
A laboratory for computational signal analysis.
Interventions:
None.
Measurements and Results:
The PhysioNet Sleep Apnea Database, consisting of 70 polysomnograms including single-lead ECG signals of approximately 8 hours duration, was used to train an ECG-based measure of autonomic and respiratory interactions (cardiopulmonary coupling) to detect periods of apnea and hypopnea, based on the presence of elevated low-frequency coupling (e-LFC). In the PhysioNet BIDMC Congestive Heart Failure Database (ECGs of 15 subjects), a pattern of “narrow spectral band” e-LFC was especially common. The algorithm was then applied to the Sleep Heart Health Study–I dataset, to select the 15 records with the highest amounts of broad and narrow spectral band e-LFC. The latter spectral characteristic seemed to detect not only periods of central apnea, but also obstructive hypopneas with a periodic breathing pattern. Applying the algorithm to 77 sleep laboratory split-night studies showed that the presence of narrow band e-LFC predicted an increased sensitivity to induction of central apneas by positive airway pressure.
Conclusions:
ECG-based spectral analysis allows automated, operator-independent characterization of probable interactions between respiratory dyscontrol and upper airway anatomical obstruction. The clinical utility of spectrographic phenotyping, especially in predicting failure of positive airway pressure therapy, remains to be more thoroughly tested.
Citation:
Thomas RJ; Mietus JE; Peng CK; Gilmartin G; Daly RW; Goldberger AL; Gottlieb DJ. Differentiating obstructive from central and complex sleep apnea using an automated electrocardiogram-based method. SLEEP 2007;30(12):1756-1769.
Keywords: Complex sleep apnea, cardiopulmonary coupling, ECG, spectrogram, central
INTRODUCTION
STANDARD RECOMMENDATIONS FOR THE SCORING OF RESPIRATORY ABNORMALITY IN PATIENTS WITH SLEEP APNEA IDENTIFY OBSTRUCTIVE, CENTRAL, AND MIXED apneas; hypopneas; and periodic breathing.1 The polysomnographic morphology of relatively pure obstructive disease is well described. The respiratory abnormalities range from complete cessation of airflow (apneas) with continued respiratory effort, to discernable reductions in airflow (hypopneas), to flow limitation-recovery breath sequences.1,2 The duration of significant abnormality is usually 10 seconds or more, but use of flow monitoring with the nasal cannula-pressure transducer system can show an evolution over much longer or shorter intervals.2 Central apneas, periodic breathing (a pattern of waxing and waning respiratory effort), and Cheyne-Stokes respiration are patterns that suggest chemoreceptor-mediated respiratory control dysfunction.3 Traditionally, central apnea syndromes are defined by a central apnea index ≥5/h of sleep and a predominance of central events relative to the total events scored. This stringent approach may underestimate the contribution of chemoreflex abnormalities to sleep apnea pathogenesis. Moreover, accurate discrimination between obstructive and central hypopneas is thought to be unreliable using visual pattern recognition methods based on respiratory band and airflow signals; it requires esophageal manometry to quantify instantaneous respiratory effort.1
There is evidence that central and obstructive features may coexist in many individuals with sleep apnea. Reduced and oscillating motor tone to the upper airway can result in intermittent upper airway collapse in those with hypoxia-induced periodic breathing,4 and direct visualization of the upper airway reveals collapse at the nadir of the respiratory cycle to be common in central sleep apnea.5 As all respiratory events with evidence of flow limitation or presence of respiratory effort are conventionally scored as “obstructive” events, the role of respiratory control mechanisms in sleep apnea is likely further underestimated. We define complex sleep apnea as sleep disordered breathing secondary to simultaneous upper airway obstruction and respiratory control dysfunction.6,7 This pathophysiological definition results in predictable characteristics: 1) A polysomnographic pattern—respiratory oscillations that have a single dominant frequency due to chemoreflex driving and an improvement during REM sleep. 2) A specific therapeutic response to positive airway pressure—improvement of obstruction but worsening of periodic breathing with or without the induction of central apneas. 3) A sensitivity to indirect or direct manipulations of carbon dioxide (CO2), with worsening of respiratory events by progressive pressure increases or standard bilevel ventilation; improvement by minimizing hyperventilation with adaptive forms of positive airway pressure, exogenous CO2 or allowing re-breathing of CO2. Complex sleep apnea is different from central sleep apnea as the majority of apneas and hypopneas are obstructive, but the oscillatory pattern has a strong resemblance to periodic breathing. This syndrome is thus a mixture of obstructive sleep apnea and hypopnea with a periodic breathing pattern frequently made more overt, often with the induction of central apneas, by the pneumatic stabilization of the upper airway with positive airway pressure.
A recent study suggested a relatively high prevalence of complex sleep apnea in clinical practice8 but required positive airway pressure titration-induced central apneas and periodic breathing for diagnosis. Centers for Medicare and Medicaid Services has recently promulgated a definition of complex sleep apnea that requires: 1) an obstructive apnea hypopnea index ≥5/h on the diagnostic polysomnogram, and 2) a central apnea-hypopnea index of ≥5/h, which is more than half of all scored respiratory events, during positive airway pressure titration. Because central hypopneas are rarely scored in clinical practice, the definition essentially requires the occurrence of central apneas that make up more than 50% of all other scored respiratory events, a threshold that could miss clinically significant nonobstructive sleep apnea. A technique to identify the presence of central ventilatory instability on diagnostic polysomnograms that is not dependent on the identification of central apneas alone could be clinically useful, since such patients may not fully respond to positive airway pressure therapy, which primarily targets upper airway obstruction.
Highly predictable and almost metronomic oscillations of heart rate, blood pressure, arousals, and ventilation are well known features of sleep apnea syndromes driven by respiratory control dysfunction.9–12 In contrast, the upper airway consists of multiple interacting components that could exhibit variable intrinsic oscillatory patterns.13–16 We therefore hypothesized that a primarily obstructive upper airway abnormality would result in variable event-to-event cycle times, and that this difference in the regularity of pure obstructive versus central or complex sleep apnea would facilitate discrimination of these two syndromes. We recently developed and validated a method of characterizing cardiopulmonary interactions using time series analysis of a single-lead electrocardiogram (ECG).12 This methodology involves extracting and mathematically combining heart rate variability and ECG-derived respiration (as determined by amplitude modulation of the QRS complex associated with breathing). This ECG-based method generates a spectrographic measure of “cardiopulmonary coupling.” Two basic patterns of cardiopulmonary coupling are demonstrable in health and disease: high-frequency coupling (HFC), associated with breath-to-breath stability of tidal volume and sinus arrhythmia; and low-frequency coupling (LFC), associated with breath-to-breath cycles of fluctuating tidal volumes and cyclic variation in heart rate, usually recurring every 25–50 seconds, seen in health but markedly accentuated in those with sleep apnea.12 We hypothesized that relatively pure obstructive sleep apnea would result in multiple broad bands of low-frequency cardiopulmonary coupling spectral peaks, while central or complex sleep apnea, strongly influenced by instabilities in chemoreceptor control, would demonstrate cyclic oscillations at a relatively fixed frequency, resulting in a narrow band of low-frequency cardiopulmonary coupling.
To test this hypothesis, we first used an annotated sleep apnea database to train the cardiopulmonary coupling algorithm to detect periods of sleep apnea regardless of etiology or type, based on a subset of LFC oscillations, elevated LFC or e-LFC, that correlate with apneas and hypopneas. We then used a Holter monitor database of congestive heart failure subjects to train the algorithm to specifically detect central apnea-like physiological oscillations, based on the presence of narrow spectral band e-LFC. To confirm concordance between visual scoring and spectrographic types of sleep apnea, we applied the algorithm to polysomnograms acquired by the Sleep Heart Health Study (SHHS) that contained the highest amounts of either narrow spectral band e-LFC or broad spectral band e-LFC. Finally, we assessed the prevalence of the different types of cardiopulmonary coupling in SHHS subjects with an AHI ≥5, contrasting polysomnographic severity of those with and without narrow spectral band e-LFC.
