Abstract
Background
Mice with a deleted Cav1 gene encoding caveolin-1 develop adipocyte abnormalities and insulin resistance. From genomic DNA of patients with atypical lipodystrophy and hypertriglyceridemia who had no mutations in any known lipodystrophy gene, we used DNA sequence analysis to screen the coding regions of human CAV1 (MIM 601047).
Results
We found a heterozygous frameshift mutation in CAV1, designated I134fsdelA-X137, in a female patient who had atypical partial lipodystrophy, with subcutaneous fat loss affecting the upper part of her body and face, but sparing her legs, gluteal region and visceral fat stores. She had severe type 5 hyperlipoproteinemia, with recurrent pancreatitis. In addition, she had some atypical features, including congenital cataracts and neurological findings. Her father was also heterozygous for this mutation, and had a similar pattern of fat redistribution, hypertriglyceridemia and congenital cataracts, with milder neurological involvement. An unrelated patient had a different heterozygous frameshift mutation in the CAV1 gene, designated -88delC. He also had a partial lipodystrophy phenotype, with subcutaneous fat loss affecting the arms, legs and gluteal region, but sparing his face, neck and visceral fat stores. He also had severe type 5 hyperlipoproteinemia, with recurrent pancreatitis; however he had no clinically apparent neurological manifestations. The mutations were absent from the genomes of 1063 healthy individuals.
Conclusion
Thus, very rare CAV1 frameshift mutations appear to be associated with atypical lipodystrophy and hypertriglyceridemia.
Background
Lipodystrophies are a heterogeneous group of diseases that result in abnormal fat distribution and severe insulin resistance [1-5]. The molecular basis for several forms of partial and complete lipodystrophy syndromes have been characterized [6], but some patients with inherited lipodystrophies do not have mutations in the known lipodystrophy genes. Finding other candidate genes for evaluation can be challenging because the families of such probands are often small, so positional cloning (or linkage analysis) using genome-wide marker sets cannot be performed. Another approach to find causative mutations is to select human candidate genes by analogy from genes that have been manipulated in animal models with a comparable phenotype. For instance, mice with induced deficiency in Cav1 encoding the cell surface protein caveolin-1 (MIM 601047) showed depleted and abnormal adipocytes with insulin resistance and severe hypertriglyceridemia [7-9]. Since no human mutations in CAV1 have yet been reported, we screened the genomic DNA of 60 unrelated adults with partial lipodystrophy and hypertriglyceridemia and no mutation in any known lipodystrophy gene to search for coding sequence mutations in CAV1.
Results
Demographics of study sample
From a tertiary referral lipid clinic, we evaluated 60 patients (80% female) who had partial lipodystrophy, with diabetes or moderate to severe (type 4 or 5) hypertriglyceridemia. Age, body mass index, untreated fasting plasma cholesterol and triglycerides (mean+standard deviation [SD]) were, respectively, 52.5 ± 14.0 years, 26.2 ± 3.8 kg/m2, 6.9 ± 5.0 mmol/L and 11.1+10.0 mmol/L. All subjects consented to DNA analysis. No coding sequence mutations were found in LMNA, PPARG, BSCL2 or AGPAT2 genes encoding nuclear lamin A/C, peroxisome proliferator-activated receptor gamma, seipin or 1-acyl-sn-glycerol-3-phosphate acetyltransferase, respectively.
