Abstract
Background
Much remains to be known about the mechanisms by which O2-dependent host defenses mediate broad antimicrobial activity.
Methodology/Principal Findings
We show herein that reactive nitrogen species (RNS) generated by inducible nitric oxide (NO) synthase (iNOS) account for the anti-Burkholderia mallei activity of IFNγ-primed macrophages. Inducible NOS-mediated intracellular killing may represent direct bactericidal activity, because B. mallei showed an exquisite sensitivity to NO generated chemically. Exposure of B. mallei to sublethal concentrations of NO upregulated transcription of [Fe-S] cluster repair genes, while damaging the enzymatic activity of the [Fe-S] protein aconitase. To test whether [Fe-S] clusters are critical targets for RNS-dependent killing of B. mallei, a mutation was constructed in the NO-induced, [Fe-S] cluster repair regulator iscR. Not only was the iscR mutant hypersusceptible to iNOS-mediated killing, but its aconitase pool was readily oxidized by NO donors as compared to wild-type controls. Although killed by authentic H2O2, which also oxidizes [Fe-S] clusters, B. mallei appear to be resilient to NADPH oxidase-mediated cytotoxicity. The poor respiratory burst elicited by this bacterium likely explains why the NADPH oxidase is nonessential to the killing of B. mallei while it is still confined within phagosomes.
Conclusions/Significance
Collectively, these findings have revealed a disparate role for NADPH oxidase and iNOS in the innate macrophage response against the strict aerobe B. mallei. To the best of our knowledge, this is the first instance in which disruption of [Fe-S] clusters is demonstrated as cause of the bactericidal activity of NO congeners.
Introduction
The gram negative, nonmotile B. mallei bacillus is the causative agent of glanders, a disease that can be transmitted to humans upon cutaneous, mucosal or aerosol exposure to mucopurulent discharge from the eyes, nose and lips of infected solipeds [1]. The clinical presentation of glanders is characterized by an acute or chronic suppurative syndrome involving the upper and lower respiratory tract. If untreated, the local signs of glanders often evolve into full-blown sepsis, multiorgan system failure and shock. The poor understanding of the pathogenesis of glanders, the severity and clinical diversity of the infection and a lack of vaccines make B. mallei a desirable bioterrorist agent as has been demonstrated empirically in humans and animals in both World War I and II [2].
Pathogens adapted to an intracellular lifestyle avoid competition with other microbes that colonize host surfaces, while taking advantage of the nutritional resources provided by the cell. The cost of intracellular parasitism is the potential exposure to a variety of host defenses. For example, intracellular pathogens may encounter the O2-dependent antimicrobial mechanisms that are coupled to NADPH oxidase and iNOS enzymatic activities. The NADPH phagocyte oxidase is assembled on endocytic or plasma cell membranes, whereupon it catalyzes the NADPH-dependent univalent reduction of O2 to superoxide (O2 •−). This radical serves as precursor to a variety of reactive oxygen species (ROS) endowed with widespread antimicrobial activity [3]. The electrogenic nature of the NADPH oxidase may also contribute to the host cell arsenal by promoting the release of cationic proteases from the proteoglycan matrix into the phagosomal lumen [4]. Professional phagocytes independently use O2 and NADPH in the oxidation of L-arginine with the consequent generation of L-citrulline and NO [5]. Similar to ROS, products of the reaction of NO with O2, O2 •− and metals are endowed with antimicrobial activity against phylogenetically diverse microorganisms [6].
Recent investigations have demonstrated that members of the genus Burkholderia survive within mononuclear phagocytes [7], prompting an interest in the role of ROS and RNS in defense against these bacteria [8]–[12]. The importance that the NADPH oxidase plays in resistance to some Burkholderia spp. is made evident by the fact that B. cepacia is the second most lethal infection in chronic granulomatous disease patients carrying mutations in membrane-bound or cytosolic components of the NADPH oxidase [13]. The clinical importance of NADPH oxidase in resistance to B. cepacia has been recreated in p47phox-deficient mice [14]. The NADPH oxidase has also been linked to the anti-B. pseudomallei arsenal of macrophages [12]. In contrast to ROS, current investigations on NO-related anti-Burkholderia activity have been rather controversial. Experimental animal models and macrophage cell cultures have shown that iNOS is dispensable for innate host defense against B. cepacia and B. pseudomallei [12], [14]. Moreover, others have shown that the greatest Burkholderia growth occurs during maximal NO synthesis [8]. Inhibition of iNOS mRNA transcription appears to underlie the lack of a role of RNS against B. pseudomallei [9], [10]. On the other hand, IFNγ can enhance NO-mediated intracellular killing of B. pseudomallei [11]. Recently, it has been reported that B. mallei is susceptible to NO generated by macrophages [15], although the mechanisms of antimicrobial activity remain unclear. Similarly, it remains unclear whether the NADPH oxidase plays a role in resistance to the intracellular pathogen B. mallei. The major goal of this study was to characterize the contribution of NADPH oxidase and iNOS hemoproteins to the macrophage antimicrobial arsenal against B. mallei.
Methods
Bacterial Strains and genetic manipulations
B. mallei strain ATCC 23344 was used in these studies (table 1). Bacteria grown overnight in 10 ml of Luria Bertani broth supplemented with 4% glycerol (LBG) at 37°C in a 315 RPM shaking incubator were sub-cultured into pre-warmed LBG and grown to an OD600 of 0.6. The B. mallie iscR homologue, locus BMA1709, was disrupted by inserting a 400 bp internal region of the BMA 1709 using homologous recombination. The 400 bp internal region was amplified by PCR using an iscR forward primer containing a BamHI restriction site (5′-tgactacggatccgcccggtgacgcttgcaggcatcag-3′) and the iscR reverse primer containing an SphI restriction site (5′-aagcccgtcgcatgcgcgacgggctccggcttgcgcttg-3′). After double digestion with BamHI and SphI, the PCR product was directionally cloned into the suicide vector pMO90, creating the disruption plasmid pMO126. pMO126 was introduced into B. mallei using triparental mating [16] in the presence of the helper E. coli DH5α pRK2013 strain [17]. Mating reactions were plated on LB agar plates supplemented with 30 µg/ml kanamycin to select for transconjugants, and 20 µg/ml polymyxin B to select against the helper and donor E. coli strains. The resulting colonies were re-streaked for isolation on LB plates supplemented with 30 µg/ml kanamycin and 20 µg/ml polymyxin B. Insertion of pMO126 into the B. mallei genome and the disruption of BMA 1709 was confirmed by PCR. The replicative plasmid pMO79 encoding a green fluorescence protein was conjugated into B. mallei strain ATCC 23344 by triparental mating as described above. The presence of pMO79 in B. mallei was confirmed by fluorescence microscopy.