METHODS
Subjects
PhysioNet Sleep Apnea Database
The open-access PhysioNet Sleep Apnea Database (http://www.physionet.org/physiobank/database/apnea-ecg/) was used to train the apnea detection algorithm to identify sleep apnea, as described below. This database (Table 1) consists of 70 single-lead ECG signals of approximately 8 hours, digitized at 100 Hz, extracted from full laboratory polysomnograms. Each recording includes a set of reference annotations, one for each minute of the recording, which indicates the presence or absence of apnea or hypopnea during that minute. All apneas in these recordings are either obstructive or mixed. The original reference annotations were made by an experienced sleep researcher on the basis of simultaneously recorded respiration signals. Thermistors were used for flow estimates. As a 50% reduction in amplitude accompanied by a drop in oxygen saturation of at least 4% and followed by compensating hyperventilation was required for scoring hypopneas, the respiratory events were severe. The subjects of these recordings are men and women between 27 and 60 years of age, with weights between 53 and 135 kg and AHI ranges from 0 to 93.5. The 70 polysomnogram recordings were divided into 3 groups based on the number of epochs containing apneas or hypopneas: a) No/trivial disease: 20 recordings from 11 men and 9 women, aged 27 to 42 years, containing fewer than 5 minutes with apnea or hypopnea during the recording; b) Moderate: 10 recordings from 8 men and 2 women, aged 39 to 53 years, which contain between 5 and 99 minutes with apnea during the recording; and c) Severe: 40 recordings from 38 men and 2 women, aged 29 to 63 years, which contain at least 100 minutes with apnea during the recording.
Table 1.
PhysioNet Sleep Apnea Database Analysis
| Measure | No Apnea (n=20) | Moderate Apnea (n=10) | Severe Apnea (n=40) | Combined (n=70) |
|---|---|---|---|---|
| Age(y) | 32.6 ± 5.4 | 47.2 ± 5.9 | 50.9 ± 8.3 | 45.1 ± 10.8 |
| Sex (M/F) | 11 / 9 | 8 / 2 | 38 / 2 | 57 / 13 |
| AHI, events/h of sleep | 0.04 ± 0.10 | 12.1 ± 12 | 46 ± 22.6 | 28 ± 27.5 |
| Apnea Time (min) | 0 | 0.1 ± 0.07 | 0.62 ± 0.22 | 0.37 ± 0.34 |
| e-LFC (proportion of spectral windows) | 0.08 ± 0.05 | 0.25 ± 0.14 | 0.58 ± 0.27 | 0.39 ± 0.31 |
| e-LFCNB (proportion of spectral windows) | 0.002 ± 0.007 | 0.02 ± 0.04 | 0.20 ± 0.20 | 0.12 ± 0.18 |
| e-LFCBB (proportion of spectral windows) | 0.08 ± 0.05 | 0.23 ± 0.12 | 0.38 ± 0.20 | 0.28 ± 0.21 |
AHI: Apnea-hypopnea index
Apnea Time = proportion of total sleep time in apnea or hypopnea, by human visual scoring
LFC: low frequency coupling
e-LFC: elevated LFC
e-LFCNB: narrow spectral band eLFC
e-LFCBB: broad spectral band ELFC
PhysioNet Congestive Heart Failure Database
The open-access PhysioNet BIDMC Congestive Heart Failure database (http://www.physionet.org/physiobank/database/chfdb/) was used to further train the apnea detection algorithm to identify central or complex sleep apnea, as described below. This database consists of 15 subjects (11 men, aged 22 to 71, and 4 women, aged 54 to 63) with severe congestive heart failure (NYHA class 3–4). The individual recordings are each about 20 hours and contain 2 continuous ECG signals each sampled at 250 samples per second. This group of subjects was part of a larger study group receiving conventional medical therapy prior to receiving the oral inotropic agent, milrinone. The original analog recordings were made at Boston's Beth Israel Hospital (now the Beth Israel Deaconess Medical Center) using ambulatory ECG recorders. This dataset did not contain reference apnea annotations. One subject was excluded because of atrial fibrillation.
Sleep Heart Health Study-I
The trained apnea detection algorithm was then used to analyze the SHHS data. The characteristics of the SHHS have been described in detail.17,18 Unattended overnight PSG was performed with a portable PS-2 system (Compumedics, Abottsville, Australia). Sensors were placed and equipment was calibrated during an evening home visit by a certified technician. Data collection included C3/A1 and C4/A2 EEGs; right and left electrooculograms; a bipolar submental electromyogram; thoracic and abdominal excursions (inductive plethysmography bands); airflow (detected by a nasal-oral thermocouple [Protec, Woodinville, WA]); finger pulse oximetry (Nonin, Minneapolis, MN) sampled at 1 Hz; electrocardiogram (ECG) sampled at 125 Hz; body position (mercury gauge sensor); and ambient light (on/off, by a light sensor secured to the recording garment). After equipment retrieval, the data were forwarded to a central Reading Center (Case Western Reserve University, Cleveland, OH) for scoring according to a standard protocol. The polysomnographic methods, scoring protocol, and quality assurance procedures have been previously described.17,18
Cardiopulmonary Coupling Analysis and Generation of Sleep Spectrograms
The cardiopulmonary coupling technique12 is based on a continuous ECG signal and uses the Fourier Transform to analyze 2 features of the signal: 1) heart rate variability and 2) the fluctuations in R-wave amplitude induced by respiration. These signals tend to have to have two basic patterns: a high-frequency component due to physiological sinus arrhythmia that reflects breath-to-breath fluctuations and a low-frequency component that reflects cyclic variation across multiple breaths. Quantification of cardiac and respiratory interactions involves calculating the cross-power and coherence between these 2 signals.
The steps involved in the calculation of cardiopulmonary coupling are as follows: 1) An automated beat detection algorithm is used to detect beats, classify them as either normal or ectopic, and determine amplitude variations in the QRS complex. From these amplitude variations a surrogate ECG-derived respiratory signal (EDR) is obtained. 2) A time series of normal-to-normal sinus (NN) intervals and the time series of the EDR associated with these NN intervals are then extracted from the RR interval time series. 3) Outliers due to false or missed R-wave detections are removed using a sliding window average filter with a window of 41 data points and rejection of central points lying outside 20% of the window average. 4) The resulting NN interval series and its associated EDR are then cubic spline resampled at 2 Hz. 5) The cross spectral power and coherence of these two signals are calculated over a 1024-sample (8.5 minute) window using the Fast Fourier Transform applied to the 3 overlapping 512-sample subwindows within the 1024-sample coherence window. The 1024-sample coherence window is then advanced by 256 samples (2.1 min) and the calculation repeated until the entire NN interval/EDR series is analyzed.
For each 1024-sample window the product of the coherence and cross-spectral power is used to calculate the ratio of coherent cross power in the low-frequency (0.01–0.1 Hz) band to that in the high-frequency (0.1–0.4 Hz) band. A preponderance of power in the low-frequency band tends to be associated with periodic sleep behaviors, while predominance of power in the high-frequency band is associated with respiratory sinus arrhythmia and sleep with stable respiration and EEG.12 A preponderance of power in the very-low-frequency (0–0.01 Hz) band is associated with periods of wakefulness or REM sleep. This technique thus generates a moving average of the dominant oscillatory frequencies of autonomic drive coupled with respiration during sleep.
Cardiopulmonary Coupling Analysis and Estimation of Elevated Low Frequency Coupling (e-LFC) Subtypes
Analysis of the PhysioNet Sleep Apnea Database using the cardiopulmonary coupling technique indicated that elevated power in the low-frequency coupling region coincided with periods of scored apnea/hypopnea. Optimal detection thresholds required that the minimum low-frequency power be >0.05 normalized units and that the low to high frequency ratio be >30 to define periods of probable apnea/hypopnea, which we term elevated LFC (e-LFC). Since the apneas and hypopneas in this database were scored in 60-s epochs and cardiopulmonary coupling measurements made every 2.1 min, 60-s linear interpolation between consecutive 2.1-min measurements was done. The 70 recordings in this database contained a total of 34,243 minutes of which 13,062 (38%) were scored as containing episodes of apnea/hypopnea. Sensitivities and specificities for minute-by-minute apnea detection were calculated for a range of low-frequency coupling powers and low/high coupling ratios. Receiver-operator curves were then calculated and the thresholds giving the maximum combined sensitivity and specificity for apnea/hypopnea detection was selected as optimal. Thus, e-LFC is defined here as a subset of low-frequency coupled cardiopulmonary oscillations, periods of which correlated significantly with periods of manually scored apneas and hypopneas in the PhysioNet Sleep Apnea Database.
