Abstract
Background
Asthma accounts for considerable burden on health care, but in most cases, asthma can be controlled. Quality-of-care indicators would aid in monitoring asthma management. We describe the quality of asthma care using a set of proposed quality indicators.
Methods
We performed a retrospective cross-sectional study using health databases in Saskatchewan, a Canadian province with a population of about 1 million people. We assessed 6 quality-of-care indicators among people with asthma: admission to hospital because of asthma; poor asthma control (high use of short-acting β-agonists, admission to hospital because of asthma or death due to asthma); no inhaled corticosteroid use among patients with poor control; at least moderate inhaled corticosteroid use among patients with poor control; high inhaled corticosteroid use and use of another preventer medication among patients with poor control; and any main preventer use among patients with poor control. We calculated crude and adjusted rates with 95% confidence intervals. We tested for differences using the χ2 test for proportions and generalized linear modelling techniques.
Results
In 2002/03, there were 24 616 people aged 5–54 years with asthma in Saskatchewan, representing a prevalence of 3.8%. Poor symptom control was observed in 18% of patients with asthma. Among those with poor control, 37% were not dispensed any inhaled corticosteroids, and 40% received potentially inadequate doses. Among those with poor control who were dispensed high doses of inhaled corticosteroids, 26% also used another preventer medication. Hospital admissions because of asthma were highest among those aged 6–9 years and females aged 20–44 years. Males and those in adult age groups (predominantly 20–44 years) had worse quality of care for 4 indicators examined.
Interpretation
Suboptimal asthma management would be improved through increased use of inhaled corticosteroids and preventer medications, and reduced reliance on short-acting β-agonist medications as recommended by consensus guidelines.
Asthma is a chronic respiratory disease that can limit patients' activity levels, reduce their quality of life and increase their likelihood of being admitted to hospital; it is also a rare cause of death.1 The prevalence of asthma has recently increased in industrialized countries,2–4 and over 2 million Canadians have asthma.5 According to survey data, asthma prevalence in Canada in 2003 was 8.4% among people aged 12 years or more,6 with rates in Saskatchewan just below the national average at 8.1%. In the United States in 2001–2003, asthma prevalence among people of all ages was reported at 7.2%.7 This has led to a considerable burden on health care systems.
Asthma can be controlled,8 and guidelines defining control have been published.9,10,11 Evidence-based guidelines for asthma care include patient education, appropriate diagnosis, recognition of symptoms, identification and removal of environmental triggers, and use of medications (primarily maintenance therapy with inhaled corticosteroids and acute symptom relief with short-acting β-agonists).9,10,11
Health care administrative databases allow the evaluation of adherence to asthma management guidelines on a population level. We report the quality of asthma care in a provincial health system using 6 easy-to-measure indicators and existing administrative databases.12
Methods
Study design and population
There are about 1 million people who live in Saskatchewan, Canada. The median age is 36.7 years and 49.7% are male.13 There are 13 municipalities classified as cities, which account for 56% of the province's population.13 About 99% of residents receive the province's universal medical coverage.14 With regards to prescription drug coverage, the Government of Saskatchewan provides some benefits to residents under the Prescription Drug Plan, such as copayments when a family exceeds a deductible. It is estimated that in this jurisdiction there are 1 400 people per physician.13 The Lung Association of Saskatchewan is the premier source of asthma resources for patients and health care professionals.15 This organization has trained a number of certified asthma educators who are licensed health care professionals and work in communities across the province. In addition, there are asthma clinics established in several urban centres.
We performed a retrospective cross-sectional study using data from 2 fiscal years (Apr. 1–Mar. 31, 2002/03 and 2003/04). We used data from 2002/03 to identify asthma cases and to determine asthma prevalence. We included Saskatchewan residents who had a valid health insurance number at the mid-point of the fiscal year. We excluded people aged 5 years or less to avoid difficulties associated with diagnoses of bronchiloitis or bronchitis, and we excluded those aged 54 years or more to avoid difficulties associated with diagnoses of chronic obstructive pulmonary disease. We excluded patients with cystic fibrosis because they commonly receive antiasthma medications. We excluded First Nations people with registered Indian status because data on their prescription drug use are not available in provincial databases. In 2003/04, we measured asthma quality-of-care indicators among people who had been identified as having asthma in 2002/03 and who still lived in the region. We used different years to identify cases (2002/03) and to measure quality-of-care indicators (2003/04) to avoid artifactual findings.
The University of Saskatchewan biomedical research ethics board determined that this study did not require ethical review because it involved the secondary analysis of de-identified data, it did not require contact with research participants and only aggregated results were reported.