Table 1. Bacterial strains and Plasmids.
| Strains/Plasmids | Relevant properties | Description | Source |
| B. mallei ATCC 23344 | Wild type | Isolated in 1944 from a human case of glanders: Gms, Pbr | [50] |
| B. mallei Mo126.2 | iscR mutant | bma1709::pMO126 | This study |
| S. Typhimurium BC696 | fliC− fljB− | SL1344 ΔfliC ΔfljB | [51] |
| DH5α | DH5α harboring pRK2013 | F− ø80lacZM15 endA1 recA1 hsdR17(rK− mK+) supE44 thi-1 ΔgyrA96 relA1Δ (lacZYA-argF)U169] | Laboratory stock |
| JM109 | Cloning strain harboring pMO79 & pMO126 | e14−(McrA−) recA1 endA1 gyrA96 thi-1 hsdR17 (rK− mK+) supE44 relA1 Δ(lac-proAB) [F′ traD36 proAB lacIqZΔM15] | Stratagene |
| pRK2013 | Helper plasmid | RK2 derivative, Kanr mob + tra + ColE1 | [16] |
| pMO79 | Mobilizable replicative plasmid | oripBBR1 Kanr mob+ gfp rfp | Hamad & Voskuil |
| pMO90 | Mobilizable siucide plasmid | ColE1 Kanr mob + gfp xyle | Hamad & Voskuil |
| pMO126 | Mobilizable disruption plasmid | pMO90 carrying an internal fragment of the B. mallei iscR homologue | This study |
Gms = gentamicin sensitive.
Pbr = polymixin B resistant.
Kmr = kanamycin resistant.
Macrophages
C57BL/6 and congenic iNOS−/− [18] or gp91phox−/− [19] mice were bred in our animal facility according to Institutional Animal Care and Use Committee guidelines. Peritoneal macrophages were harvested from mice 4 days after intraperitoneal inoculation of 1 mg/ml sodium periodate as described [20]. The peritoneal exudate cells were resuspended in RPMI 1640 medium (Sigma-Aldrich, St. Louis, MO) supplemented with 10% heat-inactivated fetal bovine serum (BioWhittaker, Walkersville, MD), 15 mM Hepes, 2 mM L-glutamine, 1 mM sodium pyruvate (Sigma-Aldrich), and 100 U ml−1/100 mg ml−1 of penicillin/streptomycin (Cellgro) (RPMI+ medium). The RPMI+ medium used to culture the THP-1 cell line was supplemented with 50 µM 2-mercaptethanol. The peritoneal exudate cells were seeded in flat-bottom 96-well plates for macrophage killing assays at a density of 2×105 cells per well. The macrophages were selected by adherence after 24 h of culture at 37°C in a 5% CO2 incubator. Murine J774 (clone ATCC TIB-67) and AMJ2-C11 (clone ATCC CRL-2456) and human U937 (clone ATCC CRL-1593.2) and THP1 (clone ATCC TIB-202) macrophage-like cells grown in RPMI+ medium supplemented as described above were used as additional sources of mononuclear phagocytes. Selected groups of macrophages were treated with 200 U/ml of IFNγ (Life Technologies, St. Paul, MN) overnight prior to Burkholderia infection. Just prior to infection the macrophages were washed with pre-warmed RPMI without antibiotics.
Macrophage killing assays
The macrophage killing capacity was quantified by a gentamicin protection assay following a modified protocol described for Salmonella [21]. B. mallei were grown overnight in LBG broth and sub-cultured to OD600 of 0.6 as described above. The bacteria were spun down for 5 min at 1500 RPM onto the macrophages at an MOI of 200 after opsonization in 10% normal mouse serum in RPMI+ medium. Unless specified, extracellular bacteria were removed from the monolayers after a 2 h incubation by washing with pre-warmed RPMI+ medium containing 6 µg/ml of gentamicin (Sigma-Aldrich). After washing the noninternalized bacteria, the MOI was determined to be 10. Burkholderia-infected macrophages were lysed with 1% Triton X-100 in phosphate buffered saline (PBS) at the indicated times after challenge. The intracellular bacteria recovered at various points after infection were enumerated on LB agar plates. The % survival was calculated as (cfu tn/cfu t0)×100.
Superoxide anion determination
O2 •− was quantified by the superoxide dismutase–inhibitable reduction of ferricytochrome c [22]. The macrophages were infected at an MOI of 40 with Burkholderia resuspended in phenol red–free Earle's balanced salt solution containing 60 µM ferricytochrome c. Because B. mallei is aflagellated, a strain of Salmonella enterica serovar Typhimurium deficient in fliC fljB was used as a positive control. After 1 h incubation in 5% CO2 at 37°C, the OD of the supernatants was determined spectrophotometrically at 550 nm. The concentration of O2 •− was calculated by using an ε550 of 2.1×103 M−1 cm−1. All reagents were purchased from Sigma-Aldrich.
Nitrite measurement
The concentration of nitrite (NO2 −) produced by Burkholderia-infected macrophages 6 h post-challenge was estimated spectrophotometrically at 550 nm in a Biotek Synergy HT-2 reader after mixing culture supernatants with an equal volume of Griess reagent (0.5% sulfanilamide and 0.05% N-1-naphthylethylenediamide hydrochloride in 2.5% phosphoric acid). The NO2 − concentration was calculated by regression analysis using a NaNO2 standard curve.
Susceptibility to RNS and ROS in vitro
Overnight cultures of B. mallei diluted 1∶100 in LBG broth were grown at 37°C with shaking to OD600 of 0.6. Bacteria were concentrated by centrifugation and the pellets resuspended in PBS. The bacteria were diluted 1∶100 in PBS and incubated with spermine NONOate (Cayman Chemical, Ann Arbor, MI), H2O2 (ThermoFisher Scientific, Waltham, MI), or spermine (Sigma-Aldrich, St. Louis, MO) at 37°C. At the end of the incubation, 200 units of catalase (Sigma-Aldrich, St. Louis, MO) were added to the H2O2-treated samples to consume any remaining H2O2. Serial dilutions were spotted on LBG agar plates and the number of colony forming units counted after 48 h of culture.
Microarrays
RNA from B. mallei was isolated in Triazol reagent from cultures grown to an OD600 of 0.1 in LB medium. Selected cultures were treated with 1 mM DEANO for 30 min before the isolation of the RNA. Synthesized cDNA was labeled as previously described for Mycobacterium tuberculosis [23] with the following changes. An additional phenol/chloroform extraction was added to clean the RNA after isolation. The resulting RNA was further purified using a Qiagen RNeasy kit. 5 µg RNA were used for cDNA synthesis. After cDNA synthesis, the samples were further purified by phenol/chloroform extraction followed by concentration using a microcon YM-30 column (Millipore, Bedford, MA). Hybridization reactions contained 5 µl cDNA, 1 µl yeast tRNA (Sigma), and 15 µl hybridization solution (400 µl formamide, 239 µl H2O, 250 µl 20× SSC, 10 µl 10% SDS 10 µl). Samples were heated at 98°C for 2 min, cooled 5 min at 25°C and placed on pre-hybridized Burkholderia array slides (Colorado State University RM-RCE Genomics Core). Hybridization was conducted in standard hybridization chambers overnight in a 42°C water bath and washed with 1× SSC and 0.05% SDS, followed by two washes in 0.06× SSC. The slides were scanned using a Genepix Axon 4000B scanner. Initial data analysis was conducted using Genepix Pro software, followed by analysis using Microsoft Excel as described [23].
