Abstract
Purpose
To compare occupational morbidity estimates for migrant and seasonal farmworkers obtained from survey methods versus chart review methods, and to estimate the proportion of morbidity treated at federally recognized migrant health centers (MHCs) in a highly agricultural region of New York.
Methods
Researchers simultaneously conducted: a) an occupational injury and illness survey among agricultural workers; b) MHC chart review; and c) hospital emergency room (ER) chart reviews.
Results
Of the 24 injuries reported by 550 survey subjects, 54.2% received treatment MHCs 16.7% at ERs, 16.7% at some other facility, and 12.5% were untreated. For injuries treated at MHCs or ERs, the incidence density based on survey methods was 29.3 injuries per 10,000 worker-weeks versus 27.4 by chart review. The standardized morbidity ratio (SMR) for this comparison was 1.07 (95% CI = 0.65 – 1.77).
Conclusion
Survey data indicate that 71% of agricultural injury and illness can be captured with MHC and ER chart review. MHC and ER incidence density estimates show strong correspondence between the two methods. A chart review-based surveillance system, in conjunction with a correction factor based on periodic worker surveys, would provide a cost-effective estimate of the occupational illness and injury rate in this population.
Keywords: migrant farmworkers, seasonal farmworkers, agricultural workers, occupational illness and injury, farm laborers
INTRODUCTION
Efforts to create a reliable occupational injury and illness surveillance system within agriculture face three major challenges. First, since approximately 95% of U.S. farms employ fewer than 11 workers, they are exempt from Occupational Safety and Health Administration (OSHA) reporting regulations (1). For this reason, measures of agricultural illness and injury using data from federal sources are incomplete.
Second, identification of agricultural injuries or illnesses is limited by the fact that a large portion of the agricultural workforce (between 3.5 – 5 million workers nationwide) (2,3,4,5) is employed on a temporary basis. When injured or ill, these workers may leave their temporary employment or refrain from reporting it to employers due to fear of job loss (6).
Third, the fact that the majority (roughly 78%) of this temporary workforce is foreign-born adds barriers to reporting injury or illness (7). Many have limited English proficiency and little education, resulting in social isolation and a high level of dependence on the employer (8). Also, according to some studies, as many as 53% (7) are working without legal documentation. These cultural factors combine to create a barrier to reporting anything that might reflect poorly on one’s own ability to work, or on the employer (9).
Some of the same factors that make this population difficult to study also lead researchers to speculate that they may be at especially high risk for occupational injury and illness. For example, without OSHA incident reporting, there may be less motivation to provide worksite protections and training. Also, the piece-rate pay system that often accompanies temporary employment encourages long hours of manual labor with few breaks (10). These long hours of hand-harvest orchard or field work can lead to musculoskeletal disorders as well as dermatitis, dehydration and sun stroke (8), and the potential for acute or chronic pesticide poisoning (11,12). Additionally, unsanitary living and field conditions can lead to infection and injury (13,14).
This combination of incomplete surveillance data and assumed high risk has led researchers to seek an alternative occupational injury and illness surveillance method for the agricultural workforce. To do this, the authors established a surveillance system based on annual chart reviews of federally funded migrant health centers (MHCs) in New York and Pennsylvania in 1999. Details of this system are described elsewhere (15). An expanded surveillance system was then established in seven northeastern states in 2000. This system collected chart review data from 12 of these health programs, resulting in the identification of 1,678 agricultural illnesses and injuries between 2000–2003.
An additional key component of this type of surveillance is an accurate estimate of the temporary agricultural person-time at risk. Worker-hours have been calculated for New York State by the authors, using published production data to create an estimated labor demand (16). These exposure data made it possible to estimate an occupational morbidity rate for this population.
One limitation of this method was that agricultural injuries and illnesses treated at locations other than federally funded MHCs were not captured. There is data suggesting that this proportion of the total morbidity may be quite large (17,18). If the magnitude and types of cases missed by MHC chart review could be determined, this information could be used to adjust morbidity estimates based on chart review.
