In a recent issue of the American Journal of Epidemiology,1 we described the relation between sustained population-wide weight loss and a decline in all-cause mortality and in the rates of death from diabetes mellitus and cardiovascular disease in Cuba. The widespread weight loss resulted from the economic crisis known as the “Special Period,” which Cuba experienced in the 1990s after the collapse of the Soviet Union. This period of economic and social hardship also had negative consequences for health. For example, a neuropathy outbreak, possibly due to vitamin deficiencies, affected 50 000 people between 1992 and 1993,2 and the decline in infant mortality that Cuba had been experiencing reversed between 1990 and 1993.3 The neuropathy outbreak did not affect children, elderly people or pregnant women because a special rationing system was in place to protect them. The Cuban population showed high levels of social cohesion, especially within families, in a time of economic hardship.2
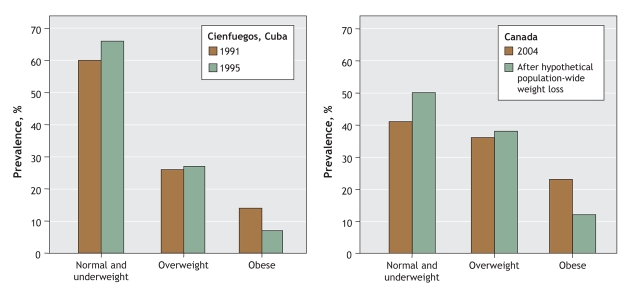
During this Special Period, per capita daily energy intake fell from 2899 kcal (12 180 kJ) to 1863 kcal (7820 kJ), and energy expenditure increased because fuel shortages led people to walk or ride their bicycles rather than use public transportation. The proportion of physically active adults increased from 30% to 67%. Population-representative studies in Cienfuegos, Cuba, in 1991 and 1995 showed a 1.5-unit decrease in the body mass index. The prevalence of obesity declined from 14% to 7%, the prevalence of overweight increased from 26% to 27%, and the prevalence of normal weight increased from 60% to 66% (Figure 1). The decline in body weight in the population represents a modest weight loss of 4–5 kg, or 5%–6% of body weight per adult. In subsequent years, rates of death decreased markedly from 1997 to 2002: by 51% for diabetes, 35% for coronary artery disease, 20% for stroke and 18% for all-cause mortality.
Figure 1: Left: The change in obesity prevalence in Cienfuegos, Cuba, between 1991 and 1995, a period during which energy intake decreased and physical activity increased, resulting in population-wide weight loss and a reduction in obesity by half. Right: The comparable impact on obesity prevalence in Canada after a hypothetical population-wide weight loss.
The large decline in all-cause mortality and in the rates of death from cardiovascular disease and diabetes that we observed suggests that population-wide policies intended to reduce energy intake while preserving nutritional sufficiency and increasing physical activity could result in significant population-wide weight loss. This experience further suggests that public health strategies could lead to major improvements in obesity-related conditions such as diabetes and cardiovascular disease.