Characterization of patients with CAV1 mutations
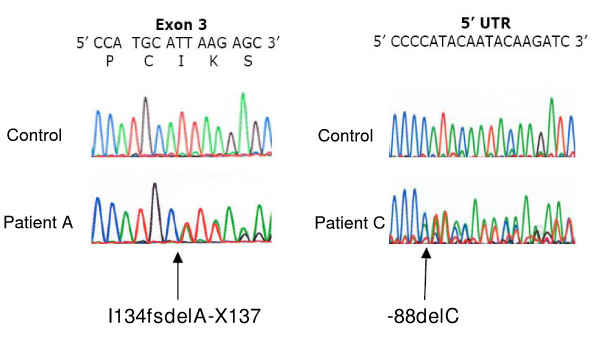
Two rare heterozygous coding sequence variants in CAV1 were found among the screened patients, I134fsdelA-X137 in one patient and -88delC in another (Figure 1). These frameshift mutations were absent from the genomes of 1063 normolipidemic control subjects. The I134fsdelA-X137 mutation predicted premature termination, with loss of the carboxy terminal half of the protein product. This mutation was subsequently found in the proband's father, who had a similar phenotype. The -88delC mutation occurred within the 5'-untranslated region with a potential effect on the reading frame. The clinical features of the father and daughter with the heterozygous I134fsdelA-X137 mutation and the singleton patient with the heterozygous -88delC mutation are summarized in Table 1.
Figure 1.
Electropherogram scans showing the novel heterozygous CAV1 frameshift mutations in the lipodystrophy patients. The left half of the figure shows a portion of CAV1 exon 2 from genomic DNA of a control subject and Patient A. The right half of the figure shows a portion of CAV1 5' untranslated region (5'UTR) from genomic DNA of a control subject and Patient C. For each tracing, normal nucleotide sequence is shown in the top line of letters, with single letter amino acid codes and codon numbers beneath for exon sequence. The position of each inserted nucleotide is indicated by the arrows for the respective mutations I134fsdelA-X137 and -88delC.
Table 1.
Clinical and biochemical features of atypical lipodystrophy patients with CAV1 mutations
| Attribute | Patient A | Patient B | Patient C |
| Ancestry | Northern Europe | Northern Europe | Northern Europe |
| CAV1 mutation name | I134fsdelA-X137 | I134fsdelA-X137 | -88delC |
| age at assessment (years) | 28 | 55 | 35 |
| sex | female | male | male |
| lipodystrophy onset | birth | birth | adulthood |
| BMI (kg/m2) | 25.0 | 24.5 | 25.6 |
| waist circumference (cm) | 86 | 88 | 92 |
| Subcutaneous fat changes: | |||
| face | decrease | decrease | increase |
| arms | decrease | decrease | decrease |
| gluteal region | increase | increase | decrease |
| thighs | increase | increase | decrease |
| calves | increase | increase | decrease |
| visceral | increase | increase | increase |
| age of diabetes onset (years) | none | 30 | 33 |
| hypertension and age of onset | none | none | 33 |
| hyperlipoproteinemia | type 5 | type 4 | type 5 |
| pancreatitis | recurrent | no | recurrent |
| highest historical plasma triglyceride | 20.4 mmol/L | 80 mmol/L | 16.5 mmol/L |
| acanthosis nigricans | present | absent | present |
| congenital cataracts | bilateral | bilateral | absent |
| atypical retinitis pigmentosa | bilateral | bilateral | absent |
| tinnitus | moderate | absent | absent |
| nystagmus | severe | absent | absent |
| spastic ataxia | severe | mild | absent |
| dysdiadochokinesia | severe | mild | absent |
| muscle power in lower limbs | diminished (4/5) | normal | normal |
| sensory glove/stocking neuropathy | severe | mild | absent |
| Babinski sign | bilateral | absent | absent |
| finger past-pointing | severe | absent | absent |
| other comments | wheel-chair bound since age 20; similarly affected paternal aunt (deceased) | Patient A's father; legally blind | requires 120 U of insulin daily |
The history and clinical features of the I134fsdelA-X137 mutation proband (Patient A) and her affected father (Patient B) have been previously reported [10]. Briefly, the proband, who was assessed at age 28 years, was a woman of Northern European origin who was wheelchair bound since early adulthood. At birth, she was noted to have a lack of facial and upper body subcutaneous fat, micrognathia and congenital cataracts. Later, diplopia, tinnitus and a central auditory processing defect were noted. She had severe type 5 hyperlipoproteinemia with recurrent pancreatitis; she had insulin resistance but no diabetes. On examination, she was noted to have orthostatic hypotension, a high arched palate, taut skin with sparing of subcutaneous fat on buttocks, hips and thighs. She