In the current study, researchers simultaneously conducted the following in a highly agricultural region of rural New York: a) an occupational injury and illness survey among agricultural workers; b) MHC chart review; and c) hospital emergency room (ER) chart reviews. This made it possible to estimate the proportion of morbidity that is treated at places other than the MHC. In addition to its high level of agricultural activity, the region was selected for its similarity, in terms of both demographics and health care options, to many other areas of the agricultural Northeast.
METHODS
Study Population
This study population included temporary agricultural workers employed in field or orchard harvest work in the Finger Lakes region of New York State (16). This region was defined as Ontario, Steuben, Wayne and Yates counties.
Sampling Frame
Collaborative relationships were created between the researchers and various agencies throughout the Finger Lakes. These included New York State agencies (Department of Health and Department of Labor), migrant education programs, migrant health care programs (namely Finger Lakes Migrant Health Care Project, Inc. (FLMHCP)), and other regional organizations. These agencies create an annual list of migrant camps that was used as a sampling frame. In addition, they assisted in hiring data collectors and informally publicizing the study.
Subject Selection
An initial random sample of 55 camps was drawn. Once a camp was selected, the goal was to interview all workers housed there. This design was intended to result in a total of 550 interviews based on a preliminary estimate of ten workers per camp. It subsequently became necessary to recruit an additional 20 camps in order to reach this total of 550.
Survey Data Collection in the Field
The surveys were conducted over the course of a twelve-week period from mid-August to mid-November of 2005. This interval was selected to correspond to the time during which most of the migrant workers would still be present, and would also have accumulated a significant amount of exposure time. This interval was established by reviewing New York commodity harvest season data (19). The selected timeframe was designed to capture a representative group of farmworkers across several crop harvests.
Sixteen trained interviewers visited migrant camps on weekday evenings and weekends to conduct surveys. Upon arrival at a camp that was situated on farm property, the interviewers sought out the farm owner to gain consent to conduct interviews prior to obtaining consent from the workers themselves. On camps with no farm affiliation, farmworkers were approached directly. Participants were privately read a consent form in English, Spanish, or Haitian Creole as appropriate. Once informed consent was obtained, the interview was conducted, and the farmworker was given a $10 money order.
Survey Instrument
The survey instrument was created with emphasis on simplicity of language and cultural appropriateness using input from agricultural service agencies, outreach workers, FLMHCP, and consultant findings from pilot testing.
For the pilot phase of the project, researchers contacted several farm owners in the Finger Lakes region to obtain consent to approach workers. The questionnaire was tested with twelve workers from three camps, with Spanish and Haitian Creole speaking consultants conducting the interviews. These consultants took note of problematic survey questions and other farmworker comments, and the survey was adjusted to incorporate both farmworker and consultant feedback.
The final survey form contained the camp number, survey date, and identity of the data collector. Participants were asked the initial question “In this past season in New York have you gotten hurt or sick at work?” If the participant said yes, subsequent questions were asked concerning the nature of the injury, whether or not treatment was sought, and from where that treatment was received. Additionally, questions regarding who chose the health care location, and any language barriers encountered with medical personnel, were asked.
All respondents were also asked whether they had heard of local MHCs and whether they had visited one of those facilities in the past for any reason. General demographic information was collected, including age, country of origin, and annual travel patterns to New York State.
Establishment of Inclusion Dates for Chart Review
New York commodity harvest season data were used to establish inclusion dates for chart reviews. The beginning date was defined as two weeks prior to the beginning of the earliest harvest season (strawberries), and two weeks after the conclusion of the final season (cabbage). This resulted in an interval extending from May 15th to December 31st.
Migrant Health Center Chart Review Methods
Following conclusion of the harvest season, reviews of medical charts at the two clinic locations of FLMHCP were conducted. Every fifth chart was selected from an alphabetized master list of all farmworker patients (as determined by intake data), aged 12 or older, visiting the clinics between May 15th and December 31st, 2005.