Quality-of-care indicators
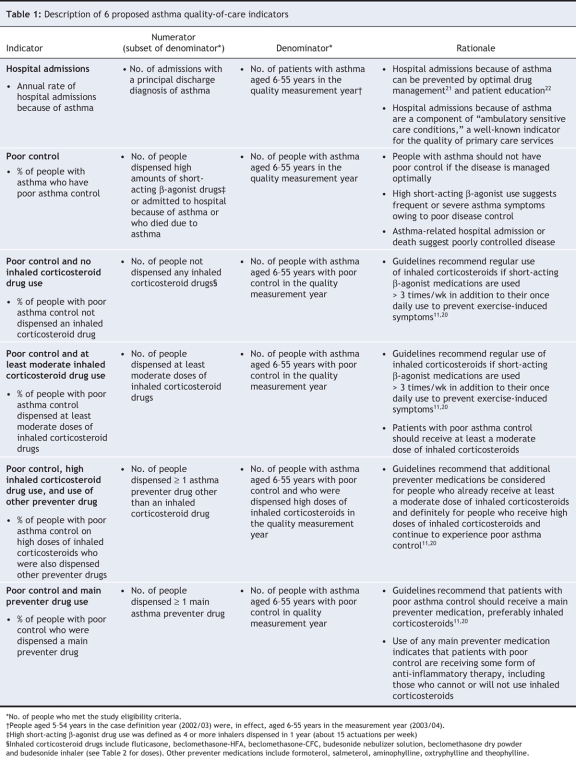
Using literature reviews16–19 and local expert input, we developed quality-of-care indicators and definitions based on 1999 and 2001 Canadian consensus guidelines for asthma.11,20 Table 1 provides a description of the 6 proposed asthma quality-of-care indicators included in our study.
Table 1
We classified a person as having asthma if he or she met at least 1 of the following criteria in a 1-year period: 3 or more prescriptions dispensed for an antiasthma drug; 2 or more physician services claims for asthma (International Classification of Diseases, 9th revision [ICD-9] code 493); 2 or more hospitalization claims for asthma (ICD-9 493.x or ICD-10 J45.x in any diagnostic field); 1 or more claims for physician services for asthma and 1 or more pharmacy claim for an antiasthma drug; or 1 or more hospitalization claim for asthma and 1 or more pharmacy claim for an antiasthma drug. This case definition is part of the Health Plan Employer Data and Information Set,23 a quality measurement system used by the National Committee for Quality Assurance in the United States.
We extracted data from 6 health administrative databases that were linked by use of anonymous personal identifiers. Database linkage was 99.9% successful. We identified age, sex, urban or nonurban residence location and health insurance status from the Person Registry System database, and we tracked physician visits using the Physician Services database. We identified hospital admissions from the Hospital Discharge Abstract database and medication use from 2 prescription drug databases. We used the Vital Statistics database to identify deaths caused by asthma. Validation studies specific to asthma deaths and admission to hospital have been completed using Saskatchewan Health databases.24,25
For hospital admission rates, we included admissions with a principal discharge diagnosis of asthma (ICD-9 493.x or ICD-10 J45.x) and an admission date during the measurement year. If a patient was transferred between facilities, all temporally contiguous admissions were considered part of the same hospital admission.
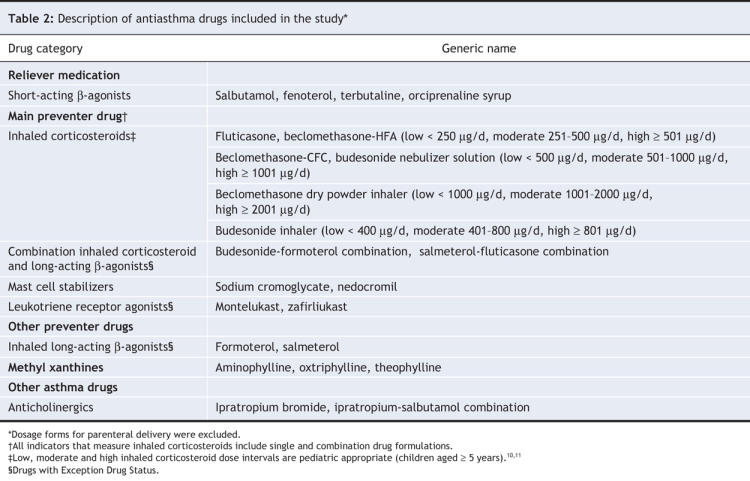
The antiasthma drugs that were available on the provincial drug formulary during the study period are presented in Table 2. We excluded tiotropium (rarely used for asthma) and oral corticosteroids (not specific for asthma). The definitions of low, moderate and high yearly inhaled corticosteroid use are shown in Table 2.10,11 These dose ranges are also appropriate for children aged 5 years or more.10,11
Table 2
The 1999 and 2001 Canadian asthma guidelines suggest that short-acting β-agonist medications should be used no more than 3 times per week with 1 additional dose allowed per day before exercise,11,20 which equates to 3 inhalers each year. We defined high short-acting β-agonist use as more than 4 inhalers dispensed in a 1-year period (about 15 actuations per week), which allows for the maximum recommended dose and lost or spare inhalers. A pediatrician and pediatric respirologist deemed this definition to be valid for children aged 5 years or more. Short-acting β-agonists administered by different inhalation methods were converted to an equivalent salbutamol puffer dose (100 μg by metered dose inhaler). Poor asthma control was defined as high use of short-acting β-agonists, admission to hospital for asthma or death caused by asthma in the measurement year. Further methodologic technical details have been described.12
We assigned people to urban or nonurban residence locations according to definitions used by Statistics Canada.26 Information about residence location was missing for less than 0.5% of people with asthma. People missing this information were excluded from our analysis of residence location.