Some spectrograms from the PhysioNet Sleep Apnea Database demonstrated periods of near-constant frequency spectral peaks in the e-LFC region that was reminiscent of the sinusoidal oscillations of heart rate variability seen in Cheyne-Stokes respiration in heart failure patients, which has a relatively constant cycle length.14–16 To explore this phenomenon further, we applied the algorithm to the PhysioNet Congestive Heart Failure Database, with the expectation that the database would provide more prolonged episodes with central periodic oscillations. Since the times during which these subjects were sleeping are not known, the 6 continuous hours of lowest heart rate was taken as the putative sleep time. Since the period of central apnea can be as slow as 120 seconds or longer, we used the frequency band between 0.006 and 0.1 Hz to define narrow spectral band e-LFC (putative central sleep apnea, periodic breathing, or complex sleep apnea). We required (1) a minimum power in this band of 0.3 normalized units and (2) that the coupling frequency of each pair of consecutive measurements remains within 0.0059 Hz of each other over 5 consecutive sampling windows (totaling 17 continuous min). Periods of e-LFC not meeting these criteria were defined as broad spectral band e-LFC (putative pure obstructive sleep apnea). The amounts of broad and narrow spectral band coupling in e-LFC bands were then expressed as the percentage of windows detected in relation to the total sleep period. Thus, the narrow spectral band e-LFC identified periods with oscillations that have a single dominant coupling frequency, suggesting central sleep apnea or periodic breathing. The broad spectral band e-LFC identified periods with oscillations that have variable coupling frequencies, suggesting an alternative mechanism, which we posited was dominance of anatomic upper airway obstructive processes. As it takes 17 min of continuous narrow-band cardiopulmonary coupling to reach the detection threshold, we estimated that this would be approximately equal to an averaged central apnea index of 5/h of sleep, assuming 6 h of sleep and a periodic breathing cycle length of approximately 35 seconds.
Spectrographic Analysis of the SHHS Database
Clinical characteristics of the subjects selected from the SHHS were obtained from the SHHS Coordinating Center. Rules for scoring respiratory events in the SHHS have been previously reported.19 Sleep stages were scored according to the guidelines developed by Rechtschaffen and Kales.20 Arousals were identified according to American Sleep Disorders Association criteria,21 modified to accommodate situations in which electromyogram artifact obscured the EEG signal. The common criterion to define an apnea (regardless of the nature of corroborating physiologic occurrences) was a complete or almost complete cessation of airflow (<25% of baseline), as measured by the amplitude of the thermocouple signal, lasting '10 s. The common criterion to define hypopnea (regardless of the nature of corroborating physiologic occurrences) was a clear reduction in the amplitude of flow or volume (detected by the thermocouple or by thorax or abdominal inductance band signals) to below 70% of the amplitude of “baseline” breathing for ≥10 s, but one that did not meet the criterion for apnea. Apneas were considered to be “central” if no effort was noted on both the thorax and abdominal effort channel. No attempt was made to classify hypopneas as obstructive or central in nature. After apneas and hypopneas were identified, software linked each event to data from the oxygen saturation and EEG channels. Each event was then characterized according to the degree of maximum associated desaturation (occurring up to 25 s after the end of the event) and to the presence of associated arousal (occurring up to 3 s after the event). Discrete respiratory disturbance indices were calculated on the basis of the airflow or volume criteria in conjunction with various combinations of associated desaturation and arousal. For this analysis, we considered the AHI based on events associated with 4% desaturation.
Of the 6430 SHHS-I polysomnograms available for analysis, 1183 did not meet the following inclusion criteria: a minimum of 4 h of available ECG data, no drop out of ECG signal for contiguous periods of more than 4 min, and ≥80% of R waves annotated by the software as normal R waves. Thus, studies with high rates of ectopy, atrial fibrillation, and excessively tall T waves that interfered with accurate QRS detection were excluded. An additional 1258 polysomnograms were excluded because sensor loss prevented scoring of central apnea by the SHHS Reading Center. These exclusions left 3989 studies suitable for comparing the full range of conventional scoring and spectrographic phenotyping. The 15 studies with the highest percentage of narrow spectral band e-LFC (Group I) and the 15 studies with the highest percentage of broad spectral band e-LFC (Group II) were selected for further analysis, as described below (“extreme” groups, Table 2). Examples of sleep spectrograms derived from SHHS polysomnograms, shown in Figures 1–4, demonstrate: 1) healthy sleep; 2) predominant broad spectral band e-LFC; 3) predominant narrow spectral band e-LFC; 4) alternating narrow and broad spectral band e-LFC.
Table 2.
Characteristics of “Extreme” Subjects Selected from the Sleep Heart Health Study
| Variable | Group I e-LFCNB n=15 | Group II e-LFCBB n=15 | P value |
|---|---|---|---|
| Age, y | 68.6 ±14.7 | 68.3 ± 7.4 | 0.9 |
| Body mass index, kg/m2 | 29.7 ± 6.1 | 29.6 ± 5.4 | 1.0 |
| Sex: F/M | 2/13 | 2/13 | 1.0 |
| Epworth Sleepiness Score | 10.6 ± 5.1 | 8.4 ± 4.1 | 0.2 |
| SHHS Sleep Scoring | |||
| Total sleep time (TST, min) | 308 ± 68.7 | 302 ± 80.8 | 0.8 |
| Sleep efficiency, % TST | 80.3 ± 8 | 72.3 ± 10.8 | 0.1 |
| Stage I % TST | 7.7 ± 6.5 | 11.6 ± 9.9 | 0.2 |
| Stage II % TST | 71.5 ± 12.4 | 55.8 ± 12.4 | 0.002 |
| Stage III + IV % TST | 6.8 ± 8 | 11.7 ± 9.6 | 0.15 |
| Stage REM % TST | 14.1 ± 6.3 | 20.9 ± 7.7 | 0.02 |
| Arousal index (per h of sleep) | 43 ± 20.9 | 32.2 ±17 | 0.14 |
| SHHS Respiratory Scoring | |||
| Obstructive Apnea Index* (per h of sleep) | 36.1 ±25.2 | 11.3 ± 15.6 | 0.008 |
| Central Apnea Index* (per h of sleep) | 8.7 ±13.2 | 1.5 ± 2.7 | 0.05 |
| AHI (per h of sleep) | 52.4 ± 17.7 | 34.4 ± 36.4 | 0.10 |
| AHI REM (per h of sleep) | 43.8 ± 16.8 | 30.5 ± 24 | 0.09 |
| AHI NREM (per h of sleep) | 53.5 ± 18.7 | 25.7 ± 18.6 | < 0.001 |
| Minimum saturation REM sleep (%) | 75.5 ± 12.5 | 83.4 ± 8.8 | 0.06 |
| Minimal saturation NREM sleep (%) | 77.6 ± 9.1 | 83.3 ± 5.7 | 0.06 |
| Spectrographic analysis | |||
| Low-frequency coupling, % of spectral windows | 90.2 ± 6.0 | 85.2 ± 5.7 | 0.03 |
| e-LFCNB, % of spectral windows | 58.2 ± 10.0 | 7.0 ± 8.5 | < 0.001 |
| e-LFCBB, % of spectral windows | 23.3 ± 12.4 | 63.6 ± 3.0 | < 0.001 |
| High-frequency coupling, % of spectral windows | 5.5 ± 6.5 | 2.5 ± 2.1 | 0.09 |
| Very low frequency coupling, % of spectral windows | 3.7 ± 3.0 | 11.0 ± 4.8 | < 0.001 |
e-LFC: elevated low frequency coupling
e-LFCNB: narrow band ELFC
e-LFCBB: broad band ELFC
SHHS: Sleep Heart Health Study
REM: rapid eye movement sleep
NREM: non-REM sleep
AHI: apneas + hypopneas associated with 4% oxygen desaturation/h of sleep
events identified independent of the presence of absence of oxyhemoglobin desaturation
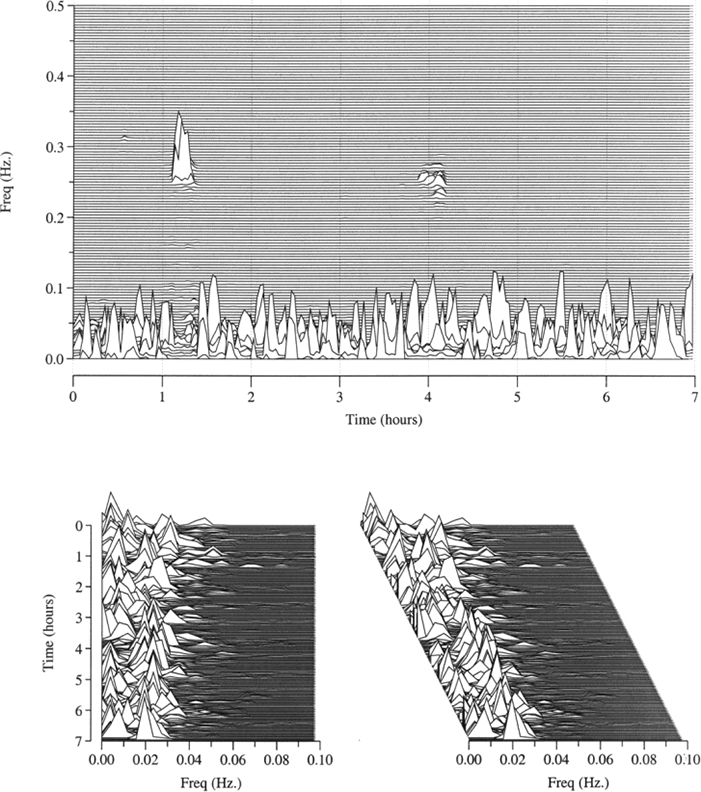
Figure 1.