Researchers reviewed each chart to confirm farmworker status and assess the presence of occupational illness or injury using registration forms or the physician or nurse’s progress notes. In order to qualify as occupational, the injury or illness must have been attributable to, or aggravated by, working in the field, orchard, or packing house. In addition, the injury must have occurred within the four study counties.
For farmworkers found to have an occupational injury, information on injury date, type, cause, location on the farm, commodity, and body part affected was collected. No personally identifying information about the patient was collected, but demographic characteristics, such as patient age, gender, and country of origin were recorded.
Emergency Room Chart Review Methods
On two dates during the 2005 harvest season, reviews of ER medical charts were conducted at six Finger Lakes region hospitals. Charts were selected if they contained patient visits between May 15th and December 31st, 2005, and explicitly stated that the patient was a “migrant farmworker,” “seasonal worker,” “farm laborer,” or employed by a crop farm doing hand harvest work. A nurse then evaluated these charts for occupational illness or injuries using the same criteria described above for the MHC chart review.
When an occupational injury event was identified, the nurse recorded the physician or nurse’s note verbatim, and recorded the patient’s age, gender, country of origin, commodity, county where the injury took place, injury type, cause, location on the farm, and body part affected.
Statistical Analyses
Sampling Fraction Adjustment
Prior to being combined with the ER chart review data, the total number of occupational incidents documented via MHC chart review was multiplied by five since only every fifth medical record was reviewed.
Demographic Summary of Surveyed Workers
Continuous variables, such as age and weeks worked, were summarized as means and standard deviations. Categorical variables, such as country of origin, were summarized as frequencies and proportions.
Injured Subjects Comparisons
Continuous variables, such as age, were compared between injured survey respondents and injured workers identified by chart review using independent samples t-tests. Categorical variables, such as country of origin, crop, type and severity of injury, were compared between the two groups using chi-square, or Fisher’s Exact Test where appropriate.
Treatment Method Morbidity Comparisons
This analysis included only those subjects whose injury was treated at either an ER or MHC. For each method (interview versus chart review) a proportion was defined as follows:
These proportions were compared between the two methods using the normal approximation to the test of two independent binomial proportions. Any discrepancy observed in these two proportions might be an indicator of where undercounting, or underreporting, may have occurred.
The proportion of all injuries for which treatment was not sought, or was sought at a location other than an ER or MHC, was calculated only for survey respondents.
Estimation of Incidence Density
In order to provide for a meaningful comparison of incidence densities from the interview versus chart review methods, the numerator for these estimates considered only cases treated at either ERs or MHCs. This was necessary since these were the only sources of care considered for the chart review.
The person-time denominator for these estimates was expressed in worker-weeks. Person-time for interview subjects was taken as the number weeks of work reported up to the time of the interview. For chart reviews, the worker-weeks measure was an estimate taken from a demand for labor study completed by Alice Larson (16). Thus, both the number of injuries (numerator) and the person-time (denominator) used in the estimation of the two (survey versus chart review) incidence densities were arrived at from completely independent sources. Therefore, close agreement in the two incidence densities would allow for confidence in this occupational morbidity estimate for this population.
Estimation of the Standardized Morbidity Ratio
The two incidence densities were compared via calculation of the standardized morbidity ratio:
Because the two incidence density estimates are being made for the same population, the ratio may be considered as standardized without the necessity of formal adjustment for differential demographic profiles.
RESULTS
Survey Demographics
A total of 550 completed surveys were obtained from 731 workers, resulting in a response rate of 75.2%. These 550 workers represented a total of 72 camps. The age of the respondents ranged from 14 to 74 years with a mean and standard deviation of 33.3 and 13.0 respectively (Table 1). The most common country of origin was Mexico (69%). This was followed by Puerto Rico (9.7%), Jamaica (8.7%), and Haiti (6.0%). The majority of the remaining 6.5% were from the United States and Guatemala.
Table 1.
