Abstract
Study Objective:
To test the effects of coffee and napping on nocturnal driving in young and middle-aged participants.
Design:
A cup of coffee (200 mg of caffeine), a placebo (decaffeinated coffee, 15 mg of caffeine), or a 30-minute nap were tested. Participants drove 125 highway miles between 18:00 and 19:30 and between 02:00 and 03:30 after coffee, placebo, or a nap.
Setting:
Sleep laboratory and open French highway.
Participants:
Twelve young (range, 20–25 years) and 12 middle-aged participants (range, 40–50 years).
Measurements:
Inappropriate line crossings, self-perceived fatigue and sleepiness, and polysomnographic recordings were analyzed.
Results:
Compared to daytime, after placebo the number of inappropriate line crossings was significantly increased (2 versus 73 for young participants, P < 0.01 and 0 versus 76 for the middle-aged participants, P < 0.05). Both coffee and napping reduced the risk of inappropriate line crossings, compared with placebo, in young participants (respectively, by three-quarters, incidence rate ratios [IRR] = 0.26 95% confidence interval [CI], 0.09–0.74, P < 0.05 and by two thirds, IRR = 0.34 95% CI, 0.20–0.58, P < 0.001) and in middle-aged participants (respectively by nine tenths, IRR = 0.11 95% CI, 0.05–0.21, P < 0.001 and by one fifth, IRR = 0.77 95% CI, 0.63–0.95, P < 0.05). A significant interaction between age and condition (IRR = 2.27 95% CI, 1.28–4.16 P < 0.01) showed that napping led to fewer inappropriate line crossings in younger participants than in middle-aged participants. During napping, young participants slept more (P < 0.01) and had more delta sleep (P < 0.05) than middle-aged participants.
Self-perceived sleepiness and fatigue did not differ in both age groups, but coffee improved sleepiness (P < 0.05), whereas napping did not.
Conclusions:
Coffee significantly improves performance in young and middle-aged participants. Napping is more efficient in younger than in older participants. Countermeasures to sleepiness should be adapted according to the age of drivers.
Citation:
Sagaspe P; Taillard J; Chaumet G; Moore N; Bioulac B; Philip P. Aging and nocturnal driving: better with coffee or a nap? a randomized study. SLEEP 2007;30(12):1808-1813.
Keywords: Night driving, coffee, age, sleepiness, countermeasures, prevention, road accidents
INTRODUCTION
DAYTIME SLEEPINESS IS WIDESPREAD AND HAS A NEGATIVE IMPACT ON EVERYDAY LIFE.1 UP TO 20% OF ALL TRAFFIC ACCIDENTS IN INDUSTRIAL SOCIETIES ARE sleep related.2–4 Connor et al3 have shown that driving between 02:00 and 05:00 multiplies by 5.6 the risk of traffic accidents. Despite this, many people persistently repeat this dangerous behavior because of financial reasons in professional drivers5 or sociocultural factors.6,7 Traffic accidents at work or during the trip from work to home are a major cause of injury and death among workers.8,9 Young medical residents are often victims of sleep-related traffic accidents10 and/or are involved in medical errors11 related to extensive hours of work associated with sleep deprivation. Young people are clearly overrepresented in sleep-related accidents,4,12,13 but the question of overexposure to the risk or increased vulnerability to sleep-related accidents has not yet been clarified.
Past studies have shown that young people are more vulnerable to sleep loss than are middle-aged people,14–16 but young people are also very exposed to sleep deprivation,7,10,17 which could explain the high percentage of young drivers involved in sleep-related accidents. Responsiveness to countermeasures to sleepiness at the wheel might also be different among age groups.
