Abstract
The goal of this study was to determine the effectiveness of an asthma educational intervention in improving asthma knowledge, self-efficacy, and quality of life in rural families. Children 6 to 12 years of age (62% male, 56% white, and 22% Medicaid) with persistent asthma (61%) were recruited from rural elementary schools and randomized into the control standard asthma education (CON) group or an interactive educational intervention (INT) group geared toward rural families.
Parent/caregiver and child asthma knowledge, self-efficacy, and quality of life were assessed at baseline and at 10 months post enrollment. Despite high frequency of symptom reports, only 18% children reported an emergency department visit in the prior 6 months. Significant improvement in asthma knowledge was noted for INT parents and young INT children at follow-up (Parent: CON = 16.3; INT = 17.5, p < 0.001; Young children: CON = 10.8, INT = 12.45, p < 0.001). Child self-efficacy significantly increased in the INT group at follow-up; however, there was no significant difference in parent self-efficacy or parent and child quality of life at follow-up. Asthma symptom reports were significantly lower for the INT group at follow-up. For young rural children, an interactive asthma education intervention was associated with increased asthma knowledge and self-efficacy, decreased symptom reports, but not increased quality of life.
Keywords: asthma education, self-efficacy, quality of life, rural, children
Introduction
In the United States, the prevalence of asthma is 7.4% for school children 5 to 14 years of age (1, 2). Prevalence rates of asthma in rural children are scant; however, recent studies indicate that the asthma prevalence rate in rural school age children is 12% to 13% (3, 4). Asthma mortality increased from 1980 to 1997 in children 5 to 10 years of age and has been attributed to a decrease in access and utilization of health care, incorrect medication use, and lack of prevention or self-management strategies (2). Limited health care resources and access to care, often noted in rural settings, may result in less preventive and self-management asthma interventions targeted to rural families (5). Asthma self-management interventions are important for parents of children with asthma to decide the extent that they will adhere to prescribed medications (6), limit their activity, or avoid exposures that exacerbate their child’s asthma.
Many self-management asthma interventions have demonstrated an increase in asthma knowledge (7–9), reduced emergency department visits (10), increased self-efficacy (11–12), and quality of life (13–14). The type of self-management interventions, specifically individualized and interactive educational interventions, have been suggested to have the strongest effect on asthma morbidity (10).
Self-efficacy, the confidence that one can carry out a behavior necessary to obtain a desired goal, is another critical component of self-management education (6, 15). Interventions incorporating self-efficacy and other cognitive-behavioral techniques have been associated with improving self-management skills (12). One primary outcome associated with effective self-management interventions is quality of life (16) that has been associated with frequency of symptom severity (17). Thus, it follows that an increase in asthma knowledge should be associated with increased self-efficacy and ultimately quality of life.
Few studies have tested asthma self-management educational interventions in increasing knowledge, self-efficacy, and quality of life in rural pediatric populations. The goal of this study was to test the effectiveness of an asthma educational intervention in improving asthma knowledge, self-efficacy, and quality of life in rural children and their parent/caregivers. We hypothesized that an interactive asthma educational intervention would increase parent/caregiver and child asthma knowledge resulting in increased self-efficacy and quality of life in rural families of children with asthma.
Methods
This study was a two-group, repeated measures, randomized clinical trial testing the effectiveness of an educational intervention for rural children with asthma and their parents. Children and their parent/caregivers who were randomized into the control (CON) group received standard asthma education. Children assigned to the intervention (INT) schools received the educational intervention consisting of two educational workshops, an asthma coloring book, in addition to parental educational workshops. Primary outcome measures included parent/caregiver and child asthma knowledge, self-efficacy, and quality-of-life scores. Data were collected via face-to face and telephone interviews. This study was approved by the Institutional Review Board at the Johns Hopkins University Medicine Institutions, Baltimore, Maryland, and informed consent was obtained from all participating parents/caregivers. Assent was obtained from all participating children.
Recruitment, Randomization and Follow-Up of Study Subjects
We recruited elementary school age children (6 to 12 years) with asthma and their parents/caregivers living in seven rural counties of Maryland from August 2001 to August 2003. Over 1300 letters (1,337) were mailed to parents/caregivers of children attending elementary public schools in the 7 Maryland counties. A total of 378 parents/caregivers responded to the letter and agreed to have their child participate in the study. Of the 378 children who agreed to participate, 288 (76%) were eligible for the study based on having a physician diagnosis of asthma, asthma symptoms over the past 12 months, currently taking an asthma medication either daily or on an as-needed basis, night awakening due to symptoms within the past month, and no other co-morbid pulmonary disease. We randomized at the county level to eliminate potential contamination of children attending the same school but randomized to different groups. All families and children were followed for an entire school year or 10 months, and over 90% of children and parents completed the 10-month, follow-up (Figure 1). Twenty families (9%) did not complete the follow-up interviews primarily due to family relocation out of study area, lost to follow-up, or refusal to continue with the follow-up interviews.
Figure 1.
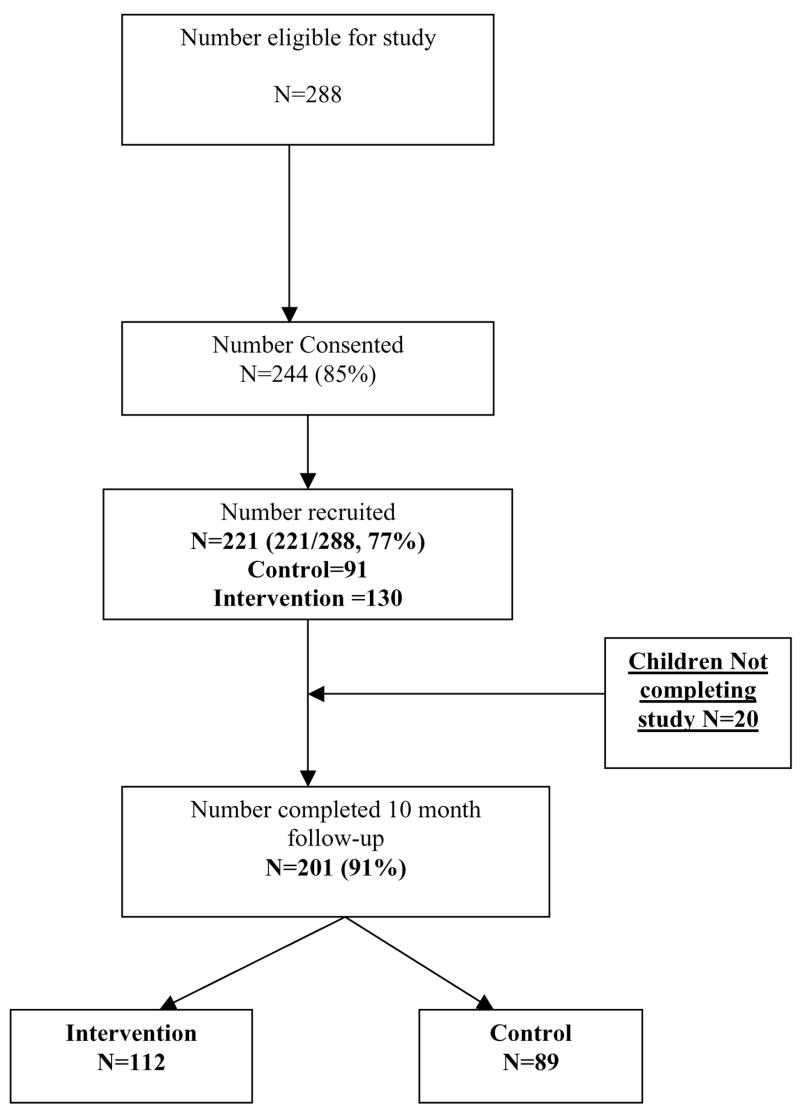
Recruitment flow diagram.