Aconitase enzymatic assay
3 mL of stationary phase B. mallei grown in LBG medium were pelleted by centrifugation and resuspended in an equal volume of LB medium. Selected cultures containing 36 OD were treated with either 500 µM or 1 mM spermine NONOate for 30 min. The cultures were pelleted by centrifugation at 4°C, washed with 50 mM Tris-HCl buffer, pH 7.6 and the cytoplasmic proteins extracted in 400 µL B-PER (Pierce, Rockford IL) after vortexing for 30 sec. The samples were diluted 1∶2 in 50 mM Tris-HCL buffer, pH 7.6. After removing the insoluble fraction by centrifugation, the supernatants were filter-sterilized. Aconitase activity in the soluble fractions was estimated spectrophotometrically at 240 nm by following the formation of cis-aconitate in 50 mM Tris-HCl buffer pH 7.4 containing 30 mM isocitrate. Aconitase activity is expressed as ΔOD240/min/µg protein.
Electron microscopy
The phagocytes were plated as described above for killing assays at a density of 4×105 per chamber of a 8-well Permanox Labtek chamber slide system (Nalgene Nunc International, Rochester, NY). The macrophages were challenged with B. mallei at an MOI of 10 as described above. Between 2 and 3.5 h after infection, the cells were fixed in 2.5% glutaraldehyde in phosphate buffer, pH 7.4. The specimens were postfixed in 1% osmium tetraoxide, treated with uranyl acetate, dehydrated in ascending ethanol series, and infiltrated with Embed 812. Ultrathin sections were examined in a FEI Technai 62 electron microscope operated at 80 kV.
Fluorescence microscopy
Macrophages plated on 13 mm glass coverslips in a 24-well plate at a density of 2.5×105 cells/well were infected as described above with GFP-expressing B. mallei. The specimens were washed in PBS 3 h after infection and fixed overnight at 4°C in 2% paraformaldehyde (Electron Microscopy Sciences, Hatfield, PA) diluted in PBS. After fixation, the coverslips were washed in PBS and the cells were permeablized for 5 min with 0.1% Triton X-100 in PBS. After washing, F-actin was visualized by labeling the infected macrophages with Alexa Fluor 568 phalloidin (Invitrogen). The coverslips were washed with PBS and mounted onto glass slides prepped with Vectashield mounting medium containing DAPI nucleic acid stain (Vectashield Laboratory, Burlingame, CA). The specimens were examined with a Zeiss Axiophot fluorescence microscope equipped with a charge-coupled-device camera controlled by the SlideBook deconvolution image-processing software (Intelligent Imaging Innovations, Denver, CO).
Statistical analysis
Data are presented as mean ± SEM or in box-and-whiskers plots as median, intraquartile and total ranges. A two-tailed, Student's t-test was used for statistical analysis and the data considered statistically significant when p<0.05.
Results
Survival of B. mallei in human and murine cell lines
The number of log phase B. mallei internalized by J774 cells increased as a function of time, reaching approximately 106 CFU/105 macrophages 2 h after infection. Because of this delay phagocytosis, all subsequent Burkholderia infections, unless indicated, were carried out for 2 h before gentamicin was added to the medium. Mice offer a wide variety of genetic reagents that facilitate investigations of O2-dependent host defenses in host–pathogen interactions. Therefore, we deemed it important to compare the intracellular growth of B. mallei in a number of murine (J774 and alveolar AMJ-C11 macrophages) and human (i.e., THP1 and U937) cell lines (fig. 1). Remarkably, all murine and human macrophage-like cell lines tested killed B. mallei with very similar kinetics. These findings indicate that murine macrophages are a relevant model in which to study B. mallei-phagocyte interactions.
Figure 1. Antimicrobial activity of murine and human macrophage-like cell lines against B. mallei.
Intracellular survival of B. mallei was studied over a 20 h period in murine (i.e., J774 and AMJ) and human (i.e., THP1 and U937) macrophage-like cell lines. Data from 8–14 independent observations gathered in 3 separate experiments are represented in box-and-whiskers plots as median, intraquartile and total ranges.
IFNγ enhances killing of B. mallei by macrophages
It has been shown that IFNγ enhances the antimicrobial activity of macrophages against the opportunistic pathogen B. pseudomallei. However, to our knowledge, no data are available on the role that IFNγ plays in intracellular resistance to B. mallei. Because IFNγ has recently been shown to be critical for resistance of mice to B. mallei [24], we tested the effect of IFNγ treatment on the anti-Burkholderia activity of J774 cells (fig. 2). IFNγ-primed macrophages were significantly (p<0.01) more efficient at killing B. mallei than unstimulated controls. The number of B. mallei recovered from IFNγ-treated macrophages was at least 10-fold lower than controls (fig. 2). In some cases, IFNγ-primed J774 cells completely eliminated the bacteria from the cell cultures. These data demonstrate that IFNγ enhances the innate resistance of murine macrophages to B. mallei.
Figure 2. Anti-Burkholderia activity of IFNγ-primed macrophages.

The intracellular survival of B. mallei was assessed in control and IFNγ-primed J774 cells. Selected groups of macrophages were treated with 200 U/ml IFNγ 16 h before infection. Data from 6 independent observations gathered on 2 separate experiments are represented in box-and-whiskers plots as median, intraquartile and total ranges. *P<0.01 compared to unstimulated control macrophages.
Reactive oxygen and nitrogen species differentially contribute to the anti-B. mallei activity of IFNγ-primed macrophages
ROS and RNS are key components of the antimicrobial arsenal of the innate and the activated response of macrophages against a variety of intracellular pathogens [25]. To test the importance of ROS and RNS in the killing of B. mallei, macrophages were obtained from C57BL/6 mice and their congenic gp91phox −/−, iNOS−/− and gp91phox −/−/iNOS−/− immunodeficient strains. Unstimulated macrophages isolated from C57BL/6 mice killed over 99% of B. mallei within 5 h of infection (fig. 3A). Strikingly, singly or doubly immunodeficient macrophages lacking gp91phox and/or iNOS hemoproteins exhibited similar bactericidal activity as that of unstimulated wild-type controls. These findings suggest that neither ROS nor RNS appear to play a significant role in the early killing of B. mallei by unstimulated macrophages. Similar to the improved killing seen in the J774 cell line, IFNγ increased (p<0.001) the anti-B. mallei activity of primary macrophages isolated from C57BL/6 mice. It should be noted that some of the IFNγ-primed macrophages completely eliminated B. mallei from the cultures, a phenomenon that was seen in all of the IFNγ-primed, gp91phox-deficient macrophages (fig. 3B). These findings suggest that ROS are dispensable for the anti-B. mallei activity of IFNγ-primed macrophages. Conversely, RNS contributed to the anti-B. mallei arsenal of IFNγ-activated macrophages (fig. 3B). In fact, this intracellular pathogen was recovered in significantly higher numbers from both IFNγ-primed, iNOS−/− and iNOS−/−/gp91phox −/− macrophages than from wild-type or gp91phox −/− controls. The killing activity of IFNγ-treated, iNOS- or iNOS/gp91phox- deficient macrophages was similar to that of unstimulated wild-type controls. Collectively, these data indicate that RNS but not ROS mediate the anti-Burkholderia activity of IFNγ-primed macrophages, while neither RNS nor ROS appear to add to the early innate host defenses of macrophages against B. mallei.