was noted also to have webbed toes, acanthosis nigricans, retinitis pigmentosa, iris deposits, marked nystagmus, ocular dysmetria, past-pointing on finger-nose testing, dysdiadochokinesis, a spastic-ataxic gait, spontaneous clonus of legs, bilateral Babinski signs, reduced power in the lower extremity and lost vibration sense in a glove-and-stocking distribution. She had leg spasms, a stiff gait, paresthesiae, imbalance and urinary incontinence. Investigations showed lipemic plasma with markedly elevated serum cholesterol (9.3 mmol/L) and triglycerides (20.4 mmol/L). Her father (Patient B), a 55 year old diabetic man of Northern European origin, had similar body fat distribution to his daughter. He also had congenital cataracts and retinitis pigmentosa, but no neurological complaints, and was ambulatory and well-functioning. On examination, he was noted to have absent facial, neck, and limb fat with increased abdominal and lower back subcutaneous fat. He also had decreased sensation in both legs, with normal muscle power and tone; an unsteady narrow-based gait was elicited. He had milder biochemical abnormalities than his daughter, with mild hypertriglyceridemia and no history of pancreatitis. Of note, Patient B's sister (the paternal aunt of Patient A) died from an undefined neurological condition at age 40. Medical records showed a clinical presentation similar to Patient A, with analogous fat redistribution, leg weakness and ataxia beginning at age 18 and requirement for a wheelchair at age 20 [10]. Patient C, a heterozygote for the CAV1 -88delC mutation, was 35 years old at assessment. He was noted in his early 20's to have redistributed fat stores, with a relative loss of subcutaneous fat on his arms, gluteal region, thighs and calves and increased visceral fat on abdominal ultrasound examination. He had severe hypertriglyceridemia (range 10 to 80 mmol/L) beginning in his late 20's, with recurrent episodes of pancreatitis. He was diagnosed with diabetes at age 33 and currently takes 120 units of insulin daily in addition to fenofibrate 200 mg daily. Physical examination revealed fat redistribution, with no ocular, neurological, dermatologic or musculoskeletal findings.
Discussion
Caveolin-1 is expressed in numerous tissues and is a central component of cell surface caveoli, which are plasma membrane microdomains that regulate signaling pathways and processes such as cell migration, polarization, proliferation and especially endocytosis [11-13]. Cav1 appears to have a significant role in murine adipocyte metabolism, and disruption of the gene leads to severe hypertriglyceridemia, insulin resistance and adipocyte abnormalities, which are all features that are consistent with human partial lipodystrophy [7-9]. Our genetic findings suggest that CAV1 might also have a role in human adipose, insulin and triglyceride metabolism, albeit only two frameshift mutations in CAV1 were found among 60 lipodystrophic patients with a normal coding sequence of known lipodystrophy genes.
The frameshift mutations would be expected to result in a compromised gene product from the affected allele. The I134fsdelA-X137 mutation co-segregated with the phenotype from father to daughter, but the more severe phenotype in the daughter suggests that other factors – perhaps genetic or non-genetic – can modulate the severity of the phenotype. The presence of a comparably severe phenotype in Patient A's paternal aunt suggests that gender might also modulate the severity of phenotypic expression in carriers. Also, the variable organ system involvement – the ocular and central nervous systems in Patients A and B but not in Patient C – is consistent with the variable multi-system phenotypes seen in Cav1 deficient mice depending on genetic background [11-13]. However, heterozygous Cav1 deficient mice do not show any phenotype, again suggesting that other factors are required for phenotypic expression in these patients. Unfortunately, we could not further extend the families in order to document phenotypes seen in other CAV1 mutation carriers at present, although this is planned for the future.