Such countermeasures include the use of awakening agents such as caffeine or napping. Caffeine is a widely used substance mainly consumed in coffee and similar beverages. It has been estimated that adults in western societies have an average all-source daily caffeine intake of about 200 to 300 mg18 and that these amounts increase with age.19 Within this dose range and at higher levels, caffeine increases alertness and acutely reduces sleep propensity. Napping is also a well-known countermeasure to combat fatigue, and countermeasures significantly improve nocturnal driving performances in young drivers.20
Because middle-aged people respond differently than young people to sleep deprivation,14,15,21 we decided to test the influence of age on the response to sleepiness countermeasures. To test this hypothesis, we designed a randomized, partially double-blinded, crossover study of the effects of coffee and napping in young and middle-aged participants on nighttime highway driving.
METHODS
Participants
Twenty-four participants, 12 young (range 20–25 years) and 12 middle-aged (range 40–50 years), were recruited. The research protocol was approved by the local ethics committee (consultative committee for the protection of persons participating in biomedical research [CCPPRB Bordeaux A]). All participants provided written informed consent.
Inclusion criteria required volunteers to be excluded if they reported excessive daytime sleepiness (Epworth Sleepiness Scale22 score > 9) or a sleep complaint such as sleep apnea or insomnia (Basic Nordic Sleep Questionnaire,23 items score < 4), if they were not intermediate in terms of morningness and eveningness according to the Horne-Ostberg questionnaire24 (score between 42 and 58), or if they showed evidence of psychopathology on the Symptom Check List25 (SCL-90R score>59).
A clinical interview with a sleep specialist was designed to exclude volunteers with sleep disorders or organic disorders affecting sleep, poor sleep hygiene or abnormal usual sleep patterns, night workers or shift-workers, and substance abusers (caffeine, drug, or alcohol).
Participants were moderate consumers of coffee (2–3 cups a day), and they denied using caffeine to restrict their usual sleep duration (no caffeine intake after 16:00).
Volunteers had to have 7 consecutive days of monitoring using actimeters (Actiwatch®, Cambridge Neurotechnology, UK)26 showing at least 85% mean sleep efficiency.27
Participants were not professional drivers, had had their driving license for at least 2 years, and drove between 10,000 and 20,000 km per year.
Study Design
This was a randomized controlled study with 2 double-blind conditions (coffee-placebo intake) and a napping condition. All participants performed 4 driving sessions: 1 baseline session from 18:00 to 19:30 (daytime condition) and 3 sessions from 02:00 to 03:30 (coffee, placebo, and nap conditions), with at least 1 week between sessions. All participants started on the daytime condition. The order of nocturnal driving sessions was randomly attributed to each participant in a balanced design by using a random permutations sequence. No stimulant of any kind was allowed during the study except for the scheduled caffeine condition.
Sleep Schedules and Sleep Recordings
Participants were instructed to maintain a regular sleep-wake schedule and were monitored by actimetry during the 3 days before each experimental session to verify the absence of sleep deprivation. Only the last night's sleep parameters are presented in the Results section. For the nocturnal testing periods, the participants came to the laboratory at 20:00 and were equipped with an ambulatory polysomnograph (Deltamed, Paris, France). They were not allowed to sleep before the driving sessions. Electroencephalography, electromyography, and electrooculography were recorded during the nap, the driving session, and the rest of the night after driving. After each driving session, all participants returned to the laboratory to be tested and to sleep in a research room. Sleep latency was calculated from the time of lights out to the first epoch of stage 1 sleep. Sleep efficiency was calculated by dividing time in bed by total sleep time from lights out to lights on.
Polysomnography
Two electroencephalograms (C3/A2, O2/A1), 1 electromyogram, 2 electrooculograms, and 1 electrocardiogram were recorded during the nap and the night after driving (Trackit, Deltamed France). Signals were digitized at a sampling rate of 256 Hz and filtered with a digital filter at a cutoff frequency of 35 Hz.
Data were manually analyzed (Coherence, Deltamed, France) by an experienced sleep technician (blinded to participants' condition) in 30-second epochs according to Rechtschaffen and Kales' recommendations.28 Non-rapid eye movement (NREM) sleep (stages 2, 3, and 4) during the first hour of sleep was retained for spectral analysis. Electroencephalographic signals of C3/A2 derivation were subjected to analysis by fast Fourier transformation (Coherence). Power spectra were computed for consecutive 2-second epochs, providing a frequency resolution of 0.5 Hz. The delta frequency band (0.5–4.5 Hz) was exploited.