Figure 3. Contribution of reactive oxygen and nitrogen species to the anti-Burkholderia activity of macrophages.
The contribution of ROS and RNS to host defense against B. mallei was assessed by comparing the antimicrobial activity of primary macrophages isolated from immunocompentent C57BL/6 mice (control) or congenic phox−/−, iNOS−/− or phox−/−iNOS−/−-immunodeficient mice. Selected groups of macrophages were treated with 200 U/ml IFNγ 16 h before infection. The number of B. mallei recovered from the macrophages was estimated 5 h after the infected macrophages were treated with gentamicin. Data from 16 independent observations gathered on 3 separate experiments are represented in box-and-whiskers plots as median, intraquartile and total ranges. *P<0.05 compared to unstimulated control macrophages. **P<0.05 compared to IFNγ-primed macrophages from C57BL/6 mice.
B. mallei is susceptible to RNS
The poor anti-Burkholderia activity of IFNγ-primed macrophages lacking iNOS suggest that RNS generated by activated phagocytes exert early antimicrobial activity against B. mallei. Consequently, the ability of macrophages to produce NO in response to B. mallei infection was tested by measuring the accumulation of NO2 −. Supernatants of B. mallei-infected J774 cells contained about 200 µM NO2 − after 5 h of infection (fig. 4A). The concentration of NO2 − seen in B. mallei-infected cells closely paralleled the NO3 − levels contained in RPMI medium, raising the possibility that a bacterial nitrate reductase activity is responsible for the observed NO2 − burst. This idea was substantiated by the fact that the putative B. mallei nitrate reductase activity could be inhibited by the flavoprotein inhibitor diphenyleneiodonium (fig. 4A). To determine whether host cell iNOS activity can be stimulated upon B. mallei challenge, the capacity of macrophages to generate NO2 − was therefore estimated in NO3 −-free medium. As shown in figure 4B, IFNγ-primed macrophages, but not unstimulated controls, generated copious amounts of NO congeners in response to B. mallei. Accumulation of NO2 − in the supernatants reflects a functional iNOS enzymatic complex, since the amount of NO2 − generated by iNOS-deficient macrophages was negligible. Figure 4C shows that B. mallei are extraordinarily susceptible to RNS. Spermine NONOate reduced the viability of B. mallei in a dose and time dependent manner (fig. 4C & D). The viability of B. mallei was significantly reduced after a 4 h exposure to as low as 10 µM of the NO donor spermine NONOate (fig. 4C). A time course indicated that the killing of B. mallei by 100 µM spermine NONOate was already evident after 30 min and continued unabated for at least 2 h (fig. 4D). The anti-B. mallei effects associated with spermine NONOate are specific to RNS generated by this NO donor, since the viability of B. mallei was similarly unaffected upon culture in PBS or exposure to the spermine base control.
Figure 4. Antimicrobial activity of reactive nitrogen species generated by Burkholderia-infected macrophages.
The ability of B. mallei to generate NO2 − in RPMI+ medium is shown in A. Selected samples were treated with 10 µM of the flavin inhibitor diphenyleneiodonium (DPI). The NO2 −-producing capacity of macrophages responding to B. mallei was assessed in low NO3 − DMEM medium (B). The survival of B. mallei to increasing concentrations of the NO donor spermine NONOate is shown in C. The effects of 100 µM spermine NONOate on the viability of B. mallei was studied overtime (D). Untreated or spermine-treated B. mallei were used as controls. Data in panel A are represented in box-and-whiskers plots as median, intraquartile and total ranges. The rest of the data represent the mean ± sem.
NO enhances transcription of genes associated with [Fe-S] cluster assembly
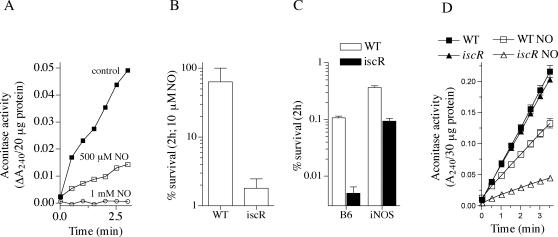
To gain insight into the targets of RNS antimicrobial activity, global transcriptional profiles were compared between B. mallei cultures untreated or treated with sublethal NO concentrations. Microarray expression analyses showed the transcriptional up-regulation of gene products involved in iron acquisition and [Fe-S] cluster assembly and repair (table 2). This pattern of transcription suggests that [Fe-S] clusters of dehydratases are critical B. mallei targets of RNS-mediated cytotoxicity. Accordingly, the enzymatic activity of the [Fe-S] cluster protein aconitase was markedly reduced in B. mallei cultures treated with spermine NONOate. For instance, about 100 pmoles of NO per 106 bacteria completely inactivated the activity of aconitase (fig. 5A). To test more directly whether [Fe-S] clusters are a key target of the anti-B. mallei activity of RNS, an insertion mutant was constructed in the iscR transcriptional factor that regulates [Fe-S] cluster assembly. The lack of iscR increased the susceptibility of B. mallei to RNS generated by the NO donor spermine NONOate (fig. 5B). We next tested whether the iscR mutant is susceptible to NO produced by activated macrophages. Because wild-type B. mallei is already highly susceptible to the iNOS-mediated antibacterial activity of IFNγ-primed macrophages after 5 h of infection (fig. 3B), the survival of wild-type and iscR-deficient B. mallei was compared after 2 h of challenge. As anticipated (fig. 5B), at this early time the iscR mutant was more susceptible than wild-type controls to the antimicrobial activity of IFNγ-primed macrophages (fig. 5C). The difference in intracellular survival of wild-type and iscR-deficient bacteria was not as great in IFNγ-primed macrophages lacking iNOS compared to those containing iNOS (fig. 5C). These data suggest that iscR mutant bacteria are hypersusceptible to the RNS generated by the host cells. The aconitase activity of the iscR mutant grown overnight in LBG medium was similar to that of wild-type controls (fig. 5D). However, the enzymatic activity of aconitase was more vulnerable to RNS-mediated inactivation in the absence of a functional iscR. Together, these findings are consistent with the notion that [Fe-S] clusters are key targets of the RNS-dependent bactericidal activity against B. mallei.