Conclusion
The association of these rare frameshift mutations in CAV1 with atypical presentations of partial lipodystrophy with insulin resistance and hypertriglyceridemia, the absence of these mutations from healthy controls together with evidence from mouse models link the CAV1 gene with human metabolic phenotypes. Since only two mutations were found among 60 screened subjects, CAV1 mutations are a very rare cause of lipodystrophy and hypertriglyceridemia.
Methods
Genomic DNA analysis
The exons and intron-exon boundaries of CAV1 were amplified and bi-directionally sequenced using the primers and conditions in Table 2. All coding sequence mutations were confirmed by a second sequencing reaction performed on another day. The frequency of the CAV1 exon 3 I134fsdelA-X137 variant was determined in healthy control subjects using genomic DNA amplification with primers 5'-ATG GAT ACT GAA TAG TGG GTT TTT and 5'-TGT TGC TGT ATT AGC AAC TTG GA. The 509 bp product was digested with restriction enzyme NsiI (New England Biolabs, Mississauga, ON) and fragments were resolved on 2% agarose gels. The digested fragments of the wild-type allele were 280 and 229 base pairs (bp) in size, while the digested fragment of the mutant allele was 509 bp in size. The frequency of the CAV1 exon 1 -88delC variant was determined in healthy control subjects using genomic DNA amplification with primers 5'-AG ATG ATG CAC TGG GAA AA and 5'-CTA GGC CCC CTC TCC ATT AG, with allele specific diagnostic (SNaPShot) primer 5'-GAT CTT GTA TTG TAT GGG GG.
Table 2.
Primers used for sequencing CAV1
| Exon | Primers | Fragment size (nucleotide base pairs) |
| 1 | F-5' GAG ATG ATG CAC TGG GAA AA R-5' CTA GGC CCC CTC TCC ATT AG |
633 |
| 2 | F-5' GTA GCT GTC GGA GCG GTT AG R-5' GGA GCT CCC ACA CAT CAA AC |
480 |
| 3 | F-5' ATG GAT ACT GAA TAG TGG GTT TTT R-5' TGT TGC TGT ATT AGC AAC TTG GA |
509 |
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
HC and LA carried out all molecular analysis and participated in manuscript writing. JR participated in obtaining patient samples for analysis. RAH conceived of the study, participated in its design, analysis, interpretation and manuscript preparation. All authors approved the final version of the manuscript.
Acknowledgments
Acknowledgements
This work was supported by operating grants from the Canadian Institutes of Health Research (MOP-13430, MOP-39533, MOP-39833), the Heart and Stroke Foundation of Ontario (PRG-5967, NA-6059, T-6018), the Ontario Research Fund, and Genome Canada through the Ontario Genomics Institute. RAH is a Career Investigator of the Heart and Stroke Foundation of Ontario (CI-5710) and holds the Edith Schulich Vinet Canada Research Chair (Tier I) in Human Genetics and the Jacob J. Wolfe Distinguished Medical Research Chair. While this paper was under review, Ae Kim and colleagues reported the first human mutation in CAV1 in a patient with generalized lipodystrophy 14.
Contributor Information
Henian Cao, Email: hcao@robarts.ca.
Lindsay Alston, Email: lalston@uoguelph.ca.
Jennifer Ruschman, Email: Jennifer.Ruschman@cchmc.org.
Robert A Hegele, Email: hegele@robarts.ca.
