Abstract
Objective
The 17-item PCS was designed for priority-setting and queue management of children and adolescents referred for mental health services. Here we assess aspects of the validity of the Children’s Mental Health (CMH) Priority Criteria Score (PCS), developed by the Western Canada Waiting List Project (WCWL). The PCS was evaluated across clinical settings of increasing acuity and in terms of its relationship to two variables reflecting criteria-related validity and actual wait times.
Method
Intake workers completed PCS forms for 497 referrals enrolled for treatment in three clinical areas over approximately two fiscal years. The completion time of the PCS form was estimated in relation to the total referral and screening process. Intake workers completed the PCS items and did not use the total score at the time of intake and form completion to triage or place clients; hence, the PCS was independent of enrollment and placement within the continuum of care. Furthermore, clinicians in the receiving programs had to accept the triage decisions for the PCS to be used in the study analysis.
Results
The PCS score was meaningfully related to the measures of criteria-related validity (e.g., clinician perceived urgency, clinician perceived maximum acceptable waiting times) and triage to clinical settings of increasing acuity. There was a significant mean difference in the PCS for those accepted to community, day, or inpatient settings.
Conclusions
The PCS appears to be a useful, efficient measure of clinical urgency adequate for use in priority-setting for children waiting for mental health services.
Keywords: wait list management, prioritization, access
Résumé
Objectif général
Le Questionnaire de priorisation des critères (QPC) en 17 points a été conçu pour établir les priorités et gérer les listes d’attente des enfants et des adolescents reférés à des services de santé mentale. Cet article évalue le questionnaire de priorisation des critères en santé mentale pédiatrique mis au point dans le cadre du projet relatif aux listes d’attente dans l’Ouest canadien (WCWL). La validité des critères et le temps d’attente réel ont été évalués par le biais de cas cliniques plus ou moins graves.
Méthodologie
Les intervenants du service d’admission ont rempli un QPC pour les 497 patients référés – sur une durée d’environ deux ans - pour traitement dans trois secteurs cliniques. Le temps nécessaire pour remplir le questionnaire a été calculé en fonction du processus total de référence et de triage. Les intervenants ont rempli le questionnaire sans toutefois se baser sur la note obtenue pour trier ou placer les patients. Les patients ont été inscrits et placés dans le continuum de soins indépendamment des résultats du QPC. En outre, les médecins des programmes qui accueillaient les patients étaient tenus d’accepter les décisions en matière de triage.
Résultats
La note du QPC est liée de façon significative à la validité de critères comme l’urgence telle que la perçoit le clinicien, le délai maximum acceptable pour le clinicien et l’envoi des patients vers des unités cliniques de soins aigus, après le triage. On constate un écart moyen significatif dans la note selon que les patients sont admis dans des services communautaires, des unités de jour ou des hôpitaux.
Conclusions
Le QPC est un instrument utile et efficace de mesure de l’urgence clinique qui permet de prioriser les services de santé mentale pédiatrique.
Keywords: gestion des listes d’attente, priorisation, accès
Introduction
In the National Action Agenda for Children’s Mental Health, the U.S. Surgeon General warned that the nation is facing a public crisis in caring for children and adolescents with behavioral, psychological, and emotional problems (Department of Health and Human Services, 2001). It was estimated that almost 21 percent of U.S. children ages 9 to 17 had a diagnosable mental or addictive disorder that caused at least some impairment. Comparative data exist for Canada (Waddell et al., 2002). However, in any given year, less than one in five of these youth receives needed treatment (WHO, 2001). Unmet need in children’s mental health (CMH) is an apparent and substantial problem in the United States and Canada. Short of having adequate funding to meet basic need, services in Canada must find standard ways to prioritize patients’ urgency in order to appropriately ration services.