Statistical analysis
We stratified indicators by age, sex and urban or nonurban residence location. For each variable, we calculated crude and adjusted rates with corresponding 95% confidence intervals (CI). Rates for age and sex were adjusted for sex and age, respectively, by use of the variable denominator population. Similarly, the rates for urban or nonurban residence location were adjusted for age and sex. All indicators were tested for interaction between age and sex. If an interaction was identified, we reported the data by sex and age. We tested for differences between binomial variables using the χ2 test for proportions. For nonbinomial variables, we used generalized linear regression modelling techniques to compare the index group to the mean rate across all other groups within the categorizing variable. For hospital admission rates, we tested for significance between males and females for each age group using a Poisson model. The level of significance was set at α = 0.05.
Results
In 2002/03, 3.8% (24 616/650 752) of eligible people in Saskatchewan met the asthma case definition (Table 3). In 2003/04, 24 180 people who met the same definition in 2002/03 were still alive and living in the region. Of these, 49% were female, and the mean age was 27.3 (standard deviation [SD] 15) years.
Table 3
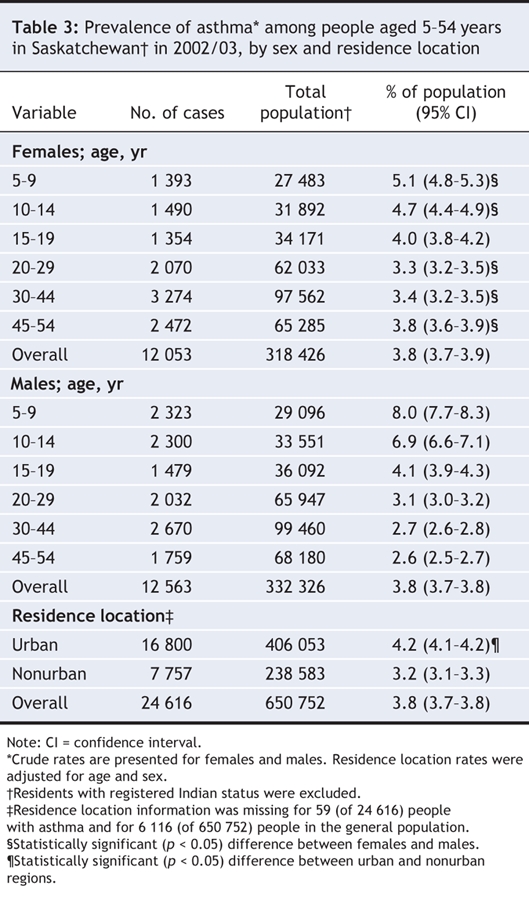
We identified a significant interaction between age and sex. For both males and females, asthma prevalence was highest among children aged 5–9 years, and it declined with age. The prevalence of asthma was higher among males in the younger age groups (aged 5–14 years), and it was higher among females in the adult age groups (aged 20-54 years) (Figure 1). Asthma prevalence was significantly higher among those who lived in urban areas (4.2%) compared with those who lived in nonurban areas (3.2%).
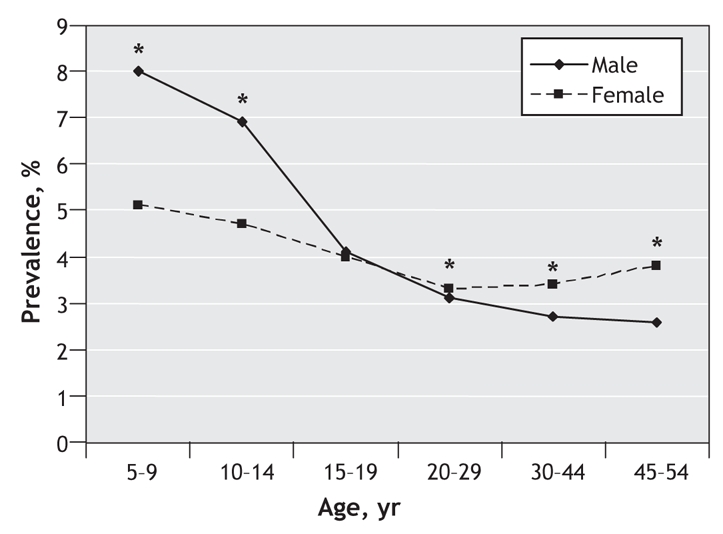
Figure 1: Prevalence of asthma in Saskatchewan by age and sex in 2002/03. *Significant difference (p < 0.05) between males and females.