The obesity epidemic currently affects most countries around the world.4 In 2004, 23% of Canadian adults were obese and 36% overweight5 (Figure 1). In the same year in the United States, 32% of the adult population was obese and 34% overweight.6
When studying the implications of the of the Special Period in Cuba, one must note that Cuba's population before the crisis had a low prevalence of obesity (14%).1 The effects of population-wide weight loss could be larger in Canada and the United States, where more than half of the population is either overweight or obese.4,5
The current discussion on the effect of body weight on mortality underscores the difficulty in interpreting the effects of diet, physical activity and body weight on mortality.7–10 Therefore, caution is warranted in the interpretation of such observational studies. Ongoing trials examining the impact of voluntary weight loss on cardiovascular morbidity and mortality in people with diabetes, such as the Look AHEAD (Action for Health in Diabetes) study,11 may further clarify this issue. Preliminary results of this study show that a costly, state-of-the-art individual lifestyle intervention resulting in 8% weight loss can lead to large improvements in blood pressure and levels of triglycerides and high-density lipoprotein cholesterol.12
The large body of research in the area of lifestyle interventions shows that behavioural changes need to happen on both sides of the energy balance — reductions in energy intake and increases in energy output12 — and that maintenance of weight loss requires high levels of physical activity.13
In his classic examination of preventive interventions, Rose14 described 2 approaches: the high-risk approach, which seeks to protect susceptible individuals, and the population approach, which seeks to affect the underlying causes that make the condition common. To explain the differences in prevalence of a given condition in a population at 2 points in time, we would need to understand the determinants of health that affect the population as a whole. The population approach is the attempt to shift the whole distribution of exposure in a favourable direction. In the case of obesity prevention, the objective would be to lower mean body weight, which is precisely what occurred in Cuba during the Special Period. This shift in the mean body weight can explain in part the large aggregate effects on mortality from diseases related to body weight, such as diabetes and cardiovascular disease. Population-wide strategies are optimal preventive approaches for continuously distributed risk factors such as high blood pressure and elevated serum cholesterol levels,14 and body weight might be an important risk factor susceptible to population-wide interventions.
From a public health perspective, several questions arise: What can be learned from the Cuban experience to reduce body weight at a population level in an industrialized country such as Canada? What public health measures can lead to population-wide body weight reductions? In Figure 1, we propose a hypothetical population-wide weight loss in Canada in which the prevalence of obesity would be reduced by almost half. As in Cuba, the per capita reduction in energy intake and increase in physical activity levels, if sustained for at least 5 years, would lead to a 1.5-unit decrease in body mass index or 5% of body weight per adult.
Population-wide changes in the context of a society such as Canada's need to directly affect the total energy intake and physical activity levels of all individuals. Reductions in energy intake may be achieved by an increase in the consumption of low-energy foods, such as fruits and vegetables, and a decrease in the consumption of high-energy foods. Paradoxically, these changes are most likely to occur if structural changes take place identifying the population as the unit of intervention. Population changes would need to be made at all social and political levels, including provincial, territorial and municipal levels and at schools, workplaces and households. In countries such as Canada and the United States, where obesity affects minorities and lower income populations disproportionately,15 population-wide policies should make the effort to include those populations in order to reduce the already existing inequalities.16 The 2006 Canadian clinical guidelines for the prevention of obesity already recognize the need for population-wide strategies that will require the cooperation of policy-makers and other interested parties.17 Structural changes toward the prevention of obesity were highlighted in the 2006 guidelines by Raine and Wilson.18
A number of interventions could directly affect total energy intake and physical activity of the whole population, thereby reducing body weight. Population-wide interventions related to energy intake should include promoting low-energy, nutritious foods, for example making fruits and vegetables more readily available19 and less expensive,15 and limiting the availability and increasing the prices of high-energy foods. Interventions related to physical activity should include promoting walking and bicycling as means of transportation. In addition, urban planners, schools and workplace designers should prioritize physical activity in their plans.
In contemporary societies in which more than half of the individuals are either overweight or obese, population-wide interventions to keep body weight within the normal limits may be the best suited to prevent conditions such as diabetes and cardiovascular disease. As seen in Cuba, small, individual changes affecting the whole population have large preventive potential for diseases with high prevalence.
Key points
• During the economic crisis Cuba experienced in the 1990s, energy intake per capita gradually decreased to 1863 kcal/d (7820 kJ/d) and the proportion of physically active adults increased from 30% to 67%. These changes affected the whole population and were sustained for almost 5 years.
• The result was widespread modest weight loss (4–5 kg, or 5%–6% of body weight) and a decline in all-cause mortality and rates of death from diabetes and cardiovascular disease.
• Countries such as Canada and the United States, where more than half the population is either overweight or obese, could benefit from health policies whose aim is population-wide weight loss.
• Population changes would need to be made at all social and political levels, including provincial, territorial and municipal levels and at schools, workplaces and households.