Sleep spectrogram in health. The sleep spectrogram in a 57-year-old male, demonstrating the normal profile of high and low-frequency cardiopulmonary coupling (HFC and LFC, respectively) across a normal night of sleep. The AHI is 5 events per hour of sleep. Top: The all night sleep spectrogram. The spectrographic display of cardiopulmonary coupling shows the bimodal stability states, with health (as in this case) dominated by high-frequency cardiopulmonary coupling. Lower left and right: 90° and 60° rotated views of the low-frequency spectral zone from the same subject showing the spectral dispersion within the sparse periods of low-frequency cardiopulmonary coupling.
Figure 2.
Spectrographic obstructive sleep apnea. A 62-year-old man with an AHI of 49 events per hour of sleep. Broad spectral band e-LFC suggests oscillations driven by anatomical abnormality. Top: The all night sleep spectrogram. The upper panel shows nearly complete loss of high frequency coupling. Lower left and right: 90° and 60° rotated views of the low-frequency spectral zone from the same subject showing the spectral dispersion within the low-frequency cardiopulmonary coupling spectrum. This view demonstrates the characteristics of virtually pure elevated broad spectral band LFC. Conventional scoring of the respiratory events in this instance is usually “obstructive”, but may also be “mixed.”
Figure 3.
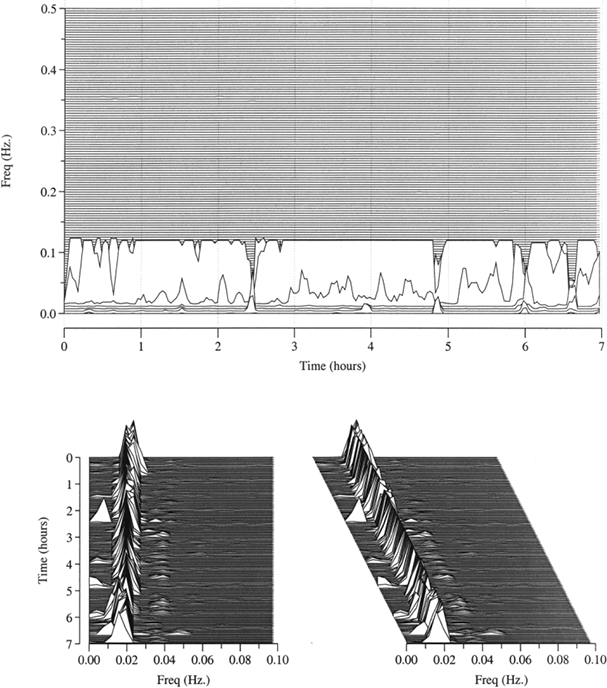
Sleep spectrogram in “complex” sleep apnea - I: A 77-year old-male with an AHI of 65 events per hour of sleep. Continuous narrow spectral band e-LFC suggests oscillations driven by chemoreflexes. Top: The all night sleep spectrogram. The upper panel shows complete loss of high frequency coupling. Lower left and right: 90° and 60° rotated views of the low-frequency spectral zone from the same subject showing the spectral dispersion within the low-frequency cardiopulmonary coupling spectrum. This view demonstrates the characteristics of virtually pure elevated narrow spectral band e-LFC. Conventional scoring of the respiratory events in patients with respiratory dyscontrol may be “central” or have varying degrees of obstruction as determined by visual inspection of the flow signals and respiratory effort. The respiratory events thus could be highly periodic obstructive apneas and hypopneas or classic periodic breathing and central apneas – the spectrographic signatures of all of these types of respiratory abnormalities are indistinguishable by this method.
Figure 4.
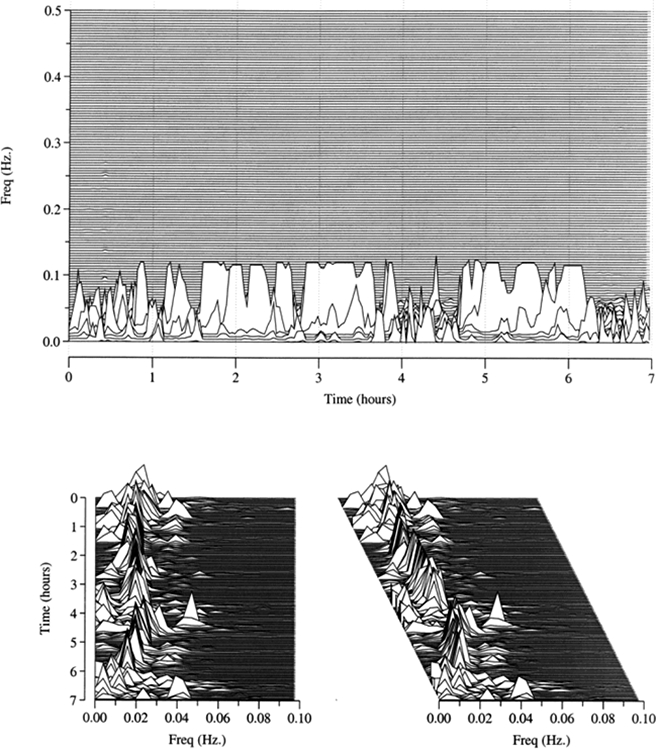
Sleep spectrogram in complex sleep apnea - II: A 60-year-old male with an AHI of 75 events per hour of sleep. Top: The all night sleep spectrogram. The upper panel shows complete loss of high frequency coupling. Lower left and right: 90° and 60° rotated views of the low-frequency spectral zone from the same subject showing the spectral dispersion within the low-frequency cardiopulmonary coupling spectrum. Alternating narrow and broad spectral band e-LFC is seen, suggesting varying moment to moment predominance of central ventilatory control versus anatomic factors in the pathogenesis of sleep apnea in this subject. Conventional scoring of the respiratory events may be “central,” “obstructive” or “mixed,” often showing significant temporal variability.
Sleep Laboratory Titration Response Database
A retrospective assessment was performed of archived polysomnographic data from consecutive patients seen in the AASM-accredited Multidisciplinary Sleep Disorders Center at the Beth Israel Deaconess Medical Center, Boston, Massachusetts between January and June 2005. IRB approval was obtained for access to the raw polysomnographic data, sleep study reports, and clinical covariates. The polysomnographic selection criteria were: 1) Diagnostic polysomnogram with subsequent positive airway pressure titration polysomnogram, or split night polysomnogram. 2) Apnea-hypopnea index (AHI) ≥10. Exclusion criteria were: 1) Low awake baseline oxygen saturations (≤92%). 2) Presumed hypoventilation, identified by oxygen saturations ≤90% with positive airway pressure optimized to control obstruction and flow-limitation during sleep; 3) nocturnal oxygen use; 4) diabetes with retinopathy, neuropathy, or nephropathy; heart failure; chronic renal failure on dialysis; or stroke; 5) use of sedative or antidepressant medications, 6) cardiac rhythm disturbances that preclude or degrade cardiopulmonary coupling analysis (atrial fibrillation, ventricular bigeminy or trigeminy, demand or biventricular cardiac pacing); 7) total sleep time <4 h on the diagnostic assessment if not a split-night study; and 8) mask intolerance due to claustrophobia. Of 546 sleep studies, 77 were selected for further analysis. The most common cause for exclusion was use of exclusionary medications (321 subjects). Others included wake or sleep hypoventilation (34), cardiac arrhythmia (28), inadequate total sleep time (16), and high risk clinical condition (88). More than one reason for exclusion was present in 18 subjects.
The rationales for some of these strict exclusionary criteria for the preliminary assessment of our technique were as follows: 1) Subjects with hypoventilation syndromes may have abnormal (reduced) chemosensitivity and thus be less likely to exhibit periodic breathing; moreover, supplemental oxygen may have been used that could reduce periodic breathing. 2) Those with baseline oxygen desaturation may acclimatize to hypoxia and thus exhibit some resistance to periodic breathing. 3) Patients with advanced diabetes, heart failure, post-stroke and renal failure are known to be at high risk for complex sleep apnea, and the target sample for this preliminary analysis was the typical sleep laboratory patient devoid of high risk features. 4) Sedative medications may reduce periodic breathing periods by increasing the proportion of stable NREM sleep and thus cause false negative results, while antidepressants have complex and not fully defined effects on upper airway physiology.