Data from the Great Smoky Mountains Study of Youth, a population-based study of psychopathology and mental health service use among children, show somewhat higher rates of mental health service use than has been reported previously, while continuing to show substantial unmet need, even among children with both a psychiatric diagnosis and functional impairment (Ezpeleta, Keeler, Erkanli, et al., 2001; Burns et al., 1995). Such findings are similar in Canada (Offord et al., 1987) and point to the need for a fair and transparent method of managing and improving access to mental health systems for children and adolescents.
Managing waiting lists for children’s mental health (CMH) services is a major concern in countries with publicly funded health care systems, given scarcity of resources and levels of unmet need. Although the estimated prevalence of psychiatric disorders in children and adolescents ranges across Canada from 3% with a debilitating mental problem to 20% that have a diagnosable mental problem, specialized CMH services reach only a minority of such individuals. Long waiting times interfere with timely interventions or are associated with non-attendance, whereby families simply “give up” and leave the waiting list. In many cases, children deteriorate to a more urgent state. Several methods have been attempted to better manage waiting lists for CMH services. Published work has included the use of multi-disciplinary teams, shorter consultation periods, reviewing the accuracy of the waiting list, appropriate allocation of referrals, and improving efficiency by intervening with non-attendance.
Assessments of urgency are often done by multi-disciplinary teams but there is little, if any, recognized standardization across programs. In one study of priority-setting for child and adolescent mental health problems by general practitioners, cases presenting with self-harm, child abuse, and those considered to be ‘unsafe’ were rated as the highest priority. Safety (imminent harm) is a criterion that would naturally distinguish lesser urgent from emergent cases. However, the need remains for brief, inexpensive assessment tools for priority-setting in children awaiting CMH services. Despite this, there have been few reports of standardized methods directed toward achieving this goal (Srebnik, Uehara, & Smukler, 1998).
Priority-setting based on perceived urgency is central to improving the fairness of wait list management, by ensuring that patients have timely and fair access to services according to need. The PCS for CMH is one of five tools developed by the Western Canada Waiting List Project to assess clinical urgency, and provides an explicit and transparent method for setting priorities among children and adolescents awaiting CMH services.
In preparation for full implementation, this field study examined aspects of the PCS validity. Validity is the degree to which the available evidence supports the interpretability and appropriateness of the PCS as a measure of patient urgency. For example, within the central intake system, skilled clinicians place referrals within the continuum of services available. Patients receiving inpatient referrals are more acutely and severely afflicted than those referred to ambulatory settings. If this assumption is supported in field-testing, the external validity of the CMH PCS is greatly enhanced, given that such testing involves real-world child and family clients (U.S. Public Health Service, 2000). Consequently, the questions and analyses that follow consider the urgency of adolescents along the continuum of practice in general psychiatry including community-based care, day treatment, and inpatient admission as a proxy for urgency.
The following research questions were considered:
-
Does the PCS map to placement within clinical settings which represent increasing urgency within the continuum of care? We hypothesized that those assigned to inpatient settings have higher PCSs than those in day or community settings.
Convergent validity is the ability of the PCS to relate appropriately to other measures that assess a similar construct. To study this aspect of validity, the PCS has included two independent items that estimate the construct of urgency and have been used to established the psychometric properties of the CMH-PCS based on paper cases. The following questions are also considered in this study:
Is there congruence between the PCS and the two other measures of urgency (VAS and MAWT), and actual wait times? We hypothesized that the MAWT, the VAS and actual wait time, like the PCS, are related to clinical setting and are similarly correlated with the PCS (Smith et al., 2002).
Does completion of the CMH-PCS contribute substantially to overall workload? We expected that the PCS form would have low respondent burden, taking little time overall to complete.
Method
This study received approval through the standard review process of Mental Health Quality Management Committee within the Calgary Health Region’s Department of Psychiatry and more recently through the Conjoint Ethics committee as part of larger study examining regional children’s mental health data (ID: E-18958).