• Interventions should include making fruits and vegetables more readily available and less expensive, reducing the availability and increasing the prices of high-energy foods, and promoting walking and bicycling as means of transportation.
Supplementary Material
Footnotes
Une version française de cet article est disponible à l'adresse www.cmaj.ca/cgi/content/full/178/8/1032/DC1
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. Manuel Franco, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, 2024 E Monument St., Ste. 2-607, Baltimore MD 21205, USA; fax 410 955-0476; mfranco@jhsph.edu
REFERENCES
- 1.Franco M, Ordunez P, Caballero B, et al. Impact of energy intake, physical activity, and population-wide weight loss on cardiovascular disease and diabetes mortality in Cuba, 1980–2005. Am J Epidemiol 2007;166:1374-80. [DOI] [PubMed]
- 2.Ordunez-Garcia PO, Nieto FJ, Espinosa-Brito AD, et al. Cuban epidemic neuropathy, 1991 to 1994: history repeats itself a century after the “amblyopia of the blockade.” Am J Public Health 1996;86:738-43. [DOI] [PMC free article] [PubMed]
- 3.Ministerio de Salud Publica. Estadísticas de salud en Cuba. Havana (Cuba): Ministerio de Salud Publica; 2006.
- 4.Caballero B. The global epidemic of obesity: an overview. Epidemiol Rev 2007;29:1-5. [DOI] [PubMed]
- 5.Tjepkema M. Measured obesity: adult obesity in Canada — measured height and weight. In: Nutrition: findings from the Canadian Community Health Survey. Ottawa: Statistics Canada; 2007. Cat no 82-620-MWE2005001. Available: www.statcan.ca/english/research/82-620-MIE/2005001/pdf/aobesity.pdfm (accessed 2008 Jan 23).
- 6.Wang Y, Beydoun MA. The obesity epidemic in the United States — gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6-28. [DOI] [PubMed]
- 7.Flegal KM. The epidemic of obesity: What's in a name? [editorial] Int J Epidemiol 2006;35:72-4. [DOI] [PubMed]
- 8.Caballero B, Wang Y. Obesity and mortality–light at the end but still a long tunnel [editorial]. Int J Epidemiol 2006;35:21-2. [DOI] [PubMed]
- 9.Flegal KM, Graubard BI, Williamson DF, et al. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005;293:1861-7. [DOI] [PubMed]
- 10.Flegal KM, Graubard BI, Williamson DF, et al. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 2007;298:2028-37. [DOI] [PubMed]
- 11.Ryan DH, Espeland MA, Foster GD, et al. Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials 2003;24:610-28. [DOI] [PubMed]
- 12.Look AHEAD Research Group. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care 2007;30:1374-83. [DOI] [PMC free article] [PubMed]
- 13.Phelan S, Wyatt HR, Hill JO, et al. Are the eating and exercise habits of successful weight losers changing? Obesity (Silver Spring) 2006;14:710-6. [DOI] [PubMed]
- 14.Rose G. Sick individuals and sick populations. Int J Epidemiol 2001;30:427-32. [DOI] [PubMed]
- 15.Drewnowski A. The real contribution of added sugars and fats to obesity. Epidemiol Rev 2007;29:160-71. [DOI] [PubMed]
- 16.Commission on the Social Determinants of Health, World Health Organization. Measurement and evidence knowledge network. The social determinants of health: developing an evidence base for political action. Geneva: The Organization; 2007.
- 17.Lau DCW, Douketis JD, Morrison KM, et al. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 2007;176:S1-13. [DOI] [PMC free article] [PubMed]
- 18.Raine K, Wilson E. Obesity prevention in the Canadian population: policy recommendations for environmental change. CMAJ 2007;176:S106-10.
- 19.Franco M, Nandi A, Glass T, et al. Smoke before food: a tale of Baltimore City. Am J Public Health 2007;97:1178. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.