Table 2. Iron-sulfur cluster assembly genes induced by nitric oxide.
| Gene No. | Gene | Ratio | St.Dev. | Protein Function | Pathway |
| BMA2033 | 2.7 | 1.4 | iron compound ABC transporter | iron assimilation | |
| BMAA0021 | 4.6 | 1.3 | siderophore-interacting protein | iron assimilation | |
| BMAA0883 | 4.5 | 2.7 | iron permease, FTR1 family | iron assimilation | |
| BMAA1800 | 14.1 | 3.0 | putative bacterioferritin-associated ferredoxin | iron assimilation | |
| BMA0666 | cysD-1 | 3.5 | 0.7 | sulfate adenylyltransferase, subunit 2 | sulfur assimilation |
| BMA0667 | cysN | 4.3 | 0.5 | sulfate adenylyltransferase, subunit 1 | sulfur assimilation |
| BMA2729 | 2.2 | 0.4 | sulfur carrier protein | sulfur assimilation | |
| BMA0610 | sufS | 3.8 | 1.7 | cysteine desulfurase | [Fe-S] assembly |
| BMA1706 | 3.3 | 0.1 | [Fe-S] assembly accessory protein | [Fe-S] assembly | |
| BMA1707 | iscU | 2.3 | 0.7 | [Fe-S] assembly scaffold | [Fe-S] assembly |
| BMA1708 | iscS-1 | 3.9 | 0.5 | cysteine desulfurase | [Fe-S] assembly |
| BMA1709 | iscR | 6.9 | 2.9 | [Fe-S] assembly transcription factor | [Fe-S] assembly |
| BMAA1430 | 2.0 | 0.5 | [Fe-S] binding protein | [Fe-S] assembly |
Figure 5. iscR-deficient B. mallei is hypersusceptible to NO-mediated cytotoxicity.
The aconitase activity of B. mallei exposed to spermine NONOate (NO) for 30 min can be seen in panel A. Panel B shows the cytotoxicity of 10 µM spermine NONOate against wild-type (WT) or iscR-deficient B. mallei. The intracellular survival of WT and isogenic iscR-deficient B. mallei was recorded in IFNγ-treated macrophages isolated from wild-type C57BL/6 mice (B6) or iNOS-deficient congenic controls (C). The % survival after 2 h of infection was estimated according to the number of bacteria originally added to the macrophages. The aconitase activity present in overnight cultures of wild-type or iscR-deficient B. mallei is shown in D. Selected groups of bacteria were treated with 500 µM spermine NONOate for 30 min before the aconitase activity present in cytoplasmic extracts was recorded. Panels A & D represent data of two independent experiments. Data in panel B & C are the mean ± sem from 4–8 independent observations.
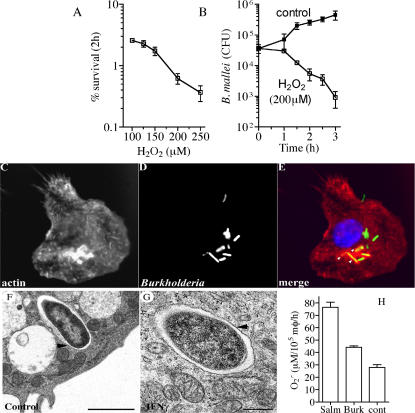
B. mallei is resistant to the oxidative burst of macrophages despite its marked susceptibility to ROS
We investigated the possible mechanism for the apparent dispensability of the NADPH oxidase in the intracellular killing of B. mallei. B. mallei was found to be susceptible to authentic H2O2 (fig. 6A). As little as 100 µM H2O2 killed over 90% of B. mallei after 2 h. A kinetic study revealed that the viability of B. mallei was markedly reduced 90 min upon exposure to 200 µM H2O2, declining further thereafter (fig. 6B). These findings demonstrate that B. mallei are extraordinarily susceptible to ROS-mediated killing. The ability of Burkholderia to escape into the cytosol [26], [27] could rationalize the apparent dispensability of NADPH oxidase in the anti-B. mallei arsenal of macrophages. To test the intracellular localization of B. mallei, the ability of the bacterium to form actin-tails was evaluated by fluorescence microscopy. As shown in figure 6C–E, B. mallei do not appear to polymerize actin tails at the early times examined here, although polymerization of actin was evident in about 10% of the B. mallei-containing phagosomes (figure 6E). Electron microscopy studies revealed that the totality of B. mallei were found within phagosomes in both unstimulated and IFNγ-primed macrophages (fig. 6F and G). Collectively, the fluorescence and electron microscopy studies indicate that B. mallei remain within the confines of phagosomal membranes during the early stages of infection studied herein, irrespective of whether the phagocytes are stimulated with IFNγ (fig. 6F & G). We tested whether the seeming dispensability of the NADPH oxidase in the anti-B. mallei activity of macrophages was due to a poor respiratory burst. Estimates of O2 •− production by the superoxide dismutase-inhibitable reduction of cytochrome c revealed that B. mallei was a poor stimulant of the respiratory burst as compared to an aflagellated fliC fljB Salmonella control (fig. 6H).
Figure 6. Susceptibility of Burkholderia to ROS generated by macrophages.
The susceptibility of B. mallei to increasing concentrations of H2O2 is shown in A. Kinetic analysis of the viability of B. mallei in response to 200 µM H2O2 is shown in B. The cellular localization of phalloidin-labeled actin filaments (C) and GFP-expressing B. mallei (D) was examined by fluorescence microscopy. The host cell nucleus labeled with DAPI (blue), B. mallei (green) and actin (red) are visualized in the merge panel (E). The micrograph is representative of a total of 285 bacteria examined from 33 cells collected in 2 independent experiments. The location of B. mallei in the cytoplasm of control (F) and IFNγ-primed (G) macrophages from C57BL/6 mice was visualized by transmission electron microscopy 3.5 h after infection. Bars in F and G denote 2 and 0.5 µm, respectively. The micrographs are representative of 97 Burkholderia-containing phagosomes from 5 independent experiments. Production of superoxide by B. mallei-infected macrophages isolated from C57BL/6 mice was assessed spectrophotometrically as the superoxide dismutase-inhibitable reduction of cytochrome c (H). Data in panels A, B and G represent the mean ± sem from 6 independent observations.
Discussion
O2-dependent host defenses are the best-characterized components of the antimicrobial arsenal of professional phagocytes. O2 is used by NADPH oxidase and iNOS hemoproteins for the generation of O2 •− and NO, which are the precursors of a plethora of ROS and RNS. Pathogenic microorganisms show a spectrum of susceptibilities to the antimicrobial actions of RNS. For example, RNS are essential for resistance to Mycobacterium tuberculosis and Leishmania major [12], [28], but appear to be dispensable in host defense against Legionella pneumophila and Pseudomonas aeruginosa [25]. Similar to Mycobacterium and Leishmania, our investigations have shown that the intracellular pathogen B. mallei is highly susceptible to RNS-mediated host defenses. We find that the inactivation of [Fe-S] clusters is a major component of the anti-B. mallei activity of RNS.