Instrumentation
The PCS is a score derived from an instrument designed to prioritize referrals accepted for treatment in children’s mental health services. It is not a screening instrument. During the pilot phase of CMH-PCS development, the reliability of the criterion was assessed, based on clinicians’ ratings of ‘paper’ cases. One of the two items that independently measure criteria-related validity of the 17 item scale are included in the survey and originate from the original study. The Visual Analogue Scale of perceived urgency (VAS) and perceived Maximum Allowable Wait Time in days (MAWT) were of particular importance with regard to establishing the criteria-related validity of the PCS rating of the paper cases. The VAS urgency represents the clinician’s ‘gestalt’ or overall intuition about a case’s urgency, and the MAWT is what clinicians feel should be the outer bound of waiting time for such a case. Both of these variables are included in this study for the purpose of establishing the criteria-related validity of the WCWL-CMH-PCS score (weighted sum of items 1–17) completed in the field. The 17 item scale is less subject to bias as it is comprised of multiple and more objective items, nevertheless the VAS and MAWT directly tap urgency, the construct of interest. As in the pilot study, we anticipated that the PCS would be related to the VAS urgency, and to placement in the continuum of care. The PCS should also be related to clinician-estimated MAWT (weeks), as well as actual waiting times (Days).
The PCS (Table 1), developed by an expert clinical panel (Smith et al., 2002), consists of 17 standardized criteria that relate to the severity of mental or emotional disturbance, family and social factors, and estimates of the likely benefits of intervention. With the addition of the VAS, the 17 items making up the PCS represent the more detailed referral information used in screening, triage, and placement. Because these 17 items are based on a wide range of patient information, the assumption is the PCS is more comprehensive and objective and hence ‘fairer’ than an overall or ‘gestalt’ impression such as the VAS. The performance properties of the CMH-PCS have been described elsewhere (Smith et al., 2002: www.wcwl.ca). In this study, this previous work is extended by examining the internal consistency (coefficient alpha) and temporal stability of the PCS scale items, as tested in the field.
Table 1.
CMH-PCS form items2
| # | Item |
|---|---|
| 1 | Danger to self |
| 2 | Danger to Others |
| 3 | Psychotic Symptoms |
| 4 | Global age-appropriate developmental progress |
| 5 | Children’s GAF (CGAS) Global Assessment of Function Scale3 |
| 6 | Internalized Symptoms |
| 7 | Externalized Symptoms |
| 8 | Co-morbid medical conditions |
| 9 | Co-morbid psychiatric conditions |
| 10 | Harmful substance use/misuse |
| 11 | Significant biological family history of mental illness |
| 12 | School and/or work |
| 13 | Social/friendships/community functioning |
| 14 | Does the patient have problems in the context of the home? |
| 15 | Family functioning or factors affecting child |
| 16 | Prognosis without further intervention. Will the client remain the same, get better, or worse in your view without intervention? |
| 17 | Degree of likely benefit with further intervention |
| 18 | All things considered, how would you rate the urgency or relative priority of this patient? (Internal validity measure: VAS) |
| 19 | Estimate in weeks the length of time that you as a clinician feel that the client could wait for treatment. (Internal validity measure: MAWT) |
Complete form with scoring and weights available at www.wcwl.ca
Equivalent to DSM_IV-TR Axis V: GAF
Participants
Over approximately a 24-month period, intake workers for children’s mental health completed the WCWL PCS for 497 referred clients accepted for treatment by the child and adolescent regional access and intake system for the Calgary Health Region. About half the calls to central intake are redirected to community services; however, PCS forms are not completed for these callers. The study included patients referred to the central intake service and admitted (accepted by the staff of the service to which they were triaged), who also had PCS forms completed between April 2002 and April 2003. (Standard practice was that the PCS form was completed only for referrals that the intake workers considered eligible for treatment).