Instrumentation and Measures
Baseline information was obtained from parents/caregivers by telephone or face-to-face interviews using a questionnaire that included demographic, asthma knowledge, quality-of-life, self-efficacy scales, child asthma morbidity, health care utilization, and asthma medication use items. All child asthma knowledge, self-efficacy, and quality of life data were collected during face-to-face interviews. Families without telephones or those who could not be contacted were mailed a card with a toll-free number to call, which linked them to an interviewer who administered the interview.
Parent/caregiver asthma knowledge
Asthma knowledge was assessed using a 20-item multiple choice questionnaire. Content was derived from the current National Asthma Educational Prevention Program (NAEPP) Guidelines (18–19), asthma symptom identification interventions (20), and evidence-based data on rural exposure to allergens and irritants (21). The final 20-item Asthma Knowledge Questionnaire reading level was written at a 4.7 grade level (Flesch-Kincaid grade level). Content validity of the parent knowledge scale, assessed by an expert panel of a pediatric allergist and pediatric asthma nurse experts, was high. Cronbach’s alpha reliability coefficient was moderate at 0.61. Total scores on the asthma knowledge scale ranged from 0 to 20 points.
Parent/caregiver asthma self-efficacy
Parent/caregiver self-efficacy was assessed using a modified 19-item parent self-efficacy instrument (22). The original 18-item questionnaire has 3 subscales: Treatment Efficacy, Attack Prevention, and Asthma Attack Management. Modifications to the questionnaire included adding one item to the Asthma Attack Management subscale. All of the subscales required the parent to select one of five responses ranging from “not at all” scored as 1 point to “completely sure” scored as 5 points. For the original self-efficacy scale, Cronbach alpha reliability co-efficients were 0.76 for the 5-item Treatment efficacy, 0.77 for the 6-item Attack Prevention, and 0.82 for the 7-item Asthma Attack Management subscale. Reliability coefficients for the modified self-efficacy subscales were moderate at 0.67 for Treatment Efficacy, 0.54 for Attack Prevention, and 0.80 for Asthma Attack Management. Scores for the subscales and total questionnaire were Treatment Efficacy (range 5–25), Attack Prevention (range 6–30), and Asthma Attack Management (range 8–40) for a total range of self-efficacy scores between 19 to 95.
Parent/caregiver’s quality of life
The parent/caregiver’s quality of life was ascertained using the Pediatric Caregiver Quality of Life Questionnaire (PC-QOLQ) (16). Intraclass correlation coefficients for total PCQOLQ score and the Emotional Function and Activity Limitation domains were. 80 to .85 (16). Each of the 13 items in the PCQOLQ was measured on a 7-point likert scale ranging from “all of the time” to “none of the time” with lower scores indicating “ none of the time” allowing for a total range of scores between 13 to 91. Scores were calculated for the total quality of life and the two domains of emotional function and activity limitation for each parent. Minimal important differences in quality-of-life scores are 0.5 points and a change of 1.0 is considered a moderate change (23).
Child asthma knowledge
Asthma knowledge for children in grades 1 to 2 was measured by a 15-item picture questionnaire developed using principles identified by Wiley and Hendricks (24) for picture identification research instruments. The 15 items in the questionnaire addressed the content present in the children’s workshop. Each item had three choices based on evidence that the maximum number of choices that young children can discriminate (24). There was only one correct answer for each item, and total scores could vary from 0 to 15 points. Asthma knowledge for children in grades 3 to 5 was measured using a 15-item multiple-choice questionnaire with four option multiple choice responses with only one correct answer for each item. The total score on the test could vary from 0 to 15 points. The child knowledge questionnaire for children in grades 3 to 5 was written at a 2.7 grade level (Flesch-Kincaid readability scale).
Child asthma self-efficacy
Self-efficacy of the child was measured using the 9-item Child Asthma Self-Efficacy measure developed for use in the multisite Childhood Asthma Management Program (CAMP) study (25). This instrument requires the child to select one of four responses ranging from “none of the time, most of the time, some of the time and all of the time” to indicate how often they will be able to perform specific asthma management activities. Responses were scored on a 4-point scale with “none of the time” scored as 0 and “all of the time” scored as 3. Total scores on the self-efficacy questionnaire could range from 0 to 27 points. The Cronbach alpha reliability coefficient was 0.75 for the original child self-efficacy scale (25). For children in grades 1 to 2, the questionnaire was individually administered to each child. Children in grades 3 to 5 were assembled in a group, and the questionnaire was administered to the children as a group.
Child quality of life
The Paediatric Asthma Quality of Life Questionnaire (PAQLQ) (26) was administered to children for measurement of quality of life. The PAQLQ contains 23 items that children with asthma have identified as troublesome in their daily lives. The instrument includes three subscales: activity limitations (5 items), symptoms (10 items), and emotional function (8 items). Response options for each item are on a 7-point anchored scale with a score of 1 indicating maximum impairment and 7 indicating no impairment. All items are weighted equally. Results are presented as the mean score for each subscale as well as the total quality-of-life scale. Intraclass correlation coefficients for children 7 to 10 years of age were 0.89 for overall quality of life, 0.83, 0.87, and 0.68 for the three subscales activity limitations, symptoms, and emotional function, respectively (26). The instrument was administered to each child by a research assistant and lasted for approximately 20 minutes.
Child asthma morbidity
Child asthma morbidity was measured by asking the parent/caregiver the frequency of the child’s day and night symptoms of cough, wheeze, shortness of breath, or chest tightness over the past 6 months. Number of hospitalizations, emergency department (ED), and preventive visits for asthma and specialty care visits were ascertained over a 6-month period. Current asthma medication use was assessed by asking the parent to name all of the child’s current asthma medications, including the names of all controller or quick-reliever medications and the number of steroid courses used over the past 12 months.