Napping
During the naps, the driver's seat was fully reclined, the participants were covered with a blanket, and an electrical heating system was installed in the car to maintain a constant temperature (19°C). The car was parked in a quiet rest area and guarded by the copilot in order that nobody disturbed the drivers. The 30-minute nap started at 01:00, 1 hour before the driving session. We selected the nap duration according to epidemiologic data7,17 showing that the mean usual duration of stops for freeway drivers is around 30 minutes.
Coffee and Placebo
Coffee and placebo were prepared from single packs of the relevant instant coffee (normal or decaffeinated) provided by Nestlé (Nestlé, Noisiel, France). Coffee contained 4.25% caffeine and placebo (decaffeinated coffee) contained less than 0.3% caffeine. Placebo and coffee were not distinguishable by taste or appearance.
Each participant drank 125 ml of coffee (about half a cup of coffee, containing 200 mg of caffeine) or 125 ml of placebo (containing 15 mg of caffeine) 30 minutes before the nighttime driving session.
Driving Sessions
All participants drove 200 km (125 miles) on the same 2-lane highway (100 km [62.5 miles]) 1 way and 100 km the other way) for all conditions.
The nighttime driving session started 30 minutes after ingestion of coffee or placebo or 30 minutes after awakening from the nap.
Driving conditions were a straight highway on weekdays with usually light traffic conditions, in fair weather. All drivers were exposed to the same or very similar conditions. During a training session, participants were instructed to maintain a constant speed (130 kph [80 mph]), to drive in the center of the lane, and not to cross the painted lines separating the lanes except to pass a slower vehicle.
During the whole experiment, a professional driving instructor monitored the driving speed and noted the number of line crossings. He was ready to take control of the car (equipped with dual controls) if needed. If a participant could no longer drive during a session, he was driven back to the rest area. The car used for the experiment was equipped with a video camera that filmed and recorded the road, as has been described elsewhere.20,29–31
After driving, participants returned to the laboratory to sleep as long as they wished.
Sleepiness and Fatigue
Back in the laboratory (04:15), participants were asked to rate their sleepiness on the Karolinska Sleepiness Scale (a 9-point scale from 1 = “extremely alert” to 9 = “very sleepy, great effort to keep alert, fighting sleep”) and their instantaneous fatigue (“describe how fatigued you are now” on a 100-mm visual analogue scale from 0 “not at all tired” to 100 “very tired”).
Outcome Measures
The main outcome measure was the number of inappropriate line crossings (ILC) identified from the video recordings. This measure was selected because epidemiologic findings have shown that 65% of sleep-related accidents occur after an ILC.32 Several studies have also shown that impaired daytime alertness induces lateral deviations during driving33–35 and that sleep-related accidents frequently occur with a single car driving off the road and hitting an obstacle with no reaction from the driver.13, 32 We have also demonstrated that the number of ILCs is affected by sleep deprivation29, 30 and improved by classic countermeasures to sleep loss.20
An ILC was recorded when the car crossed a lateral highway lane marker, as evidenced by video-recording analysis. Exceptions were overtaking maneuvers or some other necessary driving action, as recorded by the driving instructor. Driving-instructor and video-recording timelines were synchronized at the beginning of each session. Deviations related to traffic interference were excluded so as to concentrate on line crossings related to driver status. The scorer of video recordings was blind to the driving condition.
Our secondary outcome measures were self-rated sleepiness and fatigue and sleep parameters during the subsequent sleep.
Statistical Analysis
The results were analyzed by using negative binomial regression in Stata, version 8.0 (Stata Corp., College Station, Texas), using number of ILC per participant as dependent variables and conditions (daytime, coffee, placebo, or nap) and age as determinants clustered on participants. We reported comparisons of ILC between conditions as incidence rate ratios (IRR) with 95% confidence intervals (CI). Where binomial negative regression was not possible because there was no line crossing, the Wilcoxon nonparametric test was used.