In addition to the 497 clients accepted into treatment, 58 were not accepted by the service level to which they were referred (about 10%), and were referred to other services. Acceptance of clients by the staff of the service level to which they were triaged constituted an independent assessment of the intake staff’s clinical judgment and therefore contributed to the validity of the findings, discussed below. Only those accepted for treatment were considered in the present study, which prevented an examination of the sensitivity and specificity of the PCS. Examining the utility of the PCS as a screening instrument was beyond the scope of this study.
Procedures
The intake workers were clinically trained and held professional licensure, possessing at least 5 years clinical experience in psychology, social work or nursing. The staff screened referrals and accepted approximately 50% for placement and treatment. They were instructed to complete the 17 item scale for those accepted into treatment, once sufficient information was gathered in the usual course of screening and intake. Staff did not view and were blind to the total PCS (weighted sum of items 1–17). Specifically, the PCS was not utilized to assign or order placement or enrollment. Accordingly, the PCS was not used to alter the normal clinical practice in placement services. The main purpose was to examine whether or not the PCS was meaningfully related to the field-based construct of urgency (clinical level), as well as the criteria-related items, VAS and MAWT. Hence, in addition to completing the individual PCS (items 1–17), intake workers were asked to rate the overall urgency of each case on a visual analogue scale from 0 (not urgent) to 100 (maximally urgent). Intake workers, based on their experience, also recorded a perceived maximum allowable wait time in weeks for each individual, an estimate of the maximum time that individuals should have to wait for treatment given their condition. The information used to complete the forms was a core component of the normal business practice of processing and documenting referrals. The VAS and MAWT were completed last. In order to be included in this study, which focused on the validity of the intake workers PCS scores, clients triaged in the above manner had to be accepted for treatment (deemed appropriate) in the level of service to which they were assigned.
Additional Data
The actual waiting times were calculated from the regional access and intake database, as the difference (days) from referral date to the date of enrolment in the assigned clinical setting (date of the first face-to-face treatment-related contact). Data were extracted from the regional access and intake system database of the Calgary Health Region in one query-linked spreadsheet which was stripped of unique identifiers and used only for purposes of analysis. Additionally, the time required to complete the PCS was estimated from analyzing recorded workload data.
Analyses
Each variable considered in the study was described by clinical setting. In Table 2, the key to interpreting the values of each cell are given under the variable label, such as sample size, mean, standard deviation. Multiple logistic regression analysis was also used to assess the relationship between the PCS and clinical setting as a field-based measure of construct validity, together with the items measuring criteria-related validity, including actual wait times, the VAS and the MAWT. Clinical setting variable included: clinical area (categorical: ambulatory-community (value 1); day treatment (value 2); and, inpatient treatment (value 3). Multiple logistic regression analysis addressed the main question of this paper: Does the PCS meaningfully discriminate placement within clinical settings, which represent increasing urgency within the continuum of care?
Table 2.
Descriptive Statistics and Pearson Product Moment Correlations (PPMC)
| Variable n=497 | Community n = 300 mean (std. dev.) | Day Treatment n = 60 mean (std. dev.) | Inpatient n = 137 mean (std. dev.) |
|---|---|---|---|
| PCS | 36.2 (12.2) | 45.8 (9.6) | 57.5 (12.4) |
| VAS (1–100) | 62.2 (17.0) | 72.6 (11.6) | 92.0 (11.9) |
| MAWT (Days) | 55.8 (34.6) | 30.1 (20.5) | 9.4 (17.7) |
| Actual Wait Times (days) | 96.2 (67.3) | 62.5 (45.1) | 20.9 (28.7) |
Results
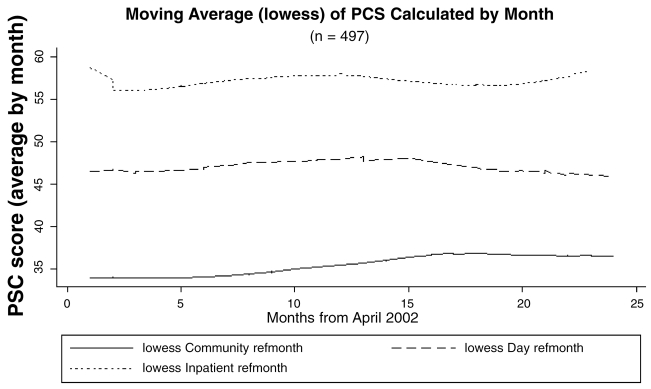
The PCS had mean values that were greater for those enrolled to the day treatment and inpatient clinical settings compared to community treatment settings. Mean values of the PCS tended to remain temporally stable, when averaged by month over the study period (Figure 1). The internal consistency of the PCS items was excellent (coefficient alpha = .76) indicating that the items were measuring a similar construct.