Demographic information for all survey respondents (n=550).
| Survey Responses | |
|---|---|
| Age (years) | |
|
| |
| Mean (SD) | 33.3 (13.0) |
| Range | 14 – 74 |
| Country of Origin n (%) | |
|
| |
| Mexico | 379 (69.0) |
| Puerto Rico | 53 (9.7) |
| Jamaica | 48 (8.7) |
| Haiti | 33 (6.0) |
| United States | 21 (3.8) |
| Guatemala | 9 (1.6) |
| Other | 6 (1.1) |
| Time living in NY (days) | |
|
| |
| Mean | 90.1 |
| Median | 76 |
| Range | 6 – 287 |
| Seasons Migrated to NY | |
|
| |
| Mean | 4.7 |
| Median | 3 |
| Range | 1 – 52 |
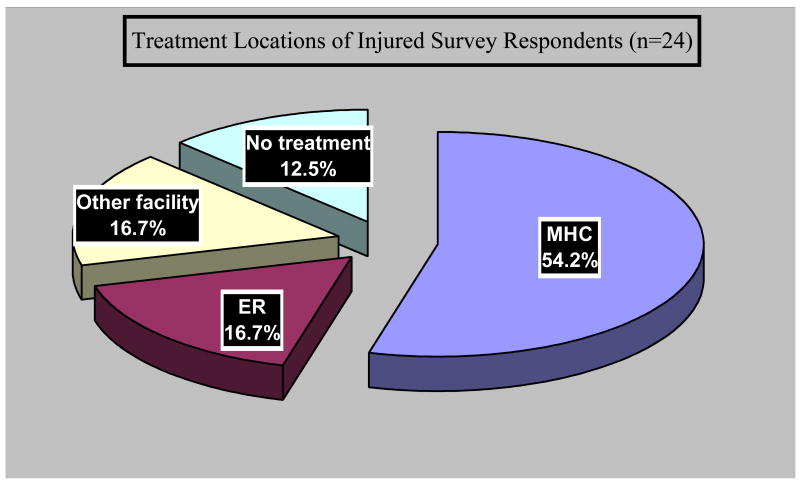
The survey respondents reported a total of 26 injuries. Two of these 26 were eliminated from further consideration where the victim specifically stated that treatment was unnecessary. Of the remaining 24, thirteen received treatment at MHCs (54.2%) and four were treated at ERs (16.7%) (Figure 1).
FIGURE 1.
Proportions of treatment methods among injured survey respondents (n=24).
Seven of the 24 injured individuals (29.2%) identified by interview did not seek treatment at either an ER or MHC. Three of these seven (12.5%) did not seek any treatment at all, with one respondent stating the intention to seek treatment in the event that the injury did not resolve. The other four sought treatment at non-MHC or ER facilities; one was treated by a chiropractor, one was treated at home, and the remaining two attended hospitals or clinics not identifiable as an ER or MHC.
Injured Subjects Comparisons
The mean age of the 24 interview respondents reporting an injury (37.8 years) was not significantly different from injured workers identified by chart review (34.3 years) (Table 2). The predominant nationality of injured workers identified by both chart review and interview was Mexican (chart review=69.5%, interview=66.7%). The predominant crop being harvested at the time of injury was apples (chart review=58.2%, interview=57.1%) and did not differ significantly between the two methods.
Table 2.
Comparisons between survey and chart review methods for injured subjects identified by survey (n=24) and chart-review (n=141).