The effects of age and driving conditions on sleepiness and fatigue were evaluated by analyses of variance for repeated measurements (ANOVAs). Actimetric data were evaluated by ANOVAs. The effect of age on nap sleep parameters was evaluated by a 1-way ANOVA. To correct for sphericity, all P values derived from ANOVA were based on Huynh-Feldt corrected degrees of freedom.
Nocturnal sleep parameters assessed with polysomnography were analyzed with nonparametric paired tests. Results for sleep parameters are reported as means and standard deviations.
RESULTS
The results on the young group of subjects have been previously published in a recent article.20 We report here the results of young and middle-aged participants and the difference between the groups.
Performance
Line Crossings
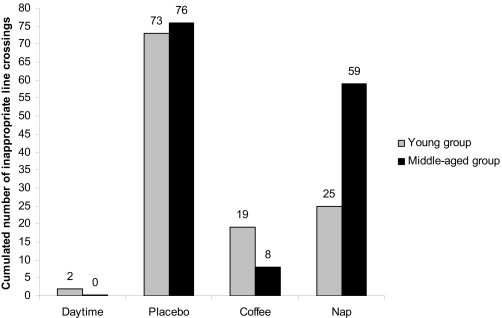
Compared to daytime, after placebo the number of ILCs was significantly increased in young participants (2 vs 73, Wilcoxon test, Z = −2.814, P < 0.01) and in middle-aged participants (0 vs 76, Wilcoxon test, Z = −2.232, P < 0.05). No interaction between age and condition was found (IRR = 2.08; 95% CI, 0.14–29.2, NS) (Figure 1), both age groups being similarly affected by extended wakefulness. After placebo, 9 out of 12 (75%) of the middle-aged participants had a driving performance comparable to that in the daytime condition (0 or 1 line crossing) but only 3 out of 12 (25%) of the young did (χ2 (8) = 15.75, P < 0.05).
Figure 1.
Cumulative number of inappropriate line crossings across all participants in young and middle-aged groups in all driving conditions.
After caffeinated coffee, the risk of ILC compared to placebo was reduced by three-quarters (IRR = 0.26 95% CI, 0.09–0.74, P < 0.05) in young participants and by nine-tenths (IRR = 0.11 95% CI, 0.05–0.21, P < 0.001) in middle-aged participants. No interaction between age and condition was found (IRR = 0.4 95% CI, 0.11–1.41, NS). Nine subjects in the young group had a driving performance comparable to that in the daytime condition, and 10 did in the middle-aged group.
After napping, the risk of ILC compared to placebo was reduced by two-thirds (IRR = 0.34 95% CI, 0.2–0.58, P < 0.001) in young participants and by one-fifth (IRR = 0.77 95% CI, 0.63–0.95, P < 0.05) in middle-aged participants. However, an interaction between age and condition (IRR = 2.27 95% CI, 1.28–4.16, P < 0.01) showed that napping led to fewer ILC in younger participants than in middle-aged participants (Figure 1). Eight subjects out of 12 in both age groups had a driving performance comparable to that of the daytime condition.
Self-Perception of Sleepiness and Fatigue
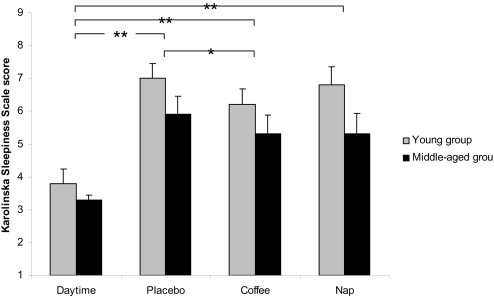
There was a significant increase in sleepiness as measured by Karolinska Sleepiness Scale scores among the conditions (Daytime < Coffee < Placebo = Nap) (respectively, ANOVA, F1–22 = 30.289 P < 0.001, F1–22 = 5.466, P < 0.05 and F1–22 = 2.469, NS) (Figure 2). No effect of age (ANOVA, F1–22 = 2.939, NS) and no interaction of condition with age (ANOVA, F3–66 = 0.828, NS) were found (Figure 2).