Polysomnogram Scoring
All polysomnograms included central and occipital EEG derivations, bilateral electro-oculograms, submental electromyogram, chest and abdominal excursion by piezo bands, finger pulse oximetry, single-lead ECG in the Lead II configuration, leg electromyogram, snoring by pre-tracheal microphone, and body position. Airflow was monitored with thermistors and nasal-cannula pressure transducer set-ups during diagnostic sleep studies. Flow (pneumotachograph) and mask pressure were monitored during positive airway pressure titration. Sleep and arousal scoring were performed using standard criteria.20,21 Respiratory event scoring was a minor modification of the research standard.1 Apneas were scored by an experienced (>10 y) certified sleep technologist when flow was reduced to ≤10% of baseline on the nasal pressure and thermistor signals for ≥10 s with ongoing effort (obstructive) or loss of effort (central). Hypopneas were scored when there was one or more of the following: a clear reduction in nasal pressure and/or thermistor amplitude; progressive flow limitation with any reduction in amplitude; or a few flow limited breaths, all terminated by an abrupt sinusoidal recovery breath. An apnea-hypopnea index (AHI) was calculated as the number of apneas and hypopneas associated with 4% oxygen desaturation per hour of sleep. The respiratory disturbance index (RDI) includes events without 4% desaturation but associated with an arousal or arousal equivalent (<3 s but associated with one of the following: cardiac acceleration, submental electromyogram tone elevation, or a cluster of slow waves, all temporally linked to the recovery of airflow).
Positive Airway Pressure Titration
Continuous (CPAP) and bilevel positive airway pressure titration was accomplished by trained and certified sleep technologists. The criteria employed by the sleep laboratory for initiation of a split-night PAP titration are an AHI ≥10 or an RDI ≥40. The technicians are trained to recognize in real time stable and unstable NREM sleep using the electroencephalographic features of cyclic alternating pattern, to avoid inappropriate increases in pressure during stable NREM sleep.22,23 The endpoint for successful continuous positive airway pressure titration was control (normalized flow and arousal-free sleep, RDI on optimal pressure ≤5 per hour of sleep) in supine REM and unstable NREM sleep. Once this was accomplished, bilevel positive airway pressure titration was initiated with the same end-points (more likely on a dedicated full-night positive pressure titration than a split night). Our laboratory routinely attempts to evaluate bilevel pressure following continuous pressure titration to avoid repeat assessments secondary to home pressure intolerance. In those who have central apneas on CPAP, bilevel positive airway pressure with and without a back-up rate and narrow inspiratory-expiratory (2–4 cm H2O) pressure difference is evaluated. If there was any worsening of sleep apnea control, as can happen in those with central or complex sleep apnea, bilevel pressure was immediately discontinued with a return to CPAP.
Determination of Positive Airway Pressure Titration Outcome
All titrations were reviewed blindly epoch-by-epoch by a board certified sleep specialist to assess polysomnographic success or failure. Adequate control of sleep apnea was defined as elimination of apneas, hypopneas, flow limitation, desaturations, and respiratory-related arousals during REM and unstable NREM sleep. The residual RDI when control was adequate was ≤5 per hour of sleep. The clinical criterion for positive airway pressure titration failure was a central apnea index of ≥5 per hour of sleep at or below the pressure required to control upper airway obstruction on the titration component of the polysomnogram.
Statistical Analysis
Descriptive statistics are presented regarding the performance of the cardiopulmonary coupling algorithm in the development databases (PhysioNet Sleep Apnea and Congestive Heart Failure Databases). Clinical characteristics and polysomnographic features of the 2 groups of SHHS subjects (predominant narrow spectral band e-LFC and predominant broad spectral band e-LFC) were compared using independent sample t-tests or chi-square tests as appropriate. In the SHHS-I dataset, using those with an apnea-hypopnea index of ≥5/h of sleep (2499 polysomnograms), correlation coefficients were estimated between automated detection of central sleep apnea (percentage of windows with narrow spectral band e-LFC) and conventional event scoring (central apnea index).
For evaluation of positive airway pressure titration response, both the presence of narrow spectral band e-LFC and success of positive airway pressure titration were considered as categorical variables. Comparison of polysomnographic and spectrographic variables between groups that had successful or failed titration used unpaired t-tests. Stepwise logistic regression analysis was used to estimate the odds ratio for titration success, adjusting for central apnea index, sleep apnea severity (AHI above or below 30/hr), sex, age, and oxygen desaturation severity. STATA/SE 8.0 was used for statistical analysis.
RESULTS
Sleep Apnea and Congestive Heart Failure Databases
The final ECG-based algorithm for detecting sleep apnea based on the presence of low-frequency cardiopulmonary coupling was compared to sleep apnea detection by expert human scoring of the PhysioNet Sleep Apnea Database (Table 1). Based on scoring by an experienced human sleep researcher, for the entire sample of 70 subjects the mean AHI was 28.1 ± 27.5 (range 0–93.5) events/hour and 38% ± 34% of sleep time contained apneas or hypopneas. The ECG-based algorithm identified e-LFC in 39% ± 31% of sleep time. The overall coefficient of correlation for the percentage of recording time detected as e-LFC by the ECG-based method vs. the percentage of time scored as containing apneas or hypopneas by human scoring was r = 0.88, P < 0.01. Although human scoring identified all apneas in this database as obstructive or mixed in nature, the ECG-based algorithm identified 28% ± 21% of sleep time as containing obstructive sleep apnea based on the presence of broad spectral band e-LFC, and 12% ± 18% of sleep time as central or complex sleep apnea based on the presence of narrow spectral band e-LFC. The fraction of time detected as obstructive vs. central or complex sleep apnea differed across the three previously identified subsets of this database: a) Severe sleep apnea: 0.38 ± 0.20 vs. 0.20 ± 0.20; b) Moderate sleep apnea: 0.23 ± 0.12 vs. 0.02 ± 0.04; and c) Minimal sleep apnea: 0.08 ± 0.05 vs. 0.002 ± 0.007. The percentage of total e-LFC that was narrow-band for the three groups was 34.0%, 8.3% and 1.8%, respectively. In the PhysioNet Congestive Heart Failure Database, the fraction of putative sleep time detected as broad-band (obstructive) and narrow band (central or complex) sleep apnea was 0.19 ± 0.16 and 0.18 ± 0.23, respectively; thus, 48.0% of detected sleep apnea in this sample was identified as central or complex.
SHHS–I
Narrow spectral band e-LFC was present in 957 of 3989 subjects (24%) by the ECG-based spectrographic method, while a central apnea index ≥5 was observed in 89 (2.2%) by conventional scoring. When the analysis is restricted to the 2499 subjects with AHI-4% ≥5, central or complex sleep apnea defined by the presence of narrow spectral band e-LFC was present in 37% of subjects. The sex ratio was (male/female) 69.9/30.1 and 56.9/43.1 in the narrow vs. broad spectral band e-LFC groups, respectively (chi square P: < 0.001). The AHI was 22.9 ± 18 and 13.7 ± 10.9/h of sleep (t-test P: < 0.001), in those with and without narrow spectral band e-LFC. There was a modest but statistically significant correlation between the percentage of time with narrow-band coupling and frequency of central apneas (r: 0.18, P < 0.001).
Two groups of 15 SHHS-I subjects were identified on the basis of high percentages of broad or narrow spectral band e-LFC, as described above. The 2 groups were similar in age, body mass index, and daytime sleepiness as measured by Epworth Sleepiness Scale score. Sleep stage distribution was notable for a lower percent REM sleep in the group with narrow-band coupling (Table 2). Those with a predominance of narrow spectral band e-LFC also had a predominance of conventionally scored central apneas, with a nearly 6-fold higher central apnea index. In contrast to those with broad spectral band e-LFC, the AHI in the group with narrow spectral band e-LFC was higher in NREM than REM sleep, a pattern commonly seen during sleep at high altitude or in those with central sleep apnea. This group also had more severe obstructive disease, as demonstrated by the higher frequency of obstructive apneas, and lower minimum saturations.
Sleep Laboratory Titration Response Database
Subject and Polysomnographic Characteristics
These subjects (n=77) had very severe sleep apnea, as demonstrated by daytime sleepiness (Epworth Sleepiness Scale score of 14 ± 3.2) and high AHI (47.2 ± 15.7), and had predominantly obstructive disease by conventional scoring. Only 18 of 77 had a central apnea index ≥5/h of sleep. Narrow spectral band e-LFC was identified in 32 of 77 (41.6%) patients in this retrospectively analyzed group of severe sleep apnea patients. Sleep disordered breathing was of greater severity in those with narrow spectral band e-LFC than in those with broad spectral band e-LFC, but the central apnea indices and the total amount of broad spectral band e-LFC were similar across groups, as were sleep stage distribution and arousal frequency (Table 3). The reduced total sleep time seen in those with narrow spectral band e-LFC may in part reflect earlier application of therapy due to greater disease severity.