| Survey | Chart Review | p-value | |
|---|---|---|---|
| Age (years) | |||
|
| |||
| Mean (SD) | 37.8 (14.9) | 30.4 (13.8) | 0.3367 |
| Range | 19 – 68 | 16 – 75 | |
| Country of Origin n (%) | |||
|
| |||
| Mexico | 16 (66.7) | 98 (69.5) | 0.0057 |
| Jamaica | 4 (16.7) | 0 | |
| Haiti | 2 (8.3) | 20 (14.2) | |
| United States | 1 (4.2) | 7 (4.9) | |
| Guatemala | 1 (4.2) | 5 (3.6) | |
| Puerto Rico | 0 | 2 (1.4) | |
| Other | 0 | 9 (6.4) | |
| Crop Type n (%) | |||
|
| |||
| Apples | 12 (57.1) | 82 (58.2) | 0.0798 |
| Vegetables | 0 | 22 (15.6) | |
| Other | 9 (42.9) | 37 (26.2) | |
| Mechanism of Injury n (%) | |||
|
| |||
| Strain/Sprain | 11 (45.8) | 53 (37.6) | 0.5990 |
| Rash/Irritant/Exposure | 7 (29.2) | 25 (17.7) | |
| Cut/Caught/Crushed | 1 (4.2) | 17 (12.1) | |
| Struck | 1 (4.2) | 17 (12.1) | |
| Fall | 2 (8.3) | 15 (10.6) | |
| Unknown | 2 (8.3) | 14 (9.9) | |
There was no significant difference in the “mechanism of injury” profile between the two methods (Table 2). The most common mechanism for both chart review and interview was “strains and sprains” (chart review=37.6%, interview=45.8%) followed by rashes or irritant exposures (chart review=17.7%, interview=29.2%).
Treatment Method Comparisons
Less than one quarter (18.4%) of the injuries identified by chart review were treated at ERs. In contrast, based on interview, 23.5% of injuries (among those treated at ERs or MHCs) were ER visits. This difference in treatment modalities as estimated by the two methods was not significant.
Survey Incidence Density
When limited to injuries treated only at ERs and MHCs, this incidence density was estimated to be 17 injuries/5,801 worker-weeks = 29.3 per 10,000 worker-weeks. For injuries treated only at ERs, the incidence density was 4/5,801 = 6.9 injuries per 10,000 worker-weeks (Table 3).
Table 3.
Comparison of incidence density estimates among temporary agricultural workers between survey and chart review methodology, and current and previous research. Estimates of number of injury events per 10,000 worker-weeks.
Chart Review Incidence Density
A total of 250 charts at two MHCs were reviewed, resulting in the identification of 23 injuries. Adjustment of this data for the sampling fraction (multiplication by 5) yields an estimate of 115 injuries. Ninety-nine ER charts were identified for review, yielding 26 injuries. Based on the Demand for Labor estimating methodology, the total number of worker-weeks required for harvesting labor in a typical year in Wayne, Ontario, Yates, and Steuben counties was 51,507. From this, the incidence density based on this methodology for ERs plus MHCs was estimated to be 27.4 injuries per 10,000 worker-weeks (Table 3). ER-specific incidence density was estimated to be 26/51,507= 5.0 injuries per 10,000 worker-weeks.
The standardized morbidity ratios comparing incidence densities between interview and chart review methods were close to 1.0 both for injuries treated at ERs and MHCs (1.07, 95% CI = 0.65 – 1.77) (Table 3) and for injuries treated at ERs only (1.37, 95% CI = 0.48 – 3.91).
DISCUSSION
The congruence of the results obtained for the ER and MHC data from these two very different methods (survey=29.3 chart review=27.4 injuries/10,000 worker-weeks) is notable. As noted in the methods, the complete independence of the data used in arriving at the two estimates, combined with their congruence, provides a high level of confidence in this measure of morbidity.
It is also noteworthy that a study using worker’s compensation claims among orchard fruit workers in California produced a virtually identical incidence density of 24.4 injuries per 10,000 worker-weeks (20). The current study’s estimates are also similar to McCurdy et al’s (21) estimates using survey data among Hispanic farmworkers in California (approximately 23 injuries/10,000 worker-weeks) (see Appendix A).
The survey data indicate that 54.2 percent of all work-related morbidity experienced by this population is treated at an MHC, and another 16.7 percent is treated at ERs. Thus, a surveillance system based on MHC and ER chart review could be expected to capture approximately 70.9 percent of the morbidity affecting this population.
The farmworker survey required the commitment of 2.5 FTEs for a period of three months. In addition, the planning and design of the study required an additional one FTE for nine months. In contrast, MHC chart review for the two MHCs in the study region required roughly only 40 hours to complete. Emergency room chart reviews, including ER recruitment for the study, involved the commitment of 0.25 FTEs for a period of six months.