Figure 2.
Self-perceived sleepiness (Karolinska Sleepiness Scale) in driving condition in young and middle-aged participants (Mean ± SE).
* P < 0.05
** P < 0.001
* and ** represent significant differences between Driving conditions. No effect of Age and no interaction Age x Driving condition were found.
There was a significant increase in fatigue (visual analogue scale) from the baseline condition to nocturnal conditions (Daytime [35 ±19] < Coffee [50 ±19] = Placebo [58 ±23] = Nap [58 ±19]) (respectively, ANOVA, F1–22 = 20.706 P < 0.001, F1–22 = 3.755, NS, and F1–22 = 0.034, NS). No effect of age (ANOVA, F1–22 = 0.386, NS) and no interaction of condition with age (ANOVA, F3–66 = 0.499, NS) were found.
Sleep Parameters
Actimetry
Sleep time did not differ during the night before the driving conditions (ANOVA, F3–66 = 1.101, NS) (Daytime [427 minutes ± 30.9; range 356–501 minutes], Placebo [442 minutes ± 31.7, range 373–536 minutes], Coffee [436 min ± 35.5, range 347–494 minutes], Nap [429 minutes ± 30.8, range 349–473]). No effect of age (ANOVA, F1–22 = 0.161, NS) (young participants [435 minutes ± 34.5] and middle-aged participants [432 minutes ± 30.3]) and no interaction of condition with age (ANOVA, F3–66 = 0.347, NS) were found.
Polysomnography
Nap
Sleep duration was shorter in middle-aged participants than in young ones (14 ± 9 versus 22 ± 4 minutes, ANOVA, F1–22 = 9.942, P < 0.01). Young participants had higher power in the delta frequency band (259 ± 216.2 versus 99.6 ± 57.6 μV2/Hz, ANOVA, F1–22 = 6.101, P < 0.05) than middle-aged participants.
Nocturnal Sleep
Back in the lab after driving, sleep latencies were slightly increased by coffee, compared with placebo, for both groups (2.54 ± 1.7 vs 1.71 ± 1.6 minutes, Wilcoxon test, Z = −1.976, P < 0.05 for young group and 6.08 ± 3.4 vs 4.58 ± 1.9 minutes, Wilcoxon test, Z = −2.059, P < 0.05 for middle-aged group). Sleep efficiency were not modified by coffee, compared with placebo, for both age groups (respectively, Wilcoxon test, Z = −1.490, NS for young group, and Z = −1.883, NS for middle-aged group).
For the nap condition, neither sleep latency nor sleep efficiency differed between the young and middle-aged groups (3.1± 3 vs 5.5 ± 7 minutes, ANOVA, F1–22 = 1.196, NS, and 94% vs 92%, F1–22 = 1.177, NS).
There was no difference between sleep latencies and sleep efficiency in placebo versus nap conditions (3.15 ± 2.3 vs 4.37 ± 5.4 minutes, Wilcoxon test, Z = −0.921, NS and 93% ± 5.4 vs 92% ± 5.2, Wilcoxon test, Z = −1.186, NS).
DISCUSSION
Our first analysis (odds ratio on cumulative data) showed that both age groups were affected by sleep deprivation. Previous studies14,15,21 have shown that middle-aged people are less vulnerable to sleep deprivation than young people (i.e., older subjects have worse baseline performances than younger subjects but their proportional performance decrement under sleep deprivation is lower). Our findings could appear contradictory with the results of the above-mentioned studies, but they are clearly explained by the large interindividual variability in both groups. Indeed, the proportion of resilient subjects was higher in the middle-aged group (9 out of 12) than in the young group (3 out of 12), which confirms the protective effect of age against sleep deprivation. Because we carefully controlled sleep duration before each driving session and since each driver had an identical total sleep time, this age-related interindividual variability cannot be explained by previous sleep deprivation or differences in total sleep duration between age groups.