There were 263 hospital admissions because of asthma in 2003/04, representing 10.9 admissions per 1000 people with asthma aged 6–55 years, with significant interaction between age and sex. Among females, admission rates were highest among girls aged 6–9 years and women aged 20–44 years, and the rates were lowest among youth aged 10–14 years (Table 4). Among males, admission rates were highest among boys aged 6–9 years and lowest among men aged 30–44 years. Among females aged 20–44 years, hospital admission rates were 3 times greater than those among males (Figure 2), which was a larger than expected difference based on prevalence.
Table 4
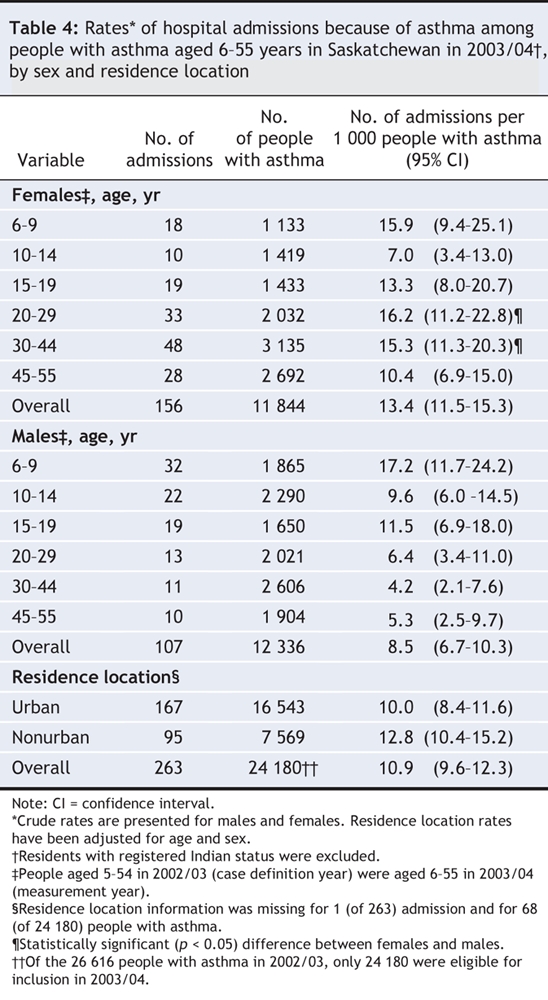
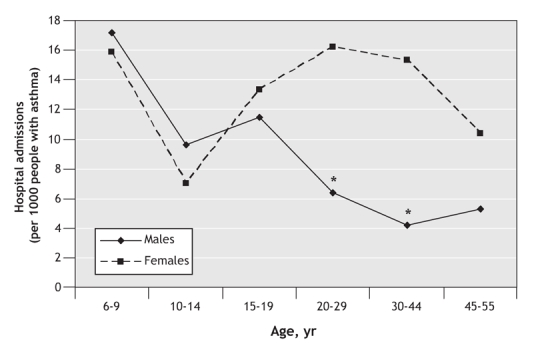
Figure 2: Rates of hospital admission because of asthma among people with asthma in Saskatchewan in 2003/04. *Significant difference (p < 0.05) between males and females.
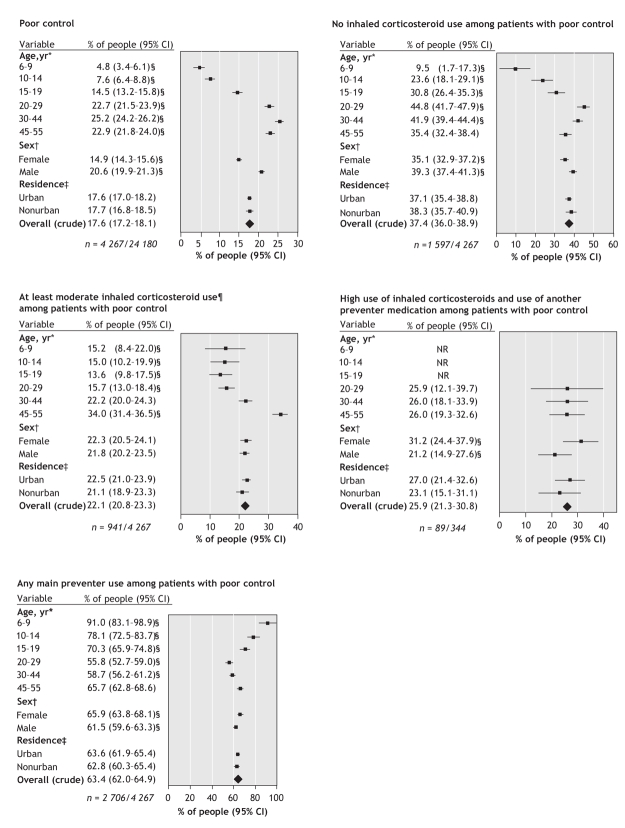
Among the 24 180 people with asthma, 47.9% were dispensed a preventer medication (46.4% received inhaled corticosteroids and 5.8% received an alternative preventer drug). Of those with asthma, 18% (4267) had poor control (Figure 3), and 97% of those with poor control had high use of short-acting β-agonists. There were fewer than 6 deaths due to asthma. The rate of poor control increased with age and was higher among males compared with females.