These data suggest that a surveillance system based on annual MHC and ER chart reviews, adjusted by a correction factor based on less frequent worker surveys, would provide a cost effective estimate of the rate of work-related illness and injury in this population. The surveys, which would be performed at perhaps five-year intervals, would allow this correction factor to incorporate secular trends in health care utilization of migrant workers. Based on the ER and MHC data obtained in 2005, the correction factor would be 1.41, or (1/0.709).
Another noteworthy strength of this surveillance method would be the detailed medical information obtained from direct chart review. In addition to being a more objective assessment of the injury or illness, this written documentation is not vulnerable to memory loss.
LIMITATIONS
As noted previously, the survey could only obtain information from the date of administration back to the arrival date of the worker. These surveys were all completed prior to December, whereas the period covered by the chart review included that month. Although both estimates were corrected for exposure time, it was possible that the incidence density in December was different from the remainder of the season. However, because of the congruence of the two estimates (chart review versus survey), it is considered unlikely that this bias existed.
It should be emphasized that this surveillance system was designed to capture acute events, namely work-related traumatic injuries, rather than to assess the overall health of this population as evidenced by underlying conditions and chronic illnesses. To make this latter assessment would require periodic health examinations and would be prohibitively expensive.
CONCLUSION
The results obtained in this research are in agreement with agricultural injury and illness incidence densities found in previous studies. Study results indicate that a surveillance system based on annual migrant health center and emergency room chart reviews, in conjunction with a correction factor based on periodic worker surveys, would provide a cost effective estimate of the rate of work-related illness and injury in this population. Future research will be needed to determine the stability of the correction factor of 1.41 over time and across regions of the Northeast.
Acknowledgments
This research was made possible by a grant from the National Cancer Institute (#R01 CA08468-05). The authors would like to extend thanks to the Finger Lakes Migrant Health Care Project, Inc., the Finger Lakes Coalition of Farmworker Agencies, and the many New York farm owners, crew bosses, and farmworkers for their support with this study.
LIST OF ABBREVIATIONS
- NYCAMH
New York Center for Agricultural Medicine and Health
- MHC
Migrant health center
- ER
Emergency room
- FLMHCP
Finger Lakes Migrant Health Care Project, Inc
- SMR
Standardized Morbidity Ratio
Appendix A
Conversion of person-time to worker-weeks for direct comparisons
California (Villarejo, 1998)
Published Rate: 12,678 claims/100000 FTE
Total payroll for season (orchard fruit workers): $478,700,000
Average weekly wage: $207.78
Total worker-weeks: 2,303,879
Worker’s Compensation paid claims (i.e., injuries): 5,617
5,617 claims/2,303,879 worker-weeks = 24.38/10,000 worker-weeks
California (McCurdy et al, 2003)
Published Rate: 9.3 injurious events/100 FTE
Person time unit: Full-time equivalents (FTE’s)
1 FTE = 2,000 worker-hours (wh)
100 FTE = 200,000 wh
1 worker-week (per Minimum Labor Demand Method, Earle-Richardson et al, 2005) = 49.5 wh
100 FTE = 4,040 worker-weeks (200,000 wh/49.5wh in 1 worker-week)
9.3 injuries/4,040 worker-weeks = 23.01/10,000 worker-weeks
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Schenker MB. Preventive medicine and health promotion are overdue in the agricultural workplace. J Public Health Policy. 1996;17(3):275–305. [PubMed] [Google Scholar]
- 2.Wilk VA. Occupational health of migrant and seasonal farmworkers in the U.S.: progress report. Farmworker Justice Fund; Washington DC: 1998. [Google Scholar]
- 3.McCurdy SA, Carroll DJ. Agricultural Injury. Am J Ind Med. 2000;38:463–480. doi: 10.1002/1097-0274(200010)38:4<463::aid-ajim13>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 4.Report of the Commission on Agricultural Workers, November, 1992, Washington, D.C.