Figure 1.
Lowess curves of mean PCS scores calculated by month. Upper trace represents Inpatient, middle trace represents Day Treatment and lower trace represents community treatment settings, respectively. Figure reflects temporal stability of PCS in each clinical setting.
Table 2 provides a summary of the PCS and the other measured variables, in terms of the three levels of clinical placement that address the main research questions in descriptive terms.
The VAS, MAWT, and actual waiting times were related to the clinical settings in the same manner as the PCS with higher priority and lower estimated wait times in clinical settings accepting more urgent and severe cases (Table 2).
As well, in terms of Pearson Product Moment correlations, the VAS (r = .67), MAWT (r = −.58), and actual wait times (r = −.25) were related significantly with the PCS (p < .05). A multivariate model of main effects was developed in a multiple logistic regression analysis to determine the extent to which the PCS, actual wait times, VAS and MAWT discriminated between levels of treatment. The model, shown in Table 3, indicated that the PCS, more than the VAS and like the MAWT had a statistically significant relationship discriminating each clinical level. In practical terms, compared to admission in a community treatment setting, for every 10 point increase in the PCS, the likelihood of placement in Day or Inpatient settings increases 11 fold, respectively.
The PCS required between 2 and 4 minutes to complete electronically, after clinical information is gathered in the course of a normal screening and intake. A comprehensive referral, triage and enrollment usually required from 30–60 minutes to process (average 48 minutes) to the point of assigning a disposition.
Discussion
The purpose of the PCS is to provide a clinically acceptable and transparent method of priority-setting for those seeking CMH services. Currently, no such system is in place. This field study was specifically designed to examine the relationship of the PCS to specific clinical settings, known to differ in acuity and urgency. The results indicate the PCS to have convergent validity in terms of the observed statistical relationships with clinical setting and the other variables, actual wait times, MAWT and VAS. There are few who would disagree that inpatient settings tend to treat more severe and hence more urgent cases than ambulatory community settings. Importantly, the PCS was also related to actual waiting times for the clinical settings, which lays the groundwork for establishing standards. As well, the relationship of the PCS to the VAS and the MAWT provided evidence of criteria-related and concurrent validity of the PCS. While the relationship with VAS confirms previous findings (Smith et. al., 2002), the relationship of the PCS and placement in real clinical settings, as well as actual waiting times, independently validates the PCS construct as a measure of urgency and priority.
Moreover, the PCS appears to be completed consistently over time (Figure 1). Beyond global clinical judgment alone, the PCS appears to be a tool that may be used to assess urgency with some consistency, accuracy and fairness as a result of the PCS score reflecting the sum of 17 unique items reflecting different clinical and environmental components of the client’s profile. The results are in keeping with test theory, which holds that using more items to measure a construct more accurately assesses it.