Description of Parent/Caregiver and Child Asthma Educational Intervention
Parent/caregiver educational intervention
Intervention parents/caregivers received a 1-hour asthma education session taught by a rural asthma educator in local schools and libraries. Spsecific content addressed in the educational sessions included early warning signs of asthma exacerbations, levels of asthma severity, avoidance of rural environmental exposures, types of asthma medications, how to obtain and use an asthma action plan, and use of cue cards to communicate with their child’s health care provider. Interactive demonstrations with the parents/caregivers included demonstrating the use of the peak flow meter and metered dose inhaler with spacer. To facilitate effective communication with health care providers, each parent/caregiver received cue cards with tips on how to ask questions about home asthma care during the child’s primary care visits. Additionally, all parents received a quarterly newsletter and a resource guide to asthma management care that listed types of insurance, locations for allergy testing, and organizations that conduct smoking cessation sessions. At the end of each parent workshop, participants were asked to evaluate the workshop on a 5-point likert scale ranging from strongly agree, agree, neutral, disagree, and strongly disagree and provide open-ended evaluative comments.
Costs of conducting the educational intervention were estimated US $95.00 per child based on personnel time (registered nurse with asthma education certification and community health worker), supplies of asthma education coloring books, peak flow meters, spacers and toy incentives, travel for personnel, and food for both parents and children. Use of libraries and schools for sessions eliminated any space costs. Cost to the parents and children were primarily time (4 to 5 hours total), and travel expenses to get to educational sessions. We estimate the cost to the family of approximately US $20.00 for travel expenses. Because all child educational sessions were conducted after school, there was no loss of classroom time for any child, and parent sessions were conducted in the evenings to reduce loss of work time.
Child educational intervention
Intervention children received 4 hours of instruction during two separate sessions in the child’s school taught by the asthma educator. The goal of the educational sessions was to provide asthma management information in an interactive format tailored to each child’s developmental level. Specific workshop content included anatomy of asthma, types of asthma medications, i.e., quick reliever versus controller, warning signs of an acute asthma attack, how to use a peak flow meter, how to use a metered-dose-inhaler (MDI) with a spacer, rural environmental factors that exacerbate asthma symptoms, including home and farm exposures, and a description of an asthma action plan. The sessions were highly interactive in that the children practiced and demonstrated their peak flow meter and metered-dose inhaler technique. The children also discussed their asthma medicines and environmental exposures with the asthma educator. In addition, each child received a copy of the “My Asthma Coloring Book” (27), a peak flow meter, spacer device, and a certificate of completion at the final session. Educational materials were written at a 2 to 3 grade level including the coloring book with a reading level at grade 2.6 (Flesch-Kincaid readability scale).
Description of Control or Standard Asthma Care
Parents/caregivers assigned to the standard asthma care or control group were mailed an asthma newsletter on a quarterly basis and received an asthma resource guide at the completion of the study. Control group parents had no formal contact with the asthma nurse educator.
Follow-up data collection
All families received a follow-up interview via telephone at 10 months or the end of the child’s school year to ascertain changes in parent and child asthma knowledge, self-efficacy, quality of life, child asthma morbidity, asthma medication use, and health care utilization. Families were remunerated with a $10.00 check after completion of each follow-up interview.
Data analysis
All analyses were conducted using Stata statistical software system v.7.0 (28) and R Version 2.0.1 (29). Children were categorized by group assignment to the control (CON) or the intervention (INT) group. Severity scores were calculated for each child with a zero score reflecting mild intermittent and a score of 3 indicating severe persistent asthma. The primary outcome variables were parent and child knowledge, self-efficacy and quality-of-life scores. Mean parent and child knowledge, self-efficacy, and quality-of-life scores and change in scores between baseline and follow-up were compared by group assignment. Differences in demographic, outcome, and predictor variables between groups were evaluated using the χ2 test for categorical variables, i.e., parent educational level and analysis of variance for continuous variables, i.e., parent knowledge scores. For variables with a non-normal distribution, the Wilcoxon rank sum test was used to test differences between groups. Statistical significance was accepted as p < 0.05.
Results
Sociodemographic and Child Health Characteristics at Baseline
A total of 288 children and their parents/caregivers were eligible for recruitment as seen in Figure 1. Of this group, 244 (85%) parents/caregivers consented for their child to participate, and 221 (77%) children were recruited into the study. The primary reason for nonparticipation was lack of availability of the parent/caregiver to sign consent. As seen in Table 1, parents/caregivers of children enrolled in the study were primarily the child’s mother (90%), over half reporting some college education or college graduate, employed (78%), and earning income greater than $29,999 (69%). The parents/caregivers had a mean age of 36.2 ± 8.0 years. Almost all children were covered by some form of health insurance (96%), yet only 22% reported having Medical assistance as the type of health insurance. Study children were primarily white (56%) and male (62%) with a mean age of 8 ± 1.7 years. Child asthma severity levels were categorized into mild intermittent (39%), mild persistent (39%), and moderate to severe (22%) persistent asthma. Asthma morbidity was high for this group of children. Over half of children (54–59%) reported daytime symptoms of cough, wheeze, and shortness of breath at least 4 or more times a week. Night cough was reported by almost two thirds of children (64%). Despite high symptom reports, health care utilization was low with only 6% of children reporting a hospitalization and 18% an emergency department (ED) visit for asthma within the past 6 months. Almost one third (31%) of the children reported missing one or more weeks of school for asthma in the past 6 months. Over one third (37%) of children reported 1 or more specialty care visits for asthma.
Table 1.
Sociodemographic and child health characteristics at baseline by group status (N = 221).