Table 3.
Comparison by Spectrographic Phenotypes - Diagnostic
| Measure | e-LFCBB n=45 | e-LFCNB n=32 |
|---|---|---|
| Age (y) | 47 ± 7.3 | 53.3 ± 8.2 |
| Sex (male/female) | 36/9 | 26/6 |
| Body Mass Index (Kg/M2) | 28 ± 3 | 27.6 ± 2 |
| Epworth Sleepiness Score | 14 ± 2.8 | 14.6 ± 3.7 |
| Conventional polysomnographic analysis | ||
| Total Sleep Time (TST, min) | 232.1 ±124.3 | 171.7 ± 102.2 |
| Wake After Sleep Onset | 21.1 ± 14.6 | 22.8 ± 13.9 |
| Sleep Efficiency | 74.7 ± 16.1 | 68 ± 15.7 |
| Stage I % TST | 15.7 ± 14.9 | 21.9 ± 15.4 |
| Stage III+IV % TST | 4.4 ± 7.6 | 4.4 ± 8 |
| Stage REM %TST | 9.3 ± 7.9 | 6.3 ± 7.3 |
| Arousal index (per h of sleep) | 77.3 ± 23.1 | 89.2 ± 33.2 |
| Apnea Hypopnea Index (per h of sleep) | 37.6 ± 40.9 | 61.8 ± 40.9 |
| Central Apnea Index (per h of sleep) | 4.4 ± 6 | 6.6 ± 13.1 |
| Obstructive Apnea Index (per h of sleep) | 18.6 ± 29.5 | 36.5 ± 36 |
| Periodic Limb Movement Index (per h of sleep) | 1.8 ± 2.8 | 1.6 ± 3.8 |
| Minimal nocturnal oxygen saturation | 83 ± 7.1 | 76.8 ± 8.3 |
| Spectrographic analysis | ||
| Low Frequency Coupling (% of spectral windows) | 60.7 ± 10.1 | 64.7 ± 11.5 |
| High Frequency Coupling (% of spectral windows) | 14.3 ± 11.2 | 15.1 ± 11.2 |
| e-LFCBB (% of spectral windows) | 33 ± 8 | 32.4 ± 12.1 |
| e-LFCNB (% of spectral windows) | 0 | 12 ± 9 |
| Very low frequency coupling, % of spectral windows | 23.4 ± 5.2 | 19.9 ± 4.3 |
*Chi Square Total Sleep Time includes split night studies (40/77).
e-LFCBB: Elevated low frequency cardiopulmonary coupling – broad band
e-LFCNB: Elevated low frequency cardiopulmonary coupling – narrow band
Positive Airway Pressure Titration Outcomes
Forty of the 77 analyzed polysomnograms were combined diagnostic and therapeutic assessments (“split-night” studies), of which 28 were in the group with complex sleep apnea based on failure of positive airway pressure titration). Using a threshold of ≥5 central apneas per hour of sleep, only 16 subjects (21%) would have been identified as having complex sleep apnea. All subjects were first evaluated with CPAP. Bilevel positive pressure therapy, with and without a back-up rate when central apneas were induced, was evaluated in 62 subjects, including 100% in the complex sleep apnea group and 64% of the group with successful positive airway pressure titration. The mean continuous positive pressure that controlled flow-limitation was 12 ± 2.1 cm H2O in the group with successful titration, compared to a maximum tolerated pressure without worsening periodic breathing and central apneas of 8.2 ± 2.3 cm H2O in the group with failed titration. Bilevel positive airway pressure application (inspiratory pressure range 7–18 and expiratory pressure range 5–12) was noted to worsen respiratory instability in 26 of 35 (74%) of the group with failed titration, but in none of the group with successful titration. The duration of bilevel positive pressure application was 42%± 12% vs. 8% ± 4% of total titration time in the successful vs. failed titration groups. In contrast to those with successful positive airway pressure titration, sleep quality and sleep disordered breathing remained markedly abnormal in those with positive pressure titration failure due to induction of complex sleep apnea (Table 4). High frequency coupling was increased to a greater extent than conventionally scored slow wave sleep during successful pressure titration.
Table 4.
Comparison by Spectrographic Phenotypes - Titration
| Measure | Successful Titration n=42 | Failed Titration n=35 | P |
|---|---|---|---|
| Conventional polysomnographic analysis | |||
| Total Sleep Time (TST, min) | 379.6 ± 70.1 | 220.6 ± 48.6 | 0.04 |
| Wake After Sleep Onset | 9.7 ± 4.7 | 27.9 ± 11.2 | 0.02 |
| Sleep Efficiency | 90.6 ± 8.1 | 72.4 ± 9.6 | 0.01 |
| Stage I % TST | 8.5 ± 2.2 | 16.9 ± 6.2 | 0.01 |
| Stage III+IV % TST | 18.9 ± 4.4 | 4.6 ± 3.1 | < 0.001 |
| Stage REM %TST | 18.9 ± 7.2 | 18.1 ± 6.2 | 0.1 |
| Arousal index (per h of sleep) | 18.8 ± 4.1 | 32.5 ± 6.9 | 0.001 |
| Apnea Hypopnea Index (per h of sleep) | 8.4 ± 2.5 | 33.9 ± 7.8 | < 0.001 |
| Central Apnea Index (per h of sleep) | 0.7 ± 1.2 | 15.9 ± 6.4 | < 0.001 |
| Obstructive Apnea Index (per h of sleep) | 1.7 ± 0.9 | 3.6 ± 2.1 | 0.04 |
| Periodic Limb Movement Index (per h of sleep) | 5.7 ± 3.2 | 6.3 ± 3.7 | 0.2 |
| Minimal nocturnal oxygen saturation | 96.3 ± 3.3 | 88.8 ± 6.4 | 0.01 |
| Spectrographic analysis | |||
| Low Frequency Coupling (% of spectral windows) | 12.6 ± 4.7 | 56.7 ± 7.3 | < 0.001 |
| High Frequency Coupling (% of spectral windows) | 72.2 ± 9.2 | 21.9 ± 4.6 | < 0.001 |
| e-LFCBB (% of spectral windows) | 14.3 ± 3.4 | 28.6 ± 7.9 | < 0.01 |
| e-LFCNB (% of spectral windows) | 1.4 ± 2.1 | 19.2 ± 5.4 | < 0.001 |
| Very low frequency coupling, % of spectral windows | 14.3 ± 4.1 | 20.8 ± 6.3 | 0.01 |
Total Sleep Time includes split night studies (40/77).
Predictive Value of Polysomnographic and Spectrographic Measures
In stepwise regression analysis, the presence of narrow spectral band e-LFC was the strongest predictor of success or failure of positive airway pressure titration. Only two of the 32 (6.3%) subjects with the presence of any narrow spectral band e-LFC had a successful positive airway pressure titration, due to induction of complex sleep apnea. In those without narrow spectral band e-LFC, only 5 of 45 (11%) failed titration due to induction of complex sleep apnea. The adjusted (for age, sex, body mass index, AHI, central apnea index, and minimal nocturnal desaturation) odds ratio of positive airway pressure titration success in the presence of narrow spectral band e-LFC was 0.001 (CI: 0.0–0.04; chi square = 66.4, P: < 0.001); unadjusted odds ratios are summarized in Table 5. As a method to predict successful positive airway pressure titration, the spectrographic measure had the following predictive characteristics: specificity: 95.2%, sensitivity: 85.7%, positive predictive value: 88.9%, negative predictive value: 93.7%, correctly classified: 90.9%. Single-channel ECG-derived spectrographic narrow spectral band e-LFC was superior to categorization based on severity of nocturnal oxygen desaturation, sleep apnea severity, or a conventional central apnea index threshold (≥5/h of sleep) (Table 5).
Table 5.