- 5.Rust GS. Health Status of Migrant Farmworkers: A Literature Review and Commentary. American Journal of Public Health. 1990;80(10):1213–1216. doi: 10.2105/ajph.80.10.1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mobed K, Godl EB, Schenker MB. Occupational health problems among migrant and seasonal farm workers. In Cross Cultural Medicine: A Decade Later (Special Edition) West J Med. 1992;157:367–373. [PMC free article] [PubMed] [Google Scholar]
- 7.Carroll D, Samardick RM, Bernard S, Gabbard S, Hernandez T. Demographic and Employment profile of United States Farmworkers. Findings from the National Agricultural Workers Survey 2001–2002; March 2005. [Google Scholar]
- 8.McCurdy SA. Occupational Health Status of Migrant and Seasonal Farmworkers. In: McDuffie HH, Dosman JA, Semchuk KM, Olenchock SA, Senthilselvan A, editors. Agricultural Health and Safety: workplace, environment, sustainability (supplement) Lewis Publications; Chelsea, Michigan: pp. 213–216. (Peer-reviewed conference proceedings) [Google Scholar]
- 9.Schmidley A, Dianne A. Profile of the Foreign-Born Population in the United States: 2000. Washington, DC: US Census Bureau; 2001. [Google Scholar]
- 10.LaPlante Stein LM. Health Care Delivery to Farmworkers in the Southwest: an Innovative Nursing Clinic. Journal of the American Academy of Nurse Practitioners. 1993;5(3):119–124. doi: 10.1111/j.1745-7599.1993.tb00852.x. [DOI] [PubMed] [Google Scholar]
- 11.Goldsmith MF. As Farmworkers help keep America healthy, illness may be their harvest. Journal of the American Medical Association. 1989;261:3207–3213. [PubMed] [Google Scholar]
- 12.Villarejo D, Baron SL. The Occupational Health of Hired Farm Workers. Occupational Medicine: State of the Art Reviews. 1999;14(3):613–635. [PubMed] [Google Scholar]
- 13.Hansen E, Donohoe M. Health Issues of Migrant and Seasonal Farmworkers. Journal of Health Care for the Poor and Underserved. 2003;14(2):153–163. doi: 10.1353/hpu.2010.0790. [DOI] [PubMed] [Google Scholar]
- 14.Sakala C. Migrant and Seasonal Farmworkers in the United States: A review of Health Hazards, Status and Policy. Int Migr Rev. 1987 Fall;21(3):659–87. [PubMed] [Google Scholar]
- 15.Earle-Richardson G, Jenkins PL, Slingerland DT, Mason C, Miles M, May JJ. Occupational injury and illness among migrant and seasonal farmworkers in New York State and Pennsylvania, 1997–1999: pilot study of a new surveillance method. Am J Ind Med. 2003 Jul;44(1):37–45. doi: 10.1002/ajim.10233. [DOI] [PubMed] [Google Scholar]
- 16.Earle-Richardson G, Jenkins PL, Stack S, Sorensen JA, Larson A, May JJ. Estimating farmworker population size in New York State using a minimum labor demand method. J Agric Saf Health. 2005 Aug;11(3):335–45. doi: 10.13031/2013.18576. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control. HIV invection, syphilis, and tuberculosis screening among migrant farm workers 0 Florida. MMWR. 1992;41(39):723–725. [PubMed] [Google Scholar]
- 18.Office of Technology Assessment. Health Care in Rural America (OTA Publication No. OTA-H-434) Washington, DC: 1990. [Google Scholar]
- 19.National Agricultural Statistics Service. United States Department of Agriculture. 2002 Census of Agriculture.
- 20.Villarejo D. Occupational Injury Rates Among Hired Farmworkers. Journal of Agricultural Safety and Health. 1998;(1):39–46. [Google Scholar]
- 21.McCurdy SA, Samuels SJ, Carroll DJ, Beaumont JJ, Morrin LA. Agricultural Injury in California Migrant Hispanic Farm Workers. American Journal of Industrial Medicine. 2003;44:225–235. doi: 10.1002/ajim.10272. [DOI] [PubMed] [Google Scholar]