| Characteristic | Control (N = 91) | Intervention (N = 130) | Total (N = 221) | Significance | Characteristic | Control (N = 91) | Intervention (N = 130) | Total (N = 221) | Significance |
|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic characteristics | Sociodemographic characteristics | ||||||||
| Caregiver respondent | Day cough symptom frequency | ||||||||
| Mother | 83 (91.2) | 115 (88.5) | 198 (89.6) | χ2 = 5.05 | |||||
| Father | 2 (2.2) | 8 (6.2) | 10 (4.5) | p = 0.41 | 1 time a week | 4 (5.2) | 3 (2.9) | 7 (3.9) | χ2 = 1.3547 |
| Stepmother | 1 (1.1) | 1 (0.7) | 2 (0.9) | 2–3 times a week | 31 (40.3) | 36 (34.9) | 67 (37.2) | p = 0.51 | |
| Grandmother | 4 (4.4) | 2 (1.5) | 6 (2.7) | 4+ times a week | 42 (54.5) | 64 (62.1) | 106 (58.9) | ||
| Legal guardian/other | 1 (1.1) | 4 (3.1) | 5 (2.3) | Day wheeze symptom frequency | |||||
| Parent age (mean, SD) | 35.9 (7.4) | 36.4 (8.4) | 36.2 (8.0) | t = −0.51 | |||||
| p = 0.31 | 1 time a week | 6 (7.1) | 5 (4.5) | 11 (5.6) | χ2 = .7589 | ||||
| Parent education | 2–3 times a week | 33 (39.3) | 42 (37.8) | 75 (38.5) | p = 0.68 | ||||
| <HS | 10 (11.0) | 12 (9.3) | 22 (10.0) | χ2 = 2.43 | 4+ times a week | 45 (53.6) | 64 (57.7) | 109 (55.9) | |
| HS grad | 36 (39.6) | 42 (32.6) | 78 (35.4) | p = 0.48 | Day shortness of breath symptom frequency | ||||
| Some college | 33 (36.7) | 49 (38.0) | 82 (37.3) | ||||||
| College grad + | 12 (13.2) | 26 (20.2) | 38 (17.3) | 1 time a week | 4 (5.1) | 11 (11.1) | 15 (8.5) | χ2 = 2.1501 | |
| Parent income | 2–3 times a week | 29 (37.2) | 37 (37.4) | 66 (37.2) | p = 0.34 | ||||
| <$10,000 | 4 (4.4) | 13 (10.1) | 17 (6.0) | χ2 = 5.918 | 4+ times a week | 45 (57.7) | 51 (51.5) | 96 (54.2) | |
| $10–29,999 | 32 (35.2) | 34 (26.4) | 66 (23.4) | p = 0.21 | Night cough symptom frequency | ||||
| $30–39,999 | 14 (15.4) | 18 (13.4) | 98 (34.2) | ||||||
| $40,000 + | 37 (40.6) | 62 (48.1) | 99 (34.6) | 1 time a week | 2 (2.4) | 2 (1.7) | 4 (2.0) | χ2 = .1167 | |
| Refused | 4 (4.4) | 2 (1.6) | 6 (2.1) | 2–3 times a week | 29 (34.5) | 39 (33.9) | 68 (34.1) | p = 0.94 | |
| Mother employed | 68 (74.7) | 104 (80.0) | 172 (77.8) | Z = 0.5845 | 4+ times a week | 53 (63.1) | 74 (64.3) | 127 (63.8) | |
| Yes | p = 0.44 | Hospitalized last 6 months | |||||||
| Health Insurance for child’s asthma | 85 (97.7) | 113 (95.0) | 198 (96.1) | Z = .4115 | Yes | 7 (7.9) | 7 (5.4) | 14 (6.4) | Z = .2284 |
| Yes | p = 0.52 | Emergency room visits last 6 months | p = 0.63 | ||||||
| Medical insurance | 18 (19.8) | 30 (23.3) | 48 (21.8) | Z = .2016 | |||||
| Medical assistance (Yes) | p = 0.65 | None | 73 (82.1) | 107 (83.0) | 180 (82.2) | χ2 = .1556 | |||
| 1 | 9 (10.0) | 11 (8.5) | 20 (9.1) | p = 0.93 | |||||
| Child characteristics | 2 or more | 8 (8.9) | 11 (8.5) | 19 (8.7) | |||||
| Child age (mean, SD) | 8.08 (1.48) | 8.02 (1.87) | 8.05 (1.72) | t = −.2545 | Number of school days missed last 6 months | ||||
| p = 0.80 | |||||||||
| Child gender | None | 20 (22.2) | 34 (26.2) | 54 (24.5) | χ2 = 1.6309 | ||||
| Male | 51 (56.0) | 86 (66.2) | 137 (62.0) | χ2 = 1.9128 | 1–2 | 17 (18.9) | 20 (15.4) | 37 (16.8) | p = 0.65 |
| Female | 40 (44.0) | 44 (33.8) | 84 (38.0) | p = 0.17 | 3–5 | 22 (24.4) | 38 (29.2) | 60 (27.3) | |
| Child race/ethnicity | 6 or more | 31 (34.4) | 38 (29.2) | 69 (31.4) | |||||
| White (non-Hispanic) | 47 (51.6) | 76 (58.5) | 123 (55.7) | χ2 = 2.94 | Specialty care visits | ||||
| African American | 34 (37.4) | 45 (34.6) | 79 (35.7) | p = 0.40 | 1 or more | 37 (41.6) | 44 (33.1) | 81 (37.2) | Z = .957 |
| Hispanic | 2 (2.2) | 4 (3.1) | 6 (2.7) | p = 0.33 | |||||
| Other | 8 (8.8) | 5 (3.8) | 13 (6.9) | ||||||
| Asthma Severitya | Taking daily controller asthma medicine | Z = 0.089 | |||||||
| Mild intermittent | 39 (42.9) | 47 (36.2) | 86 (38.9) | χ2 = 1.8317 | Yes | 55 (60.4) | 73 (57.5) | 128 (58, 7) | p = 0.77 |
| Mild persistent | 34 (37.4) | 51 (39.2) | 85 (38.5) | p = 0.61 | Number of steroid courses past year | ||||
| Moderate persistent | 8 (8.8) | 18 (13.8) | 26 (11.7) | ||||||
| Severe persistent | 10 (10.9) | 14 (10.8) | 24 (10.9) | None | 40 (43.9) | 58 (45.7) | 98 (44.9) | χ2 = 3.468 | |
| Day symptoms (yes) | 1–2 | 37 (40.7) | 43 (33.9) | 80 (36.7) | p = 0.32 | ||||
| Wheezing | 83 (91.2) | 114 (87.7) | 197 (89.1) | p = .5437 | 3–4 | 9 (9.9) | 22 (17.3) | 31 (14.2) | |
| Shortness of breath | 76 (85.4) | 100 (78.1) | 176 (82.7) | p = 0.24 | 5 or more | 5 (5.5) | 4 (3.1) | 9 (4.1) | |
| Daytime cough | 77 (85.6) | 105 (80.7) | 182 (82.7) | p = 0.46 | Prednisone in home | Z = 0 | |||
| Night time cough | 84 (92.3) | 117 (90.0) | 201 (90.9) | p = 0.73 | Yes | 27 (29.7) | 39 (30.2) | 66 (30.0) | p = 1.0 |
| With exercise | 59 (65.6) | 80 (62.0) | 139 (63.5) | p = 0.68 | |||||
| With colds | 79 (86.8) | 112 (87.5) | 191 (87.2) | p = 1.0 | |||||
Use of a controller daily medication was reported by most children (59%) and over half (55%) reported use of oral steroids over the past year with one of six children (18%) reporting three or more steroid courses within the past year. Comparison of baseline characteristics of caregiver age, education, income and child age, gender, race, type of insurance, asthma severity, symptom frequency, medication use, receipt of specialty care, hospitalizations, ED visits school days missed, and having an asthma action plan by group status (CON versus INT) revealed no significant differences (Table 1).