Predictive (of PAP Failure) Characteristics of Polysomnographic and Spectrographic Measures
| Measure | Sensitivity | Specificity | PPV | NPV | Success odds ratio (C.I.) | P (for odds) |
|---|---|---|---|---|---|---|
| CAI-5 (per h of sleep) (n=19) | 81 | 31.4 | 58.6 | 57.9 | 0.51 (0.18–1.47) | 0.21 |
| AHI-30*(per h of sleep) (n=45) | 54.8 | 74.3 | 71.9 | 57.8 | 0.29 (0.11–0.76) | 0.01 |
| Sat80 (%) (n=48) | 66.7 | 42.9 | 58.3 | 51.7 | 1.5 (0.59–3.79) | 0.39 |
| Presence of narrow spectral band e-LFC** (n=32) | 95.2 | 85.7 | 88.9 | 93.7 | 0.01 (0–0.05) | < 0.001 |
Significant after adjustment for minimum nocturnal oxygen saturation, age, sex, but not narrow spectral band e-LFC
Significant after adjustment for AHI, nocturnal oxygen saturation low, age, sex; provided values are after adjustment
PPV: Positive Predictive Value
NPV: Negative Predictive Value
CAI-5: Grouping with central apnea index of less or greater than 5/hour of sleep
AHI-30: Grouping with AHI less and more than 30/h of sleep
Sat80: Grouping with minimum nocturnal oxygen saturation ≤/≥ more than 80%
DISCUSSION
In the present study, we have described a method to classify sleep apnea based on spectral profiles of ECG-based cardiopulmonary coupling. The 2 spectral profiles, broad-band and narrow-band, are visually distinctive. While the ability of these different spectral profiles to discriminate central from obstructive sleep apnea appears generally concordant with human visual-manual scoring, the cardiopulmonary coupling method detects more central-appearing sleep apnea than do conventional respiratory scoring approaches. The presence of narrow spectral band e-LFC identifies subjects with evidence of a prominent central component to their sleep apnea, as indicated by a high proportion of central apneas and a relative NREM predominance of apneas and hypopneas. The results in the heart failure database should be taken with caution. Sleep and breathing were not recorded, the putative sleep time is a rough estimate, and it is not really known if the subjects had periodic breathing. However, the presence of relatively large amounts of narrow spectral band e-LFC in patients with heart failure was an important intermediate step in our conceptualization of the sleep spectrographic approach to phenotyping sleep apnea.
Among SHHS-I subjects with AHI ≥5, those with narrow spectral band e-LFC had greater disease severity and a more striking male predominance than those with purely broad band e-LFC. A similar male preponderance has been described for central sleep apnea in heart failure.24 There is also evidence that respiratory control dysfunction contributes to severity of obstructive sleep apnea.25–27 Thus, the cardiopulmonary coupling methodology may be capable of noninvasively providing insights into the complex interactions between respiratory control and upper airway obstruction. We speculate that the presence of elevated narrow spectral band e-LFC reflects abnormal chemoreflex modulation of respiration during sleep regardless of the exact polysomnographic event designation (obstructive or central apnea, hypopnea, or periodic breathing), although the present study does not provide direct evidence of this. Thus, central and complex sleep apnea, and periodic breathing, can be thought to be driven in part by aberrant chemoreflex modulation of respiratory control. CPAP-induced central sleep apnea is a characteristic of complex sleep apnea, but both central and complex sleep apnea have identical spectral signatures—they cannot be distinguished by the spectrographic technique.
Our preliminary findings suggest that the classification of sleep apnea syndromes based on the 2 distinct spectral profiles, narrow spectral band e-LFC and broad spectral band e-LFC, may have clinical utility. In a preliminary assessment, the presence of narrow spectral band e-LFC was able to identify individuals at high risk for the induction of central apneas during positive airway pressure titration with high accuracy. This characteristic pattern may, therefore, permit identification of individuals with “complex sleep apnea” during diagnostic polysomnograms, prior to application of positive airway pressure therapy. Neither central apnea index nor the severity of sleep apnea (as reflected by the AHI or oxygen desaturation) during the diagnostic polysomnogram reliably predicted positive airway pressure failure. Bilevel positive airway pressure can induce or worsen central sleep apnea, and our routine evaluation of bilevel pressure therapy may have amplified differences between groups. However, the short duration of bilevel positive airway pressure assessment in those with complex sleep apnea suggests that this did not have a large impact on the findings. The SHHS is an observational study, and the outcomes of treatment, if any, are not available.
The differences in the spectrographic display of obstructive sleep apnea (multiple frequencies, broad-band pattern) and central and complex sleep apnea (single frequency, narrow-band pattern) are both visually striking and readily quantifiable. Mixed patterns of coupling spectra are presumed to reflect varying degrees of anatomical and respiratory control dysfunction, although more intensive physiologic studies are needed to confirm this hypothesis. As esophageal manometry, the gold standard for respiratory effort and central apnea detection,28 was not available in any of the polysomnograms analyzed, the relationships of esophageal pressure patterns with cardiopulmonary-coupling detected complex physiology cannot be established from our data. Whether increased hypoxic or hypocapnic sensitivity explains some of the variance in coupling characteristics merits further study.
The ECG-based cardiopulmonary coupling methodology has several advantages over conventional visual scoring of polysomnograms. The method is automated, reliable, easily repeated, and relatively inexpensive. It may permit classification of periods of hypopneas as central versus obstructive; although hypopneas constitute the large majority of scored respiratory events, they are typically not classified as central or obstructive due to the limitations of conventional polysomnographic methodology. Accurate classification of respiratory abnormality during sleep may allow improved risk stratification in epidemiological studies and may also improve therapy in patients with sleep apnea. Increasing evidence suggests that positive airway pressure fails to adequately treat those in whom respiratory control abnormality is significant.6,29 These groups may include patients with stroke,30 congestive heart failure,31 idiopathic central apnea, and those who have NREM-dominant obstructive disease.6 Such patients may need a multimodality approach that includes positive airway pressure, adaptive servo-ventilation, supplemental oxygen, minimization of hypocapnia, and stabilization of sleep state.7,32–34 Sleep spectrograms could help both to improve diagnostic accuracy and to allow estimation of therapeutic efficacy. The cardiopulmonary coupling methodology may also allow dynamic tracking of pathophysiology across a night. For example, switches between anatomic and respiratory control dysfunction may occur with changes in body position, sleep stage, time of night, or positive airway pressure therapy. It may suggest respiratory control dysfunction as a cause of failure of positive airway pressure therapy, if narrow spectral band e-LFC persists, or if broad converted to narrow spectral band e-LFC during treatment. With the availability of new forms of positive airway pressure therapy and adjunctive approaches to management of nonobstructive forms of sleep apnea, phenotyping using methods that complement conventional approaches may better select patients who may benefit from these modalities. However, the clinical usefulness of such an approach remains unproven.
Limitations of the cardiopulmonary coupling methodology include the lack of respiratory event severity quantification and unreliability in the presence of atrial fibrillation or frequent ventricular ectopy. Thus, in populations at high risk for arrhythmias, such as heart failure, there may be significant limitations using ECG alone. Using direct airflow measures may overcome some of these limitations. As methodological constraints require a minimum of 17 min of sustained narrow-band coupling for detection, shorter sequences of central apneas, or repetitive brief clusters of central apneas and periodic breathing may not be detected as such. Due to the averaging inherent in the technique, if mixtures of central and obstructive respiratory events are present within the analysis window, the sleep spectrogram could underestimate or overestimate either the narrow band or broad band component. Thus, the described technique is more likely to prove useful as an adjunct to, rather than a replacement for, standard polysomnography, providing phenotypic information in certain circumstances with greater accuracy than otherwise possible by visual event-based scoring. Our preliminary assessment of the value of the sleep spectrogram in predicting positive airway pressure failure is limited by the stringent patient selection; its generalizability to an unselected sleep laboratory population requires testing. Moreover, the ability of the spectrographic technique to predict long-term clinical outcome is not unknown, nor can its accuracy in identifying complex sleep apnea in those with milder but clinically significant sleep apnea be inferred from our data.
In summary, a spectrographic assessment of cardiopulmonary coupling using a single-lead ECG-based technique helps to differentiate sleep apnea phenotypes (pure obstructive vs. central or complex) that may usefully complement conventional approaches. Such differences may be evident on the diagnostic polysomnogram, prior to the initiation of positive airway pressure therapy. Detecting a very distinct ECG-based spectrographic pattern of e-LFC with a narrow-band profile may facilitate the identification of disorders of respiratory control during sleep. The technique seems to hold promise in predicting failure of conventional positive airway pressure titration.
ACKNOWLEDGMENTS
Grants from the National Institutes of Health Heart Lung and Blood Institute (R21HL079248) and the National Institute of Biomedical Imaging and Bioengineering/National Institute of General Medical Sciences (U01EB008577), the James S. McDonnell Foundation, the G. Harold and Leila Y. Mathers Foundation, the Defense Advanced Research Projects Agency, and an unrestricted grant from the Periodic Breathing Foundation
The authors thank Sleep Heart Health Study for access to the original raw data and relevant study covariates. This paper represents the work of the authors and not the SHHS. The opinions expressed in this paper are those of the authors and do not necessarily reflect the views of the Indian Health Service.