Figure 3: Rates of asthma quality-of-care indicators in Saskatchewan in 2003/04. All rates, except crude overall rates, were adjusted using the indicator denominator population (Table 1). Residents with registered Indian status were excluded from our study. Of the cases identified in 2002/03 (26 616), 24 180 were eligible for inclusion in 2003/04. *Adjusted for sex. †Adjusted for age. ‡Adjusted for age and sex. §Significantly different (p < 0.05) from the rate across all other categories within the variable group. ¶At least moderate inhaled corticosteroid use was defined as ≥ 251 μg/d for fluticasone and beclomethasone-HFA, ≥ 501 μg/d for beclomethasone-CFC and budesonide nebulizer solution, ≥ 1001 μg/d for beclomethasone dry powder inhaler, ≥ 401 μg/d for budesonide inhaler. Note: CI = confidence interval, NR = not reported (owing to a sample size of less than 6).
Among those with poor asthma control, 37% (1597/4267) did not use inhaled corticosteroids (Figure 3). Poor control was lowest among children aged 6–9 years and highest among adults aged 20–44 years. Males were significantly more likely than females to have poor control and to not use inhaled corticosteroids. Overall, 22% of those with poor control were dispensed moderate or high doses of inhaled corticosteroids. The rate of at least moderate inhaled corticosteroid use was lowest among people aged 6–29 years and was highest among people aged 45–55 years. There was no differences in the rate of at least moderate doses of inhaled corticosteroids between males and females.
Of people with poor asthma control who used high doses of inhaled corticosteroids, 26% (89/344) of patients also received another asthma preventer medication (Figure 3). There were no significant differences by age, and females were significantly more likely than males to take another preventer medication.
Of those with poor asthma control, 63.4% (2706/4267) were dispensed 1 or more main asthma preventer medication (Figure 3). Almost all children aged 6–9 years with poor control were dispensed preventer medications. The use of preventer medications decreased with age and was lowest among those aged 20–44 years. The rate of preventer medication use was significantly higher among females compared with males.
There were no significant differences in hospital admission rates or in any of the 5 drug quality indicators between urban and nonurban residence locations.
Interpretation
Based on our system-wide indicators of asthma quality of care, we found that asthma management was suboptimal. In a health system with an asthma prevalence of 3.8%, nearly 1 in 5 people with asthma had poor control that required overly frequent use of short-acting β-agonists (> 4 inhalers dispensed in a 1-year period). National surveys report that over half of people with asthma experience frequent symptoms6 or poor control.5,27,28
Among those with poor control, 37% did not receive any inhaled corticosteroids and 40% received potentially inadequate doses. Inhaled corticosteroids reduce asthma symptoms, exacerbations and hospital admissions.21,29 Furthermore, those with poor control who take high doses of inhaled corticosteroids may benefit from additional preventer medications. However, in our study the number of such patients who received 1 or more additional preventer medications was fewer than expected (26%). Among those with poor control, use of main preventer medications was lowest among people aged 20 years or more.
Most (91%) children aged 6–9 years with poor asthma control received at least some inhaled corticosteroids. However, relatively few received a moderate dose, suggesting a problem with underdosing. Among adults aged 20–44 years, more than 2 of 5 patients received no inhaled corticosteroids. Of adults dispensed inhaled corticosteroids, most received less than a moderate dose. This would also suggest insufficient dosing.
The higher rate of poor control among males compared with females is unexpected. Other studies have suggested women have more symptoms than men.6,30 Comparison of our criteria for poor asthma control with validated references was outside the scope of this study and may be a limitation. Males with poor control were also less likely than females to use preventer medications as recommended by Canadian guidelines for 3 of the 4 prescribing indicators.
Several pharmacoepidemiologic studies that used data from administrative databases have defined asthma severity to investigate asthma outcomes.21,24,29,31 We could find no other comparative studies that proposed a definition for poor control. A key principle is the differentiation between asthma “control” and asthma “severity.”8 Current guidelines9,10 stress establishing and achieving certain treatment goals that define ideal asthma control. These goals are the same for all degrees of asthma severity.
Our findings are comparable to other studies performed using health databases. A Californian study that used data from managed care administrative databases reported that 60% of patients aged 5–56 years received a controller medication and 13% received 6 or more short-acting β-agonist canisters each year.32 A study in Florida that used automated dispensing data found that 8.2% patients overused short-acting β-agonists (more than 2 consecutive early refills).33 Of these people, 48% did not receive a concomitant preventer medication.