Poor killing of B. mallei by IFNγ-treated macrophages lacking iNOS, irrespective of the NADPH oxidase status of the cell, suggests that the RNS-mediated killing of B. mallei does not depend on host-derived ONOO− synthesis. NO itself, nitrogen oxides derived from the autooxidation of NO in the presence of O2, or ONOO− generated in the bacterial cytoplasm from the reaction of NO with endogenous O2 •− represent a few of the RNS that may be responsible for the iNOS-dependent killing of B. mallei. B. mallei are extraordinarily susceptible to RNS as shown by the profound killing seen after treatment with 10 µM spermine NONOate. NO donors also exert antimicrobial activity against phylogenetically diverse microbes such as Candida albicans, Salmonella enterica and Escherichia coli [29]–[31]. However, NO donors, even when used at high micromolar or low millimolar concentrations, are cytostatic for these microbial pathogens. Therefore, our studies identify B. mallei as one of the few pathogens for which host-derived RNS are microbicidal.
Aconitase is inactivated upon incubation of B. mallei with NO congeners, possibly reflecting the RNS-dependent oxidation of the solvent exposed Feα in the [Fe-S] cluster [32], [33]. It is therefore not surprising that genes encoding for iron-sulfur cluster assembly are highly transcribed in NO-treated B. mallei. RNS-mediated oxidation of [Fe-S] clusters of dehydratases [33]–[36] has for a long time been seen as a concomitant event of cytotoxic, NO-producing macrophages [32]. However, a causative relationship between the oxidation of [Fe-S] clusters and killing by RNS has not been previously demonstrated. The rapid loss in viability and aconitase activity of an iscR mutant exposed to sublethal NO concentrations demonstrate a direct relationship between [Fe-S] cluster damage and the bactericidal activity of RNS against B. mallei. Oxidation of [Fe-S] prosthetic groups of dehydratases critical for intermediate metabolism may explain the bactericidal activity of RNS against the obligate aerobe B. mallei. According to our model, the overt resistance of facultative anaerobes to NO reflects the ability of these microbes to generate energy by switching from oxidative phosphorylation heavily dependent on RNS-modifiable dehydratases to fermentative pathways resilient to nitrosative stress. Future experiments will be needed to test this hypothesis.
Our data indicate that the NADPH oxidase is dispensable for intracellular killing of B. mallei. These findings might seem striking since B. mallei are readily killed upon exposure to H2O2. Microbes have devised an assortment of strategies to avoid NADPH oxidase-dependent cytotoxicity. For example, detoxification of oxyradicals by superoxide dismutases, catalases and hydroperoxydases or scavengers such as low molecular weight thiols are efficient ways to diminish oxidative stress [6]. The antimicrobial activity of the NADPH oxidase is best manifested against intracellular pathogens confined within endocytic membranes [37], [38]. At the early times examined here, B. mallei do not escape into the cytosol as has been shown for various Burkholderia spp. at later time points after infection [27], [39]. The poor respiratory burst elicited by B. mallei represents a mechanism for minimizing exposure to the NADPH oxidase during the time that this intracellular pathogen remains in the phagosome. Analogous to other microorganisms [40], the putative polysaccharide extracellular capsule [41] may help B. mallei avoid signaling cascades that stimulate a productive respiratory burst. The resistance of B. mallei to the NADPH oxidase-mediated antimicrobial activity of macrophages does not, however, eliminate the possibility that this hemoprotein may play a role in the purulent phase of the host response as has been shown for B. cepacia and B. pseudomallei [12], [14].
O2-independent mechanisms are a significant component of the innate killing of B. mallei as indicated by the fact that macrophages from doubly immunodeficient mice lacking both NADPH oxidase and iNOS hemoproteins efficiently kill this bacterium. Innate activation of the autophagic pathway as described for the respiratory pathogen Legionella pneumophila [42]–[44] is one possible mechanism for the O2-independent killing of B. mallei seen in macrophages lacking both gp91phox and iNOS. Recent studies have shown that small GTPases induced in response to IFNγ stimulate killing of M. tuberculosis by promoting autophagosome formation [45], [46]. Most of the enhanced antimicrobial activity stimulated by IFNγ against M. tuberculosis and Salmonella enterica is nonetheless associated with the production of RNS [21]. In contrast to these two intracellular pathogens, the enhanced killing of B. mallei by IFNγ-primed macrophages is exclusively dependent on the expression of functional iNOS. This role for RNS in the bactericidal activity of IFNγ-primed macrophages against B. mallei contrasts with the apparent dispensability of iNOS to the early innate host defenses of unstimulated macrophages. The short time course of the infection studied herein likely prevented innate production of nitrogen oxides in B. mallei-infected macrophages. Given the extraordinary susceptibility of B. mallei to RNS (studies herein) and the stimulation of TLR4 signaling by LPS purified from B. mallei [47], it is not surprising that NO produced at later times of the innate response contributes to the killing of this intracellular pathogen [15].
In summary, our studies indicate that despite its susceptibility to ROS and RNS, B. mallei are selectively killed by RNS generated by IFNγ-activated macrophages. These investigations place B. mallei among the limited number of microorganisms for which NO congeners are microbicidal. Our biochemical and genetic studies indicate that [Fe-S] clusters are critical targets of RNS-mediated killing of B. mallei. The extraordinary hypersusceptibility of B. mallei to RNS raises the intriguing possibility that NO donors could be explored as antibiotics to treat glanders, as shown in the experimental treatment of cutaneous mycosis and leishmaniasis [48], [49]. However, analogous to herpes simplex virus and toxoplasma (reviewed in 49), the possibility exists that despite exerting potent antimicrobial activity, NO could still exacerbate pathology. Future experiments will be needed to determine the value of NO donors in the treatment of glanders.
Acknowledgments
We thank Dr. Brad T. Cookson for providing the ΔfliC ΔfljB Salmonella strain BC696, Dr. Maroof Husain for help with the aconitase assays and Dot Dill for assistance with the electron microscopy.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: Support of this work was provided by the Rocky Mountain Regional Center of Excellence.