Child Health Characteristics at Follow-Up
Although there was no significant difference in the number of ED visits, hospitalizations, or regular asthma care visits between groups at follow-up, there was a significant decrease in the mean change of severity scores from baseline to follow-up between the groups with the INT group experiencing a significant decrease in severity over time (Table 2). At follow-up, parents in the INT group reported significantly fewer symptoms of shortness of breath (χ2 = 13.91; p = 0.007); fewer times when their child woke up at night with wheezing (χ2 = 11.17 p = 0.02), shortness of breath (χ2 = 10.55; p = 0.03), and chest tightness/discomfort (χ2 = 10.13; p = 0.02). Significantly more CON parents reported controller medication use at follow-up (Table 2). There was no significant difference in parental report of having an Asthma Action Plan (AAP) in the home at follow-up by group status (CON, 39.8%, INT 48.2%, Z = 1.06, p = 0.30).
Table 2.
Child health outcomes at follow-up by group status (N = 201)
| Characteristic | Control (N = 89) | Intervention (N = 112) | Total (N = 201) | Significance |
|---|---|---|---|---|
| Child health characteristics | ||||
| Emergency department visits during follow-up | ||||
| Yes | 16 (18.0) | 15 (13.4) | 31 (15.4) | χ2 = 0.90, df = 1, p = 0.34 |
| Hospitalized during follow-up | ||||
| (Yes) | 5 (5.6) | 4 (3.6) | 9 (4.5) | χ2 = 0.25, df = 1, p = 0.62 |
| Receive regular asthma care visits (non-acute) | ||||
| Yes | 64 (71.9) | 81 (72.3) | 145 (72.1) | χ2 = 0.35, df = 1, p = 0.55 |
| Controller medication use | ||||
| Yes | 56 (62.9) | 59 (52.7) | 115 (57.2) | χ2 = 3.72, df = 1, p = 0.05 |
| Severity | ||||
| Mild intermittent | 33 (37.1) | 61 (54.5) | 94 (46.8) | |
| Mild persistent | 34 (38.2) | 36 (32.1) | 70 (34.8) | χ2 = 5.81 |
| Mod persistent | 6 (6.7) | 9 (8.0) | 15 (7.4) | df = 3, |
| Severe persistent | 10 (11.3) | 6 (5.4) | 16 (8.0) | p = 0.12 |
| Missing | 6 (6.7) | 6 (3.0) | ||
| Change in severity score from baseline to follow-up based on symptom frequency (scores range from 1–4) | 0.01 (1.15) | −0.40 (1.13) | −0.22 (1.15) | T = 2.50, df = 173, p = 0.01 |
Asthma Knowledge
Parent/caregiver
Mean total parent/caregiver asthma knowledge scores were not significantly different by group at baseline; however, at follow-up the intervention group scored significantly higher on the asthma knowledge scale (CON: 16.3; INT:17.5, p = 0.0004) (Table 3). Of note is that parents in the intervention group scored significantly higher on knowledge items related to differences between quick reliever medication and controller medication use, the purpose of metered dose inhalers, and use of peak flow meters as compared to control parents. Environmental control knowledge items were not significantly different between groups (Table 3). Almost all parents in both groups reported the correct responses for protecting children from tobacco smoke.
Table 3.
Parent asthma knoweldege scores at follow-up (total score and specific items) (N = 201).
| Knowledge item | Control (N = 89) | Intervention (N = 112) | Total (N = 201) | Significance |
|---|---|---|---|---|
| Total knowledge score at | 16.34 | 17.51 | 17.0 | Wilcoxon |
| Follow-up (mean range 11–20) | Rank Sum W = 3345, p = 0.0004 | |||
| Medication knowledge items N (% correct) | ||||
| Quick reliever medicines are taken when asthma symptoms occur (63) | 61 (74.0) | 96 (86) | 157 (78.1) | Z = 3.79 |
| p = .0.05 | ||||
| Purpose of metered dose inhaler is to deliver medication directly into the lung. (64) | 53 (64) | 89 (80) | 142 (70.6) | Z = 5.11 |
| p = .0.02 | ||||
| Long-term controller asthma medicines reduce inflammation in the airways (correct) (69) | 47 (57) | 80 (71 | 127 (63.2) | Z = 3.97 |
| p = 0.046 | ||||
| When using a metered dose inhaler, a child should breathe in deeply and slowly (67) | 63 (76) | 97 (87) | 160 (80) | Z = 3.02 |
| p = 0.08 | ||||
| When child has asthma symptoms the best medicine to take is quick-reliever medicine (76) | 63(76) | 90 (80) | 153(76.1) | Z = 0.33 |
| p = 0.57 | ||||
| What inhaler or puffer should be used when child has asthma symptoms (Albuterol) (81)? | 81 (98) | 108 (96) | 189 (94) | Z = 0.002 |
| p = 0.96 | ||||
| When your child has an asthma attach at home and his/her symptoms get worse after several treatments with a quick reliever medicine, what is the next step? (contact primary care provider) (74) | 72 (80) | 101 (90) | 173 (86) | Z = 0.27 |
| p = 0.60 | ||||
| What precaution should be taken when using a quick reliever asthma medicine? (Wait at least 1 minute between puffs when using a metered dose inhaler (78) | 50 (60) | 83 (74) | 133 (66) | Z = 3.61 |
| p = 0.06 | ||||
| Peak flow meter use knowledge items | ||||
| When should a peak flow meter be used to obtain child’s personal best reading? (Twice a day when symptoms are absent) (77) | 42 (50) | 78 (70) | 120 (60) | Z = 6.52 |
| p = 0.01 | ||||
| What is the best device to use at home to monitor asthma? (Peak flow meter) (75) | 77 (93) | 111 (99) | 188 (94) | Z = 3.85 |
| p = 0.05 | ||||
| Environmental control knowledge items | ||||
| What is best way to reduce cockroaches in home (Bait traps) (65) | 70 (79) | 97 (87) | 167 (83) | Z = 0.06 |
| p = 0.81 | ||||
| Best way to protect children from tobacco smoke is to ask people to smoke outside the house (66) | 82 (92) | 111 (99) | 193 (96) | Z = 0.0 |
| p = 1.0 | ||||
| Best method to reduce dust mites in home is to cover mattresses with zippered plastic cases to (70) | 58 (70) | 76 (68) | 134 (67) | Z = 0.02 |
| p = 0.89 | ||||
| Best way to reduce child’s exposure to things in rural setting that make asthma worse (remove outdoor work/farm clothes before sitting on the sofa) (79) | 61 (74) | 93 (83) | 154 (77) | Z = 2.07 |
| p = 0.15 | ||||
Child knowledge by grade level
As seen in Table 4, at follow-up the mean total child knowledge scores for the young children (grades 1 to 2) were significantly higher in the intervention group (p < 0.0001). However, there was no significant difference between groups at follow-up in mean knowledge scores for children in grades 3 to 5. A significantly higher number of young INT children reported correct answers to items addressing peak flow meter use, exposure to cat can make asthma worse, and part of body affected by asthma. In the older children in grades 3 to 5, significantly more children in the INT group reported correct responses for items regarding use of quick reliever medication and peak flow meter use as compared to children in the CON group. Correlation between parent and child knowledge scores at follow-up were low (grades 1–2: Spearman ρ = 0.26; grades 3–5: Spearman ρ = 0.32).