References
- Bhayana S, Hegele RA. The molecular basis of genetic lipodystrophies. Clin Biochem. 2002;35:171–177. doi: 10.1016/S0009-9120(02)00297-7. [DOI] [PubMed] [Google Scholar]
- Garg A. Acquired and inherited lipodystrophies. N Engl J Med. 2004;350:1220–1234. doi: 10.1056/NEJMra025261. [DOI] [PubMed] [Google Scholar]
- Hegele RA. Lessons from human mutations in PPARgamma. Int J Obes (Lond) 2005;29 Suppl 1:S31–5. doi: 10.1038/sj.ijo.0802911. [DOI] [PubMed] [Google Scholar]
- Hegele RA, Cao H, Anderson CM, Hramiak IM. Heterogeneity of nuclear lamin A mutations in Dunnigan-type familial partial lipodystrophy. J Clin Endocrinol Metab. 2000;85:3431–3435. doi: 10.1210/jc.85.9.3431. [DOI] [PubMed] [Google Scholar]
- Pollex RL, Hegele RA. Hutchinson-Gilford progeria syndrome. Clin Genet. 2004;66:375–381. doi: 10.1111/j.1399-0004.2004.00315.x. [DOI] [PubMed] [Google Scholar]
- Hegele RA, Joy TR, Al-Attar SA, Rutt BK. Thematic review series: Adipocyte Biology. Lipodystrophies: windows on adipose biology and metabolism. J Lipid Res. 2007;48:1433–1444. doi: 10.1194/jlr.R700004-JLR200. [DOI] [PubMed] [Google Scholar]
- Cohen AW, Razani B, Schubert W, Williams TM, Wang XB, Iyengar P, Brasaemle DL, Scherer PE, Lisanti MP. Role of caveolin-1 in the modulation of lipolysis and lipid droplet formation. Diabetes. 2004;53:1261–1270. doi: 10.2337/diabetes.53.5.1261. [DOI] [PubMed] [Google Scholar]
- Cohen AW, Razani B, Wang XB, Combs TP, Williams TM, Scherer PE, Lisanti MP. Caveolin-1-deficient mice show insulin resistance and defective insulin receptor protein expression in adipose tissue. Am J Physiol Cell Physiol. 2003;285:C222–35. doi: 10.1152/ajpcell.00006.2003. [DOI] [PubMed] [Google Scholar]
- Razani B, Combs TP, Wang XB, Frank PG, Park DS, Russell RG, Li M, Tang B, Jelicks LA, Scherer PE, Lisanti MP. Caveolin-1-deficient mice are lean, resistant to diet-induced obesity, and show hypertriglyceridemia with adipocyte abnormalities. J Biol Chem. 2002;277:8635–8647. doi: 10.1074/jbc.M110970200. [DOI] [PubMed] [Google Scholar]
- Berger JR, Oral EA, Taylor SI. Familial lipodystrophy associated with neurodegeneration and congenital cataracts. Neurology. 2002;58:43–47. doi: 10.1212/wnl.58.1.43. [DOI] [PubMed] [Google Scholar]
- Frank PG, Lisanti MP. Caveolin-1 and liver regeneration: role in proliferation and lipogenesis. Cell Cycle. 2007;6:115–116. doi: 10.4161/cc.6.2.3722. [DOI] [PubMed] [Google Scholar]
- Mathew R, Huang J, Gewitz MH. Pulmonary artery hypertension: caveolin-1 and eNOS interrelationship: a new perspective. Cardiol Rev. 2007;15:143–149. doi: 10.1097/01.crd.0000249381.49138.b9. [DOI] [PubMed] [Google Scholar]
- Williams TM, Lisanti MP. The Caveolin genes: from cell biology to medicine. Ann Med. 2004;36:584–595. doi: 10.1080/07853890410018899. [DOI] [PubMed] [Google Scholar]
- Ae Kim C, Delépine M, Boutet E, El Mourabit H, Le Lay S, Meier M, Nemani M, Bridel E, Leite CC, Bertola DR, Semple RK, O'Rahilly S, Dugail I, Capeau J, Lathrop M, Magré M. Association of a homozygous nonsense Caveolin-1 mutation with Berardinelli-Seip Congenital Lipodystrophy. J Clin Endocrinol Metab. 2008 doi: 10.1210/jc.2007-1328. [DOI] [PubMed] [Google Scholar]