In our study, the rate of hospital admissions because of asthma was 10.9 per 1000 people with asthma. The age and sex patterns for admissions because of asthma are comparable to other findings in Canada34 and the United States.35 Although Canadian survey data has identified the prevalence of asthma in Saskatchewan as being below the national mean (8.1% v. 8.4% among patients aged 12 years or more),6 the rate of hospital admissions because of asthma in Saskatchewan (among those aged 5–54 years) is higher than the national mean (64.6 v. 47.6 per 100 000 residents) (Louise McRae, Public Health Agency of Canada, Ottawa, Ont.; personal communication, 2007). Nonstandardized systems for diagnosing asthma and regional differences in disease management could possibly explain these contradictory findings.
A recent study found there has been no improvement in asthma control since 1999 in Canada.28 This survey largely concluded that self-reported treatment measures aimed at controlling asthma were not widely adopted. Our system-wide approach provided actual measures of quality indicators rather than self-reported assessments. Despite the differences in approaches, both studies concluded that asthma control was suboptimal. As the result of differences in methods, temporal comparisons of quality of care are unreliable except from a global perspective. Data from 15 years earlier,24 although not strictly comparable in terms of both the topics addressed and the medications available at that time, appears to show more overuse and abuse of short-acting β-agonists and less use of inhaled corticosteroids than observed in the current study. This suggests improvement in treatment patterns that should correlate with improvement in control.
Our proposed quality-of-care indicators can be easily measured and will be useful in monitoring asthma control and system-wide interventions over time. In addition, they will be useful to compare asthma control between institutions, regions and health care systems. Our indicators provide governments, agencies, educators and researchers with a measurement tool to profile aspects of asthma care.
Despite the existence of certified asthma educators, asthma information and education resources, and several asthma clinics, there appears to be suboptimal asthma care in Saskatchewan. There are many potential reasons why our study found suboptimal asthma management, including differences in disease management between children and adults; differences in behaviour between age groups and between males and females; insufficient patient knowledge; poor coordination of care; and inadequate guideline dissemination to physicians. Several evidence-based approaches that could inform policy and system based strategies for improving the quality of asthma care are possible, including individualized self-management programs with patient education;22 decision-support tools such as asthma care flow sheets;36 delivery of care by an interdisciplinary team;37,38 interactive health professional education programs;39 and drug formulary regulations aimed at influencing prescribing practices.40
Our study has several limitations. We used databases constructed for administrative purposes. Physician billing databases capture only 1 diagnosis per visit and may not capture services provided by nurses or non–fee-for-service practitioners. Some asthma drugs were not captured in our database, including drugs dispensed to inpatients and nonidentifiable recipients of federally-funded drug programs (e.g., members of the Canadian Forces and the Royal Canadian Mounted Police, veterans and federal inmates), drugs given as free samples and nonapproved exception drug status prescriptions. Additionally, diagnostic information, prescriptions written but not dispensed and patient adherence were not captured by drug claims. Data for most dimensions of control (nocturnal awakenings, limitation in activities and exacerbations) were not available in the databases, hence, poor asthma control among our study population could be underestimated. Allowing for 1 lost inhaler per patient per year in our definition of high short-acting β-agonist use may have also contributed to an underestimation of poor control. Finally, by setting an upper age limit of 54 years, we were unable to completely rule out the possibility of asthma being misdiagnosed as chronic obstructive pulmonary disease.
We used high-quality health services data for nearly a complete provincial population and elaborate analytic methods. We determined that asthma management in Saskatchewan is suboptimal and that it would be improved by increased use of inhaled corticosteroids and preventer medications and by reduced reliance on short-acting β-agonist medications. These strategies should also reduce hospital admissions because of asthma. Although we completed a literature review and consulted with an expert advisory panel, the asthma indicators that are included in this study have not been validated with the databases used. Studies to validate the use of measurement tools such as the quality-of-care indicators used in this study should be the focus of future research. Further research is also needed to explain the age-and sex-related differences in guideline-based prescribing practices among patients with poor asthma control. Features in our study may be useful in other jurisdictions to monitor the quality of care for asthma.
@ See related article page 1027
Acknowledgments
We thank the following members of our expert panel for their contribution to the development of the proposed quality indicators included in our study: Bill Cannon, Dr. Jerry Danielson, Dr. Biswa Datta, Jan Haffner, Dr. Kumar Ramlall, Dr. Donna Rennie and Pat Smith.
Footnotes
Une version française de ce résumé est disponible à l'adresse www.cmaj.ca/cgi/content/full/178/8/1013/DC1
This article has been peer reviewed.
Contributors: Helena Klomp, Joshua Lawson, Donald Cockcroft, Benjamin Chan and Laurie Gander contributed to the study conception and design. Benjamin Chan acquired the data, which was analyzed and interpreted by Helena Klomp, Joshua Lawson, Donald Cockcroft, Benjamin Chan, Paul Cascagnette and Derek Jorgenson. The manuscript was drafted by Helena Klomp and Joshua Lawson, and Don Cockcroft took a prominant role in editing and assisting with revisions. All of the authors revised the manuscript critically and approved the final version submitted for publication.