Most relevant, the CMH PCS is meaningfully related to the level of clinical need, as represented by the relationship of PCS to clinical treatment settings. The PCS was also related to the measures of perceived urgency (VAS) and perceived waiting times (MAWT). Perceived urgency (VAS) is a global clinical judgment made by the clinician about each case, taking into account clinicians’ experience in weighing all other cases within the clinicians’ purview at the time of referral. The PCS was more accurate than the VAS in terms of discriminating between Day and Community treatment levels. Perceived MAWT is also based on clinicians’ experience and was as good as the PCS in discriminating clinical setting, although it lacks the more independent and richer clinical profile of the PCS. While these are important variables in establishing criterion-related validity, it follows that the PCS, being based on a number of items that are more concrete than a global impression, is a more objective and detailed indicator of urgency. Taken together, these findings indicate that the systematic collection and scaling of items, based on clinically relevant information that comprises the PCS, objectively and effectively measures urgency. The resulting PCS score may be used to establish priority.
The clinical implications of this study are that it is possible to use a tool such as the PCS to order patient information normally collected in the natural or usual course of screening and triage. This can occur in a way that is useful for prioritizing waiting lists for children’s mental health services. In terms of workload impact, priority scoring carries little burden for staff and yields data that are useful. A standard approach to priority-setting is not only fair, but it also offers the potential for developing and evaluating flow management strategies. The use of priority scores combined with other methods of waiting list management may facilitate optimal use of limited resources. Regrettably, there has been little or no evidence of the validity of prioritization methods. Once fully implemented, monitoring system fairness through using approaches, such as random case reviews and measurement audits, should be considered in order to more formally study the implications of prioritization and wait list management.
Prioritization of children waiting for mental health services is a complex multidimensional construct. In simple terms and at minimum, it could be said to consist of three components: pathophysiological severity, sociobehavioral impact, and potential to benefit. Urgency and severity do not have a straightforward relationship, per se. A case might be severe, yet not urgent, as in a chronic inalterable condition of known prognosis, for example disease states involving terminal malignancy. Similarly, a case might be urgent due to impact on usual role and life’s circumstances, yet not pathophysiologically severe, as is generally the rule with early interventions. We have anchored one cornerstone of this complex construct in measurement using the PCS. The results of this study have moved us closer to being able to prioritize referrals accepted for children’s mental health services and consider the exceptions that may appear to the rules as these are established and articulated. For example, the present study lays the groundwork for research into the more complex aspects of the effectiveness of wait list management interventions as a function of baseline urgency and severity as measured using the PCS. Potential indicators include the effect of urgency and severity on the need for services, length of stay and flow of particular case mixes.
Despite the fact that waiting times may be a significant barrier to accessing care, there is little understanding about the effects of waiting on children and families. In one study that followed up patients who were removed from the waiting list, 10% were re-referred within 2 years and had an average treatment time of 27 months, compared to 19 months for those kept on the waiting list. With the PCS, we are in a position to actively study the effect of waiting on a range of clinical and system level parameters.
The main limitation of the study is the small sample size in the day treatment setting (n = 60) and the narrow age range (13–19 years). Expanding the scope and duration of the study will address these issues directly. In conclusion, our results support the PCS as a measure of urgency for priority-setting and queue management of children and adolescents awaiting CMH services. As priority-setting tools are implemented, monitoring and evaluation are needed to assess their reliability, validity, stability and utility in clinical practice. Given the strong indication that the PCS is a valid measure of urgency, a manual has been developed to standardize training. Also, we have embarked on a study of the cross-cultural validity of the PCS, in terms of its utility in prioritizing referrals of patients that speak different languages. To this end we have implemented a pilot project in partnership with a clinic in Germany.1
Table 3.
Multiple Logistic Regression Model describing PCS ability to discriminate between community, day and inpatient treatment.
| Multiple Logistic Regression Model, n = 497, Pseudo R square = .42 | |||
|---|---|---|---|
| Model Chi Square = 362.7, d.f. = 6, p < 0.0001 | |||
| ‘Community’ is comparison group | OR (std err.) | p < | |
| Day | |||
| PCS | 1.1 (.02) | .004 | |
| VAS | 1.0 (.01) | .513 | |
| MAWT | .82 (.06) | .004 | |
| Inpatient | |||
| PCS | 1.1 (.02) | .0001 | |
| VAS | 1.1 (.02) | .0001 | |
| MAWT | .78 (.07) | .006 | |
Acknowledgments
The authors are indebted to the 22 partner organizations of the WCWL for their on-going support throughout the project.