A recent study15 demonstrated that a reduced circadian regulation with age rather than reduced sleep pressure (homeostatic regulation) was implicated in this age-related vulnerability, but no robust conclusions can be made about the reasons why 3 subjects out of 12 in the middle-aged group did not maintain their nocturnal performance. Only 2 studies36,37 have considered circadian and homeostatic predictors to explain interindividual vulnerability to sleep deprivation, but the physiologic predictors still remain unknown.
Caffeine improves driving performance in both young and middle-aged participants. Aging does not reduce the effectiveness of the response to caffeine. Therefore, caffeine does not seem to operate only on homeostatic or circadian components.
During the nap condition, younger drivers improved their performances much more than did middle-aged ones. Younger participants slept longer and more deeply than middle-aged ones and may have benefited from more restored functions, as previous authors have shown in past studies.38,39
Sleep pressure is known to decrease with age. Since the middle-aged participants slept less during napping than the young participants, the homeostatic drive of the middle-aged participants might be lower than that of the young ones, which would explain why brief nocturnal sleep is less restorative in this age group. Young subjects also had deeper sleep (i.e., more delta band activity), which could also explain why their naps were more restorative. Studies have explored the relationship between sleep pressure and performances according to age, using both the ability to sleep during a nap and a measure of sleep pressure during wake time (i.e., alpha theta band on the electroencephalogram during wake). Buysse et al40 have shown that older adults have a lower level and smaller circadian variations in sleep propensity, as compared with younger adults, whereas psychomotor performance rhythms tend to show increased circadian variation among the elderly.
Fatigue and sleepiness were both increased during the nocturnal conditions, but only coffee improved subjective sleepiness. This could be due to the fact that caffeine acts on alerting systems, whereas napping tends to decrease sleep pressure. This differential mode of action would imply that self-perception of sleepiness is more related to the activity of waking systems than to sleep drive. Fatigue was unresponsive to coffee or napping, which proves that this symptom is less affected by the wake or sleep drive than is self-perception of sleepiness.
In conclusion, the potential effect of age on response to sleepiness countermeasures should be considered in populations exposed to extended wakefulness. According to their age or individual physiology, subjects should implement their best countermeasures to sleepiness at the wheel.
ACKNOWLEDGMENTS
We thank the following clinical research assistants: C. Valtat for selecting participants, collecting and monitoring data and for administrative, technical, and logistic support; and V. Bibène for collecting data and data monitoring. Special thanks to Autoroutes du Sud de la France for allowing us to use their highways for our research, to Nestlé for providing normal and decaffeinated coffee, to M. Moessinger, H. Guillemot (LAB) for helping us in the administrative coordination of the project and to T. Spector and C. Gilbert for managing the GO 3 group (PREDIT). This research was supported by a grant (PREDIT GO3) from the French Ministry of Research and LAB (PSA Peugeot Citroën and Renault).