Table 4.
Child knowledge scores at follow-up by age group (N = 200).
| Children grades 1–2
|
||||
|---|---|---|---|---|
| Knowledge item | Control (N = 32) | Intervention (N = 51) | Total (N = 83) | Significance |
| Total Knowledge score at follow-up mean range 7–14 | 10.75 | 12.45 | 11.79 | T test = −3.77, p =< 0.0001 |
| Medication knowledge items N (% correct) | ||||
| Which picture of things makes asthma worse? (Cat) (3) | 18 (56) | 43 (84) | 61(73) | Z = 6.57 |
| p = 0.01 | ||||
| What picture is a peak flow meter? (6) | 13 (41) | 43 (84) | 56 (67) | Z = 15.17 |
| p =< .0001 | ||||
| What part of body gets clogged with mucus during an asthma attack? (Lung picture) (9) | 19 (59) | 44 (86) | 63 (76) | Z = 6.38 |
| p = 0.01 | ||||
| Children grades 3–5
|
||||
| Knowledge item | Control (N = 56) | Intervention (N = 61) | Total (N = 117) | Significance |
|
| ||||
| Total knowledge score at follow-up mean range 3–15 | 9.93 | 10.41 | 10.18 | t test = −0.91, p = 0.18 |
| What medicine should you take when you feel an asthma attack is starting? (Quick Reliever) (2) | 20 (36) | 40 (66) | 60 (51) | Z = 9.26 |
| p = 0.002 | ||||
| A peak flow meter is a device to see if your asthma is getting worse (7) | 25 (45) | 40 (66) | 65 (56) | Z = 4.37 |
| p = 0.04 | ||||
| The correct way to use a peak flow meter is blow out as fast and as hard as you can (8) | 22 (39) | 41 (67) | 63 (54) | Z = 8.07 |
| p = 0.004 | ||||
Self-efficacy
Parent/caregiver
As seen in Table 5, mean total and sub-scale self-efficacy scores did not differ by group at follow-up or by change score between baseline and follow-up for the three subscales (Treatment Efficacy, Attack Prevention, and Asthma Attack Management). A trend (p = 0.07) was noted in the mean total self-efficacy score with the INT group reporting high self-efficacy at follow-up as compared to the CON group.
Table 5.
Mean self-efficacy and quality-of-life scores at follow-up and change in scores from baseline to follow-up by group status*
| Mean score control | Mean score intervention | Mean change score control | Mean change score intervention | |
|---|---|---|---|---|
| Self-efficacy | ||||
| Parent/caregiver | ||||
| Treatment efficacy subscale | 22.84 (2.8) | 22.77 (2.9) | 0.44 (3.6) | 0.63 (3.2) |
| Attack prevention subscale | 27.39 (2.9) | 27.73 (2.4) | 1.89 (6.7) | 2.00 (6.2) |
| Asthma attack management subscale | 36.97 (3.3) | 37.25 (3.5) | ||
| Total scale (range 19–95) | 87.03 (7.3) | 88.56 (6.6)a | 1.88 (8.7) | 3.58 (7.6) |
| Child (all ages) | ||||
| Total scale (range 0–27) | 20.32 (6.8) | 21.02 (6.8) | −0.11 (6.9) | +2.62 (6.3)b |
| Quality of life | ||||
| Parent/caregiver | ||||
| Activity limitation subscale | 6.42 (1.0) | 6.47 (1.0) | −0.01 (1.2) | 0.20 (1.3) |
| Emotional function subscale | 6.37 (0.8) | 6.49 (0.8) | 0.16 (1.0) | 0.30 (0.9) |
| Total scale (range 1–7) | 6.38 (0.8) | 6.49 (0.8) | 0.11 (1.0) | 0.27 (0.9) |
| Child (all ages) | ||||
| Activity domain subscale | 3.51 (1.2) | 3.59 (1.2) | −0.47 (1.4) | −0.09 (1.7) |
| Emotional domain subscale | 3.19 (1.4) | 2.47 (1.4) | −0.30 (1.3) | −0.32 (1.2) |
| Symptom domain subscale | 3.20 (1.2) | 2.66 (1.2) | −0.28 (1.0) | −0.27 (1.1) |
| Total scale (range 1–7) | 4.81 (1.5) | 5.50 (1.5) | +0.34 (1.3) | +0.40 (1.4) |
All comparisons p > 0.05.
Wilcoxon Rank Sum = 2517, p = 0.07.
t = 2.86, df = 175, p = 0.005.
Child
Although mean child total self-efficacy scores did not differ by group at follow-up, INT children had a significantly higher change in total self-efficacy scores from baseline to follow-up as compared to CON children (p = 0.005) (Table 5). Correlations between child and parent total self-efficacy scores at baseline and follow-up were nonsignificant (Spearman ρ = −0.004 to 0.22).
Quality of Life (QOL)
Parent/caregiver
Mean parent total and subscale QOL scores were high at baseline and follow-up. There was no statistical difference for mean Activity Limitation, Emotional Function subscales, and total QOL scores or in the QOL change scores between baseline and follow-up by group status (Table 5).
Child
As seen in Table 5, there were no significant differences in mean child quality-of-life (QOL) scores between groups at follow-up nor by change in score between baseline and follow-up by group status. Overall, the child total quality-of-life scores were less positively skewed than the parent total quality-of-life scores.
Parent/caregiver evaluative responses to educational intervention
Most parents assigned to the intervention completed the workshop evaluation forms (81%) and reported overwhelming positive evaluations. In specific, most parents strongly agreed that after attending the educational program they understood the definition of “quick reliever or rescue medication” (82%) and when to use quick reliever medications, knew what a “controller medication” was and when to use them (79%), understood the importance of an Asthma Action Plan (83%), knew how to help their child use his/her MDI the right way (81%), and how to help their child with his/her Peak Flow meter diary (75%). Specific parental comments focused on the interactive experience during the teaching sessions, i.e. “the demonstrations of asthma devices were great”; “This class really taught me how to use my son’s peak flow meter and meds.”
Discussion
Our results indicate that an interactive child and parent asthma educational intervention significantly increased parent and young child knowledge in rural families of children with persistent asthma consistent with previous reports of school-based asthma educational programs (7, 9, 30–32), although there was no change in parent quality of life or self-efficacy. Despite high parent asthma knowledge scores recorded at baseline, we did demonstrate a significant higher knowledge level in the intervention group, suggesting that rural families may have sufficient asthma management knowledge but insufficient beliefs or ability to change their behavior around asthma management of their child.