This study was based in part on nonidentifiable data provided by the Saskatchewan Ministry of Health. The interpretations and conclusions do not necessarily represent those of Saskatchewan or the Saskatchewan Ministry of Health.
Competing interests: Donald Cockcroft has received honoraria for talks from AstraZeneca Canada, GlaxoSmithKline Canada, Merck Canada and Novartis Canada, and he has served on the advisory boards of AstraZeneca Canada, Merck Canada and Novarits Canada. None declared for Helena Klomp, Joshua Lawson, Benjamin Chan, Paul Cascagnette, Laurie Gander and Derek Jorgenson.
Correspondence to: Helena Klomp, Health Quality Council, Atrium Building, Innovation Place, 241-111 Research Dr., Saskatoon SK S7N 3R2; fax 306 668-8820; hklomp@hqc.sk.ca
REFERENCES
- 1.Canadian Institute for Health Information, Canadian Lung Association, Health Canada and Statistics Canada. Respiratory disease in Canada. Ottawa: The Institute; 2001. Available: www.phac-aspc.gc.ca/publicat/rdc-mrc01/index.html (accessed 2008 Jan 24).
- 2.Burney PG, Chinn S, Rona RJ. Has the prevalence of asthma increased in children? Evidence from the National Study of Health and Growth 1973-86. BMJ 1990;300:1306-10. [DOI] [PMC free article] [PubMed]
- 3.Mannino DM, Homa DM, Pertowski CA, et al. Surveillance for Asthma — United States, 1960–1995. MMWR CDC Surveill Summ 1998;47:1-27. [PubMed]
- 4.Senthilselvan A. Prevalence of physician-diagnosed asthma in Saskatchewan, 1981–1990. Chest 1998;114:388-92. [DOI] [PubMed]
- 5.Glaxo Wellcome Inc. Asthma in Canada: a landmark survey. Mississauga (ON): Glaxo Wellcome Inc.; 2000.
- 6.Chen Y, Johansen H, Thillaiampalam S, et al. Asthma. Health Rep 2005;16:43-53. Ottawa (ON): Statistics Canada. Available: www.statcan.ca/bsolc/english/bsolc?catno=82-003-X20040027790 (accessed 2008 Jan 24).
- 7.Moorman JE, Rudd RA, Johnson CA, et al. National surveillance for asthma — United States, 1980–2004. MMWR Surveill Summ 2007;56:1-54. [PubMed]
- 8.Cockcroft DW, Swystun VA. Asthma control versus asthma severity. J Allergy Clin Immunol 1996;98:1016-8. [DOI] [PubMed]
- 9.The Global Initiative for Asthma. Global Strategy for Asthma Management and prevention. Hamilton (ON): The Initiative; 2007. Available: www.ginasthma.com/Guidelineitem.asp?l1=2&l2=1&intId=60 (accessed 2007 Feb 19).
- 10.Lemiere C, Bai T, Balter M, et al. Adult asthma consensus guidelines update 2003. Can Respir J 2004;11(Suppl A):9A-18A. [DOI] [PubMed]
- 11.Boulet L, Becker A, Berube D, et al. Canadian asthma consensus report, 1999. CMAJ 1999;161(Suppl 11):1-5. [PMC free article] [PubMed]
- 12.Klomp H, Chan BTB, Jorgenson D, et al. Breathing easier: opportunities to improve the quality of asthma care in Saskatchewan. Saskatoon: Health Quality Council; 2005. Available: www.hqc.sk.ca/portal.jsp?FYxWfvhNG6wYVt25tmlroTBIzBf0QfLQkUwK4QBZaJtKSe5JQ5jXNFVvI5thiwzu (accessed 2008 Feb 19).
- 13.Government of Saskatchewan Publications Centre. Saskatchewan: The Government; 2007. Available: www.publications.gov.sk.ca/prdtermlist.cfm?t=1307&p=7809 (accessed 2008 Feb 19).
- 14.Downey W, Stang M, Beck P, et al. Health services databases in Saskatchewan. In: Strom BL, editor. Pharmacoepidemiology. 4th ed. Mississauga (ON): John Wiley & Sons; 2005. p. 296.
- 15.The Lung Association of Saskatchewan. Programs and events. Saskatoon (SK): The Association; 2006. Available: www.sk.lung.ca/content.cfm?edit_realword=programs (accessed 2008 Feb 25).
- 16.Baker DF, Marks GB, Poulos LM, et al. Review of proposed National Health Priority Area asthma indicators and data sources. Canberra: Australian Institute of Health and Welfare; 2004.
- 17.Report on recommended metrics for monitoring asthma care. 2Department of Defense and Veterans Health Administration (DoD/VA) asthma guideline expert panel. Available: www.mamc.amedd.army.mil/Clinical/medcom_asthma/Asthma_Metrics_Report_6_25.doc (accessed 2007 Feb 19).