Footnotes
Disclosure Statement
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Ohayon MM, Caulet M, Philip P, Guilleminault C, Priest RG. How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med. 1997;157:2645–52. [PubMed] [Google Scholar]
- 2.Philip P, Vervialle F, Le Breton P, Taillard J, Horne JA. Fatigue, alcohol, and serious road crashes in France: factorial study of national data. BMJ. 2001;322:829–30. doi: 10.1136/bmj.322.7290.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Connor J, Norton R, Ameratunga S, et al. Driver sleepiness and risk of serious injury to car occupants: population based case control study. BMJ. 2002;324:1125. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horne JA, Reyner LA. Sleep related vehicle accidents. BMJ. 1995;310:565–7. doi: 10.1136/bmj.310.6979.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnold PK, Hartley LR, Corry A, Hochstadt D, Penna F, Feyer AM. Hours of work, and perceptions of fatigue among truck drivers. Accid Anal Prev. 1997;29:471–7. doi: 10.1016/s0001-4575(97)00026-2. [DOI] [PubMed] [Google Scholar]
- 6.Philip P, Taillard J, Quera-Salva MA, Bioulac B, Akerstedt T. Simple reaction time, duration of driving and sleep deprivation in young versus old automobile drivers. J Sleep Res. 1999;8:9–14. doi: 10.1046/j.1365-2869.1999.00127.x. [DOI] [PubMed] [Google Scholar]
- 7.Philip P, Ghorayeb I, Stoohs R, et al. Determinants of sleepiness in automobile drivers. J Psychosom Res. 1996;41:279–88. doi: 10.1016/0022-3999(96)00127-4. [DOI] [PubMed] [Google Scholar]
- 8.Personick M, Mushinski M. Highway fatalities: leading cause of work-related deaths. Stat Bull Metrop Insur Co. 1997;78:19–25. [PubMed] [Google Scholar]
- 9.Harrison JE, Mandryk JA, Frommer MS. Work-related road fatalities in Australia, 1982–1984. Accid Anal Prev. 1993;25:443–51. doi: 10.1016/0001-4575(93)90073-6. [DOI] [PubMed] [Google Scholar]
- 10.Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125–34. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 11.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 12.Horne JA, Reyner LA. Vehicle accidents related to sleep: a review. Occupational and Environmental Medicine. 1999;56:289–294. doi: 10.1136/oem.56.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pack AI, Pack AM, Rodgman E, Cucchiara A, Dinges DF, Schwab CW. Characteristics of crashes attributed to the driver having fallen asleep. Accid Anal Prev. 1995;27:769–75. doi: 10.1016/0001-4575(95)00034-8. [DOI] [PubMed] [Google Scholar]
- 14.Philip P, Taillard J, Sagaspe P, et al. Age, performance and sleep deprivation. J Sleep Res. 2004;13:105–10. doi: 10.1111/j.1365-2869.2004.00399.x. [DOI] [PubMed] [Google Scholar]
- 15.Blatter K, Graw P, Munch M, Knoblauch V, Wirz-Justice A, Cajochen C. Gender and age differences in psychomotor vigilance performance under differential sleep pressure conditions. Behav Brain Res. 2006;168:312–7. doi: 10.1016/j.bbr.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 16.Bliese PD, Wesensten NJ, Balkin TJ. Age and individual variability in performance during sleep restriction. J Sleep Res. 2006;15:376–85. doi: 10.1111/j.1365-2869.2006.00557.x. [DOI] [PubMed] [Google Scholar]
- 17.Philip P, Taillard J, Guilleminault C, Quera Salva MA, Bioulac B, Ohayon M. Long distance driving and self-induced sleep deprivation among automobile drivers. Sleep. 1999;22:475–80. doi: 10.1093/sleep/22.4.475. [DOI] [PubMed] [Google Scholar]
- 18.D'Amicis A, Viani R. The consumption of coffee. In: Garattini S, editor. Caffeine, Coffee and Health. New York: Raven Press; 1993. pp. 1–16. [Google Scholar]
- 19.Sanchez-Ortuno M, Moore N, et al. Sleep duration and caffeine consumption in a French middle-aged working population. Sleep Med. 2005;6:247–51. doi: 10.1016/j.sleep.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Philip P, Taillard J, Moore N, et al. The effects of coffee and napping on nighttime highway driving: a randomized trial. Ann Intern Med. 2006;144:785–91. doi: 10.7326/0003-4819-144-11-200606060-00004. [DOI] [PubMed] [Google Scholar]