Child asthma knowledge scores were significantly increased only in the younger children in grades 1 to 2. We purposely designed the educational sessions to maximize child participation and to allow children to play with medication delivery and peak flow meters and to use a coloring book to reinforce the use of controller medications and peak flow meters in the child’s home. Interactive teaching techniques correlate with the “concrete operational thinking” described in early school age children (33). Not only did the younger children receive interactive, individualized educational sessions but also interactive knowledge tests as compared to the paper-and-pencil tests used with the older children. The interactive nature of the intervention may be one of the most effective techniques for instructing young children with asthma. Despite the difference in total knowledge scores by age group, use of a peak flow meter knowledge was consistently increased in all intervention children most likely reflecting the interactive quality of the child educational intervention. Self-management education that teaches problem solving skills and self-efficacy to patients has been shown to result in more positive outcomes (6). Our results indicate that parents increased their knowledge primarily for asthma medication use. Perhaps rural families extract the knowledge they need, i.e., medication use (5), and were uninterested or unconcerned about other asthma management skills less relevant to their child’s care.
Self-efficacy has a strong influence on the decisions and choices that children and adults make in self-management behaviors as well as the amount of effort and persistence devoted to these behaviors (34). We attribute the improved child self-efficacy scores to allowing intervention children to demonstrate use of medication and peak flow meters as well as receive corrective instruction when inaccurate use was detected. We did not support our hypothesis that increased parent and child quality of life would be associated with increased knowledge scores in that the quality-of-life scores did not meet the criteria for a minimal change in scores (23) between baseline and follow-up. However, several studies indicate that knowledge alone may not be sufficient for behavior change or improved quality of life (8, 35, 36). Alternatively, the concept of quality of life may differ in rural settings. Despite a significant decrease in symptom reports in the intervention children at follow-up, this decrease was discordant with parent quality-of-life scores. Rural individuals may perceive health as the ability to work, function, and perform daily tasks with their primary focus to be independent, self-reliant, and free from pain (37). Work and daily pressures play a primary role in one’s perception of health in rural families (38) and the ability to work is very important for rural individuals (21). Consequently, asthma symptoms in children may be tolerated for a longer period in rural families as long as the child can work or attend school and this may be perceived as good quality of life. Lack of variation in child quality-of-life scores may be related to the child’s cognitive developmental level and circumstances related to the measurement of quality of life including the developmental level of the instrument (39). For example, by first grade, children can understand the consequence of their illness, “not hurting,” and knowledge about routine medical examinations (40) but they may not be able to understand “worried or bothered about my asthma” as worded on the child quality-of-life instrument.
Although the cost of the educational program was $95.00 per family, expenses were associated with research nurse and community health worker personnel and travel costs to conduct the educational sessions. Use of school nurses to deliver the educational program after school or during Parent-Teacher Association (PTA) meetings would significantly reduce the cost of the program. Although the education program was not associated with reduction in ED visits, prevention of one emergency room visit at an average cost of $383.29 (41) would offset the cost of the educational program. The reduction in cost associated with lower frequency of symptom days is difficult to measure but is most likely associated with a reduction in caregiver stress.
This study is potentially limited by its cross-sectional design resulting in an inability to identify associations and not establish causation. Although severity decreased at follow-up, asthma severity as reported was assessed over a 6-month period and was subject to seasonal variation. Because asthma severity is not static and there is no gold standard for measurement of asthma severity (42), we cannot exclude some mis-classification of severity assignment in this sample. The study relied on a structured caregiver interview so it is possible that caregiver reports of asthma symptoms, school absences, and medication use were subject to recall bias. External validation of these characteristics was not performed. In addition, this sample may be biased toward families who were more concerned about or in need of asthma education and services.
In summary, an interactive child and parent asthma educational intervention for rural families significantly increased parent and young child asthma knowledge as well as child self-efficacy but not quality of life in either group. Rural children and their families may benefit from interactive and individualized asthma education. In particular, young rural children may benefit from interactive asthma education that enables them to learn and practice asthma management skills resulting in better asthma control. Rural health beliefs may explain the lack of change in parent reports of their quality of life. Families living in rural settings may tolerate a higher level of asthma symptoms and burden of asthma care in that rural families may believe the child can continue to work and attend school despite experiencing asthma symptoms. Future studies should address factors associated with improving parent self-efficacy and ultimately quality of life for both parents and children.
Acknowledgments
This study was funded by the National Institute of Nursing Research, NIH (NR05062). The authors thank Teresa Smith, RN, and Ann Brewer for their assistance with this project and the families for their willingness to participate in this study.
References
- 1.Centers for Disease Control and Prevention. Surveillance for asthma- United States. MMWR. 1998;47:1–27. (no. SS-1) [Google Scholar]
- 2.Akinbami LJ, Schoendorf KC. Trends in childhood asthma: Prevalence, health care utilization and mortality. Pediatrics. 2002;110(2 Pt 1):315–322. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- 3.Chrischilles E, Ahrens R, Kuehl A, Kelly K, Thorne P, Bermeister L, Merchant J. Asthma Prevalence and morbidity among rural Iowa schoolchildren. J Allergy Clin Immunol. 2004;113(1):66–71. doi: 10.1016/j.jaci.2003.09.037. [DOI] [PubMed] [Google Scholar]
- 4.Merchant JA, Naleway AL, Svendsen ER, Kelly KM, Burmeister LF, Stromquist AM, Taylor CD, Thorne PS, Reynolds SJ, Sanderson WT, Chrischilles EA. Asthma and farm exposure in a cohort of rural Iowa children. Environ Health Perspect. 2005;113:350–356. doi: 10.1289/ehp.7240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horner SD, Fouladi RT. Home asthma management for rural families. J Soc Pediatric Nurs. 2003;8:52–61. doi: 10.1111/j.1744-6155.2003.tb00187.x. [DOI] [PubMed] [Google Scholar]