- 18.National Quality Measures Clearinghouse. Quality measures for asthma. The Clearinghouse; 2004. Available: www.qualitymeasures.ahrq.gov/search/searchresults.aspx?Type=3&txtSearch=asthma&num=20 (available 2008 Feb 19).
- 19.Pearson M, Goldacre M, Coles J, et al., eds. Health outcome indicators: asthma. Report of a working group to the Department of Health. Oxford: National Centre for Health Outcomes Development; 1999.
- 20.Boulet LP, Bai TR, Becker A, et al. What's new since the last (1999) Canadian Asthma Consensus Guidelines? Can Respir J 2001;8(Suppl A):5A-27A. [DOI] [PubMed]
- 21.Senthilselvan A, Lawson JA, Rennie DC, et al. Regular use of corticosteroids and low use of short-acting beta2-agonists can reduce asthma hospitalization. Chest 2005;127:1242-51. [DOI] [PubMed]
- 22.Gibson PG, Powell H, Coughlan J, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2003;(1):CD00117. [DOI] [PubMed]
- 23.Stuart B, Singhal PK, Magder LS, et al. How robust are health plan quality indicators to data loss? A Monte Carlo simulation study of pediatric asthma treatment. Health Serv Res 2003;38:1547-61. [DOI] [PMC free article] [PubMed]
- 24.Spitzer WO, Suissa S, Ernst P, et al. The use of beta-agonists and the risk of death and near death from asthma. N Engl J Med 1992;326:501-6. [DOI] [PubMed]
- 25.Ernst P, Habbick B, Suissa S, et al. Is the association between inhaled beta-agonist use and life-threatening asthma because of confounding by severity? Am Rev Respir Dis 1993;148:75-9. [DOI] [PubMed]
- 26.Metropolitan areas 2001. Ottawa: Statistics Canada; 2001. Available: http://stds.statcan.ca/english/sgc/2001/2001-cma-searchstruc1.asp?criteria=47 (accessed 2008 Feb 14).
- 27.GlaxoSmithKline Inc. Asthma in Canada: a landmark survey [pediatric version]. Mississauga (ON): GlaxoSmithKline; 2001.
- 28.McIvor RA, Boulet LP, FitzGerald JM, et al. Asthma control in Canada: no improvement since we last looked in 1999. Can Fam Physician 2007;53:672-7. [PMC free article] [PubMed]
- 29.Suissa S, Ernst P, Kezouh A. Regular use of inhaled corticosteroids and the long term prevention of hospitalization for asthma. Thorax 2002;57:880-4. [DOI] [PMC free article] [PubMed]
- 30.Manfreda J, Becklake MR, Sears MR, et al. Prevalence of asthma symptoms among adults aged 20-44 years in Canada. CMAJ 2001;164:995-1001. [PMC free article] [PubMed]
- 31.Blais L, Suissa S, Boivin JF, et al. First treatment with inhaled corticosteroids and the prevention of admissions to hospital for asthma. Thorax 1998;53:1025-9. [DOI] [PMC free article] [PubMed]
- 32.Schatz M, Nakahiro R, Crawford W, et al. Asthma quality-of-care markers using administrative data. Chest 2005;128:1968-73. [DOI] [PubMed]
- 33.Winterstein AG, Hartzema AG. Pharmacy-specific quality indicators for asthma therapy. Res Social Adm Pharm 2005;1:430-45. [DOI] [PubMed]
- 34.Chen Y, Stewart P, Johansen H, et al. Sex difference in hospitalization due to asthma in relation to age. J Clin Epidemiol 2003;56:180-7. [DOI] [PubMed]
- 35.Skobeloff EM, Spivey WH, St Clair SS, et al. The influence on age and sex on asthma admissions. JAMA 1992;268:3437-40. [PubMed]
- 36.Ruoff G. Effects of flow sheet implementation on physician performance in the management of asthmatic patients. Fam Med 2002;34:514-7. [PubMed]
- 37.Wagner EH. Effective teamwork and quality of care. Med Care 2004;42:1037-9. [DOI] [PubMed]
- 38.Schulz M, Verheyen F, Muhlig S, et al. Pharmaceutical care services for asthma patients: a controlled intervention study. J Clin Pharmacol 2001;41:668-76. [DOI] [PubMed]
- 39.Davis RS, Bukstein DA, Luskin AT, et al. Changing physician prescribing patterns through problem based learning: an interactive, teleconference case-based education program and review of problem-based learning. Ann Allergy Asthma Immunol 2004;93:237-42. [DOI] [PubMed]
- 40.Kephart G, Sketris IS, Bowles SK, et al. Impact of a criteria-based reimbursement policy on the use of respiratory drugs delivered by a nebulizer and health care services utilization in Nova Scotia. Pharmacotherapy 2005;25:1248-57. [DOI] [PubMed]