Footnotes
Berlin Institut für Kinder- und Jugendpsychiatrie Psychotherapie und Soziale Pädiatrie, Vorstand: Dr. med. Stefan Buchmann, Dr. med. Peter Greven
Disclaimer
Funding for the Western Canada Waiting List Project is provided by Manitoba Health, Saskatchewan Health, Alberta Health and Wellness, the British Columbia Ministry of Health Services and Health Canada. The views expressed herein do not necessarily represent the official policy of federal, provincial, or territorial governments or WCWL member organizations.
References
- Boyle MH, Offord DR, Racine Y, Sanford M, Szatmari P, Fleming JE. Evaluation of the original Ontario Child Health Study scales. Canadian Journal of Psychiatry. 1993;38:397–405. doi: 10.1177/070674379303800605. [DOI] [PubMed] [Google Scholar]
- Breton JJ, Bergeron L, Valla JP, Berthiaume C, Gaudet N, Lambert J, et al. Quebec child mental health survey: prevalence of DSM-III-R mental health disorders. Journal of Child Psychology and Psychiatry. 1999;40:375–384. [PubMed] [Google Scholar]
- Burns B, Costello J, Angold A, Tweed D, Stangl D, Farmer E, Erkanli A. Children’s mental health service use across services sectors. Health Affairs. 1995;14:147–159. doi: 10.1377/hlthaff.14.3.147. [DOI] [PubMed] [Google Scholar]
- Clow D, Mustafa A, Szollar J, Wood N, Reid J, Sinden S. Reducing waiting times associated with an integrated child health service. Journal of The Royal Society Of Health. 2002;122:245–250. doi: 10.1177/146642400212200412. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. 2001 http://www.surgeongeneral.gov/topics/cmh/childreport.htm. [PubMed]
- Edwards RT, Boland A, Wilkinson C, Cohen D, Williams J. Clinical and lay preferences for the explicit prioritisation of elective waiting lists: survey evidence from Wales. Health Policy. 2003;63:229–237. doi: 10.1016/s0168-8510(02)00101-x. [DOI] [PubMed] [Google Scholar]
- Ezpeleta L Keeler G, Erkanli A Costello EJ, Andgold A. Epidemiology of psychiatric disability in childhood and adolescence. Journal of Child Psychology and Psychiatry. 2001;42:901–914. doi: 10.1111/1469-7610.00786. [DOI] [PubMed] [Google Scholar]
- Foreman DM, Hanna M. How long can a waiting list be? Psychiatric Bulletin. 2000;24:211–213. [Google Scholar]
- Hadorn DC, the Steering Committee of the Western Canada Waiting List Project. Setting priorities for waiting lists: defining our terms. Canadian Medical Association Journal. 2000;163:857–860. [PMC free article] [PubMed] [Google Scholar]
- Hadorn DC, Holmes AC. The New Zealand priority criteria project. Part 1: Overview. British Medical Journal. 1997;314:131–134. doi: 10.1136/bmj.314.7074.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones E, Lucey C, Wadland L. Triage: a waiting list initiative in a child mental health service. Psychiatric Bulletin. 2000;24:57–59. [Google Scholar]
- Jones SM, Bhadrinath BR. GPs’ views on prioritisation of child and adolescent mental health problems. Psychiatric Bulletin. 1998;22:484–486. [Google Scholar]
- Lyons JS, Rawal P, Yeh I, Leon SC, Tracy P. Use of measurement audit in outcomes management. Journal of Behavioral Health Services Research. 2002;29:75–80. doi: 10.1007/BF02287834. [DOI] [PubMed] [Google Scholar]