Footnotes
Disclosure Statement
This was not an industry supported study. Dr. Thomas has consulted for Total Sleep Holdings; has a submitted patent for CO2 adjunctive therapy for complex sleep apnea, ECG-based method to assess sleep stability and phenotype sleep apnea; and has financial interests in SomRx. Dr. Mietus has financial interests in DynaDx Corp. Dr. Peng has financial interests in DynaDx Corp. Dr. Daly has financial interests in Total Sleep Holdings and The Periodic Breathing Foundation, LLC. Dr. Goldberger is a co-author on a US patient application that describes the ECG-based spectrographic method for analyzing sleep stability states employed in this study. The other authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 2.Hosselet JJ, Norman RG, Ayappa I, Rapoport DM. Detection of flow limitation with a nasal cannula/pressure transducer system. Am J Respir Crit Care Med. 1998;157:1461–7. doi: 10.1164/ajrccm.157.5.9708008. [DOI] [PubMed] [Google Scholar]
- 3.Badr MS. Central sleep apnea. Prim Care. 2005;32:361–74. doi: 10.1016/j.pop.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Onal E, Burrows DL, Hart RH, Lopata M. Induction of periodic breathing during sleep causes upper airway obstruction in humans. J Appl Physiol. 1986;61:1438–43. doi: 10.1152/jappl.1986.61.4.1438. [DOI] [PubMed] [Google Scholar]
- 5.Badr MS, Toiber F, Skatrud JB, Dempsey J. Pharyngeal narrowing/occlusion during central sleep apnea. J Appl Physiol. 1995;78:1806–15. doi: 10.1152/jappl.1995.78.5.1806. [DOI] [PubMed] [Google Scholar]
- 6.Thomas RJ, Terzano MG, Parrino L, Weiss JW. Obstructive sleep-disordered breathing with a dominant cyclic alternating pattern--a recognizable polysomnographic variant with practical clinical implications. Sleep. 2004;27:229–34. doi: 10.1093/sleep/27.2.229. [DOI] [PubMed] [Google Scholar]
- 7.Gilmartin GS, Daly RW, Thomas RJ. Recognition and management of complex sleep-disordered breathing. Curr Opin Pulm Med. 2005;11:485–93. doi: 10.1097/01.mcp.0000183061.98665.b0. [DOI] [PubMed] [Google Scholar]
- 8.Morgenthaler TI KV, Hanak V, Decker PA. Complex sleep apnea syndrome: is it a unique clinical syndrome? Sleep. 2006;29:1203–9. doi: 10.1093/sleep/29.9.1203. [DOI] [PubMed] [Google Scholar]
- 9.Leung RS, Bradley TD. Respiratory modulation of heart rate and blood pressure during Cheyne-Stokes respiration. J Electrocardiol. 2003;36:213–7. doi: 10.1016/j.jelectrocard.2003.09.062. [DOI] [PubMed] [Google Scholar]
- 10.Leung RS, Floras JS, Lorenzi-Filho G, Rankin F, Picton P, Bradley TD. Influence of Cheyne-Stokes respiration on cardiovascular oscillations in heart failure. Am J Respir Crit Care Med. 2003;167:1534–9. doi: 10.1164/rccm.200208-793OC. [DOI] [PubMed] [Google Scholar]
- 11.Lorenzi-Filho G, Dajani HR, Leung RS, Floras JS, Bradley TD. Entrainment of blood pressure and heart rate oscillations by periodic breathing. Am J Respir Crit Care Med. 1999;159:1147–54. doi: 10.1164/ajrccm.159.4.9806081. [DOI] [PubMed] [Google Scholar]
- 12.Thomas RJ, Mietus JE, Peng CK, Goldberger AL. An electrocardiogram-based technique to assess cardiopulmonary coupling during sleep. Sleep. 2005;28:1151–61. doi: 10.1093/sleep/28.9.1151. [DOI] [PubMed] [Google Scholar]
- 13.Ryan CM, Bradley TD. Pathogenesis of obstructive sleep apnea. J Appl Physiol. 2005;99:2440–50. doi: 10.1152/japplphysiol.00772.2005. [DOI] [PubMed] [Google Scholar]
- 14.Hall MJ, Xie A, Rutherford R, Ando S, Floras JS, Bradley TD. Cycle length of periodic breathing in patients with and without heart failure. Am J Respir Crit Care Med. 1996;154:376–81. doi: 10.1164/ajrccm.154.2.8756809. [DOI] [PubMed] [Google Scholar]
- 15.Ryan CM, Bradley TD. Periodicity of obstructive sleep apnea in patients with and without heart failure. Chest. 2005;127:536–42. doi: 10.1378/chest.127.2.536. [DOI] [PubMed] [Google Scholar]
- 16.Tkacova R, Niroumand M, Lorenzi-Filho G, Bradley TD. Overnight shift from obstructive to central apneas in patients with heart failure: role of PCO2 and circulatory delay. Circulation. 2001;103:238–43. doi: 10.1161/01.cir.103.2.238. [DOI] [PubMed] [Google Scholar]
- 17.Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. Sleep. 1997;20:1077–85. [PubMed] [Google Scholar]
- 18.Redline S, Sanders MH, Lind BK, et al. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep Heart Health Research Group. Sleep. 1998;21:759–67. [PubMed] [Google Scholar]
- 19.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 20.Rechtschaffen A, Kales A. A manual of standardized terminology, techniques, and scoring system for the sleep stages of human subjects. Los Angeles: UCLA BIS/BRI Publications; 1968. [DOI] [PubMed] [Google Scholar]
- 21.EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep. 1992;15:173–84. [PubMed] [Google Scholar]
- 22.Terzano MG, Parrino L, Smerieri A, et al. Atlas, rules, and recording techniques for the scoring of cyclic alternating pattern (CAP) in human sleep. Sleep Med. 2002;3:187–99. doi: 10.1016/s1389-9457(02)00003-5. [DOI] [PubMed] [Google Scholar]
- 23.Terzano MG, Parrino L. Origin and significance of the cyclic alternating pattern (CAP) Sleep Med Rev. 2000;4:101–23. doi: 10.1053/smrv.1999.0083. [DOI] [PubMed] [Google Scholar]
- 24.Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med. 1999;160:1101–6. doi: 10.1164/ajrccm.160.4.9903020. [DOI] [PubMed] [Google Scholar]
- 25.Wellman A, Jordan AS, Malhotra A, et al. Ventilatory control and airway anatomy in obstructive sleep apnea. Am J Respir Crit Care Med. 2004;170:1225–32. doi: 10.1164/rccm.200404-510OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Younes M. Contributions of upper airway mechanics and control mechanisms to severity of obstructive apnea. Am J Respir Crit Care Med. 2003;168:645–58. doi: 10.1164/rccm.200302-201OC. [DOI] [PubMed] [Google Scholar]
- 27.Younes M, Ostrowski M, Thompson W, Leslie C, Shewchuk W. Chemical control stability in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 2001;163:1181–90. doi: 10.1164/ajrccm.163.5.2007013. [DOI] [PubMed] [Google Scholar]
- 28.Kushida CA, Giacomini A, Lee MK, Guilleminault C, Dement WC. Technical protocol for the use of esophageal manometry in the diagnosis of sleep-related breathing disorders. Sleep Med. 2002;3:163–73. doi: 10.1016/s1389-9457(01)00143-5. [DOI] [PubMed] [Google Scholar]
- 29.Johnson KG, Johnson DC. Bilevel positive airway pressure worsens central apneas during sleep. Chest. 2005;128:2141–50. doi: 10.1378/chest.128.4.2141. [DOI] [PubMed] [Google Scholar]
- 30.Nopmaneejumruslers C, Kaneko Y, Hajek V, Zivanovic V, Bradley TD. Cheyne-Stokes respiration in stroke: relationship to hypocapnia and occult cardiac dysfunction. Am J Respir Crit Care Med. 2005;171:1048–52. doi: 10.1164/rccm.200411-1591OC. [DOI] [PubMed] [Google Scholar]
- 31.Bradley TD, Logan AG, Kimoff RJ, et al. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005;353:2025–33. doi: 10.1056/NEJMoa051001. [DOI] [PubMed] [Google Scholar]
- 32.Thomas RJ. Effect of added dead space to positive airway pressure for treatment of complex sleep-disordered breathing. Sleep Med. 2005;6:177–8. doi: 10.1016/j.sleep.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 33.Thomas RJ, Daly RW, Weiss JW. Low-concentration carbon dioxide is an effective adjunct to positive airway pressure in the treatment of refractory mixed central and obstructive sleep-disordered breathing. Sleep. 2005;28:69–77. doi: 10.1093/sleep/28.1.69. [DOI] [PubMed] [Google Scholar]
- 34.Szollosi I, O'Driscoll DM, Dayer MJ, Coats AJ, Morrell MJ, Simonds AK. Adaptive servo-ventilation and deadspace: effects on central sleep apnoea. J Sleep Res. 2006;15:199–205. doi: 10.1111/j.1365-2869.2006.00515.x. [DOI] [PubMed] [Google Scholar]