- 6.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 7.Evans D, Clark NM, Feldman CH, Rips J, Kaplan D, Levison MJ, Wasilewski Y, Levin B, Mellins RB. A school health education program for children with asthma aged 8–11 years. Health Education Quarterly. 1987;14:267–279. doi: 10.1177/109019818701400302. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JM. Empowering patients: Issues and strategies. Soc Sci Med. 2000;43:697–705. doi: 10.1016/0277-9536(96)00153-0. [DOI] [PubMed] [Google Scholar]
- 9.Clark NM, Brown R, Joseph CLM, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades and absenteeism. Chest. 2004;125:1674–1679. doi: 10.1378/chest.125.5.1674. [DOI] [PubMed] [Google Scholar]
- 10.Guevara JP, Wolf FM, Grum CM, Clark NM. Effects of educational interventions for self management of asthma in children and adolescents: Systematic review and meta-analysis. Brit Med J. 2003;326(7402):1–6. doi: 10.1136/bmj.326.7402.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiang LC, Huang JL, Yeh KW, Lu CM. Effects of a self-management asthma educational program in Taiwan based on PRECEDE-PROCEED model for parents with asthmatic children. J Asthma. 2004;41:205–215. doi: 10.1081/jas-120026078. [DOI] [PubMed] [Google Scholar]
- 12.Barlow JH, Ellard DR. Psycho-educational interventions for children with chronic disease, parents and siblings: An overview of the research evidence base. Child: Care, Health and Dev. 2004;30:637–645. doi: 10.1111/j.1365-2214.2004.00474.x. [DOI] [PubMed] [Google Scholar]
- 13.Halterman JS, Yoos HL, Conn KM, Callahan PM, Montes G, Neely TL, Szilagyi PG. The impact of childhood asthma on parental quality of life. J Asthma. 2004;41:645–653. doi: 10.1081/jas-200026410. [DOI] [PubMed] [Google Scholar]
- 14.Osman LM, Baxter-Jones ADG, Helms PJ. Parents’ quality of life and respiratory symptoms in young children with mild wheeze. Eur Respir J. 2001;17:254–258. doi: 10.1183/09031936.01.17202540. [DOI] [PubMed] [Google Scholar]
- 15.Grus CL, Lopez-Hernandez C, Delamater A, Applegate B, Brito A, Wurm G, Wanner A. Parental self-efficacy and morbidity in pediatric asthma. J Asthma. 2001;38:99–106. doi: 10.1081/jas-100000027. [DOI] [PubMed] [Google Scholar]
- 16.Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma. Qual Life Res. 1996;5:27–34. doi: 10.1007/BF00435966. [DOI] [PubMed] [Google Scholar]
- 17.Levy JI, Welker-Hood LK, Clougherty JE, Dodson RE, Steinbach S, Hynes HP. Lung function, asthma symptoms and quality of life for children in public housing in Boston: a case-series analysis. Environ Health. 2004;3:13–15. doi: 10.1186/1476-069X-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Asthma Education and Prevention Program (NAEPP) National Heart, Lung, and Blood Institute. 1997. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health Publication no. 97–4051. [Google Scholar]
- 19.National Asthma Education and Prevention Program (NAEPP) National Heart, Lung, and Blood Institute. 2002. The NAEPP Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma-Update on Selected Topics 2002. National Institutes of Health Publication no. 02–5075. [PubMed] [Google Scholar]
- 20.Yoos HL, Kitzman H, McMullen A, Sidora K. Symptom perception in childhood asthma: How accurate are children and their parents? J Asthma. 2003;40:27–39. doi: 10.1081/jas-120017204. [DOI] [PubMed] [Google Scholar]
- 21.Henson D, Chafey K, Butterfiled PG. Rural Health. In: Nies MA, McEwen M, editors. Community Health Nursing: Promoting the Health of Populations. 3. B. Saunders; Philadelphia: 2001. [Google Scholar]
- 22.Bursch B, Schwankovsky L, Gilbert J, Zeiger R. Construction and validation of four childhood asthma self-management scales: Parent barriers, child and parent self-efficacy and parent belief in treatment efficacy. J Asthma. 1999;36:115–128. doi: 10.3109/02770909909065155. [DOI] [PubMed] [Google Scholar]
- 23.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol. 1994;47:81–87. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 24.Wile DC, Hendricks CM. Using picture identification for research with preschool children. J Sch Health. 1998;68:227–230. doi: 10.1111/j.1746-1561.1998.tb06343.x. [DOI] [PubMed] [Google Scholar]
- 25.Childhood Asthma Management Program Research Group. The Childhood Asthma Management Program (CAMP) Design, Rationale and Methods. Control Clin Trials. 1999;20:91–120. [PubMed] [Google Scholar]
- 26.Juniper EF, Guyatt GH, Feeny DH, Ferrie DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in children with asthma. Qual Life Res. 1996;5:35–46. doi: 10.1007/BF00435967. [DOI] [PubMed] [Google Scholar]
- 27.Naumann PL, Huss K, Calabrese B, Smith T, Quartey R, Van de Castle B, Lewis C, Hill K, Walker J, Winkelstein M. A+ Asthma Rural Partnership Coloring for Health: An Innovative Rural Asthma Teaching Strategy. Pediatr Nurs. 2004;30:490–494. [PubMed] [Google Scholar]
- 28.Stata Statistical Software: Release 7.0. College Station, TX: Stata Corporation; 2001. [Google Scholar]
- 29.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2004. [Google Scholar]
- 30.Horner SD. Effect of education on school-age children’s and parents’ asthma management. J Soc Pediatr Nurs. 2004;9:95–112. doi: 10.1111/j.1547-5069.2004.00095.x. [DOI] [PubMed] [Google Scholar]
- 31.Christiansen SC, Martin SB, Schleicher NC, Koziol JA, Mathews KP, Zuraw BL. Evaluation of a school-based asthma education program for inner-city children. J Allergy Clin Immunol. 1997;100:613–617. doi: 10.1016/s0091-6749(97)70164-7. [DOI] [PubMed] [Google Scholar]
- 32.Barrett JC, Gallien E, Dunkin J, Ryan L. Managing asthma within the context of the rural family. Pub Health Nurs. 2001;18:385–391. doi: 10.1046/j.1525-1446.2001.00385.x. [DOI] [PubMed] [Google Scholar]
- 33.Piaget J. The Origins of Intelligence in Children. New York: International Press; 1952. [Google Scholar]
- 34.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 35.Clark N, Starr-Schneidkraut N. Management of asthma by patients and families. Am J Resp Crit Care Med. 1994;149(2 Pt 2):S54–S66. doi: 10.1164/ajrccm/149.2_Pt_2.S54. [DOI] [PubMed] [Google Scholar]
- 36.LaLande R. Do training programs for asthma educators have an impact on asthma-related morbidity: How do we assess their effectiveness? Canadian Respir J. 1996;3:11–16A. [Google Scholar]
- 37.Weinert C, Burman M. Rural health and health-seeking behaviors. Annu Rev Nurs Res. 1994;12:65–92. [PubMed] [Google Scholar]
- 38.Carson D. Hardiness as a mediator of the effects of stressors and strains on reported illnesses and relational difficulties in farm and ranch families. J Rural Health. 1993;9:215–226. [Google Scholar]
- 39.Eiser C, Morse R. The measurement of quality of life in children: Past and future perspectives. J Dev Behav Pedaitr. 2001;22:248–256. doi: 10.1097/00004703-200108000-00007. [DOI] [PubMed] [Google Scholar]
- 40.Goldman SL, Whitney-Saltiel D, Granger J, Rodin J. Children’s representations of “everyday” aspects of health and illness. J Pediatr Psychol. 1991;16:747–766. doi: 10.1093/jpepsy/16.6.747. [DOI] [PubMed] [Google Scholar]
- 41.Williams RM. The costs of visits to emergency departments. N Engl J Med. 1996;334:642–646. doi: 10.1056/NEJM199603073341007. [DOI] [PubMed] [Google Scholar]
- 42.Vollmer WM, Markson LE, O’Connor E, Sanocki LL, Fitterman L, Berger M, Buist AS. Association of asthma control with health care utilization and quality of life. Am J Respir Crit Care Med. 1999;160(5 Pt 1):1647–1652. doi: 10.1164/ajrccm.160.5.9902098. [DOI] [PubMed] [Google Scholar]