- MacCormick AD, Collecutt WG, Parry BR. Prioritizing patients for elective surgery: a systematic review. Australian and New Zealand Journal of Surgery. 2003;73:633–642. doi: 10.1046/j.1445-2197.2003.02605.x. [DOI] [PubMed] [Google Scholar]
- Messick S. Validity. In: Linn R, editor. Educational measurement. 3. New York: Macmillan Publishing Company; 1989. pp. 13–103. [Google Scholar]
- Munjal A, Latimer M, McCune N. Attendance at child psychiatry new patient clinics. Irish Journal of Psychological Medicine. 1994;11:182–184. [Google Scholar]
- Noseworthy TW, McGurran JJ, Hadorn DC, the Steering Committee of the Western Canada Waiting List Project. Waiting for scheduled services in Canada: development of priority-setting scoring systems. Journal of Evaluation and Clinical Practice. 2003;9:23–31. doi: 10.1046/j.1365-2753.2003.00377.x. [DOI] [PubMed] [Google Scholar]
- Offord DR, Boyle MH, Fleming JE, Blum HM, Grant NI. Ontario Child Health Study. Summary of selected results Canadian Journal of Psychiatry. 1989;34:483–491. doi: 10.1177/070674378903400602. [DOI] [PubMed] [Google Scholar]
- Offord DR, Boyle MH, Szatmari P, Rae-Grant NI, Links PS, Cadman DT, et al. Ontario Child Health Study. II Six-month prevalence of disorder and rates of service utilization. Archives of General Psychiatry. 1987;44:832–836. doi: 10.1001/archpsyc.1987.01800210084013. [DOI] [PubMed] [Google Scholar]
- Parker KC, Froese AP. Waiting list information strategies for child psychiatry: an intervention and measurement approach. Canadian Journal of Psychiatry. 1992;37:387–392. doi: 10.1177/070674379203700607. [DOI] [PubMed] [Google Scholar]
- Potter R, Darwish A. Predicting attendance at child and adolescent clinics. Psychiatric Bulletin. 1996;20:717–718. [Google Scholar]
- Roberts S, Partridge I. Allocation of referrals within a child and adolescent mental health service. Psychiatric Bulletin. 1998;22:497–489. [Google Scholar]
- Srebnik D, Uehara E, Smukler M. Field test of a tool for level-of-care decisions in Community Mental Health Systems. Psychiatric Services. 1998;491:91–96. doi: 10.1176/ps.49.1.91. [DOI] [PubMed] [Google Scholar]
- Smith DH, Hadorn DC, the Steering Committee of the Western Canada Waiting List Project. Lining up for children’s mental health services: a tool for prioritizing waiting lists. Journal of the American Academy of Child Adolescent Psychiatry. 2002;41:367–376. doi: 10.1097/00004583-200204000-00007. [DOI] [PubMed] [Google Scholar]
- Spady DW, Schopflocher DP, Svenson LW, Thompson AH. Prevalence of mental disorders in children living in Alberta, Canada, as determined from physician billing data. Archives of Pediatric and Adolescent Medicine. 2001;155:1153–1159. doi: 10.1001/archpedi.155.10.1153. [DOI] [PubMed] [Google Scholar]
- U.S. Public Health Service. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, DC: Department of Health and Human Services; 2000. [Google Scholar]
- Waddell C Offord DR, Shepherd CA Hua JM, McEwan K. Child psychiatric epes idemiology and Canadian public policy-making: the state of the science and the art of the possible. Canadian Journal of Psychiatry. 2002;47(9):825–32. doi: 10.1177/070674370204700903. [DOI] [PubMed] [Google Scholar]
- Walker S. Mental health. Wait not, want not? Health Services Journal. 1998;108:32–33. [PubMed] [Google Scholar]
- World health report: 2001: Mental health: New understanding, new hope.