- 21.Adam M, Retey JV, Khatami R, Landolt HP. Age-related changes in the time course of vigilant attention during 40 hours without sleep in men. Sleep. 2006;29:55–7. doi: 10.1093/sleep/29.1.55. [DOI] [PubMed] [Google Scholar]
- 22.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 23.Partinen M, Gislason T. Basic Nordic Sleep Questionnaire (BNSQ): a quantitated measure of subjective sleep complaints. J Sleep Res. 1995;4:150–155. doi: 10.1111/j.1365-2869.1995.tb00205.x. [DOI] [PubMed] [Google Scholar]
- 24.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 25.Derogatis L. SCL-90-R: Administration, Scoring and Procedure. Minneapolis: Manual National Computer Systems; 1994. [Google Scholar]
- 26.Delafosse JY, Leger D, Quera-Salva MA, Samson O, Adrien J. Comparative study of actigraphy and ambulatory polysomnography in the assessment of adaptation to night shift work in nurses. Rev Neurol (Paris) 2000;156:641–5. [PubMed] [Google Scholar]
- 27.Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001;2:389–96. doi: 10.1016/s1389-9457(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 28.Rechtschaffen A, Kales A. Bethesda: US Department of Health, Education and Welfare, Public Health Service; 1968. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. [Google Scholar]
- 29.Philip P, Sagaspe P, Taillard J, et al. Fatigue, sleepiness, and performance in simulated versus real driving conditions. Sleep. 2005;28:1511–6. doi: 10.1093/sleep/28.12.1511. [DOI] [PubMed] [Google Scholar]
- 30.Philip P, Sagaspe P, Moore N, et al. Fatigue, sleep restriction and driving performance. Accid Anal Prev. 2005;37:473–8. doi: 10.1016/j.aap.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 31.Philip P, Taillard J, Klein E, et al. Effect of fatigue on performance measured by a driving simulator in automobile drivers. J Psychosom Res. 2003;55:197–200. doi: 10.1016/s0022-3999(02)00496-8. [DOI] [PubMed] [Google Scholar]
- 32.Sagberg F. Road accidents caused by drivers falling asleep. Accid Anal Prev. 1999;31:639–49. doi: 10.1016/s0001-4575(99)00023-8. [DOI] [PubMed] [Google Scholar]
- 33.Ramaekers JG, O'Hanlon JF. Acrivastine, terfenadine and diphenhydramine effects on driving performance as a function of dose and time after dosing. Eur J Clin Pharmacol. 1994;47:261–6. doi: 10.1007/BF02570506. [DOI] [PubMed] [Google Scholar]
- 34.O'Hanlon JF, Vermeeren A, Uiterwijk MM, van Veggel LM, Swijgman HF. Anxiolytics' effects on the actual driving performance of patients and healthy volunteers in a standardized test. An integration of three studies. Neuropsychobiology. 1995;31:81–8. doi: 10.1159/000119177. [DOI] [PubMed] [Google Scholar]
- 35.O'Hanlon JF, Volkerts ER. Hypnotics and actual driving performance. Acta Psychiatr Scand Suppl. 1986;332:95–104. doi: 10.1111/j.1600-0447.1986.tb08985.x. [DOI] [PubMed] [Google Scholar]
- 36.Van Dongen HP, Baynard MD, Maislin G, Dinges DF. Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Sleep. 2004;27:423–33. [PubMed] [Google Scholar]
- 37.Taillard J, Philip P, Coste O, Sagaspe P, Bioulac B. The circadian and homeostatic modulation of sleep pressure during wakefulness differs between morning and evening chronotypes. J Sleep Res. 2003;12:275–82. doi: 10.1046/j.0962-1105.2003.00369.x. [DOI] [PubMed] [Google Scholar]
- 38.Mednick S, Nakayama K, Stickgold R. Sleep-dependent learning: a nap is as good as a night. Nat Neurosci. 2003;6:697–8. doi: 10.1038/nn1078. [DOI] [PubMed] [Google Scholar]
- 39.Huber R, Ghilardi MF, Massimini M, et al. Arm immobilization causes cortical plastic changes and locally decreases sleep slow wave activity. Nat Neurosci. 2006;9:1169–76. doi: 10.1038/nn1758. [DOI] [PubMed] [Google Scholar]
- 40.Buysse DJ, Monk TH, Carrier J, Begley A. Circadian patterns of sleep, sleepiness, and performance in older and younger adults. Sleep. 2005;28:1365–76. doi: 10.1093/sleep/28.11.1365. [DOI] [PubMed] [Google Scholar]