References
- 1.Lopez J, Copps J, Wilhelmsen C, Moore R, Kubay J, et al. Characterization of experimental equine glanders. Microbes Infect. 2003;5:1125–1131. doi: 10.1016/j.micinf.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Lehavi O, Aizenstien O, Katz LH, Hourvitz A. 2002. Glanders-a potential disease for biological warfare in humans and animals. Harefuah 141 Spec No: 88–91, pp 119. [PubMed] [Google Scholar]
- 3.Babior BM. NADPH oxidase. Curr Opin Immunol. 2004;16:42–47. doi: 10.1016/j.coi.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Reeves EP, Lu H, Jacobs HL, Messina CG, Bolsover S, et al. Killing activity of neutrophils is mediated through activation of proteases by K+ flux. Nature. 2002;416:291–297. doi: 10.1038/416291a. [DOI] [PubMed] [Google Scholar]
- 5.Stuehr DJ, Marletta MA. Mammalian nitrate biosynthesis: mouse macrophages produce nitrite and nitrate in response to Escherichia coli lipopolysaccharide. Proc Natl Acad Sci U S A. 1985;82:7738–7742. doi: 10.1073/pnas.82.22.7738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang FC. Antimicrobial reactive oxygen and nitrogen species: concepts and controversies. Nat Rev Microbiol. 2004;2:820–832. doi: 10.1038/nrmicro1004. [DOI] [PubMed] [Google Scholar]
- 7.Jones AL, Beveridge TJ, Woods DE. Intracellular survival of Burkholderia pseudomallei. Infect Immun. 1996;64:782–790. doi: 10.1128/iai.64.3.782-790.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyagi K, Kawakami K, Saito A. Role of reactive nitrogen and oxygen intermediates in gamma interferon-stimulated murine macrophage bactericidal activity against Burkholderia pseudomallei. Infect Immun. 1997;65:4108–4113. doi: 10.1128/iai.65.10.4108-4113.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Utaisincharoen P, Tangthawornchaikul N, Kespichayawattana W, Anuntagool N, Chaisuriya P, et al. Kinetic studies of the production of nitric oxide (NO) and tumour necrosis factor-α (TNF-α) in macrophages stimulated with Burkholderia pseudomallei endotoxin. Clin Exp Immunol. 2000;122:324–329. doi: 10.1046/j.1365-2249.2000.01386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Utaisincharoen P, Tangthawornchaikul N, Kespichayawattana W, Chaisuriya P, Sirisinha S. Burkholderia pseudomallei interferes with inducible nitric oxide synthase (iNOS) production: a possible mechanism of evading macrophage killing. Microbiol Immunol. 2001;45:307–313. doi: 10.1111/j.1348-0421.2001.tb02623.x. [DOI] [PubMed] [Google Scholar]
- 11.Utaisincharoen P, Anuntagool N, Arjcharoen S, Limposuwan K, Chaisuriya P, et al. Induction of iNOS expression and antimicrobial activity by interferon (IFN)-β is distinct from IFN-γ in Burkholderia pseudomallei-infected mouse macrophages. Clin Exp Immunol. 2004;136:277–283. doi: 10.1111/j.1365-2249.2004.02445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breitbach K, Klocke S, Tschernig T, van Rooijen N, Baumann U, et al. Role of inducible nitric oxide synthase and NADPH oxidase in early control of Burkholderia pseudomallei infection in mice. Infect Immun. 2006;74:6300–6309. doi: 10.1128/IAI.00966-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnston RB., Jr Clinical aspects of chronic granulomatous disease. Curr Opin Hematol. 2001;8:17–22. doi: 10.1097/00062752-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Segal BH, Ding L, Holland SM. Phagocyte NADPH oxidase, but not inducible nitric oxide synthase, is essential for early control of Burkholderia cepacia and Chromobacterium violaceum infection in mice. Infect Immun. 2003;71:205–210. doi: 10.1128/IAI.71.1.205-210.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brett PJ, Burtnick MN, Su H, Nair V, Gherardini FC. iNOS activity is critical for the clearance of Burkholderia mallei from infected RAW 264.7 murine macrophages. Cell Microbiol. 2007 doi: 10.1111/j.1462-5822.2007.01063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Figurski DH, Helinski DR. Replication of an origin-containing derivative of plasmid RK2 dependent on a plasmid function provided in trans. Proc Natl Acad Sci U S A. 1979;76:1648–1652. doi: 10.1073/pnas.76.4.1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craig FF, Coote JG, Parton R, Freer JH, Gilmour NJ. A plasmid which can be transferred between Escherichia coli and Pasteurella haemolytica by electroporation and conjugation. J Gen Microbiol. 1989;135:2885–2890. doi: 10.1099/00221287-135-11-2885. [DOI] [PubMed] [Google Scholar]
- 18.MacMicking JD, Nathan C, Hom G, Chartrain N, Fletcher DS, et al. Altered responses to bacterial infection and endotoxic shock in mice lacking inducible nitric oxide synthase. Cell. 1995;81:641–650. doi: 10.1016/0092-8674(95)90085-3. [DOI] [PubMed] [Google Scholar]
- 19.Pollock JD, Williams DA, Gifford MA, Li LL, Du X, et al. Mouse model of X-linked chronic granulomatous disease, an inherited defect in phagocyte superoxide production. Nat Genet. 1995;9:202–209. doi: 10.1038/ng0295-202. [DOI] [PubMed] [Google Scholar]
- 20.De Groote MA, Ochsner UA, Shiloh MU, Nathan C, McCord JM, et al. Periplasmic superoxide dismutase protects Salmonella from products of phagocyte NADPH-oxidase and nitric oxide synthase. Proc Natl Acad Sci U S A. 1997;94:13997–14001. doi: 10.1073/pnas.94.25.13997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCollister BD, Bourret TJ, Gill R, Jones-Carson J, Vazquez-Torres A. Repression of SPI2 transcription by nitric oxide-producing, IFNγ-activated macrophages promotes maturation of Salmonella phagosomes. J Exp Med. 2005;202:625–635. doi: 10.1084/jem.20050246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pick E. Microassays for superoxide and hydrogen peroxide production and nitroblue tetrazolium reduction using an enzyme immunoassay microplate reader. Methods Enzymol. 1986;132:407–421. doi: 10.1016/s0076-6879(86)32026-3. [DOI] [PubMed] [Google Scholar]
- 23.Voskuil MI, Schnappinger D, Visconti KC, Harrell MI, Dolganov GM, et al. Inhibition of respiration by nitric oxide induces a Mycobacterium tuberculosis dormancy program. J Exp Med. 2003;198:705–713. doi: 10.1084/jem.20030205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rowland CA, Lertmemongkolchai G, Bancroft A, Haque A, Lever MS, et al. Critical role of type 1 cytokines in controlling initial infection with Burkholderia mallei. Infect Immun. 2006;74:5333–5340. doi: 10.1128/IAI.02046-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nathan C, Shiloh MU. Reactive oxygen and nitrogen intermediates in the relationship between mammalian hosts and microbial pathogens. Proc Natl Acad Sci U S A. 2000;97:8841–8848. doi: 10.1073/pnas.97.16.8841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stevens JM, Ulrich RL, Taylor LA, Wood MW, Deshazer D, et al. Actin-binding proteins from Burkholderia mallei and Burkholderia thailandensis can functionally compensate for the actin-based motility defect of a Burkholderia pseudomallei bimA mutant. J Bacteriol. 2005;187:7857–7862. doi: 10.1128/JB.187.22.7857-7862.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ribot WJ, Ulrich RL. The animal pathogen-like type III secretion system is required for the intracellular survival of Burkholderia mallei within J774.2 macrophages. Infect Immun. 2006;74:4349–4353. doi: 10.1128/IAI.01939-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Denis M. Interferon-gamma-treated murine macrophages inhibit growth of tubercle bacilli via the generation of reactive nitrogen intermediates. Cell Immunol. 1991;132:150–157. doi: 10.1016/0008-8749(91)90014-3. [DOI] [PubMed] [Google Scholar]
- 29.Vazquez-Torres A, Jones-Carson J, Balish E. Nitric oxide production does not directly increase macrophage candidacidal activity. Infect Immun. 1995;63:1142–1144. doi: 10.1128/iai.63.3.1142-1144.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brunelli L, Crow JP, Beckman JS. The comparative toxicity of nitric oxide and peroxynitrite to Escherichia coli. Arch Biochem Biophys. 1995;316:327–334. doi: 10.1006/abbi.1995.1044. [DOI] [PubMed] [Google Scholar]
- 31.De Groote MA, Granger D, Xu Y, Campbell G, Prince R, et al. Genetic and redox determinants of nitric oxide cytotoxicity in a Salmonella typhimurium model. Proc Natl Acad Sci U S A. 1995;92:6399–6403. doi: 10.1073/pnas.92.14.6399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Drapier JC, Hibbs JB., Jr Murine cytotoxic activated macrophages inhibit aconitase in tumor cells. Inhibition involves the iron-sulfur prosthetic group and is reversible. J Clin Invest. 1986;78:790–797. doi: 10.1172/JCI112642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tortora V, Quijano C, Freeman B, Radi R, Castro L. Mitochondrial aconitase reaction with nitric oxide, S-nitrosoglutathione, and peroxynitrite: mechanisms and relative contributions to aconitase inactivation. Free Radic Biol Med. 2007;42:1075–1088. doi: 10.1016/j.freeradbiomed.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 34.Hausladen A, Fridovich I. Superoxide and peroxynitrite inactivate aconitases, but nitric oxide does not. J Biol Chem. 1994;269:29405–29408. [PubMed] [Google Scholar]
- 35.Castro L, Rodriguez M, Radi R. Aconitase is readily inactivated by peroxynitrite, but not by its precursor, nitric oxide. J Biol Chem. 1994;269:29409–29415. [PubMed] [Google Scholar]
- 36.Gardner PR, Costantino G, Szabo C, Salzman AL. Nitric oxide sensitivity of the aconitases. J Biol Chem. 1997;272:25071–25076. doi: 10.1074/jbc.272.40.25071. [DOI] [PubMed] [Google Scholar]
- 37.Shiloh MU, MacMicking JD, Nicholson S, Brause JE, Potter S, et al. Phenotype of mice and macrophages deficient in both phagocyte oxidase and inducible nitric oxide synthase. Immunity. 1999;10:29–38. doi: 10.1016/s1074-7613(00)80004-7. [DOI] [PubMed] [Google Scholar]
- 38.LaCourse R, Ryan L, North RJ. Expression of NADPH oxidase-dependent resistance to listeriosis in mice occurs during the first 6 to 12 hours of liver infection. Infect Immun. 2002;70:7179–7181. doi: 10.1128/IAI.70.12.7179-7181.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stevens MP, Wood MW, Taylor LA, Monaghan P, Hawes P, et al. An Inv/Mxi-Spa-like type III protein secretion system in Burkholderia pseudomallei modulates intracellular behaviour of the pathogen. Mol Microbiol. 2002;46:649–659. doi: 10.1046/j.1365-2958.2002.03190.x. [DOI] [PubMed] [Google Scholar]
- 40.Vazquez-Torres A, Jones-Carson J, Balish E. Peroxynitrite contributes to the candidacidal activity of nitric oxide-producing macrophages. Infect Immun. 1996;64:3127–3133. doi: 10.1128/iai.64.8.3127-3133.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schell MA, Ulrich RL, Ribot WJ, Brueggemann EE, Hines HB, et al. Type VI secretion is a major virulence determinant in Burkholderia mallei. Mol Microbiol. 2007;64:1466–1485. doi: 10.1111/j.1365-2958.2007.05734.x. [DOI] [PubMed] [Google Scholar]
- 42.Swanson MS, Molofsky AB. Autophagy and inflammatory cell death, partners of innate immunity. Autophagy. 2005;1:174–176. doi: 10.4161/auto.1.3.2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Molofsky AB, Byrne BG, Whitfield NN, Madigan CA, Fuse ET, et al. Cytosolic recognition of flagellin by mouse macrophages restricts Legionella pneumophila infection. J Exp Med. 2006;203:1093–1104. doi: 10.1084/jem.20051659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zamboni DS, Kobayashi KS, Kohlsdorf T, Ogura Y, Long EM, et al. The Birc1e cytosolic pattern-recognition receptor contributes to the detection and control of Legionella pneumophila infection. Nat Immunol. 2006;7:318–325. doi: 10.1038/ni1305. [DOI] [PubMed] [Google Scholar]
- 45.MacMicking JD, Taylor GA, McKinney JD. Immune control of tuberculosis by IFN-γ-inducible LRG-47. Science. 2003;302:654–659. doi: 10.1126/science.1088063. [DOI] [PubMed] [Google Scholar]
- 46.Gutierrez MG, Master SS, Singh SB, Taylor GA, Colombo MI, et al. Autophagy is a defense mechanism inhibiting BCG and Mycobacterium tuberculosis survival in infected macrophages. Cell. 2004;119:753–766. doi: 10.1016/j.cell.2004.11.038. [DOI] [PubMed] [Google Scholar]
- 47.Brett PJ, Burtnick MN, Snyder DS, Shannon JG, Azadi P, et al. Burkholderia mallei expresses a unique lipopolysaccharide mixture that is a potent activator of human Toll-like receptor 4 complexes. Mol Microbiol. 2007;63:379–390. doi: 10.1111/j.1365-2958.2006.05519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lopez-Jaramillo P, Ruano C, Rivera J, Teran E, Salazar-Irigoyen R, et al. Treatment of cutaneous leishmaniasis with nitric-oxide donor. Lancet. 1998;351:1176–1177. doi: 10.1016/s0140-6736(05)79119-4. [DOI] [PubMed] [Google Scholar]
- 49.Vazquez-Torres A, Fang FC. Therapeutic applications of NO in infection. In: Fang FC, editor. Nitric oxide and infection. New York: Kluwer Acad/Plenum Publishers; 1999. pp. 475–488. [Google Scholar]
- 50.Yabuuchi E, Kosako Y, Oyaizu H, Yano I, Hotta H, et al. Proposal of Burkholderia gen. nov. and transfer of seven species of the genus Pseudomonas homology group II to the new genus, with the type species Burkholderia cepacia (Palleroni and Holmes 1981) comb. nov. Microbiol Immunol. 1992;36:1251–1275. doi: 10.1111/j.1348-0421.1992.tb02129.x. [DOI] [PubMed] [Google Scholar]
- 51.Bergman MA, Cummings LA, Alaniz RC, Mayeda L, Fellnerova I, et al. CD4+-T-cell responses generated during murine Salmonella enterica serovar Typhimurium infection are directed towards multiple epitopes within the natural antigen FliC. Infect Immun. 2005;73:7226–7235. doi: 10.1128/IAI.73.11.7226-7235.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]